Abstract
Background
Large epidemics frequently emerge in conflict-affected states. We examined the cholera response during the humanitarian crisis in Yemen to inform control strategies.
Methods
We conducted interviews with practitioners and advisors on preparedness; surveillance; laboratory; case management; malnutrition; water, sanitation and hygiene (WASH); vaccination; coordination and insecurity. We undertook a literature review of global and Yemen-specific cholera guidance, examined surveillance data from the first and second waves (28 September 2016–12 March 2018) and reviewed reports on airstrikes on water systems and health facilities (April 2015–December 2017). We used the Global Task Force on Cholera Control’s framework to examine intervention strategies and thematic analysis to understand decision making.
Results
Yemen is water scarce, and repeated airstrikes damaged water systems, risking widespread infection. Since a cholera preparedness and response plan was absent, on detection, the humanitarian cluster system rapidly developed response plans. The initial plans did not prioritise key actions including community-directed WASH to reduce transmission, epidemiological analysis and laboratory monitoring. Coordination was not harmonised across the crisis-focused clusters and epidemic-focused incident management system. The health strategy was crisis focused and was centralised on functional health facilities, underemphasising less accessible areas. As vaccination was not incorporated into preparedness, consensus on its use remained slow. At the second wave peak, key actions including data management, community-directed WASH and oral rehydration and vaccination were scaled-up.
Conclusion
Despite endemicity and conflict, Yemen was not prepared for the epidemic. To contain outbreaks, conflict-affected states, humanitarian agencies, and donors must emphasise preparedness planning and community-directed responses.
Keywords: armed conflicts, cholera, communicable disease control, emergencies, epidemics
Key questions.
What is already known?
In the last decade, large-scale cholera epidemics have occurred in countries affected by conflict, political instability and/or population displacement including Iraq, Sierra Leone, Somalia, South Sudan, Tanzania and Zimbabwe.
While a multisector response (including coordination; case management; water, sanitation and hygiene; social mobilisation; and oral cholera vaccination) is well-defined in practice, the major barrier in fragile and conflict-affected states is the coordinated delivery of interventions in difficult logistical contexts.
What are the new findings?
Our analysis of the 2016–2018 cholera response in Yemen outlined five major challenges for the control of large epidemics in fragile and conflict-affected states and for global health security.
Major challenges included: (1) assuring sufficient cholera preparedness and planning, (2) increasing the capacity of surveillance and data management for epidemic monitoring, (3) decentralising and targeting cholera-specific water, sanitation and hygiene and case management strategies, (4) harmonising epidemic and humanitarian coordination systems and (5) protecting water systems and health facilities during conflict.
What do the new findings imply?
Our case study starkly highlights the importance of disease risk assessment, preparedness planning and coherent early strategies for cholera control in conflict-affected states.
Preparedness and response strategies in crises should prioritise the capacity to direct responses close to cholera-affected communities through existing networks (eg, community health workers and district-level resources) and provide the necessary supplementary resources (eg, rapid response teams) early in the response in order to reduce transmission.
Introduction
Cholera outbreaks remain a marker for the world’s most marginalised communities. In 2017, the Global Task Force on Cholera Control (GTFCC) launched Ending Cholera: A Global Roadmap to 2030.1 It proposes to strengthen health systems, water, sanitation and hygiene (WASH) and coordination strategies for cholera control in low-income and middle-income countries. By 2030, the GTFCC aims to reduce cholera mortality by 90% and eliminate cholera in 20 of the 47 cholera-affected countries. Fragile and conflict-affected states (FCAS) where large and prolonged cholera epidemics have occurred, including Iraq, the Democratic Republic of Congo (DRC) and South Sudan, are critical to achieving these goals.2 Operational constraints on logistics, security and the coordination of humanitarian partners in FCAS reduce access to communities and challenge epidemic control.3 4
Since 2016, Yemen has experienced a large-scale cholera epidemic overlaid on civil war and a humanitarian crisis. In 2015, the United Nation’s (UN) declaration of a level 3 (L3) emergency activated the highest level of resource mobilisation across the humanitarian system. Before cholera emerged, 46% of 3507 health facilities were operational, blockades of sea ports prevented the entry of essential goods and medicines and severe insecurity restricted the movement of civilians, the UN and non-governmental organisations (NGOs).5 6 By 2017, food insecurity had placed 60% of the population at risk of famine.5
More than 1 million suspected cases of cholera were reported from 28 September 2016 to 2 July 2018.7 In this case study, we identified lessons from the cholera response during the first and second waves of the epidemic to better prepare Yemen and other FCAS for cholera response during humanitarian crises.
Methods
This study used an explanatory case study design to analyse decision making and intervention strategies during the first and second waves.8 Literature reviews, key informant interviews (KII) and interpretation of surveillance and airstrike data were employed. The GTFCC’s framework for cholera control was used to guide the analysis (Box 1).1
Box 1. Global Task Force on Cholera Control (GTFCC) framework for cholera control1 .
Early detection and quick response to contain outbreaks at an early stage, including early warning surveillance systems, prepositioning stocks, preparedness of water, sanitation and hygiene (WASH) systems, preparedness of the health care system and improved health care facility infrastructure, establishment of WASH and health rapid response teams, maintenance of stocks of WASH supplies, specific WASH interventions to prevent spread of disease, community engagement, mass vaccination campaigns with oral cholera vaccination (OCV) and effective supply management;
A multisectoral approach to prevent cholera in hotspots in endemic countries, including identification of hotspots requiring priority action, analysis of local transmission patterns and implementation of a package of control measures adapted to local transmission patterns;
An effective mechanism of coordination for technical support, resource mobilisation and partnership at the local and global level.
Literature reviews
A literature review of global cholera and epidemic guidance for FCAS was conducted to describe control strategies adapted for FCAS. This included a PubMed search during February 2018 using the search terms ‘cholera’ (title) AND (‘epidemic’ OR ‘control’, ‘prevention’ or ‘strategy’) AND the names of FCAS derived from the World Bank’s harmonised lists of fragile situations.9 Relevant websites (eg, GTFCC, WHO, UNICEF, Global Clusters and Médecins Sans Frontières (MSF) were also searched using this approach. A second literature review of Yemen-specific documents, including cholera preparedness and response plans, epidemiological reports, evaluations and news articles concluded in November 2018. The terms ‘Yemen’ AND ‘cholera’ were used to search the WHO, UNICEF, Global Clusters, Humanitarian Response, Devex and The New Humanitarian (formerly IRIN) websites, and documents were requested from KII respondents. One author screened the documents for relevance.
Interpretation of surveillance and airstrike data
Epidemic curves and key indicators (eg, attack rate, case fatality ratio (CFR) and proportion of cases under 5 years) from a comprehensive analysis of the first wave (28 September 2016–23 April 2017) and second wave (24 April 2017–2 July 2017) surveillance data were reviewed.7 To investigate the frequency of airstrikes on water systems and health facilities, data on the time and location of airstrikes from April 2015 to December 2017 were compiled from the Yemen Data Project, an independent database of cross-referenced, open-source data on air raids.10
Key informant interviews
KIIs were used to explain how decisions were made, how actions were implemented and personal perspectives. They were conducted with national and international practitioners, advisors, donors and government officials.
Potential respondents were identified through a stakeholder analysis.11 Semistructured interview guides were prepared by thematic area (preparedness and coordination, surveillance and laboratory, case management, nutrition, WASH, oral cholera vaccination (OCV) and insecurity). Potential respondents were contacted by email with study information, and their confidential participation was requested. KIIs were undertaken by a thematic lead by telephone/Skype or in-person and lasted 30–75 min. To improve note-taking accuracy, most KIIs involved two investigators. Detailed interview notes were kept, and some were recorded (with permission). Informed consent was documented.
Within each sector, a thematic analysis was undertaken and triangulated with the literature review and surveillance data.12 Monthly team debrief meetings were undertaken by telephone/Skype or in-person to build a broad interpretation across sectors and to generate new questions. Member checking was conducted by sharing draft reports confidentially with selected respondents, and the final draft was shared with WHO and UNICEF in Yemen, followed by a teleconference. All suggested changes were discussed by the study team and updated, as deemed appropriate.
Patient and public involvement
There was no patient or public involvement in the development or execution of this research study.
Results
The results are summarised by sector. Fifty-eight documents were reviewed and 71 of the 80 potential KIIs were conducted. Respondents were from national and international NGOs, UN agencies and government ministries (Box 2). Most respondents (75%) had worked in Yemen. Selected quotes are provided in Box 3 to emphasise the themes derived from multiple KII interviews.
Box 2. Key informant interviews: organisations (*includes at least one respondent who worked in Yemen).
Action Contre la Faim.*
Canadian Red Cross.*
CARE.*
Centers for Disease Control and Prevention.
Center for Civilians in Conflict.*
WASH cluster.*
Department for International Development.
European Civil Protection and Humanitarian Aid Operations.*
Epicentre.*
General Authority for Rural Water Supply Projects.*
Health cluster.*
Human Rights Watch: Middle East office.
International Committee of the Red Cross.
International Medical Corps.*
International Rescue Committee.*
Médecins Sans Frontières – Holland.*
Médecins Sans Frontières – Spain.*
Nutrition cluster.*
The Office of US Foreign Disaster Assistance.
OXFAM.*
Relief International.*
Save the Children.*
SOUL for Development.*
UNICEF*: Public Health Emergencies Team, WASH Team, Health Team, Nutrition Team, Middle East and North Africa Regional Office and Yemen Country Office.*
United Nations Humanitarian Coordinator.*
United Nations Office for the Coordination of Humanitarian Affairs.
World Bank.
WHO*: Emergency Operations Team, Cholera Team, EOC Operations Team, Emergency Risk Management and Humanitarian Response Team, Eastern Mediterranean Regional Office, Yemen Country Office.*
Box 3. Quotes from respondents.
Surveillance
Quote 1: ‘[We realized that] it’s not just where we are [in Aden], it’s everywhere, and it’s intense everywhere’. (Field epidemiologist, onset of second wave)
Quote 2: ‘We were seeing hundreds of cases a day. Within a week, it was 3,000 cases a day. Nobody could respond at this level’. (Senior manager, onset of second wave)
Preparedness and funding
Quote 3: ‘The small [first] wave should have put in place alerts, and people to answer to the 2nd wave. We need to analyze why the 2nd wave was so big, even with rainy season (it’s a factor), but why was it so massive’. (Epidemiologist, first wave)
Quote 4: ‘The World Bank made an investment for future, for when they can get back in-country. They showed they were willing to take a gamble. You’ll see them in more places with de facto governments to build an operational footprint’. (Senior UN official, second wave)
Water, sanitation and hygiene
Quote 5: ‘The overall struggle we’ve had with the cholera response is that, when the initial reprogramming came in in 2016, it didn’t look like a cholera response. It looked like a WASH IDP [internally displaced persons] response’. (Anonymous, first wave)
Quote 6: ‘It took a year and a half and well into the second phase of the outbreak before the kind of specific cholera interventions that are related to WASH actually kind of started and got rolled out’. (Anonymous, second wave)
Quote 7: ‘I haven’t been allowed by the authorities to be able to access the field where our teams are working … I’ve only had very limited success in seeing beyond the office’. (Anonymous, second wave)
Case management
Quote 8: ‘Some districts were completely ignored. We only addressed 1st level catchment populations and there are villages where we simply do not know what happened. [They are] very hard to reach’. (Health coordinator, second wave)
Quote 9: ‘The response from the big players has been to build up treatment capacity, and neglect community-based efforts. This is of limited value in addressing the outbreak at the source’. (Health coordinator, second wave)
Oral cholera vaccination
Quote 10: ‘South Sudan, Somalia and Yemen [are similar cases]. Each country has cholera preparedness plan. We should have revised [it] and included OCV. We only wake up when there is a cholera outbreak… we always try to introduce it once the outbreak starts’. (Anonymous, second wave)
Coordination
Quote 11: ‘In Yemen, we can’t simply turn the ship around. A child dies of malnutrition and [another] child dies of cholera. But they are both dying. What’s an appropriate way to get the funds we need and make it available [for both malnutrition and cholera control]?’ (Donor, second wave)
Surveillance
The first wave disseminated cholera in the south before an explosive surge in the second wave across the south, centre and north.7 Lasting 7 months, the first wave peaked at 2000 suspected cases weekly in December 2016 and 1663 deaths in total.10 The second wave included a rapidly increasing trend and expanding geography over 2 months, and a gradually decreasing trend over 8 months, with a massive peak of 50 832 weekly suspected cases in June 2017 and 2265 deaths in total (box 3, quotes 1–2).7 The increasing phase occurred at the onset of the rainy season and was potentially associated with a shift from household use of deep well water to contaminated surface water.7 This phase typifies the characteristics of cholera transmission including a sharp ascent, synchronous bursts across Western Yemen, a large peak, high cumulative attack rates comparable with standards (0.1%–2% in large-scale outbreaks), a small proportion of children under 5 years (18.3%), a large proportion of severe cases (30.6%) and a high CFR (>1% at the start, decreasing to <1% with treatment scale-up).13 In contrast, the first wave and the decreasing phase of the second wave demonstrate long tails, a large proportion of children under 5 years (≥30%) and a low proportion of severe cases.7 This suggests the over-reporting of endemic diarrhoea of other origin and the underestimation of the CFR.
Over-reporting appeared substantial, even considering the high sensitivity of the globally accepted suspected cholera case definition.14 There were several driving factors. The disruption in health systems meant that non-cholera patients routinely presented to diarrhoea treatment centres (DTCs) for care. Persisting into the second wave, standard methods for case ascertainment and reporting were not well reinforced in some DTCs.15 Health workers were also unpaid since 2016, giving rise to rumours that reduced reporting would lead to the cessation of DTCs and their incentive payments.16
Additionally, the national surveillance system for the early warning of outbreaks had existed since 2013 but was not optimised for the management of a large epidemic. The electronic Disease Early Warning System (eDEWS) included a 400-site sentinel network that used mobile phones to report on 31 conditions.17 18 To respond to cholera in the first wave, eDEWS rapidly expanded to 1982 sites nationally.18 However, the structure could not support data management needs of the rising cholera caseload. Line-lists from DTCs were instead emailed daily to the Ministry of Public Health and Population (MoPHP), incurring delays in processing and sharing with partners. During the second wave peak, as thousands of cases were reported daily, another system (EWARS-in-a-Box) was scaled to improve data management and reporting. It could not however quickly address the mass training and supervision required to improve poor adherence to the suspected case definition. Laboratory culture relied on only two central laboratories in Sana’a and Hodeidah, and this low capacity could not reliably monitor geographical shifts in cholera. Protocols for rapid diagnostic testing (RDT) of every 10th suspected case in DTCs were set, but RDTs were not widely available.19
Epidemiological investigations of hotspots, transmission and high-risk groups were not routinely undertaken, and there was no community surveillance to detect cases and deaths outside of DTCs. With limitations in data quality and availability, detailed interpretation of surveillance and laboratory data was absent from cholera response plans.
Preparedness and funding
Yemen’s health services were primarily organised through the UN’s Humanitarian Response Plan. Two small cholera outbreaks and a large outbreak of 30 000 suspected cases were reported between 2009 and 2011.20 The WHO’s Regional Office established a regional framework for cholera control in 2014.21 By 2015, Yemen’s water and sanitation infrastructure was degraded, and 50% of the population required WASH assistance.22 Despite these risk factors, Yemen did not have a cholera preparedness and response plan in place prior to the 2016 outbreak.
On detection of cholera in Sana’a in September 2016, the health and WASH clusters and the MoPHP rapidly developed the first wave’s cholera preparedness and response plan that same week. The plan emphasised preventative WASH approaches and case management in governorates where cholera had been confirmed or was likely to emerge, instead of geographically targeted approaches to interrupt transmission.23 It did not include key standard components, including analysis of hotspots, scenarios for OCV use, community surveillance, infection prevention and control and improvement of laboratory capacity. The lack of detailed planning meant that the initial response prioritised logistical issues such as the procurement of rehydration supplies and reinforcement of existing WASH strategies over a multisector and cholera-specific strategy. A response-wide after-action review of the first wave was not conducted despite the risk of resurgence (box 3, quote 3). Following the emergence of a second wave, the response plans were updated to include targeted approaches in 286 (of 331) districts and prevention in 47 districts.19 However, the plan was issued late after the second wave peak.
WHO and the Health Pooled Fund provided major funding during the first wave. Following an appeal during the second wave where only 47 million of 250 million requested was received, there was an initial shortfall, which required the diversion of food security and malnutrition funding to address cholera.24 The World Bank began to disburse funding (of 483 million total) early in the second wave through a recommitment of International Development Association grants that were previously cancelled due to the crisis. This allowed for the preservation of primary health and nutrition services, with sufficient flexibility to use funds for cholera control (box 3, quote 4). Respondents did not cite funding across the entire cholera response as a major challenge. This compares with annual appeals that are historically underfunded; for example, in 2016, only 47% of the Humanitarian Response Plan was funded.25 26
Water, sanitation and hygiene
Yemen is extremely water scarce, placing nearly the entire population vulnerable to the economic and physical impacts of water scarcity and health impacts of water-washed and water-borne diseases. When the first wave occurred, NGOs maintained non-specific WASH activities to improve water supply, sanitation, hygiene and solid waste management with few cholera-specific WASH activities (eg, disinfection of water and surfaces in patient homes and DTCs). However, these programmes remained community based and small scale, relative to the expanding epidemic. The 2016 cholera preparedness and response plan reinforced these blanket activities over interventions targeting cholera-affected households and communities (box 3, quote 5).
This approach continued during the second wave wherein the WASH cluster found that most beneficiaries were reached through support to urban areas including the rehabilitation of water infrastructure and maintenance of sewage treatment plants.27 Insecurity impacted the capacity of NGOs to carry out targeted programming. By the second wave, UNICEF, as the provider of last resort and the WASH cluster lead, took a major role in implementation. Due to the humanitarian roster system, it was not until the second wave peak that UNICEF and WHO were able to send cholera specialists to develop a cholera-specific WASH strategy. This new strategy focused on chlorination at all points in the water chain to reduce transmission in hotspots and scale-up of rapid response teams (RRTs) at the district level to target cholera-affected households and attempt to prevent intrahousehold and community transmission. Implemented through government staff, the RRT strategy achieved community access and scale but was implemented too late after the second wave peak to address containment (box 3, quote 6).
Insecurity restricted hygiene promotion activities (box 3, quote 7). UNICEF and WHO carried out a national household awareness campaign with 40 000 volunteers disseminating cholera awareness messages across 14 million households in all governorates during the second wave peak. While lauded by respondents, they expressed the need for earlier implementation during the increasing phase of the second wave.
Monitoring of the WASH strategy using free residual chlorine (FRC) as the primary outcome indicator was recommended by the WASH cluster. While 16 of the 25 WASH cluster partners reported routinely implementing postdistribution monitoring and FRC testing, FRC data were not easily accessible to inform programming.27
Case management
The treatment network of DTCs and oral rehydration corners (ORCs) was insufficiently decentralised throughout the epidemic to ensure adequate access for a large proportion of the population living in hard-to-reach, mountainous and insecure areas. The 2016 cholera preparedness and response plan focused on establishing DTCs in or near existing health facilities and schools instead of placement driven by epidemiological need in less accessible areas (box 3, quote 8).23 Decision making was driven by the humanitarian need to integrate all health services in a single complex due to the lack of clinicians and functioning health facilities, rather than the isolation of cholera patients to prevent secondary transmission. Health facilities and schools were not ideal as DTCs as they displaced services and disrupted infection control. It is unclear how non-cholera patients who presented to DTCs were accommodated, given the lack of practical referral options. NGO partners interviewed had few or no health staff directly supervising ORC/DTCs, so monitoring the quality of case management could not be done systematically.
Particularly in rural contexts with poor access to care, ORCs should be the first point of care for patients to provide prompt access to care for the 80% who require only rehydration.13 However, ORCs were only established during the second wave. Their placement did not address the epidemiological picture and volume for widespread access in communities. Neither Yemen’s networks of community health workers nor Red Crescent volunteers were mobilised to staff ORCs in remote areas. Only 32.4% of suspect cholera cases in Yemen visited a DTC on the same day of symptom onset, while for 10.2% of patients it took two or more days to access care.7 This meant that patients were not able to routinely access an ORC within 1 hour of walking, which is a GTFCC standard.28 The health response was cited as ‘unable to address the outbreak at the source (the community)’ (box 3, quote 9).
In large epidemics, high-risk groups including pregnant women and children with severe acute malnutrition (SAM) require case management protocols.29 Protocols were either lacking or insufficiently practical, reflecting the lack of clarity from global bodies. Protocols for SAM were not published until after the start of the second wave, and none were available for pregnant women.
Oral cholera vaccination
The use of OCV was slowed by the lack of a cholera preparedness and response plan and hence less familiarity with OCV among the MoPHP and partners. This scenario is similar to other conflict-affected countries that lack experience in implementing OCV.30 The first wave response lacked a robust discussion about carrying out an epidemiological risk assessment for OCV, despite being raised by advisors (box 3, quote 10). This is notable given recent evidence demonstrating the added value of using OCV in crises where WASH improvements are slow to achieve.31
WHO drove efforts to strategically use vaccination to interrupt spread early during the second wave. The risk assessment was challenging due to the lack of accurate data to guide vaccination strategies. Following this first risk assessment, the MoPHP requested nearly all of the 3.4 million doses from the global stockpile and the International Coordinating Group (ICG). Some partners and decision makers considered the plan too ambitious given Yemen’s lack of OCV implementation experience and its reduced operational capacity. Eventually, the ICG approved the request, beginning with an initial tranche of 500 000 doses, though the MoPHP then cancelled this request.32 Potential reasons for this stasis included political concerns about covering an adequate proportion of the population in government and opposition-controlled areas, the lack of rigorous data for targeting high-risk communities, the poor operational context and a lack of participation of partners in risk assessment.
Following a second risk assessment in January 2018, the focus shifted toward boosting prevention efforts for an anticipated surge of cholera during the rainy season (April–August 2018). Based on the risk assessment, the March 2018 cholera preparedness and response plan included a vaccination strategy, and the MoPHP made a successful request for 4.6 million doses for preventative use.19 Yemen’s campaign took advantage of innovations for delivering OCV in crises including using the far-reaching poliomyelitis infrastructure to deliver the vaccine across age groups and a single-dose strategy to enable short-term protection.31
Some respondents considered that preparedness for the 2018 rainy season should have been the focus across all sectors and agencies, with OCV playing a major role within that discussion. Instead, discussions on OCV were prolonged, and key elements including prepositioning of supplies may have been delayed or insufficiently considered.
Coordination
Yemen’s need for strong coordination remained paramount given the complexity of the cluster system managing both the humanitarian crisis and cholera epidemic and simultaneously addressing two warring government factions (box 3, quote 11). Three coordination systems operated with various success and limited complementarity. This included the: (1) health and WASH clusters, (2) cholera task force and (3) incident management system (IMS) and its emergency operations centres (EOCs). The cluster approach showed agility in developing the initial response by its leveraging of relationships with governments and through its understanding of the operational environment and the geographical distribution of partners. However, the dual workload of developing the response plan and managing the crisis was excessive. Experienced cholera specialists could not arrive until the height of the second wave due to the heavily restrictive humanitarian roster. Thus, technical advice for the cholera response was mainly delivered remotely.
WHO Yemen and the MoPHP implemented the IMS at the start of the second wave. This reflects WHO’s recent efforts to integrate the government and other partners into a unified command structure, outside of WHO’s internal structure.33 IMS aimed to ‘adopt a more operational posture by reducing the number of meetings and increasing the face-to-face working of the relevant stakeholders’ as compared with the ‘information sharing forum’ of the cluster system. However, this mandate was not clear to many respondents.
While 22 EOCs affiliated with one health RRT per district was planned, only eight EOCs were operational by April 2018.34 Drivers included insecurity and the lack of understanding across agencies, technical assistance for field implementation outside the capitals and standard guidance on IMS integration with the cluster system. Notwithstanding, the national EOCs in Sana’a and Aden achieved unified information management and response expertise in a single structure. Another positive consequence of the EOCs was for directing health RRTs, similar to those used in Haiti.35 Implemented during the second wave, health RRTs decentralised functions to the community level, including investigation, early response and quality control. In parallel, WASH RRTs investigated and provided household-based response within the first 48 hours of detection when clusters of 5–20 suspected cases were detected.
Insecurity
The progressive degradation and destruction of civilian infrastructure required the humanitarian system to rethink how best to address the epidemic in a protracted and unpredictable conflict. Major stressors included the closure of ports and airports, blockades of imported food, fuel, medications and medical supplies, and artillery fire and restriction of movement, which threatened the local delivery of aid.36
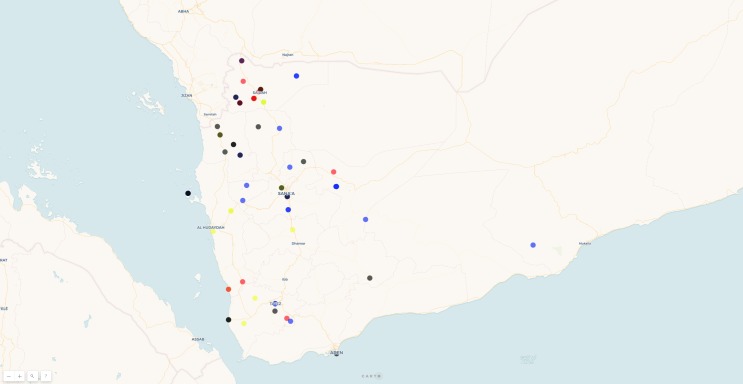
Saudi-led coalition airstrikes damaged civilian infrastructure including water desalination systems. This disrupted services, reduced water access to whole areas and potentially increased cholera transmission. The UN Office for the Coordination of Humanitarian Affairs (OCHA) provided a communication role with the Saudi-led coalition to avoid inadvertent strikes on the UN and its partners. Despite this, an airstrike hit a MSF-run DTC in Abs in June 2018.37 Between April 2015 and December 2017, 74 instances of airstrikes on water-related infrastructure including desalination systems and bottling plants in Taiz, Hodaydah, Hayz and Al Mukha and 70 instances of targeting of health facilities were documented (figure 1).10 The purposeful destruction of civilian water infrastructure is a violation of international agreements including the Geneva Conventions. These airstrikes continued throughout the epidemic, despite repeated calls from UNICEF, MSF and others for the protection of these sites.37 38 Infrastructure damage is difficult and costly to repair under a humanitarian mandate.
Figure 1.
Locations of airstrikes targeting water infrastructure, April 2015–December 2017.14 Legend: 2015 (black), 2016 (blue), 2017 (yellow) and 2018 (red).
Some of this damage may have been inadvertent and associated with military activity near these sites. However, the pattern of repeated strikes on infrastructure suggests purposeful targeting. The destruction of infrastructure is generally permitted if such facilities are deemed of military necessity. Nevertheless, such attacks would need to meet accepted criteria of proportionality, a principle that demands that combatants do not inflict damage to non-combatants in excess of the military advantage associated with an attack.39 Yet, this principle has been criticised as vague and inherently unable to protect infrastructure that is of dual use. Proportionality considerations for dual use sites did not provide much protection in Yemen. The Saudi-led coalition’s Joint Incidents Assessment Team conducted poststrike investigations, though these did not address what actions to take to improve civilian protection.40
Discussion
The response to large epidemics and the coordination of health services during crises are some of the most complex processes in public health.3 41 Given cholera epidemics in the region, water insecurity and the conflict-driven degradation of health and WASH systems, the emergence of cholera in Yemen was likely unavoidable. Our analysis suggests that the poor operating environment and the late adoption of cholera-specific control measures, however, restricted the scope for prevention of the larger epidemic. Persistent gaps included bottlenecks in surveillance and coordination and the lack of a geographically decentralised response. Key advances occurred late in the second wave, including the switch to a cholera-specific WASH strategy, expansion of the operational footprint using RRTs and adoption of preventative vaccination. Adequate funding from the World Bank underpinned the response in an environment where appeals for the larger crisis are historically underfunded.25 26 These advances, and the reduction in the population susceptible to infection, coincided with the epidemic receding.
Our findings are subject to limitations. The study presents self-reports from respondents who may have emphasised the effectiveness of their own organisations’ activities to provide a socially desirable response. Nevertheless, there was considerable variation on numerous issues among respondents within and among different organisations. Due to the restricted humanitarian roster to enter Yemen, despite repeated attempts we were unable to visit to observe the operations in person. Our study focuses on the broad strategies employed by the response but not the strategies of individual NGOs that may differ. We interviewed a limited number of national actors, despite several attempts to speak with the MoPHP and national NGOs. To address these limitations, we conducted a high number of interviews to build up a critical understanding, we used qualitative and quantitative data to triangulate the findings and we conducted several rounds of validation with respondents from different organisations. From this analysis, we propose five lessons learnt about epidemic control in Yemen and other FCAS (table 1).
Table 1.
Challenges during the cholera epidemic in Yemen, their impacts, and opportunities for FCAS
| Sector and challenge | Impacts in Yemen | Opportunities for FCAS |
| 1. Cholera preparedness and planning was lacking. |
|
|
| 2. Epidemic detection and monitoring could not be scaled. |
|
|
| 3. WASH and health cholera-specific strategies did not have a decentralised, community-based and intersectoral response. |
|
|
| 4. Coordination systems operated with limited success and complementarity. |
|
|
| 5. Protection of health facilities and WASH infrastructure during conflict. |
|
A specific UN agency (likely UNICEF) should be chosen and provide surveillance of these attacks and stronger advocacy to prevent direct harm (eg, killings) and indirect harm (eg, damage to WASH infrastructure) to civilians. |
FCAS, fragile and conflict-affected states; IMS, incident management system; MoPHP, Ministry of Public Health and Population; OCV, oral cholera vaccination; ORCs, oral rehydration corners; RRT, rapid response team; WASH, water, sanitation and hygiene; eDEWS, electronic Disease Early Warning System.
Armed conflict increases the likelihood of the emergence of epidemics.4 During the crisis in 2015 and 2016, the degradation of water and sanitation infrastructure had given rise to the proliferation of mosquitos and hence cycles of large-scale malaria and dengue outbreaks.26 42 Degraded WASH infrastructure has been cited as driving the cholera epidemic in Yemen in the dry and rainy seasons due to the reliance on unsafe water and contamination of available water, respectively.7 43 While Yemen had not experienced a cholera outbreak since 2011, a genetic lineage with the 2015–2016 outbreaks in East Africa demonstrates the persistent risk of regional dissemination.44 Yemen’s 2016 Humanitarian Response Plan, the main planning instrument for system-wide response, did not mention cholera; this suggests that cholera was not considered a key risk despite large epidemics in Somalia and Iraq in 2015.22 45 FCAS at risk of cholera should prioritise multisector preparedness planning, such as the plans used in Iraq in 2002 to anticipate the Gulf War, annual plans in South Sudan and Unicef’s Regional Cholera Platform in Africa.46 47 The process can uncover gaps and promote a cohesive understanding of the response strategy among partners. OCV provides an example where the absence of planning and delays in consensus were not unique to Yemen and have affected other FCAS that did not integrate OCV into their cholera plans (eg, Haiti, Somalia and South Sudan).30 Plans should focus on the human resource, logistical and financial limitations posed by the conflict. They should include an epidemiological risk assessment, a focus on operational gaps, defined roles for ministries and partners and the integration of epidemiological scenarios for the pre-emptive use of OCV for high-risk areas while outbreaks are relatively small. This finding concurs with that of a South Sudanese study that demonstrated that proactive planning for the preventative use of OCV during the humanitarian crisis was necessary for the procurement of vaccine and implementation before the declaration of the outbreak in South Sudan in 2014.30 48 Similarly, cholera specialists called for early steps to obtain the vaccine in Yemen, justified by the risk of uncontrolled transmission.49
In FCAS, the decentralisation of epidemic response to inaccessible areas should be anticipated. By 2016, most of Yemen’s population was in need of humanitarian aid (80%), WASH (77%) and health services (57%), and large parts of the country were insecure or difficult to access.22 Therefore, an early priority should have included decentralising the treatment network (by placing ORCs and smaller treatment units in communities to increase access to care and to reduce mortality) and WASH (through rapid response to interrupt transmission before an outbreak enlarges). Decentralisation of interventions to insecure areas remains extremely challenging, both practically and ethically, and requires partnership models that balance community linkages of national NGOs with a level of risk transfer that is acceptable to them, community health workers and Red Cross Societies.50 51 This should be accompanied by a commitment to risk assessment and capacity building for responders through remote monitoring and training.
Yemen’s response to the large-scale cholera epidemic in a widespread active conflict and extremely food and water insecure environment challenges the tools of global health security. The Inter-Agency Standing Committee procedures to designate a large-scale epidemic as an L3 emergency could have triggered an intersectoral coordination structure for the whole humanitarian system.52 WHO had implemented its Emergency Response Framework but made its IMS a cross-agency endeavour to provide a more direct approach for epidemic response in the middle of the second wave on top of the cluster system’s more collaborative approach.33 The placement of the IMS outside of WHO’s internal ERF structure was confusing to non-WHO agencies and the lack of efforts to harmonise the coordination systems hampered trust among agencies and affected the response. As large epidemics in humanitarian crises will continue, as is occurring now with the ongoing Ebola outbreak in the DRC, WHO should focus on developing operating procedures for the implementation of IMS and the clusters in an open process that includes Unicef, OCHA, other UN and humanitarian agencies and the cluster system. Finally, given the existing requirement to report attacks against heath workers and health facilities to the UN General Assembly by WHO, a similar mechanism should be implemented for attacks on public infrastructure including water systems.53 A specific UN agency, we would suggest UNICEF, given their recent focus on threats to water and sanitation in crises, should advocate strongly against such attacks on public infrastructure by warring parties, justified in part by a public health and protection mandate to prevent epidemics.54
Yemen’s experience highlights four neglected areas of research. First, protocols are needed for improving the specificity of RDTs under field conditions and their systematic use for monitoring epidemics where laboratory capacity is low.55 Second, evidence for the optimal timing and effectiveness of the RRT model, for the effectiveness of the individual health and WASH interventions in the rapid reduction of secondary transmission and the composition of an integrated package of health and WASH interventions are needed.35 56–58 Third, protocols for case management among pregnant women and severely malnourished children are urgent priorities to avoid excess mortality.29 Fourth, guidance for the decentralisation of the response with remote monitoring of epidemics in FCAS according to different contexts are lacking.
Conclusion
The challenges in delivering health services in Yemen, Syria, South Sudan and other L3 emergencies are staggering. Our study raises a broader concern over the chaos that this massive epidemic placed on a humanitarian system actively managing extreme food insecurity, displacement, drought and civil war. At the time of writing (April 2019), MSF has reported a surge in suspected cholera cases from January to March 2019 in Western Yemen resulting in nearly 109 000 suspected cases (2000 suspected cases weekly), including 190 deaths.59 However, there is room for some limited optimism in Yemen and future situations where protracted conflict gravely impacts civilians. WHO, UNICEF and its partners have reported intensive work to optimise the latest response based on review of response efforts and impacts.60 The World Bank’s funding of the response has also opened a new door to disease control in FCAS.
Nevertheless, it is clear in a world where conflicts are prolonged and disagreements among permanent members of the UN Security Council do not allow for their resolution, large-scale epidemics will likely become more common and more severe. We urge governments, the UN and the humanitarian system to learn from these and other efforts in order to be better prepared to rapidly control future epidemics in conflict-affected countries.
Acknowledgments
We wish to thank all of the respondents who shared with us their critical insights into the challenges they faced during the cholera response in Yemen. We would like to thank Annie Shiel of Stanford University for producing the map of airstrikes and David Sack of Johns Hopkins Bloomberg School of Public Health for technical advice.
Footnotes
Handling editor: Seye Abimbola
Contributors: PS, RR and DL designed the study and took the lead in the interpretation of the results and the drafting of the manuscript. NH, MN, MV and PHW provided substantial contributions to the data collection and interpretation and the drafting the manuscript. All authors made significant content contributions to the final draft of the report and critically reviewed and approved the final version.
Funding: The Office of U.S. Foreign Disaster Assistance (OFDA) provided funding to the Johns Hopkins Center for Humanitarian Health for an unsolicited proposal for a case study of the response (supported non-financially by the Department for International Development (DFID) and the Directorate-General for European Civil Protection and Humanitarian Aid Operations (ECHO). All authors had full access to all the data in the study and had the final responsibility for the decision to submit for publication.
Disclaimer: The funder had no role in study design, data analysis, data interpretation or writing of the report.
Competing interests: RR and DL declare personal fees from the Johns Hopkins Bloomberg School of Public Health for conducting the study.
Patient consent for publication: Not required.
Ethics approval: The study protocol was determined by Johns Hopkins Bloomberg School of Public Health not to be human subjects research and was exempted from review.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1. Global Task Force on Cholera Control Ending cholera. A global roadmap to 2030. Geneva, Switzerland: WHO, 2017. [Google Scholar]
- 2. WHO Cholera, 2017. Wkly Epidemiol Rec 2018;38:489–500. [Google Scholar]
- 3. Spiegel PB, Checchi F, Colombo S, et al. . Health-care needs of people affected by conflict: future trends and changing frameworks. Lancet 2010;375:341–5. 10.1016/S0140-6736(09)61873-0 [DOI] [PubMed] [Google Scholar]
- 4. Gayer M, Legros D, Formenty P, et al. . Conflict and emerging infectious diseases. Emerg Infect Dis 2007;13:1625–31. 10.3201/eid1311.061093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. UNOCHA Revised Yemen Humanitarian response plan; 2017. https://reliefweb.int/sites/reliefweb.int/files/resources/YHRP_2016_Revision_FINAL_30%20August%202016.pdf
- 6. WHO EMRO Health services decline as conflict in Yemen continues Sana. Yemen: WHO EMRO, 2017. [Google Scholar]
- 7. Camacho A, Bouhenia M, Alyusfi R, et al. . Cholera epidemic in Yemen, 2016-18: an analysis of surveillance data. Lancet Glob Health 2018;6:e680–90. 10.1016/S2214-109X(18)30230-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yin RK. Case study research: design and methods. SAGE, 1984. [Google Scholar]
- 9. World Bank Harmonized list of fragile situations FY 18, 2018. Available: http://pubdocs.worldbank.org/en/189701503418416651/FY18FCSLIST-Final-July-2017.pdf
- 10. Yemen Data Project Yemen data project, 2018. Available: http://yemendataproject.org/ [Accessed 20 Aug 2018].
- 11. Varvasovszky Z, Brugha R. A stakeholder analysis. Health Policy Plan 2000;15:338–45. 10.1093/heapol/15.3.338 [DOI] [PubMed] [Google Scholar]
- 12. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007;42:1758–72. 10.1111/j.1475-6773.2006.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Médecins Sans Frontières Cholera Guidelines. 2nd ed Paris, France: MSF, 2004. [Google Scholar]
- 14. Global Task Force on Cholera Control (Surveillance Working Group) Interim guidance document on cholera surveillance. Geneva, Switzerland: WHO, 2017. [Google Scholar]
- 15. WHO Yemen cholera response: field visits to Ibb and Hudaydah summary of immediate action points and recommendations Sana. Yemen: WHO, 2017. [Google Scholar]
- 16. Dickinson E. Banking conflict exacerbates Yemen's cholera and famine. Devex, 2017. [Google Scholar]
- 17. Ahmed K, Dauod Altaf M, Dureab F. Electronic infectious disease surveillance system during humanitarian crises in Yemen. Online J Public Health Inform 2014;6:e134 10.5210/ojphi.v6i1.5083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. WHO Electronic integrated disease early warning system launched in Yemen Sana. Yemen: WHO, 2017. [Google Scholar]
- 19. Ministry of Public Health and Population Integrated cholera prevention and control strategic plan, Yemen. Sana, Yemen: WHO, 2018. [Google Scholar]
- 20. WHO EMRO Weekly epidemiological monitor. Cairo, Egypt: WHO, 2011. [Google Scholar]
- 21. WHO EMRO Consultative meeting on developing a strategic framework for cholera prevention and control in the Eastern Mediterranean region, 2014. [Google Scholar]
- 22. UN OCHA Revised Yemen Humanitarian Response Plan, 2016. Yemen New York, USA, 2016. [Google Scholar]
- 23. Ministry of Public Health and Population, Health Cluster, WASH Cluster Integrated response plan: Yemen cholera and acute watery diarrhoea outbreak. Yemen: Sana, 2016. [Google Scholar]
- 24. Anon Health catastrophe: the toll of cholera in Yemen. Lancet Gastroenterol Hepatol 2017;2 10.1016/S2468-1253(17)30224-8 [DOI] [PubMed] [Google Scholar]
- 25. Ahmadzai TK, Maburutse Z, Miller L, et al. . Protecting public health in Yemen. Lancet 2016;388 10.1016/S0140-6736(16)32422-9 [DOI] [PubMed] [Google Scholar]
- 26. Anon Health system in Yemen close to collapse. Bull World Health Organ 2015;93:670–1. 10.2471/BLT.15.021015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yemen WASH Cluster WASH Humanitarian Response Plan Quarter 4: January - December 2017. Sana'a, Yemen: Yemen WASH Cluster, 2018. [Google Scholar]
- 28. Global Task Force on Cholera Control Technical note, organization of case management during a cholera outbreak, 2017. [Google Scholar]
- 29. Ververs M, Narra R. Treating cholera in severely malnourished children in the Horn of Africa and Yemen. Lancet 2017;390:1945–6. 10.1016/S0140-6736(17)32601-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Abubakar A, Azman AS, Rumunu J, et al. . The first use of the global oral cholera vaccine emergency stockpile: lessons from South Sudan. PLoS Med 2015;12:e1001901 10.1371/journal.pmed.1001901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. WHO Cholera vaccines: WHO position paper - August 2017. Wkly Epidemiol Rec 2017;25:477–98. [PubMed] [Google Scholar]
- 32.Slemrod, A., Almosawa, S. What’s really stopping a cholera vaccination campaign in Yemen? The New Humanitarian (formerly IRIN News) 2017
- 33. Brennan R, Holden R, Cox P, et al. . Adapting the incident management system for response to health emergencies – early experience of WHO. Wkly Epidemiol Rec 2018;20:279–83. [Google Scholar]
- 34. WHO Emergency operations center situation report, Issue No. 30; diphtheria and cholera response. Sana, Yemen: WHO, 2018. [Google Scholar]
- 35. Rebaudet S, Bulit G, Gaudart J, et al. . The case-area targeted rapid response strategy to control cholera in Haiti: a four-year implementation study. PLoS Negl Trop Dis 2019;13:e0007263 10.1371/journal.pntd.0007263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. ACAPS Crisis analysis of Yemen Geneva, Switzerland, 2018. Available: https://www.acaps.org/country/yemen/crisis-analysis [Accessed 8 August 2018].
- 37. Médecins Sans Frontières Yemen: airstrike hits MSF cholera treatment center in Abs, 2018. Available: https://www.doctorswithoutborders.org/what-we-do/news-stories/story/yemen-airstrike-hits-msf-cholera-treatment-center-abs [Accessed 20 Aug 2018].
- 38. UNICEF Access to water continues to be jeopardized for millions of children in war-torn Yemen Sana, Yemen: UNICEF, 2018. Available: https://www.unicef.org/press-releases/access-water-continues-be-jeopardized-millions-children-war-torn-yemen [Accessed 24 July 2018].
- 39. Dill J. The definition of a legitimate target of attack: not more than a moral plea? Proc. annu. meet.- Am. Soc. Int. Law 2009;103:229–32. 10.1017/S0272503700034169 [DOI] [Google Scholar]
- 40. Watch HR, Report W. Country summary: Yemen. New York, NY, USA: Human Rights Watch, 2018. [Google Scholar]
- 41. Agua-Agum J, Allegranzi B, Ariyarajah A, et al. . After Ebola in West Africa--Unpredictable Risks, Preventable Epidemics. N Engl J Med 2016;375:587–96. 10.1056/NEJMsr1513109 [DOI] [PubMed] [Google Scholar]
- 42. Burki T. Yemen's neglected health and humanitarian crisis. Lancet 2016;387:734–5. 10.1016/S0140-6736(16)00389-5 [DOI] [PubMed] [Google Scholar]
- 43. Dureab F, Shibib K, Ye Y, et al. . Cholera epidemic in Yemen. Lancet Glob Health 2018;6:e1283 10.1016/S2214-109X(18)30393-0 [DOI] [PubMed] [Google Scholar]
- 44. Weill F-X, Domman D, Njamkepo E, et al. . Genomic insights into the 2016-2017 cholera epidemic in Yemen. Nature 2019;565:230–3. 10.1038/s41586-018-0818-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cholera Cholera, 2015. Wkly Epidemiol Rec 2016;91:433–40. [PubMed] [Google Scholar]
- 46. Valenciano M, Coulombier D, Lopes Cardozo B, et al. . Challenges for communicable disease surveillance and control in southern Iraq, April-June 2003. JAMA 2003;290:654–8. 10.1001/jama.290.5.654 [DOI] [PubMed] [Google Scholar]
- 47. Ministry of Health of the Republic of South Sudan, WHO South Sudan: cholera prevention and response plan. Juba, South Sudan: Ministry of Health of the Republic of South Sudan, 2017. [Google Scholar]
- 48. Azman AS, Rumunu J, Abubakar A, et al. . Population-level effect of cholera vaccine on displaced populations, South Sudan, 2014. Emerg Infect Dis 2016;22:1067–70. 10.3201/eid2206.151592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Qadri F, Islam T, Clemens JD. Cholera in Yemen - An Old Foe Rearing Its Ugly Head. N Engl J Med 2017;377:2005–7. 10.1056/NEJMp1712099 [DOI] [PubMed] [Google Scholar]
- 50. Global Health Cluster Programming in access-constrained environments: practical guidance. Geneva, Switzerland: WHO, 2018. [Google Scholar]
- 51. Chaudhri S, Cordes K, Miller N, et al. . Humanitarian health programming and monitoring in inaccessible conflict settings: a literature review. Int J Humanitarian Action 2019;4 10.1186/s41018-019-0055-x [DOI] [Google Scholar]
- 52. Inter-Agency Standing Committee Humanitarian system-wide scale-up activation protocol for the control of infectious disease events. Geneva, Switzerland: IASC; 2019. [Google Scholar]
- 53. United Nations General Assembly Global health and foreign policy A/69/L35. Sixty-ninth session ED, 2014. [Google Scholar]
- 54. UNICEF Water under fire New York, NY, USA, 2019. Available: https://www.unicef.org/media/51286/file [Accessed March 2019].
- 55. Debes AK, Ateudjieu J, Guenou E, et al. . Clinical and environmental surveillance for Vibrio cholerae in resource constrained areas: application during a 1-year surveillance in the far North region of Cameroon. Am J Trop Med Hyg 2016;94:537–43. 10.4269/ajtmh.15-0496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Finger F, Bertuzzo E, Luquero FJ, et al. . The potential impact of case-area targeted interventions in response to cholera outbreaks: A modeling study. PLoS Med 2018;15:e1002509 10.1371/journal.pmed.1002509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lantagne D, Yates T, Treatment HW. Household water treatment and cholera control. J Infect Dis 2018;218(suppl_3):S147–S153. 10.1093/infdis/jiy488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yates T, Vujcic JA, Joseph ML, et al. . Water, sanitation, and hygiene interventions in outbreak response: a synthesis of evidence. Waterlines 2018;37:5–30. 10.3362/1756-3488.17-00015 [DOI] [Google Scholar]
- 59. Médecins Sans Frontières Yemen: cholera cases on the rise again, 2019. Available: https://www.doctorswithoutborders.org/what-we-do/news-stories/news/yemen-cholera-cases-rise-again [Accessed June 26, 2019].
- 60. Al-Mandhari A, Musani A, Abubakar A, et al. . Cholera in Yemen: concerns remain over recent spike but control efforts show promise (editorial). East Mediterr Health J 2018;24:971–2. 10.26719/2018.24.10.971 [DOI] [PubMed] [Google Scholar]