Abstract
Background
Contact with child protective services (CPS) functions as an independent marker of child vulnerability. Alaska children are an important population for understanding patterns of CPS contact given high rates of contact overall and among specific demographic groups.
Objective
We aimed to identify longitudinal trajectory classes of CPS contact among Alaska Native/American Indian (AN/AI) and non-Native children and examine preconception and prenatal risk factors associated with identified classes.
Participants and setting
We used data from the Alaska Longitudinal Child Abuse and Neglect Linkage (ALCANLink) project, a linkage of 2009–2011 Alaska Pregnancy Risk Assessment Monitoring System (PRAMS) births with administrative data including CPS records.
Methods
We conducted growth mixture modeling to identify trajectory classes of CPS contact from birth to age five years. We used Vermunt’s three-step approach to examine associations with preconception and prenatal risk factors.
Results
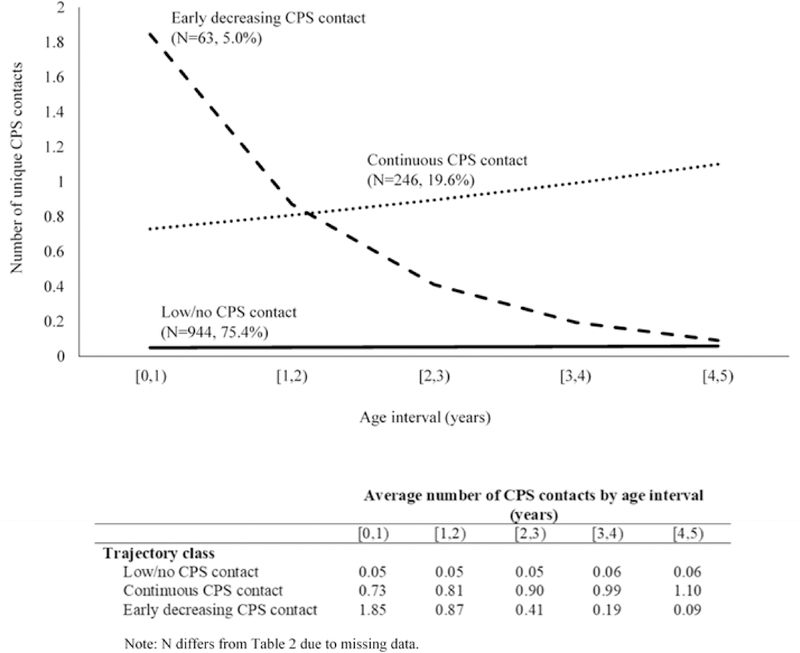
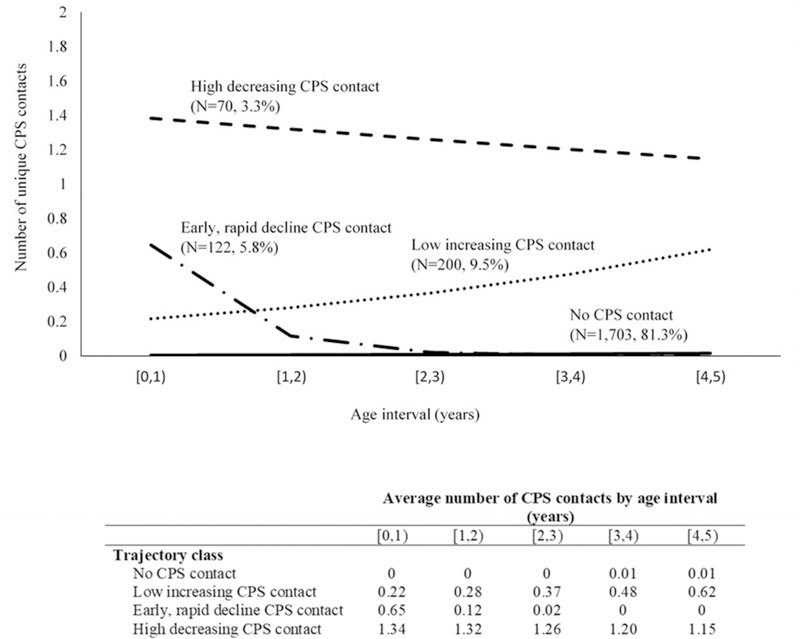
Among AN/AI children, we identified three classes: 1) no/low CPS contact (75.4%); 2) continuous CPS contact (19.6%), and 3) early, decreasing CPS contact (5.0%). Among non-Native children, we identified four classes: 1) no CPS contact (81.3%); 2) low, increasing CPS contact (9.5%); 3) early, rapid decline CPS contact (5.8%); and 4) high, decreasing CPS contact (3.3%). Maternal substance use had the largest impact on probabilities of class membership, increasing the probability of membership in classes characterized by CPS contact, among both AN/AI and non-Native children.
Conclusions
Results reveal heterogeneity in longitudinal patterns CPS contact across early childhood among Alaska children and identify maternal substance use as an important target for primary prevention.
Keywords: child protective services, child welfare, child maltreatment, racial disparities
Introduction
In 2016, child protective services (CPS) agencies in the United States received an estimated 4.1 million allegations of abuse or neglect involving approximately 7.4 million children (Services, 2018). Child maltreatment is a salient risk factor for poor outcomes across the life course with previous research demonstrating associations between child maltreatment and poor emotional and social functioning in childhood (Jonson-Reid, Drake, Kim, Porterfield, & Han, 2004; Lanier, Kohl, Raghavan, & Auslander, 2015), mental health and substance use disorders in adolescence (Hussey, Chang, & Kotch, 2006), and chronic conditions such as asthma, diabetes, pain, and obesity in adulthood (Scott et al., 2011; Shin & Miller, 2012). Importantly, previous research suggests that contact with CPS for suspected maltreatment functions as an independent marker of child risk and vulnerability (Putnam-Hornstein & Needell, 2011; Putnam-Hornstein, Schneiderman, Cleves, Magruder, & Krous, 2014; Putnam-Hornstein, Simon, Eastman, & Magruder, 2015). Thus, from a public health perspective, contact with CPS, here defined as any report of suspected maltreatment made to CPS regardless of screening or outcome determination, may represent a proxy for potential or experienced harm to the child. Understanding the nature and timing of CPS contact across early childhood and the individual- and family-level factors associated with various patterns of CPS contact is an important public health and social welfare issue.
The state of Alaska is an important context within the United States for examining child contact with CPS. The rate of maltreatment allegations received by CPS agencies in Alaska is considerably higher than the national average (86.1 vs. 55.1 allegations per 1,000 children under 18 years in 2016) (Alaska Department of Health and Social Services, 2018). Previous research has consistently found differences in CPS contact between various demographic groups of Alaska children. Most notably, research indicates Alaska Native/American Indian (AN/AI) children in Alaska have a higher likelihood of contact with CPS (Austin, Parrish, & Shanahan, 2018; Parrish, Young, Perham-Hester, & Gessner, 2011) and higher rates of substantiated maltreatment (Alaska Departmetn of Health and Social Services, 2018) compared to non-Native children. In addition, the AN/AI population in Alaska has a legacy of high rates of child removal from families and placement into out-of-home care by CPS (Sarche, Spicer, Farrell, & Fitzgerald, 2011). Thus, gaining additional insight into CPS contact among AN/AI and non-Native children in Alaska is important for informing early prevention and intervention efforts to promote child and family wellbeing in the state.
To date, much of the child maltreatment research literature has relied on dichotomous indicators of maltreatment or CPS contact. However, some research has explored more nuanced measures that consider the developmental timing, chronicity, or frequency of alleged or experienced maltreatment. This body of research shows that these nuances have important implications for understanding the impact of child maltreatment and CPS contact on health and development (Cowell, Cicchetti, Rogosch, & Toth, 2015; Jaffee & Maikovich Fong, 2011; Jonson-Reid, Kohl, & Drake, 2012; Kaplow & Widom, 2007). Specifically, multiple studies have found that an earlier age of onset of CPS contact and chronic or continuous CPS contact during childhood are associated with worse health outcomes (Cowell et al., 2015; Jaffee & Maikovich Fong, 2011; Jonson-Reid et al., 2012; Kaplow & Widom, 2007). However, in many of these studies, various nuances of CPS contact, such as developmental timing and chronicity, are not examined simultaneously. It may be that the effect of continuous CPS contact on child health and development depends on the age at which CPS contact first occurred, and vice versa. In addition, these dimensions are often examined based on broad categorizations (i.e., CPS contact prior to and after age one year), potentially obscuring additional heterogeneity in experiences across childhood and differential associations with outcomes.
More recently, a few studies have used longitudinal applications of finite mixture modeling (i.e., growth mixture modeling and latent class growth analysis) to identify groups of children with similar patterns of CPS contact across various periods of childhood (Hurren, Stewart, & Dennison, 2017; Jones et al., 2010; Proctor et al., 2012; Stewart, Livingston, & Dennison, 2008; Yampolskaya, Greenbaum, Brown, & Armstrong, 2015). In finite mixture modeling, the goal is to identify classes of individuals characterized by distinct trajectories of change in an outcome (e.g., CPS contact) over time (Bauer & Reyes, 2010; Muthén & Muthén, 2000). By identifying a small number of substantively meaningful classes, finite mixture models serve as an empirical means of parsimoniously approximating population differences with respect to patterns of change in an outcome over time (Nagin, 2005). Importantly, these methods can be used to identify trajectory classes of CPS contact in which trajectories are simultaneously characterized by the timing, chronicity, and frequency of contact. For example, Hurren et al. (2017) used latent class growth analysis to identify trajectory classes of CPS contact among children with one or more maltreatment allegations substantiated by CPS prior to age 18 years. Six trajectory classes were identified: (1) chronic CPS contact with peak frequency in adolescence; (2) CPS contact in adolescence only; (3) chronic CPS contact with peak frequency in early childhood; (4) low frequency of CPS contact from birth to adolescence with a slight increase in middle childhood; (5) CPS contact in early childhood only; (6) chronic CPS contact with peak frequency in middle childhood (Hurren et al., 2017). The trajectories were characterized by the frequency of CPS contact at each age, the developmental timing of peak or increases in CPS contact, and the chronicity of CPS contact, illustrating the capacity of these methods to summarize multiple dimensions of a complex outcome with a small number of meaningful and interpretable classes (Hurren, Stewart, & Dennison, 2017). Moreover, the trajectories were differentially associated with offending, demonstrating the importance of understanding patterns of CPS contact over time in terms of later outcomes (Hurren et al., 2017)
Previous research demonstrates the utility of longitudinal applications of finite mixture modeling for examining multiple dimensions of CPS contact over time, there are notable gaps. However, most of the existing research has focused on examining outcomes, such as juvenile offending and substance use, associated with identified trajectory classes (Hurren et al., 2017; Jones et al., 2010; Stewart et al., 2008). While important to furthering our understanding of how various patterns of CPS contact are associated with child wellbeing, this provides little information for informing primary prevention efforts and furthering our understanding of the social and environmental context associated with various trajectory classes. Additionally, previous studies regarding trajectories classes of CPS contact have used only screened-in (Jones et al., 2010; Proctor et al., 2012; Yampolskaya et al., 2015) or substantiated (Hurren et al., 2017; Stewart et al., 2008) reports of maltreatment, excluding screened-out and unsubstantiated reports. These have been shown to function as proxies for child risk and vulnerability (Putnam-Hornstein & Needell, 2011; Putnam-Hornstein et al., 2014; Putnam-Hornstein et al., 2015). Therefore, the aims of this study were to 1) identify trajectory classes of contact with CPS for alleged maltreatment from birth until age five years among AN/AI and non-Native children and 2) examine preconception and prenatal risk factors associated with identified trajectory classes.
Methods
Data sources
We used data from the Alaska Longitudinal Child Abuse and Neglect Linkage (ALCANLink) Project. ALCANLink is a population-representative data source linking 2009–2011 Alaska Pregnancy Risk Assessment Monitoring System (PRAMS) data with administrative data sources. Each year, Alaska PRAMS collects self-reported information on maternal behaviors and experiences before, during, and after delivery of a live-born infant through a systematic sample of the state’s birth certificate file, with sampling stratified by AN/AI vs. non-Native status and infant birth weight (<2,500 grams vs. ≥2,5000 grams). In ALCANLink, 2009–2011 Alaska PRAMS births are linked with administrative data sources, including data from the Alaska Office of Children’s Services (Alaska’s CPS agency), Alaska Child Death Review, and death certificates through 2016 to detect CPS contact and child deaths. Additionally, 2009–2011 Alaska PRAMS births are linked to data from the Alaska Department of Revenue regarding child receipt of a dividend from the Permanent Fund. The Permanent Fund is a constitutional amendment in Alaska that places a percent of the oil revenues received by the state into a fund. Each year, all individuals who were an Alaska resident during the previous calendar year and meet additional eligibility criteria can receive a dividend. Approximately 93% of the Alaska population applies to receive a dividend each year with nearly 95% receiving payments (Alaska Department of Revenue, 2017). We used the Permanent Fund database to approximate when children in ALCANLink emigrated out-of-state. Further details regarding data sources and linkage are published elsewhere (Parrish et al., 2017).
Measures
The outcome of interest was the number of unique contacts with CPS in each year of life from birth until age five years. We focused on the period from birth until age five years given that this is an important stage for establishing the foundation for life course health and development (Shonkoff & Phillips, 2000). We defined CPS contact as any report of suspected physical, sexual, or emotional abuse or neglect, regardless of screening or outcome classification, made to the Alaska Office of Children’s Services. We included all reports as previous research demonstrates that children with unsubstantiated reports are similar to children with substantiated reports in terms of later outcomes and risk for future contact with CPS (Drake, Jonson-Reid, Way, & Chung, 2003; Hussey et al., 2005). Moreover, including only screened-in reports makes the assumption that initial exclusions of maltreatment reports are based on sufficient information to make an informed determination.
Death and out-of-state emigration are two events that cause a child to no longer be at risk for CPS contact in a particular state. To account for out-of-state emigration prior to age five years, we identified children who did not receive a Permanent Fund dividend in each calendar year (2009–2016) and assigned these children an approximate date of out-of-state emigration as mid-year of the calendar year following the last year in which they received a dividend (Parrish et al., 2017). For age intervals beginning after the approximate date of out-of-state emigration, we coded CPS contact as missing. We also identified children who died prior to age five years using data from the Alaska Child Death Review and death certificate files. For age intervals beginning after the date of death (N=42), we coded CPS contact as missing.
We selected potential preconception and prenatal risk factors to examine as covariates of identified trajectory classes based on previous research (Coohey, Johnson, Renner, & Easton, 2013; Dubowitz et al., 2011; McDaniel & Slack, 2005; Miller, Orellana, Johnson, Krase, & Anderson-Nathe, 2013; Parrish et al., 2011; Putnam-Hornstein & Needell, 2011; Putnam-Hornstein, Needell, King, & Johnson-Motoyama, 2013; Stith et al., 2009; Thompson et al., 2013; Wu et al., 2004). Factors of interest included maternal age and education at childbirth, preconception and prenatal substance use and experiences of emotional, traumatic, partner, and financial stress in the 12 months prior to childbirth (Table 1). The items used to derive measures of stressful life events are a subset of the Modified Life Events Inventory (Whitehead, Hill, Brogan, & Blackmore-Prince, 2000). The four constructs representing stressful life events (i.e., financial stress, emotional stress, traumatic stress, and partner stress) were developed using principal components analysis to identify individual stressful life events that measured the same underlying construct (Ahluwalia, Merritt, Beck, & Rogers 2001).
Table 1.
Definitions of potential preconception and prenatal risk factors for child protective services contact, Alaska Longitudinal Child Abuse and Neglect Linkage (ALCANLink) project
| Preconception or prenatal risk factor | Definition |
|---|---|
| Maternal age at childbirth | Age at childbirth as recorded on the birth certificate |
| Maternal education at childbirth | <12 years vs. ≥12 years as recorded on the birth certificate |
| Maternal substance use | Self-reported cigarette or alcohol use during last 3 months of pregnancy, self-reported marijuana use during pregnancy or in the 12 months prior to pregnancy, or smoking or alcohol use during pregnancy as recorded on birth certificate |
| Emotional stress 12 months prior to childbirth | A family member sick and had to go into the hospital. Someone close to me died. |
| Traumatic stress 12 months prior to childbirth | I was homeless. I was in a physical fight. My husband or partner or I went to jail. Someone close to me had a problem with drinking or drugs. |
| Partner stress 12 months prior to childbirth | I got separated or divorced from my husband or partner. I argued with your husband or partner more than usual. My husband or partner said he didn’t want me to be pregnant. |
| Financial stress 12 months prior to childbirth | My husband or partner lost his job. I lost my job even though I wanted to go on working. I had a lot of bills I couldn’t pay. |
Statistical analysis
We used growth mixture modeling (GMM) to identify longitudinal trajectory classes of CPS contact. GMM permits identification of latent classes that are characterized by distinct trajectories of change in an outcome over time given patterns observed in the data (Bauer & Reyes, 2010; Muthén & Muthén, 2000). As a preliminary step, we fit a series of unconditional latent curve models to identify the appropriate functional form for modeling counts of CPS contact over time. We fit latent curve models with linear, quadratic, and cubic Poisson, zero-inflated Poisson, and negative binomial distributions. Based on indices of statistical fit, we determined that a linear negative binomial functional form provided the best fit to model counts of CPS contact over time among both AN/AI and non-Native children. Next, we fit a series of GMMs to determine the number of classes needed to adequately summarize heterogeneity in trajectories of CPS contact over time. We evaluated GMMs with one to five classes and varying assumptions related to the within class variance-covariance matrix for trajectory class parameters including 1) heteroscedastic variances and covariances across classes, 2) homoscedastic variances and covariances across classes, and 3) variances and covariances within classes fixed to 0 (i.e., no within class individual differences in change). The third variance-covariance specification is often referred to as latent class growth analysis (LCGA) (D. S. Nagin, 1999). In all models we assumed a common trajectory shape across all classes and homoscedastic residual variances over time within classes.
We compared the fit of competing GMMs, evaluating both variance-covariance assumptions and numbers of classes, using several indices of statistical fit. We used four information criteria including the Akaike Information Criterion (AIC), sample size adjusted Bayesian Information Criterion (ssBIC), Bayesian Information Criterion (BIC), and consistent Akaike Information Criterion (cAIC), with lower values indicating a more optimal balance of model fit and model parsimony (McCutcheon, 1987; Nylund, Asparouhov, & Muthén, 2007). We also used the Lo-Mendell-Rubin adjusted likelihood ratio test to examine the fit of a K-1 class model to that of a K class model, with a p-value<0.05 indicating the K class model was a significantly better fit to the data (Collins & Lanza, 2013). We used entropy, a measure of the degree to which the model produces classes that are well separated, as a descriptive measure of the final model given that entropy can be a poor tool for model selection (Collins & Lanza, 2013). In selecting the best fitting model, we also considered the absolute and relative frequencies of the smallest class and the interpretability of each identified class. To protect against locally optimal solutions, we specified that each estimated model begin with 200 random start values, optimizing the best 50, and confirmed that the maximum log likelihood value was replicated (Hipp & Bauer, 2006).
To examine associations of preconception and prenatal risk factors with identified trajectory classes, we used Vermunt’s three-step approach (Asparouhov & Muthén, 2014; Vermunt, 2010). In GMM, class membership is probabilistic, and there is an uncertainty rate associated with assigning individuals to a particular class, leading to downward biased standard errors (Collins & Lanza, 2013). Vermunt’s three-step approach is a preferred method for examining covariates associated with latent classes because it accounts for the uncertainty rate associated with class membership (Asparouhov & Muthén, 2014; Vermunt, 2010). In Vermunt’s three-step approach, a multinomial logistic regression model is estimated. We used the model estimated intercepts and slopes for each preconception or prenatal risk factor to calculate probabilities of class membership for various combinations of preconception and prenatal risk factors (Cole & Bauer, 2016; D. Nagin, 2005).
We conducted data management in SAS 9.4 and statistical analyses in Mplus 8. All analyses accounted for the complex sampling design of Alaska PRAMS and were conducted separately for AN/AI and non-Native children based on maternal self-reported race on the birth certificate. For 2009–2011 births in Alaska, mothers did not have the option to report multiple races. This study was reviewed and approved by the Institutional Review Board at [x]. Alaska PRAMS is reviewed by Institutional Review Boards at the University of Alaska Anchorage and the Centers for Disease Control and Prevention.
Results
The prevalence of CPS contact prior to age five years and the preconception and prenatal risk factors of interest by AN/AI and non-Native status are presented in Table 2. The prevalence of CPS contact prior to age five years was significantly higher among AN/AI compared to non-Native children (40.1% vs. 15.8%). In addition, the prevalence of emotional stress (33.5% vs. 26.8%) and traumatic stress (33.1% vs. 18.7%), in the 12 months prior to childbirth, maternal education ≤12 years at childbirth (79.7% vs. 41.1%), and maternal substance use (52.0% vs. 27.7%) were significantly higher among mothers of AN/AI children compared to mothers of non-Native children. Mothers of AN/AI children were also significantly younger in age at child birth compared to mothers of non-Native children (25.2 vs. 27.7 years). Additional descriptive characteristics of the study population are provided in Supplemental Table 1.
Table 2.
Prevalence of child protective services contact and preconception and prenatal risk factors by Alaska Native/American Indian and non-Native status (N=3,549)
| Alaska Native/American Indian children | Non-Native children | |||||
|---|---|---|---|---|---|---|
| (N=1,257) | (N=2,102) | |||||
| N or mean | %a (95% CI) | N or mean | %a (95% CI) | χ2 or t-test p-value | ||
| Child protective services contact prior to age 5 years | ||||||
| 536 | 40.1 (37.4, 42.9) | 333 | 15.8 (13.8, 17.8) | <0.0001 | ||
| Emotional stress 12 months prior to childbirth | ||||||
| 416 | 33.5 (30.9, 36.2) | 551 | 26.8 (24.5, 29.1) | 0.0004 | ||
| Traumatic stress 12 months prior to childbirth | ||||||
| 410 | 33.1 (30.4, 35.8) | 372 | 18.7 (16.6, 20.8) | <0.0001 | ||
| Partner stress 12 months prior to childbirth | ||||||
| 398 | 32.1 (29.5, 34.8) | 533 | 25.3 (23.0, 27.5) | 0.0003 | ||
| Financial stress 12 months prior to childbirth | ||||||
| 588 | 47.6 (44.8, 50.4) | 1,094 | 51.3 (48.7, 53.9) | 0.0700 | ||
| Maternal education ≤12 years at childbirth | ||||||
| 984 | 79.8 (77.4, 82.0) | 774 | 41.2 (38.5, 43.8) | <0.0001 | ||
| Maternal substance use | ||||||
| 655 | 52.0 (49.2, 54.8) | 565 | 27.7 (25.3, 30.1) | <0.0001 | ||
| Maternal age at childbirth | 25.2 | (24.9, 25.6) | 27.7 | (27.3, 28.0) | <0.0001 | |
All percentages are weighted to account for the complex sampling design of the Alaska Pregnancy Risk Assessment Monitoring System
Trajectory classes
Indices of statistical fit for GMMs with varying numbers of classes and assumptions regarding the variance-covariance matrix are presented in Table 3 for AN/AI children and Table 4 for non-Native children. Among AN/AI children, across variance-covariance assumptions, GMM with homoscedastic variances and covariances and the LCGA model generally resulted in lower values of the information criteria compared to GMM with heteroscedastic variances and covariances. A three-class GMM with homoscedastic variances and covariances and a three-class LCGA model provided a similar fit in terms of information criteria and produced similar estimated intercepts and slopes. Thus, we selected the more parsimonious LCGA model as the best fitting model. Among non-Native children, a four-class LCGA model provided the best fit, demonstrating the lowest values of the information criteria.
Table 3.
Fit statistics for specific growth mixture models estimated among Alaska Native/American Indian children (N=1,253)
| A. Growth mixture model with heteroscedastic variances and covariances across classes | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 6781.018 | 6811.818 | 6817.818 | 6792.759 | ||
| 2 | 0.689 | 6739.238 | 6805.971 | 6818.971 | 6764.677 | 54.688 (0) |
| 3 | 0.708 | 6732.848 | 6835.514 | 6855.514 | 6771.985 | 20.006 (0.0000) |
| 4 | 0.756 | 6742.752 | 6881.351 | 6908.351 | 6795.587 | 4.037 (0.0897) |
| 5 | 0.758 | 6755.022 | 6929.554 | 6963.554 | 6821.554 | 1.695 (0.5352) |
| B. Growth mixture model with homoscedastic variances and covariances across classes | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 6781.018 | 6811.818 | 6817.818 | 6792.759 | ||
| 2 | 0.624 | 6740.150 | 6786.350 | 6795.350 | 6757.762 | 44.777 (0) |
| 3 | 0.635 | 6733.848 | 6785.448 | 6807.448 | 6757.330 | 11.753 (0.0034) |
| 4 | 0.753 | 6736.334 | 6813.333 | 6828.333 | 6765.687 | 3.357 (0.1497) |
| 5 | 0.716 | 6737.804 | 6830.203 | 6848.203 | 6773.027 | 4.335 (0.1011) |
| C. Growth mixture model with variances and covariances fixed to 0 within classes (i.e., latent class growth analysis) | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 7253.088 | 7268.488 | 7271.488 | 7258.959 | ||
| 2 | 0.725 | 6759.160 | 6789.960 | 6795.960 | 6770.901 | 477.61 (0) |
| 3 | 0.756 | 6749.460 | 6785.660 | 6804.660 | 6767.072 | 14.998 (0.0485) |
| 4 | 0.762 | 6730.434 | 6792.034 | 6804.034 | 6753.916 | 23.91 (0.1961) |
| 5 | 0.714 | 6731.784 | 6808.783 | 6823.783 | 6761.137 | 23.022 (0.6223) |
Note: N differs from Table 2 due to missing data. AIC= Akaike Information Criterion, BIC= Bayesian Information Criterion, CAIC= consistent Akaike Information Criterion, ssBIC= sample size adjusted Bayesian Information Criterion. Lo-Mendell-Rubin adjusted likelihood ratio test p-value <0.05 indicates a better fit of the k class model compared to the k-1class model.
Table 4.
Fit statistics for specific growth mixture models estimated among non-Native children
| A. Growth mixture model with heteroscedastic variances and covariances across classes | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 4803.530 | 4837.411 | 4843.411 | 4818.348 | ||
| 2 | 0.527 | 4753.608 | 4827.017 | 4840.017 | 4785.715 | 62.749 (0) |
| 3 | 0.644 | 4755.418 | 4868.355 | 4888.355 | 4804.813 | 11.965 (0.0532) |
| 4 | 0.736 | 4766.220 | 4918.684 | 4945.684 | 4832.903 | 3.205 (0.2893) |
| 5 | 0.579 | 4778.262 | 4970.254 | 5004.254 | 4862.233 | 1.329 (0.7657) |
| B. Growth mixture model with homoscedastic variances and covariances across classes | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 4803.530 | 4837.411 | 4843.411 | 4818.348 | ||
| 2 | 0.527 | 4770.064 | 4820.885 | 4829.885 | 4792.292 | 37.818 (0.0001) |
| 3 | 0.644 | 4752.750 | 4820.512 | 4832.512 | 4782.387 | 22.337 (0.0179) |
| 4 | 0.736 | 4750.182 | 4834.884 | 4849.884 | 4787.228 | 8.21 (0.1253) |
| 5 | 0.579 | 4754.174 | 4855.817 | 4873.817 | 4798.629 | 1.925 (0.3936) |
| C. Growth mixture model with variances and covariances fixed to 0 within classes (i.e., latent class growth analysis) | ||||||
| Number of classes | Entropy | AIC | BIC | CAIC | ssBIC | Lo-Mendell-Rubin Adjusted Likelihood Ratio test (p-value) |
| 1 | 5317.460 | 5334.400 | 5337.400 | 5324.869 | ||
| 2 | 0.794 | 4790.372 | 4824.253 | 4830.253 | 4805.190 | 510.821 (0) |
| 3 | 0.736 | 4764.836 | 4815.657 | 4824.657 | 4787.064 | 30.22 (0.0114) |
| 4 | 0.736 | 4744.182 | 4811.944 | 4823.944 | 4773.819 | 25.539 (0.0611) |
| 5 | 0.584 | 4748.176 | 4832.878 | 4847.878 | 4785.222 | 1.924 (0.7345) |
Note: N differs from Table 2 due to missing data. AIC= Akaike Information Criterion, BIC= Bayesian Information Criterion, CAIC= consistent Akaike Information Criterion, ssBIC= sample size adjusted Bayesian Information Criterion. Lo-Mendell-Rubin adjusted likelihood ratio test p-value <0.05 indicates a better fit of the k class model compared to the k-1class model.
Graphical depictions of the best fitting models are provided in Figure 1 for AN/AI children and Figure 2 for non-Native children. To facilitate substantive interpretation, we have also provided the average number of CPS contacts in each age interval for the identified trajectory classes. Among AN/AI children, three-fourths (75.4%; N=944) clustered around a class characterized by a very low, but non-zero frequency of CPS contact across all age intervals. An additional 19.6% (N=246) clustered around a class characterized by CPS contact in each age interval, with the frequency of contact increasing slightly over time. The smallest class comprised 5.0% (N=63) of AN/AI children and was characterized by a high (i.e., >1) frequency of CPS contact in the first year of life followed by decreases in the frequency of contact over time.
Figure 1.
Trajectory classes of child protective services contact: Alaska Native/American Indian children (N = 1253).
Figure 2.
Trajectory classes of child protective services contact: Non-Native children (N = 2094).
Among non-Native children, the majority (81.3%; N=1,703) clustered around a class characterized by no CPS contact in any age interval. A total of 9.5% (N=200) clustered around a class characterized by a low (i.e., <0.5) frequency of CPS contact in the first year of life with the frequency of contact increasing slightly over time. An additional 5.8% (N=122) clustered around a class characterized by contact with CPS in the first year of life followed by a sharp decline in the frequency of contact, reaching no contact by age three years. The smallest class comprised approximately 3.3% (N=70) of non-Native children and was characterized by a high frequency of contact in the first year of life with the frequency of contact decreasing slightly over time.
Preconception and prenatal risk factors
Probabilities of trajectory class membership for various combinations of preconception and prenatal risk factors are presented in Table 5 for AN/AI children and Table 6 for non-Native children. For illustrative purposes, we held maternal age at the average maternal age at childbirth for AN/AI (25 years) and non-Native (28 years) children, as altering maternal age did not substantially change probabilities. Among AN/AI and non-Native children, probabilities of trajectory class membership shifted when each preconception or prenatal risk factor was considered individually. Specifically, maternal substance use had the greatest impact on probabilities, increasing the probability of membership in classes characterized by CPS contact.
Table 5.
Probability of trajectory class membership for combinations of preconception and prenatal factors: Alaska Native/American Indian children (N=1,253)
| Trajectory class probabilities | |||
|---|---|---|---|
| No/low CPS contact (N=944, 75.4%) | Continuous CPS contact (N=246, 19.6%) | Early decreasing CPS contact (N=63, 5.0%) | |
| Maternal age 25 | 0.93 | 0.07 | 0.00 |
| Maternal age 25, education ≤12 years | 0.93 | 0.06 | 0.01 |
| Maternal age 25, maternal substance use | 0.81 | 0.19 | 0.00 |
| Maternal age 25, emotional stress 12 months prior to childbirth | 0.91 | 0.09 | 0.00 |
| Maternal age 25, traumatic stress 12 months prior to childbirth | 0.91 | 0.08 | 0.01 |
| Maternal age 25, partner stress 12 months prior to childbirth | 0.88 | 0.11 | 0.01 |
| Maternal age 25, financial stress 12 months prior to childbirth | 0.90 | 0.10 | 0.00 |
| Maternal age 25, all preconception or prenatal factors | 0.52 | 0.44 | 0.04 |
Note: N differs from Table 2 due to missing data.
Table 6.
Probability of trajectory class membership for combinations of preconception and prenatal factors: non-Native children (N=2,094)
| Probability of trajectory class membership | ||||
|---|---|---|---|---|
| No CPS contact (N=1,703, 81.3%) | Low increasing CPS contact (N=200, 9.5%) | High decreasing CPS contact (N=70, 3.3%) | Early, rapid decline CPS contact (N=122, 5.8%) | |
| Maternal age 28, no risk factors | 0.97 | 0.02 | 0.00 | 0.01 |
| Maternal age 28, education ≤12 years | 0.97 | 0.02 | 0.01 | 0.01 |
| Maternal age 28, maternal substance use | 0.83 | 0.13 | 0.02 | 0.02 |
| Maternal age 28, emotional stress 12 months prior to childbirth | 0.97 | 0.02 | 0.00 | 0.01 |
| Maternal age 28, traumatic stress 12 months prior to childbirth | 0.91 | 0.05 | 0.03 | 0.00 |
| Maternal age 28, partner stress 12 months prior to childbirth | 0.95 | 0.02 | 0.02 | 0.01 |
| Maternal age 28, financial stress 12 months prior to childbirth | 0.97 | 0.02 | 0.01 | 0.01 |
| Maternal age 28, all preconception or prenatal factors | 0.46 | 0.32 | 0.19 | 0.03 |
Note: N differs from Table 2 due to missing data.
Probabilities shifted substantially when all preconception or prenatal risk factors (i.e., education ≤12 years, maternal substance use, and emotional, traumatic, partner and financial stress in the 12 months prior to childbirth) were considered in combination. For example, among AN/AI children (with a mother who was 25 years at their birth), the probability of clustering around the continuous CPS contact class was 6–19% when considering any individual risk factor in isolation. However, when all risk factors were considered, the estimated probability was 44%. Similarly, among non-Native children (with a mother who was 28 years at their birth), the probability of clustering around the low increasing CPS contact class was 2–13% when considering any individual risk factor in isolation. However, given all risk factors, the estimated probability was 32%.
Discussion
Child contact with CPS for suspected maltreatment is an important indicator of potential or experienced harm to the child and can function as an independent marker of child risk and vulnerability (Putnam-Hornstein & Needell, 2011; Putnam-Hornstein et al., 2014; Putnam-Hornstein et al., 2015). This is the first study to identify heterogeneous patterns of child contact with CPS during the first five years of life among a particularly high-risk population, Alaska children. Moreover, this study contributes to child maltreatment prevention efforts by examining preconception and prenatal factors associated with patterns of CPS contact.
Trajectory classes
We identified distinct longitudinal trajectory classes (i.e., patterns) of CPS contact among both AN/AI and non-Native children prior to age five years, with trajectory classes characterized by the timing, chronicity, and frequency of contact. Among AN/AI children, we identified three classes: 1) a no/low CPS contact class; 2) a continuous CPS contact class, and 3) an early, decreasing CPS contact class. Among non-Native children, we identified four classes: 1) a no CPS contact class; 2) a low, increasing CPS contact class; 3) an early, rapid decline CPS contact class; and 4) a high, decreasing CPS contact class. These results demonstrate heterogeneity in longitudinal patterns of CPS contact both within and between AN/AI and non-Native children in Alaska.
Overall, a larger proportion of AN/AI compared to non-Native children clustered around trajectory classes characterized by some level of CPS contact during early childhood (approximately 25% vs. 19%, respectively). In addition, trajectory classes among AN/AI children tended to be characterized by a higher frequency of CPS contact in each age interval compared to classes among non-Native children. These findings are consistent with previous research demonstrating a higher likelihood of CPS contact among AN/AI compared to non-Native children in Alaska (Parrish et al., 2011). There are multiple potential explanations for the higher likelihood of CPS contact among AN/AI compared to non-Native children, including institutional and detection bias and differing distributions of risk factors such as poverty and substance use disorders (Newby-Kew, DeLozier, Prince, Perham-Hester, & Young, 2014) between populations. Importantly, experiences of intergenerational and collective trauma among the AN/AI population in Alaska are reflected in, and contribute to, the disproportionate exposure to various risk factors among AN/AI compared to non-Native children (Evans-Campbell, 2008; Heart & DeBruyn, 1998). Further research is needed to understand the relative contributions of each to greater contact with CPS among AN/AI compared to non-Native children in Alaska.
Nearly 20% of AN/AI children clustered around the continuous CPS contact class. In addition, approximately 10% of non-Native children clustered around the low, increasing CPS contact class and 3% clustered around the high decreasing CPS contact class. While these classes differed in size and in frequency of CPS contact, each class represents children who had continuous contact with CPS from birth throughout early childhood and across multiple developmental periods. This is notable, as previous research has found that chronic or continuous CPS contact and an earlier age of onset of CPS contact are particularly detrimental for child health and development (Cowell et al., 2015; Jaffee & Maikovich Fong, 2011; Jonson-Reid et al., 2012; Kaplow & Widom, 2007). These classes may be comprised of children and families with high levels of adversity or risk that are difficult to address through traditional CPS services or referrals. In Alaska, effective provision of child and family services, such as home visiting, parenting skills, and family counseling programs, is particularly challenging given the geographic isolation of many rural communities in the state (Driscoll, Dotterrer, Miller, & Voorhees, 2010; Zuckerman, Haley, Roubideaux, & Lillie-Blanton, 2004).
The remaining 5% of AN/AI children clustered around the early, decreasing CPS contact class, and the remaining 6% of non-Native children clustered around the early, rapid decline CPS contact class. Both classes were characterized by contact with CPS in the first years of life, with the frequency of contact decreasing through age five years. In contrast to the early, decreasing CPS contact class among AN/AI children, the early, rapid decline CPS contact class among non-Native children had lower frequencies of CPS contact in each age interval and reached no contact at an earlier age. The decrease in CPS contact across early childhood observed in these classes may reflect family needs being met through appropriate services and referrals or a lower level of need among some referred families. However, the decrease in contact may also have been triggered by child removal from the home and placement into kinship or foster care. To assess the role of out-of-home placements, we conducted post-hoc analyses in which we assigned children to a trajectory class based on their highest posterior probability of membership and determined the percent of children in each class who were removed from the home prior to age five years. We found that approximately 42% of AN/AI children assigned to the early, decreasing CPS contact class and 10% of non-Native children assigned to the early, rapid decline CPS contact class experienced an out-of-home placement prior to age five years. This suggests that out-of-home placements may have played a larger role in the observed decrease in CPS contact in the early, decreasing CPS contact class among AN/AI children than in the early, rapid decline CPS contact class among non-Native children.
Preconception and prenatal risk factors
Each preconception or prenatal risk factor considered individually increased the probability of membership in trajectory classes characterized by some level of CPS contact during early childhood. Among both AN/AI and non-Native children, the individual risk factor that had the largest impact on probabilities of class membership was maternal substance use, including use of alcohol, cigarettes, and marijuana shortly before and during pregnancy. For example, given average maternal age at childbirth, the probability of membership in the continuous CPS contact class among AN/AI children was 0.07. Given average maternal age at childbirth and maternal substance use, the probability of membership in the continuous CPS contact class among AN/AI children increased to 0.19. Maternal substance use has received increasing attention in the research literature as a contributing factor to child welfare involvement (Prindle, Hammond, & Putnam-Hornstein, 2018; Rebbe, Mienko, Brown, & Rowhani-Rahbar, 2019). Previous research has found that infants exposed to substances prenatally are more likely to be referred to CPS for suspected maltreatment compared to their unexposed counterparts (Prindle et al., 2018). In our data, we were not able to determine whether maternal substance use was a primary factor contributing to CPS contact after birth or whether other risk factors that tend to co-occur with substance use, such as mental health disorders and poverty (Sadicario, Kelpin, & Svikis, 2017; Washio, Mericle, Cassey, Daubert, & Kirby, 2015), were the primary impetus for child welfare involvement. Regardless, it appears that maternal substance use may serve as an indicator of future CPS contact and a marker of unmet family need for services. This suggests that addressing maternal substance use, and other family, social, and environmental stressors contributing to such use, through evidence-based services prior to the birth of the child might alter the trajectories of CPS contact for some children, potentially leading some to follow lower contact trajectories. However, it will be important for child welfare and other social service agencies engaging with these families to acknowledge that addressing substance use is a time intensive process, as many individuals cycle through periods of substance use treatment, recovery, and return to use (Scott, Foss, & Dennis, 2005).
Limitations
The results of this study should be viewed in light of several limitations. First, data from Alaska PRAMS are based on maternal self-report and are subject to biases common to self-report data including social desirability, recall, and non-response bias. Where possible, we combined data from multiple sources (i.e., Alaska PRAMS and the birth certificate) to address some of these issues. Second, we did not assess paternal characteristics shortly before or during pregnancy that may be associated with patterns of CPS contact. Some data regarding paternal characteristics, such as race, were available from the birth certificate, but a higher percent of this data was missing than for mothers. Thus, we chose to examine factors specific to maternal characteristics and experiences. Third, we were limited in terms of the number and type of preconception and prenatal risk factors we were able to examine in this study due to model complexity and limitations of the available data. Future studies would benefit from examining additional risk factors such as maternal intimate parent violence and mental health and experiences of intergenerational and collective trauma among the AN/AI population. Fourth, we only had data pertaining to maternal use of alcohol, cigarettes, and marijuana. We lacked data on prenatal use of other substances, such as opioids and cocaine, which have also been found to be associated with CPS contact (Prindle et al., 2018; Rebbe et al., 2019). Fifth, for children who moved out of Alaska prior to age five years, the exact date of out-of-state emigration was not available. Based on the Permanent Fund data, we estimated an approximate date of out-of-state emigration. While this may have led to some imprecise exclusions, it allowed us to account for an event that causes children to no longer be at risk for CPS contact in Alaska. Sixth, we used data from one large, rural state limiting generalizability to families in other areas of the U.S.
Conclusions
Understanding patterns of CPS contact during early childhood among AN/AI and non-Native children and prenatal and preconception risk factors associated with such patterns can provide insights for informing child welfare practices and child maltreatment prevention efforts. Our results indicate variation in longitudinal trajectories of CPS contact among Alaska children, with a higher likelihood of CPS contact during early childhood noted among AN/AI compared to non-Native children. Most notably, we found that nearly one in five AN/AI children clustered around a trajectory class characterized by continuous CPS contact from birth to age five years, underscoring the need to more closely examine potential factors underlying chronic child welfare involvement among the AN/AI population. Our results also indicate that maternal substance use may be a particularly important risk factor for future CPS contact among both AN/AI and non-Native children. Integration of substance use assessment and treatment services into preconception and prenatal care may help prevent the need for child welfare involvement and ultimately contribute to children following lower frequency CPS contact trajectories.
Supplementary Material
Acknowledgments
We would like to recognize the contributions of the multiple agencies that facilitated access to the data used in this study. We would like to thank Jared Parrish (Maternal and Child Health Epidemiology Unit), Kathy Perham-Hester (Alaska PRAMS coordinator), Margaret Young (Alaska CUBS coordinator), Kim Guay (Alaska Office of Children’s Services), and Travis Erickson (Alaska Office of Children’s Services). The findings reported herein were performed using data collected and maintained by the Alaska Division of Public Health. The opinions and conclusions expressed are solely those of the authors and should not be considered as representing the policy of any agency of the Alaska government.
Funding: Ms. Austin was supported by an award to the University of North Carolina Injury Prevention Research Center from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (R49 CE002479), a training grant from the National Institute of Child Health and Development (T32 HD52468), and a grant from the Health Resources and Services Administration (R40 MC30757). Dr. Gottfredson is supported by a grant from the National Institute on Drug Abuse (K01 DA035153).
Footnotes
Conflict of interest: The authors have no potential conflicts of interest to disclose.
Financial disclosure: The authors have no financial relationships to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahluwalia IB, Merritt R, Beck LF, & Rogers M (2001). Multiple lifestyle and psychosocial risks and delivery of small for gestational age infants. Obstetrics & Gynecology, 97(5), 649–656. [DOI] [PubMed] [Google Scholar]
- Alaska Department of Revenue, Permanent Fund Dividend. (2017). Summary of Dividend Applications and Payments. Retrieved from https://pfd.alaska.gov/Division-Info/Summary-of-Applications-and-Payments. Published 2019 Accessed March 5, 2019.
- Asparouhov T, & Muthén B (2014). Auxiliary variables in mixture modeling: Three-step approaches using M plus. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 329–341. [Google Scholar]
- Austin AE, Parrish JW, & Shanahan ME (2018). Using time-to-event analysis to identify preconception and prenatal predictors of child protective services contact. Child Abuse & Neglect, 82, 83–91. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, & Reyes HL (2010). Modeling variability in individual development: Differences of degree or kind? Child Developmental Perspectives, 4(2), 114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole VT, & Bauer DJ (2016). A note on the use of mixture models for individual prediction. Structural Equation Modeling: A Multidisciplinary Journal, 23(4), 615–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2013). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences (Vol. 718): John Wiley & Sons. [Google Scholar]
- Coohey C, Johnson K, Renner LM, & Easton SD (2013). Actuarial risk assessment in child protective services: Construction methodology and performance criteria. Children and Youth Services Review, 35(1), 151–161. [Google Scholar]
- Cowell RA, Cicchetti D, Rogosch FA, & Toth SL (2015). Childhood maltreatment and its effect on neurocognitive functioning: Timing and chronicity matter. Development and Psychopathology, 27(02), 521–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake B, Jonson-Reid M, Way I, & Chung S (2003). Substantiation and recidivism. Child Maltreatment, 8(4), 248–260. [DOI] [PubMed] [Google Scholar]
- Driscoll D, Dotterrer B, Miller J, & Voorhees H (2010). Assessing the influence of health on rural outmigration in Alaska. International Journal of Circumpolar Health, 69(5), 528–544. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Kim J, Black MM, Weisbart C, Semiatin J, & Magder LS (2011). Identifying children at high risk for a child maltreatment report. Child aAuse & Neglect, 35(2), 96–104. [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23(3), 316–338. [DOI] [PubMed] [Google Scholar]
- Heart MYHB, & DeBruyn LM (1998). The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research, 8(2), 56. [PubMed] [Google Scholar]
- Hipp JR, & Bauer DJ (2006). Local solutions in the estimation of growth mixture models. Psychological Methods, 11(1), 36. [DOI] [PubMed] [Google Scholar]
- Hurren E, Stewart A, & Dennison S (2017). Transitions and turning points revisited: A replication to explore child maltreatment and youth offending links within and across Australian cohorts. Child Abuse & Neglect, 65, 24–36. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118(3), 933–942. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Marshall JM, English DJ, Knight ED, Lau AS, Dubowitz H, & Kotch JB (2005). Defining maltreatment according to substantiation: Distinction without a difference? Child Aubse & Neglect, 29(5), 479–492. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, & Maikovich Fong AK (2011). Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. Journal of Child Psychology and Psychiatry, 52(2), 184–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DJ, Runyan DK, Lewis T, Litrownik AJ, Black MM, Wiley T, … Nagin DS (2010). Trajectories of childhood sexual abuse and early adolescent HIV/AIDS risk behaviors: The role of other maltreatment, witnessed violence, and child gender. Journal of Clinical Child and Adolescent Psychology, 39(5), 667–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonson-Reid M, Drake B, Kim J, Porterfield S, & Han L (2004). A prospective analysis of the relationship between reported child maltreatment and special education eligibility among poor children. Child Maltreatment, 9(4), 382–394. [DOI] [PubMed] [Google Scholar]
- Jonson-Reid M, Kohl PL, & Drake B (2012). Child and adult outcomes of chronic child maltreatment. Pediatrics, 129(5), 839–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, & Widom CS (2007). Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology, 116(1), 176. [DOI] [PubMed] [Google Scholar]
- Lanier P, Kohl PL, Raghavan R, & Auslander W (2015). A preliminary examination of child well-being of physically abused and neglected children compared to a normative pediatric population. Child Maltreatment, 20(1), 72–79. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL (1987). Latent class analysis: Sage. [Google Scholar]
- McDaniel M, & Slack KS (2005). Major life events and the risk of a child maltreatment investigation. Children and Youth Services Review, 27(2), 171–195. [Google Scholar]
- Miller KM, Orellana ER, Johnson AB, Krase K, & Anderson-Nathe B (2013). Maternal criminal justice and child welfare involvement: Associations between risk exposures and childhood mental health. Social Work Research, 37(4), 402–413. [Google Scholar]
- Muthén B, & Muthén LK (2000). Integrating person centered and variable centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research, 24(6), 882–891. [PubMed] [Google Scholar]
- Nagin D (2005). Group-based modeling of development: Harvard University Press. [Google Scholar]
- Nagin DS (1999). Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods, 4(2), 139. [DOI] [PubMed] [Google Scholar]
- Newby-Kew AJ, DeLozier DP, Prince CB, Perham-Hester KA, & Young MB (2014). Alaska Maternal and Child Health Data Book 2014: Life Course Edition. Anchorage, AK: Alaska Department of Health and Social Services. [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. [Google Scholar]
- Parrish JW, Shanahan ME, Schnitzer PG, Lanier P, Daniels JL, & Marshall SW (2017). Quantifying sources of bias in longitudinal data linkage studies of child abuse and neglect: Measuring impact of outcome specification, linkage error, and partial cohort follow-up. Injury Epidemiology, 4(1), 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrish JW, Young MB, Perham-Hester KA, & Gessner BD (2011). Identifying risk factors for child maltreatment in Alaska: A population-based approach. American Journal of Preventive Medicine, 40(6), 666–673. [DOI] [PubMed] [Google Scholar]
- Prindle JJ, Hammond I, & Putnam-Hornstein E (2018). Prenatal substance exposure diagnosed at birth and infant involvement with child protective services. Child Abuse & Neglect, 76, 75–83. [DOI] [PubMed] [Google Scholar]
- Proctor LJ, Aarons GA, Dubowitz H, English DJ, Lewis T, Thompson R, … Roesch SC (2012). Trajectories of maltreatment re-reports from ages 4 to 12: Evidence for persistent risk after early exposure. Child Maltreatment, 17(3), 207–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam-Hornstein E, & Needell B (2011). Predictors of child protective service contact between birth and age five: An examination of California’s 2002 birth cohort. Children and Youth Services Review, 33(8), 1337–1344. [Google Scholar]
- Putnam-Hornstein E, Needell B, King B, & Johnson-Motoyama M (2013). Racial and ethnic disparities: A population-based examination of risk factors for involvement with child protective services. Child Abuse & Neglect, 37(1), 33–46. [DOI] [PubMed] [Google Scholar]
- Putnam-Hornstein E, Schneiderman JU, Cleves MA, Magruder J, & Krous HF (2014). A prospective study of sudden unexpected infant death after reported maltreatment. Journal of Pediatrics, 164(1), 142–148. [DOI] [PubMed] [Google Scholar]
- Putnam-Hornstein E, Simon JD, Eastman AL, & Magruder J (2015). Risk of re-reporting among infants who remain at home following alleged maltreatment. Child Maltreatment, 20(2), 92–103. [DOI] [PubMed] [Google Scholar]
- Rebbe R, Mienko JA, Brown E, & Rowhani-Rahbar A (2019). Child protection reports and removals of infants diagnosed with prenatal substance exposure. Child Abuse & Neglect, 88, 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadicario JS, Kelpin SS, & Svikis D (2017). Where there’s smoke: Psychosocial and mental health correlates of prenatal marijuana use. Drug & Alcohol Dependence, 171. [Google Scholar]
- Sarche MC, Spicer P, Farrell P, & Fitzgerald HE (2011). American Indian and Alaska Native Children and Mental Health: Development, Context, Prevention, and Treatment: ABC-CLIO. [Google Scholar]
- Scott CK, Foss MA, & Dennis ML (2005). Pathways in the relapse—treatment—recovery cycle over 3 years. Journal of Substance Abuse Treatment, 28(2), S63–S72. [DOI] [PubMed] [Google Scholar]
- Scott KM, Von Korff M.. Posada-Villa J (2011). Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Archives of General Psychiatry, 68(8), 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Child Maltreatment 2016. (2018). Retrieved from https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment. Published January 28. 2019 Accessed March 5, 2019.
- Shin SH, & Miller DP (2012). A longitudinal examination of childhood maltreatment and adolescent obesity: results from the National Longitudinal Study of Adolescent Health (AddHealth) Study. Child Abused & Neglect, 36(2), 84–94. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, & Phillips DA (2000). From neurons to neighborhoods: The science of early childhood development: National Academies Press. [PubMed] [Google Scholar]
- Stewart A, Livingston M, & Dennison S (2008). Transitions and turning points: examining the links between child maltreatment and juvenile offending. Child Abuse & Neglect, 32(1), 51–66. [DOI] [PubMed] [Google Scholar]
- Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, … Dees J (2009). Risk factors in child maltreatment: A meta-analytic review of the literature. Aggression and Violent Behavior, 14(1), 13–29. [Google Scholar]
- Thompson EL, Thompson LA, Black EW, Esernio-Jenssen D, Hardt N, Das R, & Roth J (2013). Identifying indicators during pregnancy for child maltreatment. Maternal and Child Health Journal, 17(10), 1817–1824. [DOI] [PubMed] [Google Scholar]
- Vermunt JK (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. [Google Scholar]
- Washio Y, Mericle AA, Cassey H, Daubert A, & Kirby KC (2015). Correlates of risk for prenatal alcohol use among WIC recipients. Drug & Alcohol Dependence, 146. [Google Scholar]
- Whitehead N, Hill HA, Brogan DJ, & Blackmore-Prince C (2002). Exploration of threshold analysis in the relation between stressful life events and preterm delivery. American Journal of Epidemiology, 155(2), 117–124. [DOI] [PubMed] [Google Scholar]
- Wu SS, Ma C-X, Carter RL, Ariet M, Feaver EA, Resnick MB, & Roth J (2004). Risk factors for infant maltreatment: a population-based study. Child Abuse & Neglect, 28(12), 1253–1264. [DOI] [PubMed] [Google Scholar]
- Yampolskaya S, Greenbaum PE, Brown CH, & Armstrong MI (2015). Heterogeneity in Trajectories of Child Maltreatment Severity: A Two-Part Growth Mixture Model. Violence and Victimization, 30(5), 916–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman S, Haley J, Roubideaux Y, & Lillie-Blanton M (2004). Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: What role does the Indian Health Service play? American Journal of Public Health, 94(1), 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.