Abstract
Background
Healthcare systems nationwide are implementing intensive outpatient care programs to optimize care for high-need patients; however, little is known about these patients’ personal goals and factors associated with goal progress.
Objective
To describe high-need patients’ goals, and to identify factors associated with their goal progress
Design
Retrospective cohort study
Participants
A total of 113 high-need patients participated in a single-site Veterans Affairs intensive outpatient care program.
Main Measures
Two independent reviewers examined patients’ goals recorded in the electronic health record, categorized each goal into one of three domains (medical, behavioral, or social), and determined whether patients attained goal progress during program participation. Logistic regression was used to determine factors associated with goal progress.
Results
The majority (n = 72, 64%) of the 113 patients attained goal progress. Among the 100 (88%) patients with at least one identified goal, 58 set goal(s) in the medical domain; 60 in the behavioral domain; and 52 in the social domain. Within each respective domain, 41 (71%) attained medical goal progress; 34 (57%) attained behavioral goal progress; and 32 (62%) attained social goal progress. Patients with mental health condition(s) (aOR 0.3; 95% CI 0.1–0.9; p = 0.03) and those living alone (aOR 0.4; 95% CI 0.1–1.0; p = 0.05) were less likely to attain goal progress. Those with mental health condition(s) and those who were living alone were least likely to attain goal progress (interaction aOR 0.1 compared to those with neither characteristic; 95% CI 0.0-0.7; p = 0.02).
Conclusions
Among high-need patients participating in an intensive outpatient care program, patient goals were fairly evenly distributed across medical, behavioral, and social domains. Notably, individuals living alone with mental health conditions were least likely to attain progress. Future care coordination interventions might incorporate strategies to address this gap, e.g., broader integration of behavioral and social service components.
Electronic supplementary material
The online version of this article (10.1007/s11606-019-05010-w) contains supplementary material, which is available to authorized users.
KEY WORDS: patient goal, patient-centered medical home, primary care redesign, Veterans
INTRODUCTION
The diverse medical, behavioral, and social challenges of high-need patients have driven demand for effective care coordination interventions. Intensive outpatient care programs (IOCPs) are one model,1–4 typically offering team-based intensive case management and individualized medical, mental health (MH), and social services.5
In recent years, the National Academy of Medicine (NAM),6 Patient-Centered Outcomes Research Institute,7 and others8, 9 have identified matching care with patients’ preferences and goals as a core attribute to effective care coordination interventions. Understanding and supporting personal goals may be an important strategy to engage high-need patients.10, 11 Despite growing literature on patient preferences for end-of-life,12–15 home care,16 and specific diseases,17 there is a gap in research regarding high-need patients’ goals and their progress within care coordination interventions. Studies on IOCPs1, 2 have examined clinical outcomes, utilization, and costs, yet to our knowledge, no study has explicitly examined IOCP patients’ goals and factors associated with their progress.
To bridge this gap, we evaluated the goals of high-need patients enrolled in a Veterans Affairs (VA) IOCP1, 18 and characteristics associated with goal progress. Previous evaluations found that, at 16 months, the program was cost-neutral with positive effects on patient experience, continuity and access, and end-of-life care.1, 19, 20 Based on literature describing characteristics common among high-need patients,21 we anticipated that lower level of multimorbidity (e.g., no MH diagnosis, fewer chronic medical conditions) and less social isolation and social needs (e.g., living with others, no history of homelessness, health insured) would be associated with goal progress.
METHODS
Intervention and Patient Population
The Palo Alto VA (PAVA) implemented an IOCP in 2012 to augment its patient-centered medical home, also known as Patient Aligned Care Teams (PACT), with an intensive management (ImPACT) team. Beginning in February 2013, outpatients were eligible for enrollment if their total VA healthcare costs in the 16-month baseline period were in the top 5% for the facility, or their 1-year hospitalization risk was in the top 5% (based on the VA’s Care Assessment Need risk-prediction algorithm).22 Patients were excluded if they were in another intensive outpatient VA program, or in the lowest cost or risk quartile.1 Beginning in April 2014, the program modified eligibility criteria to focus on patients with a 1-year hospitalization risk in the top 10% and medical-surgical hospitalization within the previous 6 months.
Although the primary purpose of an ImPACT intake visit was to build rapport and to understand a patient’s medical and social challenges, each team member (i.e., nurse practitioner, physician, social worker, recreation therapist) was also trained to elicit and record patients’ goals during the intake. Team members used open-ended questions derived from trainings, e.g., VA Whole Health Coaching Course23 and ImPACT protocols. During subsequent encounters, the team regularly assessed patients’ readiness for change and followed up on their goal progress using motivational interviewing and health coaching techniques. When patients reached program completion, the team used a discharge note template to indicate whether they had progressed toward their goals during program enrollment.
Given limited program resources, 250 of 783 eligible patients were invited to participate in ImPACT using simple random sampling without replacement between 2013 and 2015. Among those invited, 165 (66%) initially engaged in the program. We excluded patients still enrolled in ImPACT as of June 1, 2017 (n = 25), and patients who transferred care less than 30 days after enrollment (n = 3). We also excluded patients who died during program engagement (n = 24) from primary analyses due to the challenge of ascertaining their goal progress from chart review; instead, we present examples of these patients’ goals separately in the Online Appendix. These criteria resulted in a study cohort of 113 high-need patients who reached program completion (defined as meeting graduation criteria, transitioned to another program and/or geographic location, or discharged due to lack of interest or perceived non-benefit). Online Appendix Fig. 1 summarizes patient enrollment and program completion.
Previous evaluations1, 19, 20 describe the ImPACT intervention in further detail, and Online Appendix Box 1 provides additional information regarding the intervention’s core elements.
Assessment of Patients’ Goals
One reviewer (KH) conducted conventional content analysis24 to develop an initial set of codes representing common patients’ goals by preliminarily reviewing ImPACT electronic health record (EHR) notes that described patients’ goals. Two others (DZ, AT) conducted content analysis with the initial codebook and identified new codes to add to the coding scheme. Next, we identified three domains (medical, behavioral, social) to encompass patients’ goals based on the literature, including a biopsychosocial framework of high-need patient health determinants.6, 25 We categorized goal codes pertaining to a patient’s medical status and medical system determinants in the medical domain; self-management and MH needs in the behavioral domain; and social connectedness and support (including goals related to housing and transportation, work, education, travel, and socializing) in the social domain.
Two individuals (KH, AT) then independently reviewed program EHR notes that described the personal goals of each patient and their progress, and assigned each goal to one of the three domains and specific goal codes (n = 212 goals; kappa = 0.82); disagreements were resolved by discussion-based consensus between the two reviewers. Next, they determined (from care plan updates and discharge notes) whether a patient attained any progress toward each goal during program participation (n = 212 goals; kappa = 0.62); disagreements (n = 37 goals) were reviewed by a third reviewer (CS) and resolved by clinician-lead consensus (DZ, KH, AT, CS). Goals for which group consensus on goal progress could not be reached were removed from analysis (n = 4).
Data Collection
Sociodemographic, clinical, and utilization data were obtained from PAVA’s Managerial Cost Accounting office. Insurance status, mortality, and utilization data for VA-reimbursed care outside the facility were obtained from PAVA’s Office of Business Analytics. History of homelessness was identified through the ICD-9 code 60.0. Marital status (married or not married) and living alone (living alone or co-habitating with one or more individuals) were documented by the ImPACT team at time of program enrollment; these variables and mortality status were extracted from EHR by one reviewer (KH) in June 2017.
Chronic medical and MH conditions were identified using ICD-9 codes that were documented at least once in inpatient or outpatient encounters during the 16-month baseline period prior to IOCP enrollment. We used these codes to calculate the number of chronic medical conditions (Online Appendix Table 1) and to evaluate the presence of MH condition diagnoses (Online Appendix Table 2).
Statistical Analysis
Among patients with one or more goals recorded in the EHR, we assessed the proportion who set at least one goal within each domain. Of those who set goal(s) within a given domain, we examined the proportion who attained any goal progress within that domain. We conducted bivariate chi-square tests to compare the proportions of goal progress in each domain.
Our primary outcome variable was goal progress during IOCP participation as documented at time of program completion. We compared patients with goal progress in at least one goal domain to those without goal progress in any goal domains. Patients without identified goals (n = 13) were considered to be without goal progress for all analyses given that they completed the program without setting goals and attaining goal progress.
We examined patient characteristics associated with goal progress including sociodemographic (age, sex, race/ethnicity, insurance status, marital status, living arrangement, history of homelessness), baseline acute care use (emergency department visits, medical-surgical hospitalizations), clinical (burden of chronic medical conditions, one or more MH conditions), and program enrollment characteristics (enrollment after modified eligibility criteria in April 2014, years in program).
We first examined unadjusted bivariate associations between patient characteristics and goal progress, using t tests for continuous variables (age, emergency department visits, hospitalizations, burden of chronic medical conditions, years in program) and chi-square tests for categorical variables (sex, race/ethnicity, insurance status, marital status, living arrangement, ≥ 1 MH condition, enrollment after April 2014). Next, we conducted logistic regression to determine whether any characteristics were individually associated with overall goal progress after adjusting for all other characteristics. We then tested interactions one at a time for each pair of variables that had significant main effects. We used the variance inflation factor (VIF) to test for collinearity.26
In sensitivity analyses, we repeated fully adjusted logistic regression, but excluding patients without identified goals, with the rationale that choosing not to set goals during program participation may be distinct from setting goals and not attaining progress. Next, we repeated fully adjusted logistic regression separately for each goal domain to determine if any characteristics were individually associated with medical, behavioral, or social goal progress, respectively, with the rationale that predictors of goal progress might differ among the three domains.
In separate sensitivity analyses, we explored MH conditions more granularly by conducting bivariate chi-square tests to examine associations between specific MH condition diagnoses and goal progress. Lastly, we assessed patients’ goals among those who died (n = 24) during program engagement. Given the small sample size, we did not perform further statistical analysis.
All analyses were performed using Stata 14.0. Study procedures were approved by the Stanford University Institutional Review Board and PAVA Research & Development Committee.
RESULTS
Assessment of Patients’ Goals
Among 113 patients who completed ImPACT, 100 (88%) had one or more goals recorded in the EHR. Table 1 presents patients’ goals categorized by domain and goal code with specific examples extracted during chart review. Among the 100 patients with identified goal(s) upon program completion, 58 set goal(s) in the medical domain; 60 in the behavioral domain; and 52 in the social domain. Within each domain, 41 (71%) attained medical goal progress; 34 (57%) attained behavioral goal progress; and 32 (62%) attained social goal progress. There were no significant differences in the proportion of patients who made progress across different goal domains (medical vs. behavioral: p value = 0.11; medical vs. social: p value = 0.31; behavioral vs. social: p value = 0.60). Figure 1 illustrates the proportion of patients who identified goals in one, two, or all domains.
Table 1.
Patient Goal Domains by Subtype and Examples
| Goal domain and subtype | Specific patient goal examples |
|---|---|
| Medical | |
| Obtain specific health treatment (e.g., surgery, manage pain symptoms) | “Get cataract surgery” |
| “Improve hip and back pain” | |
| “Lower my A1C < 8” | |
| Manage medications | “Get off unnecessary meds” |
| “Help understanding supplements” | |
| Coordinate care (i.e., among specialists, or with move/care transfer) | “Change PCP [primary care physician]” |
| “Transition care to [another setting]” | |
| Maintain general health | “Live another year and be healthy” |
| “Maintain my health and wellbeing” | |
| Behavioral | |
| Manage weight | “I want to be under 200 pounds” |
| “Lose 10 pounds” | |
| Increase physical and/or recreational activity | “Walk 2× daily” |
| “Ride a bike” | |
| “Get physically conditioned” | |
| Quit substance, tobacco, and/or caffeine use | “Get back on my feet and stay clean and sober” |
| “I want to quit smoking” | |
| Address mental health challenges | “Manage anxiety related to retirement and cardiac conditions” |
| “Manage symptoms of depression” | |
| Social | |
| Obtain social services (e.g., financial, transportation, home assistance needs, housing) | “Get driver’s license and car” |
| “Get off the streets” | |
| “Renew food stamps” | |
| “Get more help at home” | |
| Achieve work or educational goals (e.g., enter new career, obtain academic degree) | “Complete associate’s degree in computer science” |
| “Get a real estate license” | |
| “Become a recreation therapist” | |
| “Become a pilot” | |
| Strengthen social network (e.g., socialize more often, find new partner) | “Increase social activities” |
| “Restart dating” | |
| Travel | “Plan a trip to New Orleans” |
| “Sail around the world” | |
n = 100 patients who reached ImPACT program completion with ≥ 1 identified goal
Fig. 1.
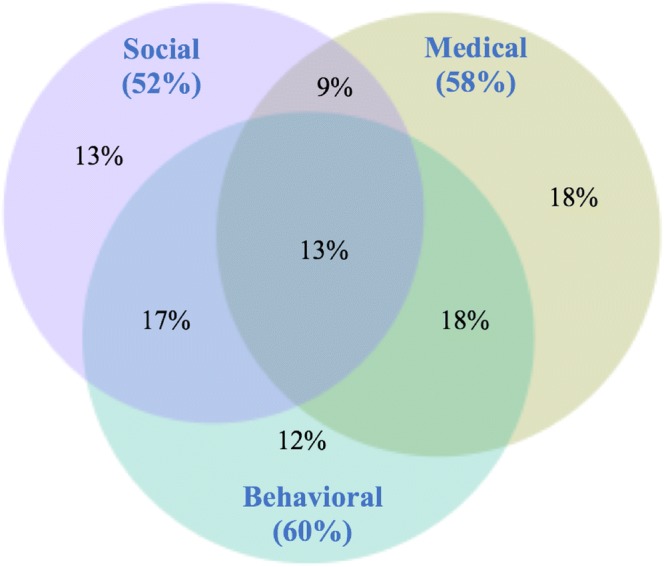
Patients with goals recorded in one, two, or three domains (n = 100 patients who reached ImPACT program completion with ≥ 1 identified goal).
Patient Characteristics Associated with Goal Progress
Over half (n = 72, 64%) of the 113 patients in the cohort attained goal progress. Table 2 describes the association between patient characteristics and goal progress. In unadjusted analyses, there were no significant associations between goal progress and any characteristics. Logistic regression demonstrated that patients with ≥ 1 MH conditions (aOR 0.3; 95% CI 0.1–0.9; p = 0.03) and those who lived alone (aOR 0.4; 95% CI 0.1–1.0; p = 0.05) were less likely to attain progress. There was no evidence for multicollinearity (VIF < 2).
Table 2.
Patient Characteristics Associated with Goal Progress
| Characteristic | Total population (n = 113) | With goal progress (n = 72) | Without goal progress (n = 41) | ||
|---|---|---|---|---|---|
| Sociodemographics | n(%) | n(%) | n(%) | Unadjusted p value* | aOR (95% CI)† |
| Age, mean (SD) | 67.0(12.4) | 66.6(12.7) | 67.6(11.9) | 0.68 | 1.0 (0.9–1.0) |
| Male sex | 102(90) | 64(89) | 38(93) | 0.12 | 1.1 (0.2–5.3) |
| White, non-Hispanic‡ | 63(56) | 39(54) | 24(59) | 0.65 | 1.0 (0.4–2.3) |
| Married | 28(25) | 16(22) | 12(29) | 0.40 | 0.3 (0.1–1.1) |
| Living alone | 50(44) | 29(40) | 21(51) | 0.26 | 0.3 (0.1–1.0)** |
| Housing instability | 30(27) | 21(29) | 9(22) | 0.40 | 1.9 (0.6–5.8) |
| Any health insurance§ | 58(52) | 32(45) | 26(63) | 0.06 | 0.6 (0.2–1.5) |
| Baseline acute care use|| | |||||
| Emergency dept visits, mean (SD) | 2.6(3.1) | 2.4(2.7) | 3.0(3.7) | 0.39 | 1.0 (0.8–1.1) |
| Acute med/surg hosps, mean (SD) | 0.8(0.7) | 0.8(0.7) | 1.0(0.7) | 0.24 | 0.7 (0.3–1.5) |
| Chronic medical, mental health conds | |||||
| No. of chronic medical conds, mean (SD) | 10.0(4.7) | 9.6(4.9) | 10.7(4.1) | 0.26 | 1.0 (0.9–1.1) 0.3 |
| ≥ 1 Mental health condition | 73(65) | 42(58) | 31(76) | 0.07 | (0.1–0.9)** |
| Program enrollment | |||||
| Enrollment after April 2014†† | 45(40) | 28(39) | 17(42) | 0.07 | 0.7 (0.2–2.1) |
| Years in program, mean (SD) | 1.7(0.9) | 1.6(0.9) | 1.7(0.9) | 0.82 | 0.9 (0.5–1.6) |
n = 113 high-need patients who reached ImPACT program completion
*Unadjusted p values determined by t tests for continuous variables and chi-square tests for categorical variables
†Adjusted odds ratios determined by full multiple logistic regression model adjusted for all sociodemographic, baseline care use, chronic medical and mental health conditions, and program enrollment characteristics
‡White, non-Hispanic versus all other white, Hispanic and all non-white race report
§Insurance status missing for n = 1
|| Baseline period defined as 16 months prior to IOCP enrollment
¶Chronic medical and mental health conditions included in Online Appendix Tables 1 and 2, respectively
** p value ≤ 0.05
††Program eligibility criteria before April 2014: top 5% based on total costs or 1-year risk of hospitalization; after April 2014: top 10% based on 1-year risk of hospitalization and hospitalization within previous 6 months
When we examined the interaction between ≥ 1 MH condition and living alone, fully adjusted logistic regression demonstrated that those living alone with ≥ 1 MH condition were least likely to attain progress (aOR 0.1; 95% CI 0.0–0.7; p = 0.02). However, those who lived alone with no MH condition and those co-habitating with ≥ 1 MH condition were not significantly different from those co-habitating with no MH condition (Table 3).
Table 3.
Association of Interaction (Between ≥ 1 Mental Health Condition and Living Alone) with Goal Progress
| Multilevel (MH and living status) | n | aOR* | 95% CI | p value |
|---|---|---|---|---|
| MH + | lives alone | 34 | 0.1 | 0.0–0.7 | 0.02 |
| MH + | co-habitates | 39 | 0.8 | 0.2–3.1 | 0.8 |
| No MH | lives alone | 16 | 2.4 | 0.3–17.2 | 0.4 |
| No MH | co-habitates | 24 | 1 | Reference | Reference |
*Adjusted odds ratios determined by a full multiple logistic regression model adjusted for all sociodemographic, baseline care use, chronic medical and mental health conditions, and program enrollment characteristics
In sensitivity analyses, repeating fully adjusted logistic regression, but excluding patients without identified goal(s) upon program completion (Online Appendix Table 3), the presence of ≥ 1 MH condition continued to show significant association (aOR 0.3, p = 0.05). Living alone did not show significant association with goal progress, though the estimated effect was in the direction of reduced likelihood (aOR 0.5, p = 0.2), as in the main model.
Repeating fully adjusted logistic regression, but for each domain separately (Online Appendix Tables 4, 5, and 6), the presence of ≥ 1 MH condition was not significantly associated with goal progress in any of the models; for all three, however, the estimated effects were in the direction of reduced likelihood of progress as in the main model (aORs ranging 0.2 to 0.7). Living alone showed a statistically significant inverse association with the likelihood of progress in the social domain (aOR 0.1; p = 0.04), but was not associated with progress in the other two domains, where directions of the estimates were in the opposite direction (aOR 1.3; p = 0.8 for medical goal progress; aOR 1.4; p = 0.6 for behavioral goal progress). Within the behavioral domain, a new association emerged: white, non-Hispanic individuals were significantly most likely to make progress toward behavioral goals (aOR 4.8 compared to all other race/ethnicities; p = 0.03).
In analyses examining MH conditions more granularly, the most common MH condition among the cohort was major depressive disorder. Chi-square testing demonstrated that only schizophrenia or other psychoses was statistically significantly associated with lower likelihood (p = 0.01) of progress (Online Appendix Table 2).
Patients’ Goals Among a Subset of Deceased Participants
Among 24 patients who died during IOCP engagement, 20 (83%) had goal(s) recorded in the EHR; 8 (40%) identified goal(s) in the medical domain; 9 (45%) in the behavioral domain; and 15 (75%) in the social domain. Many of these patients’ goals related to quality of life (examples in Online Appendix Table 7).
DISCUSSION
Healthcare models for high-need patients increasingly emphasize patient preferences, and while many IOCPs have developed methods for tracking patients’ goals,6, 27, 28 there is still much to be understood about what predicts high-need patients’ goal progress. This evaluation provides a framework for considering goal domains and progress among high-need patients enrolled in specialized programs. We found that, among IOCP participants, patient goals were fairly evenly distributed across medical, behavioral, and social domains. Notably, individuals with MH conditions who were living alone were least likely to attain goal progress. Our findings demonstrate the breadth of patient-initiated goals across all three domains and suggest that there is room to optimize IOCPs to better address patients’ sociobehavioral priorities.
This paper builds on prior literature describing the value of assessing patients’ goals near end-of-life12, 29–32 and exploring associations among living arrangement, MH status, and health outcomes.33–38 Assessments of end-of-life goals have found that hospice patients most often set goals to control end-of-life medical symptoms12 and to be cured.32 We found that while many high-need Veterans in the ImPACT program set goals related to their medical status, a similar proportion also set behavioral and social goals, which may speak to the multidimensional needs of this population.
Although in unadjusted analyses, living alone and the presence of a MH condition were not significantly associated with goal progress, logistic regression revealed significant associations with less likelihood of goal progress. Exploratory analyses revealed a significant interaction between living alone and MH status, suggesting that the combination of these factors was associated with a much lower likelihood of making progress toward goals. While no extant literature has explicitly examined the relationship among living arrangement, MH status, and goal completion, there is evidence that individuals who live alone, particularly men, may be more likely to engage in substance use,33 have anxiety or depressive disorders,34 and suffer higher rates of morbidity35 and mortality.36–38 Our finding provides further evidence that patients with MH conditions who live alone may require additional support to help them make progress toward their goals.
Our work suggests that IOCPs should consider how patients’ sociobehavioral challenges intersect and affect goal completion, and develop explicit strategies to address them. The impact of living alone on MH, particularly for depression, may be strongly mediated by the presence of social support; Joutsenniemi et al. (2006) found significantly reduced MH problems from living alone when individuals had emotional or practical support from another person.34 One strategy among IOCPs may be to better integrate family members and social networks in patient care,39 as they can provide significant emotional and practical support (e.g., some goals may be easier to execute with someone at home helping) for patients’ goals.
Another strategy may be to expand IOCP behavioral and social service components to be even more robust, perhaps at a level that compares to traditional medical services. For example, while the ImPACT team had a social worker (tasked to address social, behavioral, and medical social work needs), it lacked a MH specialist and might have benefitted from dedicated behavioral health personnel. The National Academy of medicine recommends interventions for high-need patients interventions to integrate social and community services that are not typically the province of medical teams6; this may improve an intervention’s ability to fully address high-need patients’ goals, although an upstream strategy may also be necessary to remove system-level barriers that segregate sociobehavioral health services from other insured medical services.40
Finally, our findings may also reflect that the ImPACT program intentionally asked open-ended questions allowing patients to discuss any goals important to them. This approach may have resulted in goals that the program was not able to support (e.g., “go to Paris”). At the same time, allowing patients the freedom to discuss the goals most important to them can be helpful in better understanding what motivates them and developing patient–provider relationships. Taking this into consideration, programs may want to complement, though not substitute, open-ended goal assessments with a process encouraging patients to identify actionable goals that the team can support. Setting specific, measurable, achievable, relevant, and time-bound goals through action planning is one method that has been associated with improved health and self-efficacy outcomes.41, 42
There are several limitations to this study. First, our data derive from a single-setting study and may not be generalizable to other health systems. Given the VA’s social mission and available sociobehavioral services, the ImPACT program may have been better equipped to support patients’ behavioral and social goals than programs in other settings. Next, we did not control for variability among goal recording by the authors of the EHR notes describing goal attainment. Finally, we were unable to account for other potential factors associated with goal progress, such as physical function or self-rated general health; future programs may consider implementing protocols that incorporate patient-reported health characteristics.
As innovative healthcare models develop nationwide to enhance care for high-need patients, a major challenge is to understand the goals common among their patient populations and to design resources that could fully support them. Care coordination interventions are well positioned to address patient priorities across medical, behavioral, and social domains. This study highlights that to support patient-centered goals, interventions must address all three domains; it also offers a framework for evaluating patients’ goals and goal progress that can inform strategies to engage high-need patients across their spectrum of goals.
Electronic supplementary material
(DOCX 342 kb)
Acknowledgments
The authors would like to acknowledge Josephine Jacobs, PhD, Ms. Georgezetta Rogers, and Ms. Kathryn Holloway, for their meaningful contributions to this study. Views expressed are those of the authors and not necessarily those of the Department of Veterans Affairs.
Prior Presentations
This work was previously presented on January 20, 2018, at the SGIM California-Hawaii regional meeting, on April 13, 2018, at the national SGIM meeting as an oral presentation, and on June 25, 2018, at the Academy Health Annual Research Meeting.
Funders
Ms. Hsu was supported by a MedScholars grant from Stanford University School of Medicine. Dr. Zulman is supported by VA HSR&D Career Development Award (CDA 12-173). The ImPACT program was developed and evaluated with support from the VA Office of Specialty Care Transformation (Specialty/Surgical Care Neighborhood Team Based Model Pilot Program) and by VA HSR&D (PPO 13-117).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zulman DM, Pal Chee C, Ezeji-Okoye SC, Shaw JG, Holmes TH, Kahn JS, et al. Effect of an Intensive Outpatient Program to Augment Primary Care for High-Need Veterans Affairs Patients: A Randomized Clinical Trial. JAMA Intern Med. 2017;177(2):166–75. doi: 10.1001/jamainternmed.2016.8021. [DOI] [PubMed] [Google Scholar]
- 2.Boult C, Reider L, Leff B, Frick KD, Boyd CM, Wolff JL, et al. The effect of guided care teams on the use of health services: results from a cluster-randomized controlled trial. Arch Intern Med. 2011;171(5):460–6. doi: 10.1001/archinternmed.2010.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schubert CC, Myers LJ, Allen K, Counsell SR. Implementing Geriatric Resources for Assessment and Care of Elders Team Care in a Veterans Affairs Medical Center: Lessons Learned and Effects Observed. J Am Geriatr Soc. 2016;64(7):1503–9. doi: 10.1111/jgs.14179. [DOI] [PubMed] [Google Scholar]
- 4.Hochman M, Asch SM. Disruptive Models in Primary Care: Caring for High-Needs, High-Cost Populations. J Gen Intern Med. 2017;32(4):392–7. doi: 10.1007/s11606-016-3945-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stremikis K, Connors C, Hoo E. Intensive Outpatient Care Program: A Care Model for the Medically Complex Piloted by Employers. 2017.
- 6.Long P, Abrams M, Milstein A, Anderson G, Apton KL, Dahlberg ML, Whicher D. Effective Care for High-Need Patients: Opportunities for Improving Outcomes, Value, and Health. NAM Special Publication; 2017. [PubMed]
- 7.Blaum C, Tinetti M, Rich MW, Hoy L, Hoy S, Esterson J, et al. A Research Agenda to Support Patient Priorities Care for Adults with Multiple Chronic Conditions. Patient-Centered Outcomes Research Institute New York University School of Medicine Yale University School of Medicine; 2017.
- 8.McCarthy D, Ryan J, Klein S. Models of Care for High-Need, High-Cost Patients: An Evidence Synthesis. Issue Brief (Commonw Fund). 2015;31:1–19. [PubMed] [Google Scholar]
- 9.Boult C, Wieland GD. Comprehensive primary care for older patients with multiple chronic conditions: “Nobody rushes you through”. JAMA. 2010;304(17):1936–43. doi: 10.1001/jama.2010.1623. [DOI] [PubMed] [Google Scholar]
- 10.Reuben DB, Tinetti ME. Goal-oriented patient care--an alternative health outcomes paradigm. N Engl J Med. 2012;366(9):777–9. doi: 10.1056/NEJMp1113631. [DOI] [PubMed] [Google Scholar]
- 11.Edwards ST, Dorr DA, Landon BE. Can Personalized Care Planning Improve Primary Care? JAMA. 2017;318(1):25–6. doi: 10.1001/jama.2017.6953. [DOI] [PubMed] [Google Scholar]
- 12.Kumar G, Markert RJ, Patel R. Assessment of hospice patients’ goals of care at the end of life. Am J Hosp Palliat Care. 2011;28(1):31–4. doi: 10.1177/1049909110371469. [DOI] [PubMed] [Google Scholar]
- 13.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284(19):2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 14.Cleary PD, Edgman-Levitan S. Health care quality. Incorporating consumer perspectives. JAMA. 1997;278(19):1608–12. doi: 10.1001/jama.1997.03550190072047. [DOI] [PubMed] [Google Scholar]
- 15.Wensing M, Elwyn G. Methods for incorporating patients’ views in health care. BMJ. 2003;326(7394):877–9. doi: 10.1136/bmj.326.7394.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sockolow P, Radhakrishnan K, Chou EY, Wojciechowicz C. Patient Health Goals Elicited During Home Care Admission: A Categorization. West J Nurs Res. 2017;39(11):1447–58. doi: 10.1177/0193945916676541. [DOI] [PubMed] [Google Scholar]
- 17.Hulen E, Ervin A, Schue A, Evans-Young G, Saha S, Yelin EH, et al. Patient goals in rheumatoid arthritis care: A systematic review and qualitative synthesis. Musculoskeletal Care. 2016. 10.1002/msc.1173. [DOI] [PMC free article] [PubMed]
- 18.Chang ET, Raja PV, Stockdale SE, Katz ML, Zulman DM, Eng JA, et al., eds. What are the key elements for implementing intensive primary care? A multisite Veterans Health Administration case study. Healthcare: Elsevier; 2017. [DOI] [PubMed]
- 19.Hummel DL, Hill C, Shaw JG, Slightam C, Asch SM, Zulman DM. Nurse Practitioner− led Intensive Outpatient Team: Effects on End-of-life Care. J Nurse Pract. 2017;13(5):e245–e8. doi: 10.1016/j.nurpra.2017.01.007. [DOI] [Google Scholar]
- 20.Wu FM, Slightam CA, Wong AC, Asch SM, Zulman DM. Intensive Outpatient Program Effects on High-need Patients’ Access, Continuity, Coordination, and Engagement. Med Care. 2017. 10.1097/MLR.0000000000000833. [DOI] [PubMed]
- 21.Ryan J, Abrams MK, Doty MM, Shah T, Schneider EC. How High-Need Patients Experience Health Care in the United States. Findings from the 2016 Commonwealth Fund Survey of High-Need Patients. Issue Brief (Commonw Fund). 2016;43:1–20. [PubMed] [Google Scholar]
- 22.Wang L, Porter B, Maynard C, Evans G, Bryson C, Sun H, et al. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368–73. doi: 10.1097/MLR.0b013e31827da95a. [DOI] [PubMed] [Google Scholar]
- 23.The Radical Redesign of Health Care. Partnering with Veterans for their Greatest Health and Well-Being. U.S. Department of Veterans Affairs; 2017:22-4.
- 24.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 25.California Healthcare Foundation CQC. Complex Care Management Toolkit. 2012 [01/24/19]. Available from: http://www.calquality.org/storage/documents/cqc_complexcaremanagement_toolkit_final.pdf.
- 26.O’brien RM. Caution regarding rules of thumb for variance inflation factors. Qual Quant. 2006;41:673–90. doi: 10.1007/s11135-006-9018-6. [DOI] [Google Scholar]
- 27.Lynn J, McKethan A, Jha AK. Value-Based Payments Require Valuing What Matters to Patients. JAMA. 2015;314(14):1445–6. doi: 10.1001/jama.2015.8909. [DOI] [PubMed] [Google Scholar]
- 28.Edwards ST, Peterson K, Chan B, Anderson J, Helfand M. Effectiveness of Intensive Primary Care Interventions: A Systematic Review. J Gen Intern Med. 2017. 10.1007/s11606-017-4174-z. [DOI] [PMC free article] [PubMed]
- 29.Good care of the dying patient Council on Scientific Affairs, American Medical Association. JAMA. 1996;275(6):474–8. doi: 10.1001/jama.1996.03530300058041. [DOI] [PubMed] [Google Scholar]
- 30.Lynn J. Measuring quality of care at the end of life: a statement of principles. J Am Geriatr Soc. 1997;45(4):526–7. doi: 10.1111/j.1532-5415.1997.tb05176.x. [DOI] [PubMed] [Google Scholar]
- 31.Sachs GA, Ahronheim JC, Rhymes JA, Volicer L, Lynn J. Good care of dying patients: the alternative to physician-assisted suicide and euthanasia. J Am Geriatr Soc. 1995;43(5):553–62. doi: 10.1111/j.1532-5415.1995.tb06106.x. [DOI] [PubMed] [Google Scholar]
- 32.Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Med. 2009;25(6):501–11. doi: 10.1177/1049909108328256. [DOI] [PubMed] [Google Scholar]
- 33.Hughes M, Gove WR. Living alone, social integration, and mental health. AJS. 1981;87(1):48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- 34.Joutsenniemi K, Martelin T, Martikainen P, Pirkola S, Koskinen S. Living arrangements and mental health in Finland. J Epidemiol Community Health. 2006;60(6):468–75. doi: 10.1136/jech.2005.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joung IM, Van de Mheen H, Stronks K, van Poppel FW, Mackenbach JP. Differences in self-reported morbidity by marital status and by living arrangement. Int J Epidemiol. 1994;23(1):91–7. doi: 10.1093/ije/23.1.91. [DOI] [PubMed] [Google Scholar]
- 36.Lund R, Due P, Modvig J, Holstein BE, Damsgaard MT, Andersen PK. Cohabitation and marital status as predictors of mortality--an eight year follow-up study. Soc Sci Med. 2002;55(4):673–9. doi: 10.1016/S0277-9536(01)00219-2. [DOI] [PubMed] [Google Scholar]
- 37.Davis MA, Neuhaus JM, Moritz DJ, Segal MR. Living arrangements and survival among middle-aged and older adults in the NHANES I epidemiologic follow-up study. Am J Public Health. 1992;82(3):401–6. doi: 10.2105/AJPH.82.3.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Helsing KJ, Szklo M, Comstock GW. Factors associated with mortality after widowhood. Am J Public Health. 1981;71(8):802–9. doi: 10.2105/AJPH.71.8.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Asch DA, Rosin R. Engineering Social Incentives for Health. N Engl J Med. 2016;375(26):2511–3. doi: 10.1056/NEJMp1603978. [DOI] [PubMed] [Google Scholar]
- 40.Bachrach D, Anthony S, Detty A, Manatt P, Phillips L. State strategies for integrating physical and behavioral health services in a changing Medicaid environment. The Commonwealth Fund; 2014.
- 41.Lorig K, Laurent DD, Plant K, Krishnan E, Ritter PL. The components of action planning and their associations with behavior and health outcomes. Chronic Illn. 2014;10(1):50–9. doi: 10.1177/1742395313495572. [DOI] [PubMed] [Google Scholar]
- 42.Kersten P, McCambridge A, Kayes MN, Theadom A, KM MP. Bridging the gap between goal intentions and actions: a systematic review in patient populations. Disabil Rehabil. 2015;37(7):563–70. doi: 10.3109/09638288.2014.935874. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 342 kb)


