Abstract
Clinical reasoning is a core component of clinical competency that is used in all patient encounters from simple to complex presentations. It involves synthesis of myriad clinical and investigative data, to generate and prioritize an appropriate differential diagnosis and inform safe and targeted management plans.
The literature is rich with proposed methods to teach this critical skill to trainees of all levels. Yet, ensuring that reasoning ability is appropriately assessed across the spectrum of knowledge acquisition to workplace-based clinical performance can be challenging.
In this perspective, we first introduce the concepts of illness scripts and dual-process theory that describe the roles of analytic system 1 and non-analytic system 2 reasoning in clinical decision making. Thereafter, we draw upon existing evidence and expert opinion to review a range of methods that allow for effective assessment of clinical reasoning, contextualized within Miller’s pyramid of learner assessment. Key assessment strategies that allow teachers to evaluate their learners’ clinical reasoning ability are described from the level of knowledge acquisition, through to real-world demonstration in the clinical workplace.
KEY WORDS: medical education-assessment method, medical education-assessment/evaluation, medical education-cognition/problem solving, clinical reasoning
INTRODUCTION
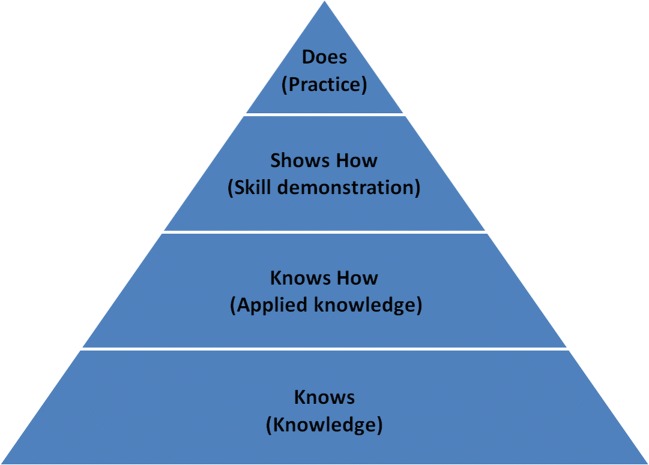
Clinical reasoning is the “thinking and decision making processes associated with clinical practice.”1 It involves pattern recognition, knowledge application, intuition, and probabilities. It is integral to clinical competency and is gaining increasing attention within medical education. Much has been written about the cognitive processes underpinning reasoning strategies and the myriad ways educators can enhance learners’ clinical reasoning abilities. Literature onassessing clinical reasoning, however, is more limited with focus on written assessments targeting the lower levels of “knows” and “knows how” of Miller’s pyramid (Fig. 1).2 This article offers a more holistic perspective on assessing clinical reasoning by exploring current thinking and strategies at all levels.
Figure 1.
Miller’s pyramid of clinical competence (supplied also as a .tif file). Adapted from Miller2.
CLINICAL REASONING MODELS
Although many clinical reasoning models have been proposed, script theory3 and dual-process theory4 have attracted particular attention among medical educators. Script theory suggests clinicians generate and store mental representations of symptoms and findings of a particular condition (“illness scripts”) with networks created between existing and newly learnt scripts. Linked to this is dual-process theory which suggests that clinical decision making operates within two systems of thinking. System 1 thinking utilizes pattern recognition, intuition, and experience to effortlessly activate illness scripts to quickly arrive at a diagnosis. Conversely, clinicians utilizing system 2 thinking analytically and systematically compare and contrast illness scripts in light of emerging data elicited from history and examination while factoring in demographic characteristics, comorbidity, and epidemiologic data. In this approach, clinicians test probable hypotheses, using additional information to confirm or refute differential diagnoses. Although system 2 thinking requires more cognitive effort, it is less prone to the biases inherent within system 1 thinking.5 Several cognitive biases have been characterized6 with key examples outlined in Table 1. With increasing experience, clinicians skillfully gather and apply relevant data by continually shifting between non-analytic and analytic thinking.7
Table 1.
Examples of Cognitive Biases
| Cognitive bias | Description |
|---|---|
| Anchoring bias | The tendency to over rely on, and base decisions on, the first piece of information elicited/offered |
| Confirmation bias | The tendency to look for evidence to confirm a diagnostic hypothesis rather than evidence to refute it |
| Availability bias | The tendency to over rely on, and base decisions on, recently encountered cases/diagnoses |
| Search satisficing | The tendency to stop searching for other diagnoses after one diagnosis appears to fit |
| Diagnosis momentum | The tendency to continue relying on an initial diagnostic label assigned to a patient by another clinician |
| Ambiguity effect | The tendency to make diagnoses for which the probability is known over those for which the probability is unknown |
Attempting to assess complex internal cognitive processes that are not directly observable poses obvious challenges. Furthermore, it cannot be assumed that achieving correct final outcomes reflects sound underpinning reasoning. Potential strategies however have been suggested to address these difficulties and are described below at each level of Miller’s pyramid.
ASSESSING CLINICAL REASONING AT THE “KNOWS” AND “KNOWS HOW” LEVELS
In the 1970s, patient management problems (PMPs) were popular and utilized a patient vignette from which candidates selected management decisions.8 Originally designed to assess problem-solving strategies, later work suggested PMPs were likely only testing knowledge acquisition.9 Often, there was disagreement among experts on the possible correct answer along with poor case specificity (performance on one case poorly predicting performance on another).10 Furthermore, experienced clinicians did not always score higher than juniors.10 As a result, the use of PMPs has declined.
Subsequently, script concordance tests (SCTs) were developed based on the previously mentioned concept of “illness script.”3 An example SCT is shown in Text box 1. Examinees are faced with a series of patient scenarios and decide, using a Likert-type scale, whether a particular item (such as a symptom, test, or result) would make a diagnosis more or less likely. Examinees’ answers are compared with those from experts, with weighted scoring applied to responses chosen by more expert clinicians.11 SCTs offer reliable assessments (achieving alpha of 0.77–0.82)11–13 with agreement from both examiners and candidates that real-world diagnostic thinking is being assessed.12,14 They predict performance on other assessments (such as Short Answer Management Problems and Simulated Office Orals),15 allow for discrimination across the spectrum of candidate ability,12 and show improved performance with increasing experience (construct validity).12
Text Box 1. Example SCT
A 55-year-old man presents to your clinic with a persistent cough of 6 weeks.
| If you were thinking of: | And then you find: | This diagnosis becomes |
| Q1: Lung cancer | Patient has smoked 20 cigarettes a day for 30 years | − 2 − 1 0 + 1 + 2 |
| Q2: Drug side effect | Patient started ace inhibitor 6 weeks ago | − 2 − 1 0 + 1 + 2 |
| Q3: COPD | Patient has never smoked | − 2 − 1 0 + 1 + 2 |
− 2 Ruled out or almost ruled out; − 1 Less likely; 0 Neither more nor less likely; + 1 More likely; + 2 Certain or almost certain
Key feature questions (KFQs) require candidates to identify essential elements within a clinical vignette in relation to possible diagnoses, investigations, or management options.16 In keeping with SCTs, KFQs similarly demonstrate good face validity, construct validity, and predictive validity of future performance.16 In addition, KFQs are thought to have an advantage over SCTs as they can minimize the cueing effect within the latter’s response format.17
The clinical integrative puzzle (CIP) bases itself on the extended matching question concept but utilizes a grid-like appearance which requires learners to compare and contrast a group of related diagnoses across domains such as history, physical examination, pathology, investigations, and management.18 CIPs encourage integration of learning and consolidation of illness scripts and demonstrate good reliability (up to 0.82) but only modest validity.19
The ASCLIRE method uses computer-delivered patient scenarios that allow learners to seek additional data from a range of diagnostic measures in order to select a final diagnosis from a differential list.20 Diagnostic accuracy, decision time, and choice of additional diagnostic data are used to differentiate reasoning abilities. It is estimated that 15 scenarios, over 180 min, would achieve a reliability of 0.7. ASCLIRE is well received by candidates and demonstrates appropriate construct validity, with experts outscoring novices.20
More recently, virtual patients have been developed with software enabling students to categorize diagnoses as unlikely or not to be missed through illness script–based concept maps.21 Although currently proposed for use as a learning tool, future development could offer assessment possibilities.
ASSESSING CLINICAL REASONING AT THE “SHOWS HOW” LEVEL
Objective structured clinical examinations (OSCEs) are widely accepted as robust assessments of learners’ clinical competencies. From the first papers describing OSCEs in the 1970s22 to the multitude of publications since, their ability to assess a range of clinical skills including problem-solving abilities has been emphasized. Despite this stated aim, the literature however is limited to components of clinical competency such as history taking, physical examination, or explanation of diagnoses, with less attention paid to understanding how OSCEs can be used to assess clinical reasoning ability.
Given the paucity of published work in this area, assessment and teaching academics from the lead authors’ institution have worked collaboratively to transform historically used OSCE stations, which often operated on simple pattern recognition, into stations that require analytical system 2 thinking. Table 2 describes strategies that have proven successful.
Table 2.
Suggested OSCE design strategies
| Station type | Design strategies |
|---|---|
| History taking stations | Create simulated patient scripts such that not all possible symptoms are present and/or add in symptoms that may suggest more than one plausible differential diagnosis |
| Include end-of-station examiner questions that require candidates to not only name, but also justify, their likely differential diagnoses | |
| In longer stations, consider stop-start techniques in which candidates are asked at different time points to list their differential diagnoses | |
| Physical examination stations | Design hypothesis-driven or presentation-based examinations (requiring the candidate to conduct an appropriate examination from a stated differential list or short clinical vignette) rather than full system-based examinations23 |
| Data interpretation stations | Utilize clinical data (either at once or sequentially) along with a clinical vignette and examiner questions to assess not just the candidate’s data reporting ability, butinterpretation ability in light of the clinical situation described |
| Explanation stations | Provide clinical results/data requiring candidate interpretation and offering real-world clinical context to base explanations and justifications |
Further modifications to the traditional OSCE format replace end-of-station examiner questions with post-encounter forms (PEF, also called progress notes or patient notes) as an inter-station task.24–28 Following a typical consultation-based OSCE station (history taking/clinical examination), the candidate is required to write a summary statement, list of differential diagnoses, and, crucial to the assessment of reasoning, their justification for each differential using supporting or refuting evidence obtained from the consultation. Post-encounter forms demonstrate good face validity24 and inter-rater reliability through the use of standardized scoring rubrics.24,25 In addition, candidates can be asked to provide an oral presentation of the case to an examiner who rates their performance on Likert-scale items.24 Although candidates’ performance on the consultation, PEF, and oral presentation poorly correlate with each other, it is suggested that this reflects the differing elements of reasoning being assessed by each.24,27
Lastly, how OSCE stations are scored may impact candidates’ demonstration of reasoning ability. Checklist-based rubrics often trivialize the complexity of patient encounters and thus may discourage the use of analytical system 2 approaches. Conversely, rating scales that assess component parts of performance (analytic) or overall performance (global) offer improved reliability and validity in capturing a more holistic perspective on candidates’ overall performance.29 However, whether analytic or global rating scales differ in their assessment of clinical reasoning remains unclear.25,27
Scale issues aside, the challenge for OSCE examiners remains trying to score, through candidate observation, the internal cognitive process of clinical reasoning. Recent work however has provided guidance, suggesting that there are certain observable behaviors demonstrated by candidates which reflect their reasoning processes as shown in Table 3.30
Table 3.
Observable Behaviors of Clinical Reasoning During Patient Interactions
| Level 1 | Student acts | Taking the lead in the conversation |
| Recognizing and responding to relevant information | ||
| Specifying symptoms | ||
| Asking specific questions pointing to pathophysiological thinking | ||
| Putting questions in a logical order | ||
| Checking with patients | ||
| Summarizing | ||
| Body language | ||
| Level 2 | Patient acts | Patient body language, expressions of understanding or confusion |
| Level 3 | Course of the conversation | Students and patients talking at cross purposes, repetition |
| Level 4 | Data gathered and efficiency | Quantity and quality of data gathered |
| Speed of data gathering |
Based on Haring et al.31
ASSESSING CLINICAL REASONING AT THE “DOES” LEVEL
Since clinical reasoning proficiency in knowledge tests or simulated settings does not automatically transfer to real-life clinical settings, it is critical to continue assessment in the workplace, thereby targeting the top of Miller’s pyramid at the “does” level.2 Clinical teachers should assess how learners tackle uncertainty and detect when the reasoning process is derailed by limitations in knowledge or experience, cognitive biases, or inappropriate application of analytic and non-analytic thinking.5,6 For example, if novice learners demonstrate non-analytic thinking, clinical teachers should question their reasons for prioritizing certain diagnoses over others. However, advanced learners can apply non-analytic thinking to simpler clinical scenarios. Experts demonstrate higher diagnostic accuracy rates and lower decision making time than novices30,32 and skillfully utilize both non-analytic and analytic thinking.7 Therefore, learners will benefit when expert clinical teachers think out loud as they develop diagnostic hypotheses.
Clinical teachers routinely observe learners to assess their clinical skills; however, such assessment is often informal, in the moment and impression-based rather than systematic. Moreover, it is often the end point that is assessed rather than the process of reasoning. While summative assessment can determine whether learners have achieved expected competencies, formative assessment fosters a climate of assessment for learning. Frameworks that allow for formative systematic assessment of clinical reasoning are therefore valuable and exemplars are described below.
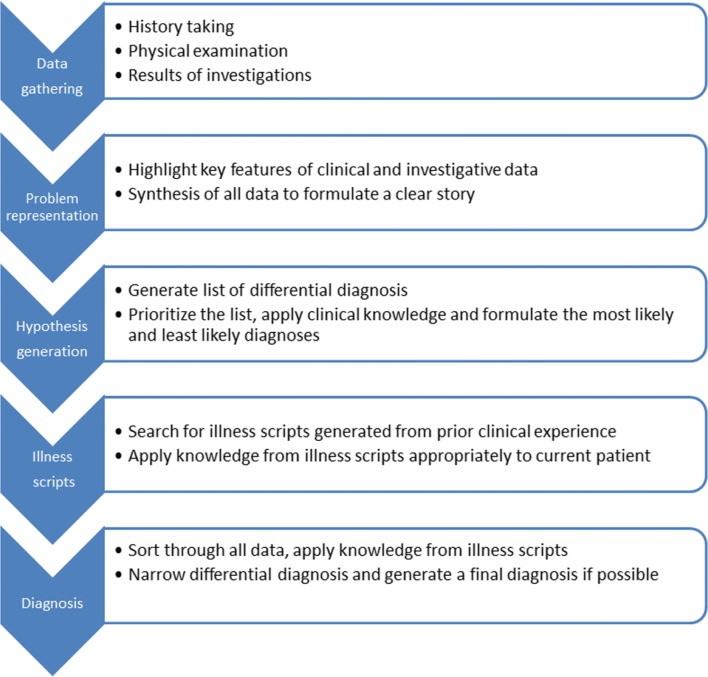
Bowen’s framework lists sequential steps that can be demonstrated and assessed by clinical teachers as shown in Figure 2.33 These include data gathering (history, examination findings, results of investigations), summarizing key features of the case (problem representation), generating differential diagnoses (diagnostic hypothesis), applying prior knowledge (illness scripts), and final diagnosis.33 The assessment of reasoning tool similarly describes a five-component assessment process (hypothesis-directed data collection, problem representation, prioritized differential diagnosis, high-value testing, and metacognition) with a simple scoring matrix that rates the learner’s degree of mastery on each component.34 The IDEA framework moves beyond observed assessments and instead evaluates the clinician’s written documentation for evidence of reasoning across four elements: interpretive summary, differential diagnosis, explanation of reasoning, and alternative diagnoses considered.35
Figure 2.
Steps and strategies for clinical reasoning (supplied also as a .tif file). Adapted from Bowen JL. Educational strategies to promote clinical diagnostic reasoning.N Engl J Med. 2006;355(21):2217–25.
Finally, the one-minute preceptor model offers a simple and time-efficient framework for formative assessment of clinical reasoning during short case presentations.36,37 Learners should develop the skills to synthesize all clinical clues from the history and physical examination, generate an appropriate differential diagnosis, and commit to the most likely diagnosis. Teachers can then pose questions exploring their learners’ skills in diagnostic hypothesis generation, investigative intent, and management planning, seeking their justifications for each. “Getting learners to make a commitment” requires “what” questions and “probing for supportive evidence” requires “how” or “why” questions. “Teaching general rules” assesses how well learners can compare and contrast similar presentations for different patients. Assessment is only meaningful when learners receive ongoing feedback on accuracy of their diagnostic reasoning processes and errors resulting from inappropriate use of non-analytic reasoning and this is achieved through “tell them what they did right” and “correct errors gently”. These steps are depicted in Table 4 in relation to corresponding steps of Bowen’s model with potential methods of assessment for each stage.
Table 4.
Clinical reasoning steps based on Bowen's model, potential methods of assessment for each step and corresponding one-minute preceptor strategies
| Clinical reasoning step from Bowen’s model | Potential assessment methods | Corresponding strategies from the one-minute preceptor model |
|---|---|---|
| Data acquisition | Direct observation of patient encounter to assess history taking and physical exam skills | |
| Case presentation: does the detailed presentation of history and physical exam contain important information? | ||
| Accurate problem representation | Direct observation: questions (pertinent positives and negatives) posed during history taking, targeted physical examination | Getting to a commitment |
| Case presentation: | ||
| -Organization of presentation | ||
| -Conciseness and accuracy of summary statement | ||
| Generation of hypothesis | Chart-stimulated recall | Probe for supportive evidence |
|
Case presentation: -Formulation of differential diagnosis linked to clinical data -Prioritization of diagnoses | ||
| Direct observation | ||
| -Questions posed to patients | ||
| -Targeted physical exam | ||
| Questioning to explore reasons for selection of differential diagnoses | ||
| Selection of illness scripts |
Chart-stimulated recall -Explanation of assessment and plans in case write ups |
Probe for supportive evidence |
|
Questioning -Assess application of clinical knowledge -Compare and contrast illness scripts developed by teachers |
Teach general rules | |
|
Think out loud -Steps taken to generate and narrow diagnostic hypotheses | ||
| Diagnosis |
Case presentation -Specific diagnosis reached |
Provide feedback |
|
Questioning -Narrow differential diagnosis |
-Tell learners about appropriate use of analytic and non-analytic reasoning -Gently point out errors |
CONCLUSIONS
This article describes a range of clinical reasoning assessment methods that clinical teachers can use across all four levels of Miller’s pyramid. Although this article has not focused on strategies to help address identified deficiencies in reasoning ability, other authors have developed helpful guidelines in this regard.38
As with all areas of assessment, no one level or assessment tool should take precedence and clinical teachers should be prepared and trained to assess from knowledge through to performance using multiple methods to gain a more accurate picture of their learners’ skills. The challenge of case specificity also requires teachers to repeatedly sample and test reasoning ability across different clinical contexts.
Clinical reasoning is a core skill that learners must master to develop accurate diagnostic hypotheses and provide high-quality patient care. It requires a strong knowledge base to allow learners to build illness scripts which can help expedite diagnostic hypothesis generation. As it is a critical step that synthesizes disparate data from history, physical examination, and investigations into a coherent and cogent clinical story, teachers cannot assume that their learners are applying sound reasoning skills when generating differential diagnoses or making management decisions. Enhancing the skills of clinical teachers in assessment across multiple levels of Miller’s pyramid, as well as recognizing and addressing cognitive biases, is therefore key in facilitating excellence in patient care.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
12/17/2019
In this perspective, we first introduce the concepts of illness scripts and dual-process theory that describe the roles of non-analytic system 1 and analytic system 2 reasoning in clinical decision making.
Contributor Information
Harish Thampy, Email: harish.thampy@manchester.ac.uk.
Emma Willert, Email: emma.willert@manchester.ac.uk.
Subha Ramani, Email: sramani@bwh.harvard.edu.
References
- 1.Higgs J, Jones M, Loftus S, Christensen N. Clinical Reasoning in the Health Professions. 3(rd) Edition. The Journal of Chiropractic Education. 2008;22(2):161–2.
- 2.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63–7. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 3.Charlin B, Tardif J, Boshuizen HP. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75(2):182–90. doi: 10.1097/00001888-200002000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022–8. doi: 10.1097/ACM.0b013e3181ace703. [DOI] [PubMed] [Google Scholar]
- 5.Croskerry P. From mindless to mindful practice--cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445–8. doi: 10.1056/NEJMp1303712. [DOI] [PubMed] [Google Scholar]
- 6.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775–80. doi: 10.1097/00001888-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Eva KW. What every teacher needs to know about clinical reasoning. Med Educ. 2005;39(1):98–106. doi: 10.1111/j.1365-2929.2004.01972.x. [DOI] [PubMed] [Google Scholar]
- 8.Harden RM. Preparation and presentation of patient-management problems (PMPs) Med Educ. 1983;17(4):256–76. [PubMed] [Google Scholar]
- 9.Norcini JJ, Swanson DB, Grosso LJ, Webster GD. Reliability, validity and efficiency of multiple choice question and patient management problem item formats in assessment of clinical competence. Med Educ. 1985;19(3):238–47. doi: 10.1111/j.1365-2923.1985.tb01314.x. [DOI] [PubMed] [Google Scholar]
- 10.Newble DI, Hoare J, Baxter A. Patient management problems. Issues of validity. Med Educ. 1982;16(3):137–42. doi: 10.1111/j.1365-2923.1982.tb01073.x. [DOI] [PubMed] [Google Scholar]
- 11.Charlin B, van der Vleuten C. Standardized assessment of reasoning in contexts of uncertainty: the script concordance approach. Eval Health Prof. 2004;27(3):304–19. doi: 10.1177/0163278704267043. [DOI] [PubMed] [Google Scholar]
- 12.Carriere B, Gagnon R, Charlin B, Downing S, Bordage G. Assessing clinical reasoning in pediatric emergency medicine: validity evidence for a Script Concordance Test. Ann Emerg Med. 2009;53(5):647–52. doi: 10.1016/j.annemergmed.2008.07.024. [DOI] [PubMed] [Google Scholar]
- 13.Piovezan RD, Custodio O, Cendoroglo MS, Batista NA, Lubarsky S, Charlin B. Assessment of undergraduate clinical reasoning in geriatric medicine: application of a script concordance test. J Am Geriatr Soc. 2012;60(10):1946–50. doi: 10.1111/j.1532-5415.2012.04152.x. [DOI] [PubMed] [Google Scholar]
- 14.Charlin B, Roy L, Brailovsky C, Goulet F, van der Vleuten C. The Script Concordance test: a tool to assess the reflective clinician. Teach Learn Med. 2000;12(4):189–95. doi: 10.1207/S15328015TLM1204_5. [DOI] [PubMed] [Google Scholar]
- 15.Brailovsky C, Charlin B, Beausoleil S, Cote S, Van der Vleuten C. Measurement of clinical reflective capacity early in training as a predictor of clinical reasoning performance at the end of residency: an experimental study on the script concordance test. Med Educ. 2001;35(5):430–6. doi: 10.1046/j.1365-2923.2001.00911.x. [DOI] [PubMed] [Google Scholar]
- 16.Hrynchak P, Takahashi SG, Nayer M. Key-feature questions for assessment of clinical reasoning: a literature review. Med Educ. 2014;48(9):870–83. doi: 10.1111/medu.12509. [DOI] [PubMed] [Google Scholar]
- 17.Wass V, Van der Vleuten C, Shatzer J, Jones R. Assessment of clinical competence. Lancet. 2001;357(9260):945–9. doi: 10.1016/S0140-6736(00)04221-5. [DOI] [PubMed] [Google Scholar]
- 18.Ber R. The CIP (comprehensive integrative puzzle) assessment method. Med Teach. 2003;25(2):171–6. doi: 10.1080/0142159031000092571. [DOI] [PubMed] [Google Scholar]
- 19.Capaldi VF, Durning SJ, Pangaro LN, Ber R. The clinical integrative puzzle for teaching and assessing clinical reasoning: preliminary feasibility, reliability, and validity evidence. Mil Med. 2015;180(4 Suppl):54–60. doi: 10.7205/MILMED-D-14-00564. [DOI] [PubMed] [Google Scholar]
- 20.Kunina-Habenicht O, Hautz WE, Knigge M, Spies C, Ahlers O. Assessing clinical reasoning (ASCLIRE): Instrument development and validation. Advances in health sciences education : theory and practice. 2015;20(5):1205–24. doi: 10.1007/s10459-015-9596-y. [DOI] [PubMed] [Google Scholar]
- 21.Hege I, Kononowicz AA, Adler M. A Clinical Reasoning Tool for Virtual Patients: Design-Based Research Study. JMIR medical education. 2017;3(2):e21. doi: 10.2196/mededu.8100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harden RM, Stevenson M, Downie WW, Wilson GM. Assessment of clinical competence using objective structured examination. Br Med J. 1975;1(5955):447–51. doi: 10.1136/bmj.1.5955.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yudkowsky R, Otaki J, Lowenstein T, Riddle J, Nishigori H, Bordage G. A hypothesis-driven physical examination learning and assessment procedure for medical students: initial validity evidence. Med Educ. 2009;43(8):729–40. doi: 10.1111/j.1365-2923.2009.03379.x. [DOI] [PubMed] [Google Scholar]
- 24.Durning SJ, Artino A, Boulet J, La Rochelle J, Van der Vleuten C, Arze B, et al. The feasibility, reliability, and validity of a post-encounter form for evaluating clinical reasoning. Med Teach. 2012;34(1):30–7. doi: 10.3109/0142159X.2011.590557. [DOI] [PubMed] [Google Scholar]
- 25.Berger AJ, Gillespie CC, Tewksbury LR, Overstreet IM, Tsai MC, Kalet AL, et al. Assessment of medical student clinical reasoning by “lay” vs physician raters: inter-rater reliability using a scoring guide in a multidisciplinary objective structured clinical examination. Am J Surg. 2012;203(1):81–6. doi: 10.1016/j.amjsurg.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Myung SJ, Kang SH, Phyo SR, Shin JS, Park WB. Effect of enhanced analytic reasoning on diagnostic accuracy: A randomized controlled study. Med Teach. 2013;35(3):248–50. doi: 10.3109/0142159X.2013.759643. [DOI] [PubMed] [Google Scholar]
- 27.Park WB, Kang SH, Lee Y-S, Myung SJ. Does Objective Structured Clinical Examinations Score Reflect the Clinical Reasoning Ability of Medical Students? The American Journal of the Medical Sciences. 2015;350(1):64–7. doi: 10.1097/MAJ.0000000000000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yudkowsky R, Park YS, Hyderi A, Bordage G. Characteristics and Implications of Diagnostic Justification Scores Based on the New Patient Note Format of the USMLE Step 2 CS Exam. Acad Med. 2015;90(11 Suppl):S56–62. doi: 10.1097/ACM.0000000000000900. [DOI] [PubMed] [Google Scholar]
- 29.Hodges B, McIlroy JH. Analytic global OSCE ratings are sensitive to level of training. Med Educ. 2003;37(11):1012–6. doi: 10.1046/j.1365-2923.2003.01674.x. [DOI] [PubMed] [Google Scholar]
- 30.Norman GR, Brooks LR, Allen SW. Recall by expert medical practitioners and novices as a record of processing attention. J Exp Psychol Learn Mem Cogn. 1989;15(6):1166–74. doi: 10.1037//0278-7393.15.6.1166. [DOI] [PubMed] [Google Scholar]
- 31.Haring CM, Cools BM, van Gurp PJM, van der Meer JWM, Postma CT. Observable phenomena that reveal medical students' clinical reasoning ability during expert assessment of their history taking: a qualitative study. BMC Med Educ. 2017;17(1):147. doi: 10.1186/s12909-017-0983-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ericsson KA. The Cambridge handbook of expertise and expert performance. 2. Cambridge: Cambridge University Press; 2018. p. 969. [Google Scholar]
- 33.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;355(21):2217–25. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 34.Society to Improve Diagnosis in Medicine. Assessment of Reasoning Tool [Available from: https://www.improvediagnosis.org/page/art. Accessed 1 Nov 2018
- 35.Baker EA, Ledford CH, Fogg L, Way DP, Park YS. The IDEA Assessment Tool: Assessing the Reporting, Diagnostic Reasoning, and Decision-Making Skills Demonstrated in Medical Students' Hospital Admission Notes. Teach Learn Med. 2015;27(2):163–73. doi: 10.1080/10401334.2015.1011654. [DOI] [PubMed] [Google Scholar]
- 36.Neher JO, Stevens NG. The one-minute preceptor: shaping the teaching conversation. Fam Med. 2003;35(6):391–3. [PubMed] [Google Scholar]
- 37.Neher JO, Gordon KC, Meyer B, Stevens N. A five-step “microskills” model of clinical teaching. J Am Board Fam Pract. 1992;5(4):419–24. [PubMed] [Google Scholar]
- 38.Audétat M-C, Laurin S, Sanche G, Béïque C, Fon NC, Blais J-G, et al. Clinical reasoning difficulties: A taxonomy for clinical teachers. Med Teach. 2013;35(3):e984–e9. doi: 10.3109/0142159X.2012.733041. [DOI] [PubMed] [Google Scholar]