Abstract
Introduction
The adverse physical consequences of female genital mutilation/cutting (FGM/C) have been thoroughly investigated and documented. Yet, we know little about the adverse mental health consequences of the practice. To fill this research gap, we systematically reviewed studies that assessed any adverse mental health consequences related to FGM/C.
Methods
We searched four databases from inception to 21 December 2018. We then reviewed all titles and abstracts for relevant studies. We used the National Institutes of Health quality assessment tool to appraise the quality of each study and the Newcastle-Ottawa Scale to rate the risk of bias within studies.
Results
We included 16 studies in this review; only six studies examined the association between FGM/C and adverse mental health outcomes as the sole research question. Among the included studies, 10 were conducted at the participants’ country of origin. The sample size of the populations studied ranged from 3 to 4800 participants. Only one study received a rating of ‘good’ methodological quality.
Fourteen of the 16 studies reported an association between FGM/C and at least adverse mental health outcome. These included eight studies that reported a higher burden of adverse mental health outcomes among women who underwent FGM compared with women who did not undergo FGM/C. Four studies reported a correlation between the severity of FGM/C and the severity of adverse mental health outcomes.
Conclusion
This systematic review documents an association between FGM/C and adverse mental health outcomes. Importantly, our review demonstrates the need for more rigorous research on the topic.
Keywords: female genital mutilation/cutting, FGM/C, depression, PTSD, anxiety, mental health
Key questions.
What is already known?
There are more than 200 million women and girls who have undergone female genital mutilation/cutting (FGM/C), living in 30 countries around the globe. Further, about 3 million girls remain at risk of being subjected to FGM/C annually.
There has been an increased interest in studying the adverse health outcomes associated with FGM/C over the past few decades. The adverse physical consequences of FGM/C have been thoroughly investigated and documented. We know, however, very little about the adverse mental health consequence of the practice.
Despite poor mental health being cited as a consequence of the practice in most reports on FGM/C, data documenting the prevalence and severity of such consequences are sparse.
What are the new findings?
The quality of the studies assessed is generally weak.
Our systematic review documents an association between FGM/C (especially among severe cases of FGM/C) and adverse mental health outcomes.
What do the new findings imply?
Future work should create more rigorous evidence, particularly on the correlation between FGM/C type and severity of adverse mental health outcomes.
Introduction
The total number of women and girls who have undergone female genital mutilation/cutting (FGM/C) is unknown. However, the United Nations International Children’s Emergency Fund estimates that there are currently more than 200 million women and girls who have undergone FGM/C, living in 30 countries around the globe.1 Moreover, while the overall rate of the practice is declining, about 3 million girls remain at risk of being subjected to FGM/C annually.2 3 The practice is most prevalent in Eastern, Northeastern, Western regions of Africa, a number of countries in the Middle east and Asia, and asylum seekers and migrant communities from these countries—mainly to high-income countries.4 5
FGM/C refers to any practice that involves deliberately cutting, injuring or changing the external female genitalia. As such, the FGM/C ranges from ritual superficial nicks to the complete removal of the external genitalia. FGM/C is often performed for cultural, religious or other non-medical reasons; often on girls between the ages of 4 and 10.6 7 WHO identifies four types of FGM/C based on the procedure and severity; type III being the most severe.8 There is a near global consensus for the need to protect girls from undergoing FGM/C, evidenced by the fact that FGM/C is illegal in most countries.3 9 Moreover, the practice is considered a violation of the international human rights laws.5 A number of international agencies and government have recently been advocating for investing in the provision of adequate care to address the health-related consequences of FGM/C.5
Over the past few decades, there has been an increased interest in studying the adverse health outcomes associated with FGM/C. The adverse physical consequences of FGM/C have been thoroughly investigated and documented.10–13 We know, however, very little about the adverse mental health consequence of the practice. Despite poor mental health plausibly being a potential consequence of FGM/C, data accurately documenting such outcomes are sparse. Prior efforts to examine the state of the evidence on adverse mental health outcomes were often non-systematic in their approach or only reported mental health disorders in conjunction with sexual health-related outcomes of women who underwent FGM/C.14–16 To our knowledge, to date, there has been no systematic effort to synthesise the evidence that examines the adverse mental health outcomes associated with FGM/C in the public health or medical literature.
To fill this research gap, we systematically reviewed studies that assessed any adverse mental health consequences related to FGM/C. This review aimed to answer the question: what are the psychological disorders associated with undergoing FGM/C?
Methods
Search strategy
We conducted a search across the following bibliographic databases: PubMed,17 Embase,18 Web of Science19 and PsycINFO20 from inception to 21 December 2018. We present the detailed search strategies in online supplementary file 1. Overall, we combined various synonyms for FGM/C with terms focusing on mental health outcomes including various synonyms for mental health, depression, anxiety and post-traumatic stress disorder (PTSD). To maximise the number of studies identified, we applied no filters (except for a filter limiting the sex of participants to female in PsycINFO database). We also conducted a manual search of the references of included studies from the database search and prior reviews on the FGM/C to account for any records we might have missed.
bmjgh-2019-001553supp001.pdf (37.8KB, pdf)
Study identification and abstraction
Following deduplication using the reference management software Mendeley, we screened the titles and abstracts of identified records to decide whether we should appraise the full paper using the systematic reviews web app Rayyan QCRI. We then screened full texts to determine whether to include or exclude articles. We excluded articles if the study was qualitative in nature, did not report psychological outcome(s), or if the full text was not written in English.
We abstracted included studies into an electronic form (Microsoft Excel). In the abstraction form, we summarised the research question(s), study population and sample size, psychological outcomes investigated, tools used for psychological assessment and study results. We present a flow chart, guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, describing the study selection process and number of articles retrieved, included and excluded in figure 1.
Figure 1.
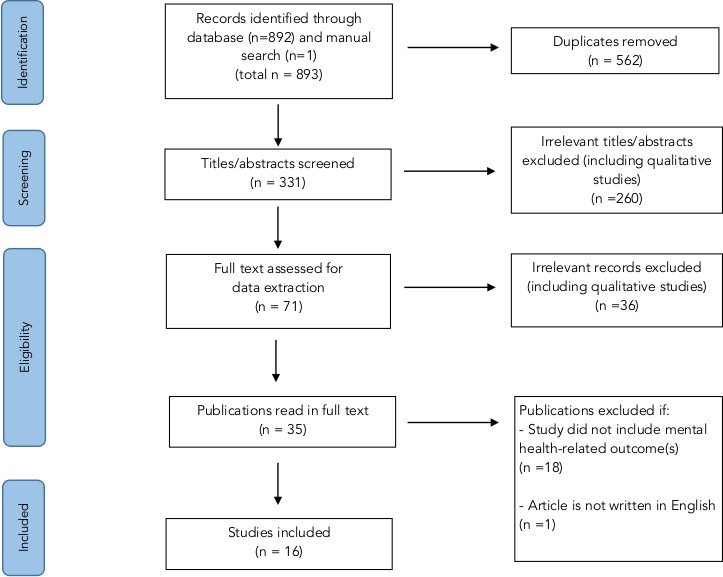
Flow chart describing the study selection process and number of articles retrieved, included and excluded.
Study quality assessment and risk of bias
No study was excluded from this review on the basis of methodological quality. We did, however, use the US Department of Health and Human Services, National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies to appraise and report on the quality of each study.21 The answers to the tool measures were ‘yes’, ‘no’, ‘not mentioned’ or ‘not relevant’. We then rated the studies as of ‘poor’, ‘fair’ or ‘good’ methodological quality.
Guided by the Newcastle-Ottawa Scale for risk assessment of non-randomised trials, we then assessed the risk of bias for each of the included studies. We assessed each study on risk of bias in participant selection (representativeness, size and non-respondents to study sample), comparability (reporting on different exposure groups) and exposure/outcome relationship measurement (quality of outcome assessment methods and appropriateness of statistical methods used for analysis).22 23 For each study, we then rated levels of risk as ‘low level of risk’, ‘high level of risk’ and ‘unclear risk’. The last category indicates that the information needed for adequate assessment was inconclusive or unavailable.
Patient and public Involvement
Patients were not involved in conducting this review.
Results
We describe the research questions, study population and sample size, mental health outcomes investigated, tools used for psychological assessment, key results and methodological quality of the 16 studies included in this review in detail in table 1.
Table 1.
Summary of key components of the 16 reviewed studies
| Author, year | Research question(s) | Study population | Mental health outcomes investigated | Tools used for psychological assessment related to FGM/C | Results (presence of mental health consequences for FGM/C) | Study quality |
| Ahmed et al, 201724 | What is the relationship between female genital mutilation (FGM) and psychiatric problems among adolescent girls? | Sample size: 204 (135 underwent FGM/C and 69 did not) adolescent girls ages between 14 and19 in Egypt. | Somatisation, depression, anxiety, hostility, phobic anxiety, obsessive–compulsive, interpersonal sensitivity, paranoid ideation, and psychoticism | Symptoms check list 90 (SCL-90) | This study did not stratify the results based on FGM/C type. Girls who underwent FGM/C had significantly higher scores than those in the non-FGM/C group for the following conditions: somatisation (33.5 vs 20.6), depression (31.7 vs 26.3), anxiety (32.1 vs 21.2), phobic anxiety (20.4 vs 14.6) and hostility (19.6 vs 16.4). Girls who underwent FGM/C had higher, but not statistically significant, scores than those in the non-FGM/C group for the following conditions: obsessive–compulsive (6.8 vs 6.6) and interpersonal sensitivity (5.5 vs 5.1). Both groups had the same mean score for paranoid ideation (3.8) and the non-FGM/V group had a higher mean score for psychoticism compared with the FGM/C group (3.2 vs 3.1). Further, there were significant differences in the three global distress indices between the FGM/C and non-FGM/C study groups, respectively: GSI (19.3% vs 7.2%), PSDI (16.3% vs 4.3%) and PST (17.0% vs 5.8%). | Fair |
| Akinsulure-Smith, 201429 | What are the experiences related to female genital cutting within an immigrant community? | Sample size: 23 (7 underwent FGM/C and 16 did not) women ages between 20 and 57 living in the USA. Countries of origin: Sierra Leone and Liberia. | PTSD and depression | PTSD: PTSD CheckList – Civilian Version. Depression: Center for Epidemiologic Studies Depression Scale. |
This study did not stratify the results based on FGM/C type. The mean score for depression scale was higher among women who did not undergo FGM/C (37.5) compared with those underwent the practice (35.4). The mean score for PTSD scale was higher among women who underwent FGM/C (29.9) compared with those who did not undergo the practice (29.2). Both measures did not detect statistically significant differences between the two groups. | Poor |
| Applebaum et al, 200825 | What is the prevalence of PTSD symptoms and other psychiatric complaints among women who had undergone ritual female genital surgery compared with an age-matched control group of women who had not undergone ritual female genital surgery? | Sample size: 37 (19 underwent FGM/C and 18 did not) Bedouin women ages 30–81 in Israel. | PTSD, somatisation, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism | PTSD: PTSD Inventory (based on DSM) Other conditions: Symptom Checklist- 90 (SCL-90). |
This study did not stratify the results based on FGM/C type. The mean PTSD symptom score was higher among the group that underwent FGM/C compared with the group that did not (57.3 vs 48.1). The mean score for obsessive–compulsive scale was also higher among those who underwent FGM/C (1.6 vs 1.4). The mean score for depression (1.8 vs 1.6), anxiety (1.4 vs 1.3) and hostility (0.8 vs 0.7) was higher among women who did not undergo FGM/C. The mean scores of the scales for somatisation (1.6), interpersonal sensitivity (1.1), phobic anxiety (0.8), paranoid ideation (0.7) and psychoticism (0.5) were similar in the two groups. Overall, all measures did not detect statistically significant differences between the two groups. | Fair |
| Behrendt and Moritz, 20057 | What is the relationship between FGM and psychiatric illnesses, especially PTSD? | Sample size: 47 (23 underwent FGM/C and 24 did not) girls and women ages 15–40 in Dakar, Senegal. | PTSD, affective disorder and anxiety. | Mini International Neuropsychiatric Interview. | This study did not stratify the results based on FGM/C type. Over 90% of the women who underwent FGM/C described feelings of intense fear, helplessness, horror and severe pain, and over 80% were still suffering from intrusive re-experiences of their circumcision. The prevalence of mental health consequences among women who underwent FGM/C was high: PTSD (30.4%), anxiety disorders (26.2%), and effective disorder (21.7%). In the control group, only one participant fulfilled the diagnostic criteria for an affective disorder. None of the women in the control group PTSD or other anxiety disorder. | Poor |
| Chibber et al, 201030 | What is the prevalence of female genital cutting among pregnant women and what is the possible association with adverse pregnancy and psychological outcomes? | Sample size: 4800 (1892 underwent FGM/C 2958 did not) girls and women ages 15–46 in Kuwait. | PTSD, affective disorder and anxiety | Mini International Neuropsychiatric Interview | This study stratified the results based on FGM/C type. Among women who underwent FGM/C types II and III, 80% continued to have flashbacks to the event; 58% had affective disorder (OR 24.6 (95% CI 1.9 to 22.2) compared with women who did not undergo FGM/C; 38% had other anxiety disorders and 30% had PTSD. None of the women who did not undergo FGM/C reported PTSD or anxiety disorders. | Fair |
| Daneshkhah et al, 201731 | What are the consequences of female circumcision on sexual function of circumcised women? Also, what is the status of FGM, its prevalence, predominant method/type of female circumcision and attitude to this practice? | Sample size: 200 (140 underwent FGM/C and 60 did not) girls and women ages 15–49 in Iran. | Somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression | The General Health Questionnaire-28 item (GHQ-28) | This study did not stratify the results based on FGM/C type. The mean score for social dysfunction (7.30 vs 7.21) and severe depression (4.87 vs 4.30) scales were higher among women who underwent FGM/C while the mean score for somatic symptoms (6.58 vs 5.99), anxiety and insomnia (6.20 vs 5.98) were higher among women who did not undergo FGM/C. Overall, none of the measures detected statistically significant differences between the two groups. | Fair |
| Elnashar and Abdelhady, 200732 | What is the rate of female genital cutting among a sample of newly married women? Also, what are the differences between women who underwent FGM those who did not regarding long-term health problems including psychological symptoms? | Sample size: 264 (200 underwent FGM/C and 64 did not) newly married women (less than 5 years) ages 15–49 in Benha city, Egypt. | Symptoms of somatisation, depression, anxiety, hostility and phobia | Symptoms check list 90 (SCL 90) | This study did not stratify the results based on FGM/C type. The mean scores of mental health symptoms were higher among the group that underwent FGM/C for all conditions: somatisation (33.2 vs 21.7), depression (30.1 vs 29.9), anxiety (31.5 vs 22.3), hostility (18.7 vs 16.9) and phobia (22.5 vs 15.3). Results of symptoms of somatisation, anxiety and phobia were statistically significant. | Poor |
| Kizilhan, 201126 | Is there an association between FGM and psychiatric illnesses, PTSD in particular? | Sample size: 140 (79 underwent FGM/C and 61 did not (30 from the same geographic area and 31 from a different area)) Kurdish girls, ages 8–14 in Northern Iraq. | PTSD, depression, anxiety, somatoform disorders, personality disorder and somatic disturbance. | PTSD: Arabic version of Child PTSD Reaction Index. Depression: Arabic version of the Children’s Depression Index The Cooper Smith Self-Esteem Inventory |
This study did not stratify the results based on FGM/C type. Over 78% of the girls who underwent FGM/C described feelings of intense fear, helplessness, severe pain and horror. Over 74% were still suffering from intrusive re-experiences of their circumcision. The study reports significantly higher mean score of PTSD symptoms (44.3 vs 14.50 vs 13.61) and depression disorder symptoms (33.6 vs 11.07 vs 12.09) among girls who underwent FGM/C compared with the mean scores of the two comparison groups of girls who did not undergo the practice. Further, girls who underwent FGM/C reported higher prevalence of multiple mental health outcomes compared with the control group of girls who did not undergo the practice but lived in the same area including: anxiety disorder (45.6% vs 6.7%), somatoform disorders (21.5% vs 3.3%), personality disorder (13.9% vs 0%) and somatic disturbance (36.7% vs 26.7). | Fair |
| Knipscheer et al, 201533 | What kind of mental health problems are reported by circumcised immigrant women from Africa? And which factors are associated with the presented psychopathology? | Sample size: 66 Immigrant women ages 18–69 in the Netherlands. Countries of origin: Somalia, Sudan, Eritrea, Ethiopia and Sierra Leone. | PTSD, depression and anxiety | PTSD: Harvard Trauma Questionnaire-30 item (HTQ-30). Depression and anxiety: Hopkins Symptom Checklist (HSCL-25). |
This study stratified the results based on FGM/C type. Of the research participants, 36% scored above the cut-off level for indicators of psychopathology. 20% met the criteria for PTSD. 33% met the criteria for depression. 30% met the criteria for an anxiety disorder. 18% scored above the cut-off level for all three psychopathology indicators. Women who underwent FGM/C type III reported a vivid memory of the circumcision and coped with their symptoms in an avoidant way, and reported experiencing severe consequences of genital circumcision | Fair |
| Köbach et al, 201827 | Is FGM associated with a heightened risk of PTSD and trauma-related shutdown dissociation? Also, is it associated with depression, anxiety, substance abuse and dependence, suicidality and psychosis? | Sample size: 167 (87 underwent FGM/C type II/III, 60 underwent FGM/C type I and 18 did not) girls and women between the ages 13–80 in Jijiga, Ethiopian Somali Region. | PTSD, depression, anxiety, substance abuse and dependence, suicidality and psychosis | PTSD diagnosis: PTSD Symptom Scale-Interview Shutdown syndrome: Shutdown Dissociation Scale (ShuD) Depression and anxiety symptoms: Hopkins Symptom Checklist-25 (HSCL-25) Major depression diagnosis: Mini-International Neuropsychiatric Interview. |
This study stratified the results based on FGM/C type. Regardless of the level of physical invasiveness, almost all women who underwent FGM/C reported having felt intense fear and/or helplessness. FGM/C types II/III, the more invasive forms, were associated with a statistically significant greater vulnerability to symptoms of PTSD, shutdown dissociation, depression and anxiety. Of the women who underwent FGM/C types II/III, 18.4% were diagnosed with PTSD, 12.6% with major depression, 4.6% with substance dependence, 1.1% with substance abuse, 10.3% with suicidal ideation and 2.3% psychotic disorder. Among women who underwent FGM/C type I, 1.7% were diagnosed with substance abuse and 8.3% with suicidal ideation. None were diagnosed with PTSD, major depression or psychotic disorder. Among women who did not undergo FGM/C, 5.4% were diagnosed with PTSD and 11.1% with substance dependence. None were diagnosed with major depression substance abuse, suicidal ideation or psychotic disorder. | Good |
| Koolaee et al, 201234 | How does marital satisfaction, mental health and sexual satisfaction compare between genital mutilated females and those who are not? | Sample size: 200 (100 underwent FGM/C and 100 did not) girls and women between the ages 15–35 in Kermanshah, Iran. | Somatic symptoms, sleep disorder and depression | GHQ-28. | This study did not stratify the results based on FGM/C type. The mean score of somatic symptoms (7.10 vs 5.86), depression (4.68 vs 3.75) and sleep disorder (7.84 vs 5.84) symptoms was higher among the group that underwent FGM/C. Only the results on sleep disorder were statistically significant. | Poor |
| Lever et al, 201828 | What is the mental health status of FGM/cutting (FGM/C)-affected women who are seeking asylum primarily due to their FGM/C status, as well as other gender-based persecutions? | Sample size: 13 women > 18 years of age who were seeking asylum in the USA primarily due to FGM/C. Countries of origin included: Burkina Faso, Djibouti, The Gambia, Guinea, Liberia, Nigeria and Sierra Leone. | Depression, anxiety and PTSD | Depression and anxiety: Hopkins Symptom Checklist-25 (HSCL-25). HTQ Revised-Part IV. |
This study did not stratify the results based on FGM/C type. Of the 13 women, checklist positive scores indicated anxiety in 12 of 13 (92%), and depression in 13 of 13 (100%) respondents, respectively. All seven women (100%) screened for PTSD had checklist positive scores, indicating they met the criteria for PTSD. | Fair |
| Mahmoudi and Hosseini, 201735 | Do couples in which the female underwent FGM/C vary from couple in which the female did not undergo the practice on relationship characteristics such as relationship satisfaction, sexual satisfaction, intimacy, spousal support and mental health? | Sample size: 414 couples (206 women underwent FGM/C and 208 in couples where women did not undergo the practice) in Kermanshah in Iran. | Overall psychological consequences | Symptom Checklist- 25 (SCL-25). | This study did not stratify the results based on FGM/C type. A significant difference was observed in mental health between women who underwent FGM/C (mean score=30.90) in comparison to women who did not (mean score=22.76). | Fair |
| Pereda et al, 201236 | What is the impact of FGM in the variable of mental health (focusing on the psychological and sexual areas) among adult immigrant women living in a European country? | Sample size: three women ages 35–45 in Spain. County of origin: Mauritania | Overall psychological consequences | Not specified | This study did not stratify the results based on FGM/C type. The psychological assessment did not reveal any significant problems. | Poor |
| Vloeberghs et al, 201237 | Does FGM/C lead to mental, social and/or relational problems? And if so, what is the nature of these problems, and which factors contribute to the development of problems? Also, what are the coping mechanisms these migrant women develop in relation to their problems and the above-mentioned factors? | Sample size: 66 Immigrant women ages 18–69 in the Netherlands. Countries of origin: Somalia, Sudan, Eritrea, Ethiopia and Sierra Leone. | PTSD, depression, and anxiety | For PTSD: HTQ-30. For depression and anxiety: Hopkins Symptom Checklist (HSCL-25). |
This study stratified the results based on FGM/C type. Of the participants, 17.5% met the criteria for PTSD, 34.9%met the criteria for depression, 31.7% met the criteria for an anxiety disorder. The mean score for HTQ-30 and HSCL-25 (psychological assessment tools) increased as the severity of FGM type increased. | Fair |
| Vrachnis et al, 201238 | What are the effects and consequences of FGM/C in women that visited an oand gynaecology department at a hospital? | Sample size: seven women who underwent FGM/C ages 17–31, in Greece. Countries of origin are: Ethiopia, Egypt, Eritrea and Somalia | Overall psychological consequences | Not specified | This study did not stratify the results based on FGM/C type. The study did not provide quantitative results of psychological assessment. | Poor |
DSM, Diagnostic and Statistical Manual; PTSD, post-traumatic stress disorder.
Research questions
Of the 16 studies we included, six focused solely on the adverse mental outcomes of FGM/C.7 24–28 The other 10 studies examined a variety of FGM/C-related health measures, including adverse mental health outcomes.29–38
Study population and sample size
Studies varied in both characteristics of populations studied and sample size. While a number of studies restricted their populations to a specific ethnic group or age category, others included a wide range of demographic characteristics. Ten studies were conducted at the participants’ country of origin: Egypt, Ethiopia, Iran, Iraq, Israel, Kuwait and Senegal7 24–27 30–32 34 35 and six studies targeted migrant women in Greece, the Netherlands, Spain and the USA.28 29 33 36–38 Seven studies examined potential adverse mental health outcomes spanning adolescence and adulthood,7 27 30–32 34 38 six studies restricted their populations to adults,25 28 29 33 36 37 two studies to adolescents24 26 and one study35 did not list participants’ age range. While the majority of studies focused on recruiting women, one study35 recruited couples. The sample size of populations studied ranged from 3 to 4800 participants.
Study design
All studies were cross-sectional in nature and did not follow participants over time. Eleven studies used comparison groups of women who did not undergo FGM/C7 24–27 29–32 34 35 while five studies reported results only from women who underwent FGM/C.28 33 36–38
Measurement of adverse mental health outcomes
Studies used a variety of instruments for psychological assessment. Four studies used the Hopkins symptoms check list 25 (SCL 25) to assess the burden of depression and anxiety.27 28 33 37 Three studies used the SCL 90 to assess the burden of somatisation, depression, anxiety, hostility and phobia.24 25 32 Three studies used the mini international neuropsychiatric interview to assess either the burden of PTSD, affective disorder, anxiety7 30 or the burden of depression.37 Two studies used the General Health Questionnaire-28 item to assess the burden of somatic symptoms, insomnia, social dysfunction and depression.31 34 Two studies used the Harvard Trauma Questionnaire-30 item to assess the burden of PTSD.28 37
Instruments used in one study to assess the burden of PTSD included the PTSD CheckList-Civilian Version,29 PTSD Inventory,25 Arabic version of Child PTSD Reaction Index26 and PTSD Symptom Scale-Interview.28 Instruments used in one study to assess the burden of depression included the Center for Epidemiologic Studies Depression Scale29 and the Arabic version of the Children’s Depression Index.26 One study used the SCL-25 to assess the overall the burden of mental health disorders.35 Two studies did not provide information on the instruments used for psychological assessment.36 38
Study quality assessment and risk of bias
Studies varied in quality but the majority received a rating of ‘fair’ quality. Only one study received a rating of ‘good’ quality,27 nine studies received a rating of ‘fair’ quality24–26 28 30 31 33 35 37 and six studies received a rating of ‘poor’ quality.7 29 32 34 36 38 Lack of sample size justification, limited assessment of confounding factors (lifetime traumatic events in particular) and lack of outcome stratification based on FGM/C type were the most common limitations. Moreover, the majority of studies did not report on the participation rate of individuals eligible for the study or whether outcome assessors were blinded to the exposure status of participants. We present the detailed quality assessment of each study in online supplementary file 2.
bmjgh-2019-001553supp002.pdf (77.1KB, pdf)
Among the three types of risk of bias we assessed, studies reported the highest risk of bias in exposure/outcome relationship measurement (eight studies) followed by comparability (four studies), then selection risk of bias (two studies). A rating of ‘unclear risk’ was given to 11 studies when assessing selection risk of bias, 10 studies when assessing comparability risk of bias and 7 studies when assessing exposure/outcome relationship measurement risk of bias. We present the detailed risk of bias assessment of each study in figure 2.
Figure 2.
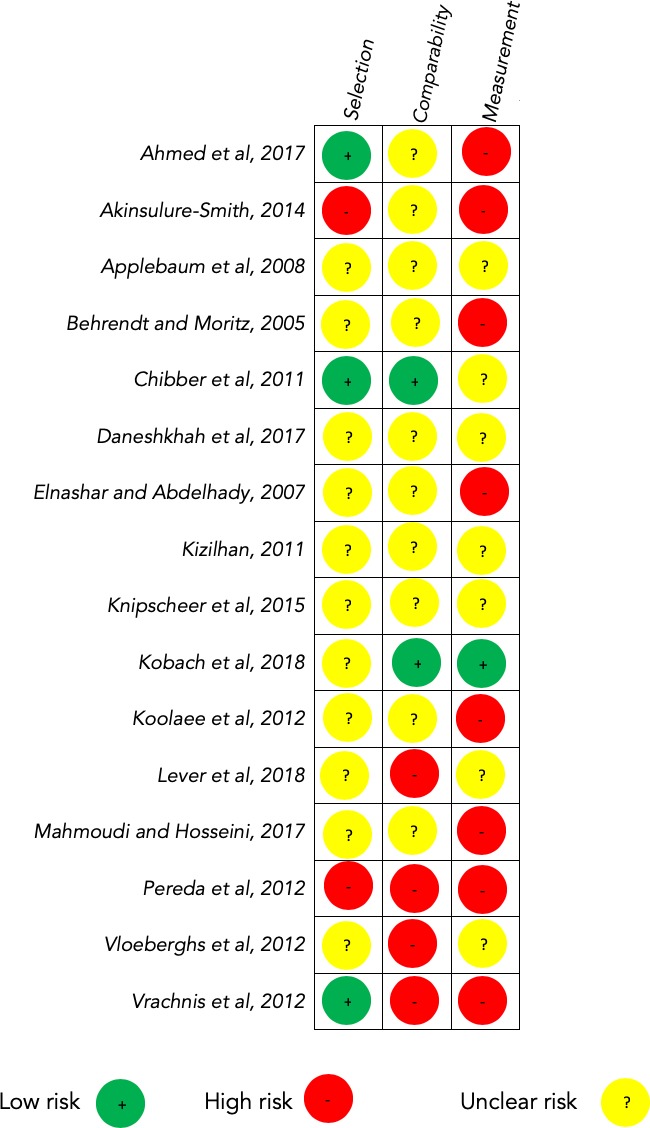
Reviewers' judgement about risk of bias for each item across included studies.
Exposure to lifetime traumatic events
Lifetime traumatic events can confound reported mental health outcomes.39 Yet, only four studies7 25 27 29 explicitly reported on lifetime traumatic events when examining the association between FGM/C and adverse mental health outcomes. Three studies7 25 29 used ‘lifetime traumatic events’ as a demographic variable of study participants. Only one study27 identified ‘lifetime traumatic events’ as a variable predictive of adverse mental health outcomes incorporated in a regression model.
Overall study results
Fourteen out of the 16 studies reported an association between FGM/C and at least 1 adverse mental health outcome7 24–35 37; five of these studies explicitly noted that the results were not statistically significant for all25 29 31 or some outcomes.32 34 Of the remaining two studies, one study36 concluded that there was no association between FGM/C and adverse mental health outcomes and the other study38 did not provide reportable results.
When stratified by study design, 11 studies7 24–27 29–32 34 35 also assessed the burden of adverse mental health outcomes among a comparison group (control group). In eight of these studies,7 24 26 27 30 32 34 35 there was a higher burden of adverse mental health outcomes among women who underwent FGM/C compared with the control group. In the remaining three studies25 29 31 that assessed a control group, the results were mixed, that is, some of adverse mental health outcomes measured were higher among the group that did not undergo FGM/C. Another five studies28 33 36–38 did not use a control group. Among these, three studies28 33 37 reported an association between FGM/C and adverse mental health outcomes.
Study results stratified by mental health outcome
As shown in figure 3, results differed depending on the mental health outcome assessed. Of the 11 studies that assessed depression as an outcome, three studies29 32 34 received a rating of ‘poor’ methodological quality. Six studies24 26 27 31 32 34 reported a higher burden of depression among women who underwent FGM/C compared with the control group of women who did not undergo FGM/C; two of these studies31 32 explicitly noted that the results were not statistically significant. Conversely, two studies25 29 reported a higher burden of depression among women who did not undergo FGM/C; both studies explicitly noted that the results were not statistically significant. Three studies28 33 37 that only assessed women who underwent FGM/C—that is, no control group—reported a high burden of depression among participants.
Figure 3.
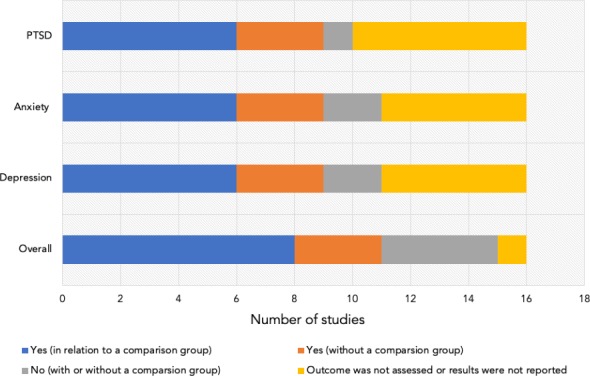
Overview of studies examining the association between FGM/C and adverse mental health outcomes. FGM/C, female genital mutilation/cutting; PTSD, post-traumatic stress disorder.
Among the 11 studies that assessed anxiety as an outcome, two studies7 32 received a rating of ‘poor’ methodological quality. Six studies7 24 26 27 30 32 reported a higher burden of anxiety among women who underwent FGM/C compared with the control group of women who did not undergo FGM/C. Conversely, two studies25 31 reported a higher burden of anxiety among women who did not undergo FGM/C; both studies noted that their results were not statistically significant. Three studies28 33 37 that only assessed women who underwent FGM/C—no control group—reported a high burden of anxiety among participants; one of these studies33 explicitly noted that the results were not statistically significant.
Of the 10 studies that assessed PTSD as an outcome, one study7 received a rating of ‘poor’ methodological quality. Six studies7 25–27 29 30 33 reported a higher burden of PTSD among women who underwent FGM/C compared with the control group of women who did not undergo FGM/C; among these, two studies25 29 noted that the results were not statistically significant. Conversely, one study31 reported a higher burden of PTSD among women who did not undergo FGM/C; the study explicitly noted that the results were not statistically significant. Three studies28 33 37 that only assessed women who underwent FGM/C—no control group—reported a high burden of PTSD among participants.
Other notable adverse mental health outcomes assessed included somatic symptoms (six studies7 24 26 30 32 34; all reported an association), overall affective disorder (two studies7 30; both reported an association) and overall psychological consequences (three studies35 36 38; one reported an association35).
Study results stratified by geographical location
Of the 10 studies conducted at the participants’ country of origin, three studies7 32 34 received a rating of ‘poor’ methodological quality. Eight of the 10 studies7 24 26 27 30 32 34 35 reported a higher burden of adverse mental health outcomes among women who underwent FGM/C compared with the control group of women who did not undergo FGM/C. Conversely, two studies25 31 reported mixed results, that is, some outcomes were higher among the group that did not undergo FGM/C.
Of the six studies that targeted migrant women, three studies29 36 38 received a rating of ‘poor’ methodological quality. One study29 that compared adverse mental health outcomes between women who underwent FGM/C and women who did not undergo FGM/C reported mixed results. Three studies28 33 37 that only assessed women who underwent FGM/C—no control group—reported a high burden of adverse mental health outcomes among participants. One study36 without a control group reported a lack of association between FGM/C and adverse mental health outcomes and another study38 did not provide reportable results.
Study results stratified by FGM/C type
Four studies27 30 33 37 investigated whether FGM/C type (severity) affected the severity of adverse mental health outcomes. All four studies reported a correlation between the severity of FGM/C and the severity of adverse mental health outcomes. FGM/C type III (the most severe form) had the highest association with adverse mental health outcomes.
Discussion
In a comprehensive review of the literature about the relation between FGM/C and adverse mental health outcome, we found that of the 16 studies included, 14 reported an association between FGM/C and at least 1 adverse mental health outcome. The studies that examined specific mental health outcomes consistently reported an association between FGM/C and that particular outcome. The four studies that stratified their results by FGM/C type found an association between the severity of FGM/C and the severity adverse mental health outcomes. Importantly, our review found that of the included studies only one received a rating of ‘good’ methodological quality. Further, the majority of studies reported ‘high risk of bias’ or ‘unclear risk’ in one or more of the categories used to assess risk of bias.
Our findings are consistent with results of prior smaller reviews. For example, the review by Berg et al (included four studies), reported an association between FGM/C and adverse mental health outcomes. The same review highlighted the lack of rigour in study design and methods in included studies (all studies received a rating of ‘moderate’ or ‘low’ quality).14 In their literature review on the long-term health consequences of FGM/C, Reisela and Creighton concluded that the FGM/C led to long-term adverse psychological outcomes (based on three studies).16 Our review adds to the literature through providing a more comprehensive overview of existing research on adverse mental health outcomes linked to FGM/C. Further, we provide a quality assessment for existing literature on the subject.
This review is not without limitations. First, like all systematic reviews, our review is subject to publication bias. It is possible that studies that did not show an association with mental health outcomes were not published. However, the consistent presence of an association across studies—and the observation of a dose–response relationship between the severity of FGM/C and mental health outcomes in four studies—mitigates the concern that what we are seeing spurious findings due to publication bias. Second, all the studies included in our review are cross-sectional in nature, with a small sample size, and many do not account for confounding factors; lifetime traumatic events in particular. It is, therefore, difficult, from these studies, to isolate causality only to FGM/C and it is not implausible that the observed mental health consequences are attributable to a host of concomitant conditions that disadvantage the women studied. Third, the quality assessment tools we used, while designed for observational studies in general, may be limited when assessing cross-sectional studies. This limitation, however, is more reflective of the lack of proper tools to assess cross-sectional studies in general. Finally, due to the heterogeneity in the psychosocial assessment tools used by the studies, and the low quality of included studies, it was not possible to conduct a quantitative meta-analysis of the results. It is worth noting that these limitations highlight the need to invest in quality longitudinal research on the adverse mental health consequences of FGM/C.
Conclusion
While there is a large body of literature on the physical effects of FGM/C, there is little quantitatively measuring the mental health consequences of the practice. This review provides a comprehensive summary of the existing literature on the adverse mental health consequences of FGM/C. The observation that FGM/C is associated with adverse mental health outcomes should not be surprising. There is abundant evidence that traumatic event experiences are associated with adverse mental health outcomes over the life course.40 FGM/C, especially severe forms, can be a traumatic experience through deliberating inflicting of harm on girls, often without anaesthesia, at a particularly sensitive life course period. This review should set to rest, once and for all, the misconception that the cultural normalisation of FGM/C somehow minimises the adverse mental health consequences associated with this practice.15 This review shows that, in addition to the physical consequence of this practice, it is also associated with poor mental health outcomes that may accompany women throughout their lives.
Importantly, our review demonstrates the need for further, better quality, research on the topic. Based on our review, future research should aim to incorporate the following criteria to improve the methodological quality of evidence on the topic: 1) improve and standardise the psychological tools necessary to assess the association between FGM/C and adverse health outcomes; 2) independently investigate the board range of potential adverse mental health outcomes that may be associated with undergoing FGM/C; 3) stratify reported outcomes based on FGM/C type; 4) address and control for potential confounding, lifetime traumatic events in particular; and 5) use longitudinal study designs to document the full scope of the mental health consequences of FGM/C over time.
Footnotes
Handling editor: Seye Abimbola
Twitter: @SalmaMHAbdalla
Contributors: SMA concieved the design of the study. SMA led the analysis process with support and supervision from SG. SMA wrote the first draft and SG commented and edited all versions of the draft. Both authors read and approved the final draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No additional data are available.
References
- 1. UNICEF Female genital mutilation, 2018. Available: https://data.unicef.org/topic/child-protection/female-genital-mutilation/ [Accessed 26 Feb 2019].
- 2. Kandala N-B, Ezejimofor MC, Uthman OA, et al. Secular trends in the prevalence of female genital mutilation/cutting among girls: a systematic analysis. BMJ Glob Health 2018;3:e000549 10.1136/bmjgh-2017-000549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO Female genital mutilation, 2018. Available: https://www.who.int/news-room/fact-sheets/detail/female-genital-mutilation [Accessed 26 Feb 2019].
- 4. Simpson J, Robinson K, Creighton SM, et al. Female genital mutilation: the role of health professionals in prevention, assessment, and management. BMJ 2012;344:e1361 10.1136/bmj.e1361 [DOI] [PubMed] [Google Scholar]
- 5. WHO Eliminating female genital mutilation: An interagency statement - OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO. WHO. Geneva 2018. [Google Scholar]
- 6. WHO Female Genital Mutilation - Integrating the Prevention and the Management of the Health Complications into the curricula of nursing and midwifery: A Student’s Manual [Internet]. Geneva, 2001. Available: https://apps.who.int/iris/bitstream/handle/10665/66857/WHO_FCH_GWH_01.4.pdf?sequence=2 [Accessed 4 Mar 2019].
- 7. Behrendt A, Moritz S. Posttraumatic Stress Disorder and Memory Problems After Female Genital Mutilation. Am J Psychiatry 2005;162:1000–2. 10.1176/appi.ajp.162.5.1000 [DOI] [PubMed] [Google Scholar]
- 8. WHO Classification of female genital mutilation. World Health Organization, 2007. [Google Scholar]
- 9. Leye E, Deblonde J, García-Añón J, et al. An analysis of the implementation of laws with regard to female genital mutilation in Europe. Crime Law Soc Change 2007;47:1–31. 10.1007/s10611-007-9055-7 [DOI] [Google Scholar]
- 10. Berg RC, Odgaard-Jensen J, Fretheim A, et al. An updated systematic review and meta-analysis of the obstetric consequences of female genital mutilation/cutting. Obstet Gynecol Int 2014;2014:1:1–8. 10.1155/2014/542859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Banks E, Meirik O, Farley T, et al. Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet 2006;367:1835–41. 10.1016/S0140-6736(06)68805-3 [DOI] [PubMed] [Google Scholar]
- 12. Serour GI. Medicalization of female genital mutilation/cutting. African Journal of Urology 2013;19:145–9. 10.1016/j.afju.2013.02.004 [DOI] [Google Scholar]
- 13. Berg RC, Underland V, Odgaard-Jensen J, et al. Effects of female genital cutting on physical health outcomes: a systematic review and meta-analysis. BMJ Open 2014;4:e006316 10.1136/bmjopen-2014-006316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Berg RC, Denison E, Psychological FA. Social and Sexual Consequences of Female Genital Mutilation/Cutting (FGM/C): A Systematic Review of Quantitative Studies [Internet]. Norwegian Knowledge Centre for the Health Services. Knowledge Centre for the Health Services at The Norwegian Institute of Public Health 2010. (cited 2019 Feb 26). [PubMed] [Google Scholar]
- 15. Mulongo P, McAndrew S, Hollins Martin C. Crossing borders: Discussing the evidence relating to the mental health needs of women exposed to female genital mutilation. Int J Ment Health Nurs 2014;23:296–305. 10.1111/inm.12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Reisel D, Creighton SM. Long term health consequences of Female Genital Mutilation (FGM). Maturitas 2015;80:48–51. 10.1016/j.maturitas.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 17. Home - PubMed [Internet]. NCBI, 2019. Available: https://www.ncbi.nlm.nih.gov/pubmed [Accessed 19 Jan 2019].
- 18. Embase Embase, 2019. Available: https://www.embase.com/#search [Accessed 27 Feb 2019].
- 19. Web of Science Web of Science. Available: http://login.webofknowledge.com/error/Error?Error=IPError&PathInfo=%2F&RouterURL=http%3A%2F%2Fwww.webofknowledge.com%2F&Domain=.webofknowledge.com&Src=IP&Alias=WOK5 [Accessed 19 Jan 2019].
- 20. PsycINFO PsycINFO | EBSCO [Internet], 2019. Available: https://www.ebsco.com/products/research-databases/psycinfo [Accessed 27 Feb 2019].
- 21. NIH Study Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [Internet], 2019. Available: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Accessed 25 Feb 2019].
- 22. Allen LN, Pullar J, Wickramasinghe KK, et al. Evaluation of research on interventions aligned to WHO 'Best Buys' for NCDs in low-income and lower-middle-income countries: a systematic review from 1990 to 2015. BMJ Glob Health 2018;3:e000535 10.1136/bmjgh-2017-000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet] 2000.
- 24. Ahmed MR, Shaaban MM, Meky HK, et al. Psychological impact of female genital mutilation among adolescent Egyptian girls: a cross-sectional study. The European Journal of Contraception & Reproductive Health Care 2017;22:280–5. 10.1080/13625187.2017.1355454 [DOI] [PubMed] [Google Scholar]
- 25. Applebaum J, Cohen H, Matar M, et al. Symptoms of Posttraumatic Stress Disorder After Ritual Female Genital Surgery Among Bedouin in Israel. Prim. Care Companion J. Clin. Psychiatry 2008;10:453–6. 10.4088/PCC.v10n0605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kizilhan JI. Impact of psychological disorders after female genital mutilation among Kurdish girls in northern Iraq. Eur J Psychiatry 2011;25(2):92–100. [Google Scholar]
- 27. Köbach A, Ruf-Leuschner M, Elbert T. Psychopathological sequelae of female genital mutilation and their neuroendocrinological associations. BMC Psychiatry 2018;18:187 10.1186/s12888-018-1757-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lever H, Ottenheimer D, Atkinson HG, et al. Depression, Anxiety, Post-traumatic Stress Disorder and a History of Pervasive Gender-Based Violence Among Women Asylum Seekers Who Have Undergone Female Genital Mutilation/Cutting: A Retrospective Case Review. J Immigr Minor Heal 2018. [DOI] [PubMed] [Google Scholar]
- 29. Akinsulure-Smith AM. Exploring female genital cutting among West African immigrants. J Immigrant Minority Health 2014;16:559–61. 10.1007/s10903-012-9763-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chibber R, El-saleh E, El harmi J. Female circumcision: obstetrical and psychological sequelae continues unabated in the 21st century. The Journal of Maternal-Fetal & Neonatal Medicine 2011;24:833–6. 10.3109/14767058.2010.531318 [DOI] [PubMed] [Google Scholar]
- 31. Daneshkhah F, Allahverdipour H, Jahangiri L, et al. Mental Well-being and Quality of Life among Kurdish Circumcised Women in Iran. Iran J Public Health 2017;46:1265–74. [PMC free article] [PubMed] [Google Scholar]
- 32. Elnashar A, Abdelhady R. The impact of female genital cutting on health of newly married women. International Journal of Gynecology & Obstetrics 2007;97:238–44. 10.1016/j.ijgo.2007.03.008 [DOI] [PubMed] [Google Scholar]
- 33. Knipscheer J, Vloeberghs E, van der Kwaak A, et al. Mental health problems associated with female genital mutilation. BJPsych Bulletin 2015;39:273–7. 10.1192/pb.bp.114.047944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Koolaee AK, Pourebrahim T, Mohammadmoradi B, et al. The comparison of marital satisfaction and mental health in genital mutilated females and non-genital mutilated females. Int J high risk Behav Addict [Internet] 2012;1:115–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mahmoudi O, Hosseini E. Psychosexual complications of female genital mutilation for couples: A comparative study. J Kermanshah Univ Med Sci 2017;20:135–40. [Google Scholar]
- 36. Pereda N, Arch M, Pérez-González A. A case study perspective on psychological outcomes after female genital mutilation. J Obstet Gynaecol 2012;32:560–5. 10.3109/01443615.2012.689893 [DOI] [PubMed] [Google Scholar]
- 37. Vloeberghs E, van der Kwaak A, Knipscheer J, et al. Coping and chronic psychosocial consequences of female genital mutilation in the Netherlands. Ethn Health 2012;17:677–95. 10.1080/13557858.2013.771148 [DOI] [PubMed] [Google Scholar]
- 38. Vrachnis N, Salakos N, Iavazzo C, et al. Female genital mutilation in Greece. Clin Exp Obstet Gynecol 2012;39:346–50. [PubMed] [Google Scholar]
- 39. Turner RJ, Lloyd DA. Lifetime traumas and mental health: the significance of cumulative adversity. J Health Soc Behav 1995;36:360–76. 10.2307/2137325 [DOI] [PubMed] [Google Scholar]
- 40. Fink DS, Galea S. Life course epidemiology of trauma and related psychopathology in civilian populations. Curr Psychiatry Rep 2015;17:31 10.1007/s11920-015-0566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001553supp001.pdf (37.8KB, pdf)
bmjgh-2019-001553supp002.pdf (77.1KB, pdf)


