Abstract
Purpose
Trauma is well known as one of the main causes of death and disability throughout the world. Identifying the risk factors for mortality in trauma patients can significantly improve the quality of care and patient outcomes, as well as reducing mortality rates.
Methods
In this retrospective cohort study, systematic randomization was used to select 849 patients referred to the main trauma center of south of Iran during a period of six months (February 2017–July 2017); the patients’ case files were evaluated in terms of demographic information, pre- and post-accident conditions, clinical conditions at the time of admission and finally, accident outcomes. A logistic regression model was used to analyze the role of factors affecting mortality among subjects.
Results
Among subjects, 60.4% were in the age-group of 15–39 years. There was a 10.4% mortality rate among patients and motor-vehicle accidents were the most common mechanism of injury (66.7%). Aging led to increased risk of fatality in this study. For each unit increase in Glasgow coma scale (GCS), risk of death decreased by about 40% (odds ratio (OR) = 0.63, 95% confidence interval (CI): 0.59–0.67). For each unit increase in injury severe score (ISS), risk of death increased by 10% (OR = 1.11%, 95% CI: 1.08–1.14) and for each unit increase in trauma revised injury severity score (TRISS), there was 18% decrease in the risk of fatality (OR = 0.82, 95% CI: 0.71–0.88).
Conclusion
The most common cause of trauma and the most common cause of death from trauma was traffic accidents. It was also found that an increase in the ISS index increases the risk of death in trauma patients, but the increase in GCS, revised trauma score (RTS) and TRISS indices reduces the risk of death in trauma patients. The TRISS indicator is better predictor of traumatic death than other indicators.
Keywords: Risk factor, Fetal mortality, Wounds and injuries
Introduction
In medical sciences, any type of strike, wound, shock, injury or accident to the human body is referred to as trauma, in the condition that it has an external cause and isn't resulted by internal factors such as disease.1, 2 The mechanisms of traumatic injury include a wide range of blunt trauma (non-penetrating trauma), penetrating trauma and burns caused by motor-vehicle collisions, sports injuries, falls from heights, natural disasters and other types of physical injury leading to immediate medical intervention.3
Trauma is known as a worldwide cause of death and disability for decades now.4, 5, 6 Our country has the leading rank for frequency of trauma cases in the Middle East.7 In an Iranian study in 2000–2001 on a population of 16,470,673 patients, 66,864 (58/100,000) deaths were reported, out of which 9733 were caused by traumatic accidents, forming 14.9% of all fatalities. With 30 deaths per each 100,000 cases, Iran has the highest rate of road-traffic fatalities in the world.8
Trauma burdens the society with a lot of direct and indirect socioeconomic costs.9 This has pushed policy-makers and healthcare officials to take fundamental measures in this relation. Nowadays, government policies are formed in accordance with preventive measures, as well as the healthcare needs of patients; these policies have led to reduced mortality rates, full recovery of patients with severe injuries and reduced socioeconomic burden in various countries.2, 10, 11 In this regard, since various factors can affect mortality in any traumatic incident,12, 13, 14 there is an increasing demand for local data on trauma, which includes not only mortality rates but also the factors involved in post-trauma mortality.15 Early detection of these risk factors can significantly increase the quality of care and therefore lead to the improvement of patient outcomes and reduction of mortality caused by acute trauma.16, 17 Further advancements in this field would require data collection, planning and development of new strategies.10, 11 However, although trauma is the leading cause of death and one of the main causes of disability in the active population of developing countries, its significance has unfortunately been overlooked.2
In conclusion, considering the high prevalence of trauma in Iran and the consequent high rate of mortality and adverse outcomes, an investigation of associated factors seems essential in this relation. Therefore, the current study aims to determine the risk factors associated with mortality among trauma patients referred to the Shahid Rajaee trauma center of Shiraz, a level one trauma center carrying the main load of trauma cases in Shiraz, as well as severely injured patients all through the Fars Province.
Methods
This research was a retrospective cohort study aimed to determine risk factors for mortality in trauma patients admitted to Shahid Rajaee trauma center, Shiraz, in 2017. Study population included all patients hospitalized in the Shahid Rajaee hospital of Shiraz, the biggest trauma center in Southern Iran, during the previous 6 months (February to July 2017). Sampling was done through systematic randomization. In this study, each patient was assigned a number using a randomization software and the patient file numbers; therefore, the anonymity of patients were protected; furthermore, one out of every 8 patients were randomly evaluated. Inclusion criteria consisted of admission to Shahid Rajaee hospital for trauma during the previous 6 months (February to July 2017); however, individuals under 15 years of age were excluded from the study. Data including demographic information, pre- and post-accident conditions, patients’ clinical conditions at the time of admission and accident outcomes were extracted from patient files in the hospital archives; demographic information included: age, gender, marital status, education, weight, height and body mass index (BMI); pre- and post-accident conditions were: time of accident, accident circumstances, accident mechanism, method of transfer, patient transfer time and use of helmet; clinical conditions at the time of admission consisted of: systolic blood pressure, heart rate, respiratory rate, mean revised trauma score (RTS), mean trauma revised injury severity score (TRISS), injured body regions, injury severity based on injury severe score (ISS), level of consciousness based on the Glasgow coma scale (GCS)18 and history of heart disease, hypertension, respiratory disease, low vision and diabetes; finally, accident outcomes included survival and death We get information from Forensic Medical for patients who die before arriving the hospital.
We assessed the effects of these risk factors on mortality. We should note that data collection was done with complete adherence to the principles and guidelines of medical ethics. Data were analyzed using SPSS Statistics (version 21.0). Statistical analysis was performed in two stages, descriptive and analytic. Descriptive information was evaluated using tables, diagrams, means and standard deviations, while analytic data were analyzed via the chi-square test and an independent samples T-test. Moreover, a logistic regression model was used to study the role of factors affecting mortality among patients. Significance level was set at 0.05 in this study.
Results
The present study aimed to evaluate the risk factors affecting mortality among trauma patients referred to Shahid Rajaee hospital, Shiraz. Results revealed a mean age of 39.27 ± 18.52 for the 849 patients admitted due to trauma during a period of 6 months in 2017 (Feb–Jul), the youngest being 15 years old and the oldest 93. There were 596 males (70.2%) and 253 females (29.8%) among the patients. Men had a mean age of 37.09 ± 17.73 and mean age of women equaled to 44.42 ± 19.35, a difference which was statistically significant (). Eighty-eight individuals (10.4%) had passed away due to trauma. Among the fatalities, there were 70 males (79.5%) and 18 females (20.5%), which indicates a significant difference ( 0.026). Most trauma patients (60.4%) were in the 15–39 age-group and the age-group of ≥ 60 had the lowest frequency (14.3%). More than 66.7% of traumatic accidents involved road traffic collisions; following that, falls from heights had the highest frequency, accounting for about 20% of all incidents. Only 0.1% of the trauma cases had occurred as a result of sports accidents, which made them the least frequent cause of trauma. Of the patients, 81.4% had been transferred to the hospital by public emergency medical services. Most incidents leading to trauma had occurred between 7:00 a.m. and 3:00 p.m. Mean period between accident occurrence and transfer to hospital was 34.65 ± 29.05 min, 10 min being the fastest time and 180 min the slowest. About 44.5% of the patients had been transferred to the hospital in under 30 min after occurrence and only 7% experienced a delay of more than 60 min. Approximately 53% of the patients had been hospitalized for more than 48 h. Of all subjects, 4.4% had a history of trauma. There was no expression of any history of alcohol or drug use in 91% of the patients. Among individuals with a history of alcohol or drug use, 7.8% were under the influence at the time of accident and 92.2% had used at other instances. As can be seen in Table 1, among trauma patients, the highest frequency related to men between 15 and 39 years of age and the lowest frequency pertained to women over 60. In terms of marital status, married men had the highest frequency, while the lowest frequency related to divorced men and widows. In relation to level of education, men with high school diplomas were more involved in traumatic incidents and women with bachelor's degrees or higher had the lowest frequency in the population under study. Regarding occupation, self-employed men had experienced more traumatic incidents. Overall, the variables of age, marital status, education, occupation and history of hypertension, diabetes and trauma showed significant differences between genders. Meanwhile, history of low vision, respiratory disease and heart disease, length of hospital stay, time of accident and nationality of the trauma patients had no significant differences in terms of gender.
Table 1.
Frequency distribution of factors associated with trauma in trauma referrals based on gender.
| Variables | Frequency (Percentage, %) |
p value | |
|---|---|---|---|
| Female | Male | ||
| Age group (years) | <0.001 | ||
| 15–39 | 120 (23.4) | 393 (76.6) | |
| 40–60 | 81 (37.7) | 134 (62.3) | |
| > 60 | 52 (43.0) | 69 (57.0) | |
| Marital status | <0.001 | ||
| Single | 63 (18.9) | 271 (81.1) | |
| Married | 170 (34.9) | 317 (65.1) | |
| Divorced or widowed | 20 (71.4) | 8 (28.6) | |
| Education | 0.032 | ||
| Illiterate | 79 (42.5) | 107 (57.5) | |
| Under diploma | 28 (19.3) | 117 (80.7) | |
| Diploma | 112 (26.7) | 307 (73.3) | |
| Academic degree | 34 (34.3) | 65 (65.7) | |
| Nationality | 0.094 | ||
| Iranian | 247 (30.4) | 566 (69.6) | |
| Afghan | 6 (16.7) | 30 (83.3) | |
| Unknown | 125 (47.0) | 141 (53.0) | <0.001 |
| Occupation | |||
| Civil servant | 34 (24.8) | 103 (75.2) | |
| Self-employed | 85 (20.6) | 328 (79.4) | |
| Cause of trauma | 0.001 | ||
| Traffic accidents | 165 (29.3) | 398 (70.7) | |
| Falling down | 71 (40.1) | 106 (59.9) | |
| Falling objects | 3 (15.8) | 16 (84.2) | |
| Hit resulting from the invasion | 10 (14.7) | 58 (85.3) | |
| Sports injuries | 0 | 1 (100) | |
| Guns | 1 (10) | 9 (90) | |
| Others | 3 (50.0) | 3 (50.0) | |
| History of heart disease | 26 (46.4) | 30 (71.4) | 0.005 |
| History of hypertension | 45 (57.0) | 34 (43.0) | <0.001 |
| History of diabetes | 27 (60.0) | 18 (40.0) | <0.001 |
| History of respiratory disease | 7 (30.4) | 16 (69.6) | 0.55 |
| History of low vision | 5 (29.4) | 12 (70.6) | 0.97 |
| History of trauma | 4 (10.8) | 33 (89.2) | 0.005 |
| Time of accident | 0.57 | ||
| 7:00–15:00 | 127 (32.5) | 264 (67.5) | |
| 15:00–20:00 | 42 (31.8) | 90 (68.2) | |
| 20:00–7:00 | 51 (28.2) | 130 (71.8) | |
| Patient transfer time (Mean ± SD) | 39.63 ± 36.42 | 32.45 ± 27.84 | 0.008 |
| Length of hospital stay (h) | 0.32 | ||
| <6 | 23 (24.5) | 71 (75.5) | |
| 6–24 | 25 (28.7) | 62 (71.3) | |
| 24–48 | 32 (27.1) | 86 (72.9) | |
| >48 | 147 (32.7) | 302 (67.3) | |
| Injured body regions | |||
| Head & neck | 99 (27.6) | 260 (72.4) | 0.12 |
| Face | 40 (27.6) | 105 (72.4) | 0.29 |
| Chest | 29 (19.9) | 117 (80.1) | 0.002 |
| Abdomen | 28 (24.3) | 87 (75.7) | 0.1 |
| Spine | 30 (27.3) | 80 (72.7) | 0.3 |
| Extremity | 156 (29.9) | 365 (70.1) | 0.48 |
| External | 2 (10.5) | 17 (89.5) | 0.4 |
| GCS (Mean ± SD) | 14.19 ± 2.54 | 13.49 ± 3.43 | 0.001 |
| ISS (Mean ± SD) | 8.68 ± 7.47 | 9.04 ± 9.06 | 0.58 |
| RTS (Mean ± SD) | 7.61 ± 0.8 | 7.41 ± 1.1 | 0.005 |
| TRISS (Mean ± SD) | 95.92 ± 11.36 | 93.36 ± 17.46 | 0.014 |
GCS: Glasgow coma scale, ISS: injury severe score, RTS: revised trauma score, TRISS: trauma revised injury severity score.
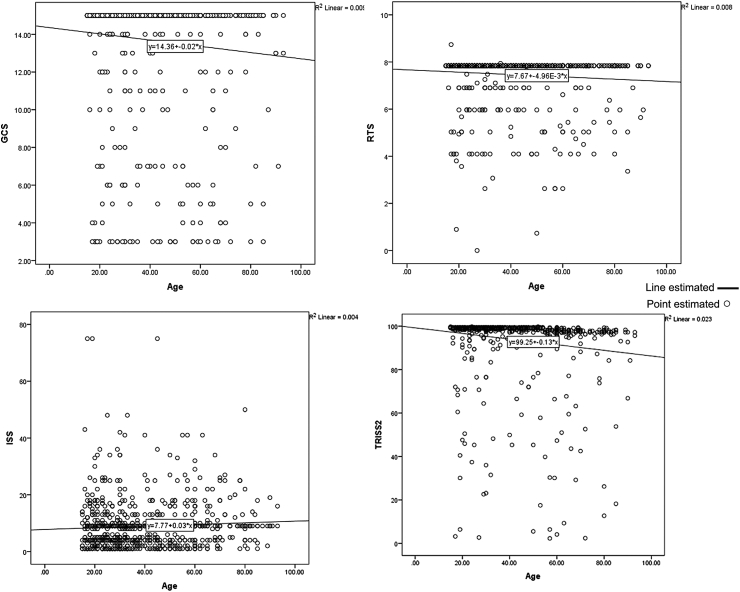
Impact of age on the indices GCS, ISS, RTS and TRISS
Fig. 1 demonstrates the relationships between age and the indices of GCS, ISS, RTS and TRISS. An evaluation of the relationship between age and GCS based on the figure revealed a linear, inverse relationship between the two variables (−0.096. Furthermore, there was a linear, direct relationship between age and ISS (0.063). A linear, inverse relationship existed between age and RTS (−0.088). Age and TRISS had a linear, inverse relationship (−0.152).
Fig. 1.
Relationship between GCS, ISS, RTS and TRISS in terms of age.
Table 2 shows that the variables of respiratory rate at the time of admission, method of patient transfer, time of accident, patient triage level and the indices of GCS, ISS and TRISS revealed significant differences between trauma fatalities and survivals, but the variables of heart rate at the time of admission, patient transfer time and RTS showed no significant differences in this relation.
Table 2.
Frequency distribution of factors associated with mortality in trauma patients.
| Variables | Frequency (Percentage, %) |
p value | |
|---|---|---|---|
| Survival | Un-survival | ||
| Blood pressure (Mean ± SD) | 123.21 ± 18.75 | 97.95 ± 36.61 | <0.001 |
| Respiratory rate (Mean ± SD) | 18.82 ± 2.789 | 19.83 ± 7.74 | 0.001 |
| Heart rate (Mean ± SD) | 84.39 ± 14.23 | 97.81 ± 35.29 | 0.25 |
| Patient transfer time (min) | 0.15 | ||
| <30 | 356 (94.4) | 21 (5.6) | |
| 30–60 | 259 (92.2) | 22 (7.8) | |
| <60 | 59 (98.3) | 1 (1.7) | |
| Method of transfer | 0.007 | ||
| Ambulance (public & private) | 622 (88.2) | 83 (11.8) | |
| Personal vehicle & others | 122 (96.1) | 5 (3.9) | |
| Time of accident | 0.007 | ||
| 7:00–15:00 | 367 (93.9) | 24 (6.1) | |
| 15:00–20:00 | 116 (87.9) | 16 (12.1) | |
| 20:00–7:00 | 175 (96.7) | 6 (3.3) | |
| Triage level | <0.001 | ||
| Level 1 | 42 (34.4) | 22 (65.6) | |
| Level 2 | 82 (71.3) | 33 (28.7) | |
| Level 3 & higher | 596 (100.0) | 0 | |
| GCS | <0.001 | ||
| 13–15 | 696 (97.8) | 16 (2.2) | |
| 9–12 | 31 (79.5) | 8 (20.5) | |
| ≤8 | 26 (29.9) | 61 (70.1) | |
| ISS | <0.001 | ||
| 0–8 | 401 (99.5) | 2 (0.5) | |
| 9–5 | 271 (88.6) | 35 (11.4) | |
| ≥16 | 87 (68.0) | 41 (32.0) | |
| RTS | 0.9 | ||
| <7.96 | 720 (90.3) | 77 (9.7) | |
| ≥7.96 | 1 (100.0) | 0 | |
| TRISS | <0.001 | ||
| <96 | 54 (46.2) | 63 (53.8) | |
| ≥96 | 668 (97.9) | 14 (2.1) | |
GCS: Glasgow coma scale, ISS: injury severe score, RTS: revised trauma score, TRISS: trauma revised injury severity score.
An estimation of risk of death due to trauma via logistic regression
According to our single-variable analysis, age and gender both had influences on the risk of mortality; in this regard, women were at a 43% lower risk of death comparing to men (odds ratio (OR) = 0.57, 95% confidence interval (CI): 0.32–0.98), which is a statistically significant difference (0.045). The variables of marital status, education and occupation also had no a significant effect on risk of death. Later it was revealed that length of hospital stay had a significant impact on risk of mortality. Patients who had been hospitalized between 24 and 48 h were at 9 times higher risk of death compared to patients who had stayed for less than 6 h (OR = 9.07, 95% CI: 2.58–31.88); this increased risk was statistically significant (0.001). The variables of patient transfer time and time of accident occurrence didn't have a significant impact on risk of death. Heart rate at the time of admission, head-and-neck injury, thorax injury and injuries to the extremities all had significant effects on risk of death due to trauma; meanwhile, history of heart disease, diabetes and respiratory disease, spinal injury and other types of injury didn't have a significant effect on risk of mortality. Our single-variable evaluations showed that for each unit increase in GCS, risk of death decreased by about 40% (OR = 0.63, 95% CI: 0.59–0.67); this observation was statistically significant ( 0.001). Moreover, risk of death increased by 10% with each unit increase in ISS (OR = 1.11, 95% CI: 1.08–1.14), a statistically significant observation ( 0.001). Regarding RTS, each unit increase in this index caused an 80% reduction in the risk of death (OR = 0.2, 95% CI: 0.15–0.26); this reduction was statistically significant as well ( 0.001). And finally, it was revealed that for each unit increase in TRISS, risk of death would decrease by 24% (OR = 0.76, 95% CI: 0.65–0.96), which is a statistically significant relationship (Table 3).
Table 3.
Estimation of risk of death due to trauma through univariate logistic regression.
| Variables | Adjusted OR | 95% CI for OR |
p value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.05 | 1.02 | 1.11 | <0.001 |
| Gender | 0.0457 | |||
| Male | – | |||
| Female | 0.57 | 0.32 | 0.98 | |
| Length of hospital stay (h) | <0.001 | |||
| <6 | Reference | |||
| 6–24 | 2.15 | 1.01 | 5.59 | |
| 24–48 | 7.23 | 1.12 | 26.19 | |
| >48 | 9.07 | 2.58 | 31.88 | |
| Occupation | 0.59 | |||
| Unemployed | – | |||
| Public | 0.05 | 0.004 | 0.88 | |
| Self-employed | 4.04 | 0.95 | 17.25 | |
| Type of injury | ||||
| Head-and-neck injury | – | |||
| Face injuries | 0.98 | 0.93 | 0.02 | 0.42 |
| Thorax injuries | 1.32 | 1.27 | 1.37 | <0.001 |
| Abdomen | 0.99 | 0.93 | 1.04 | 0.71 |
| Extremities | 1.06 | 1.04 | 1.09 | <0.001 |
| Hypertension | 5.12 | 1.05 | 14.12 | <0.001 |
| GCS | 0.63 | 0.59 | 0.67 | <0.001 |
| ISS | 1.11 | 1.08 | 1.14 | <0.001 |
| RTS | 0.2 | 0.15 | 0.26 | <0.001 |
| TRISS | 0.76 | 0.65 | 0.96 | <0.001 |
| Heart rate >100 | 1.16 | 1.05 | 1.19 | <0.001 |
OR: odds ratio, CI: confidence interval, GCS: Glasgow coma scale, ISS: injury severe score, RTS: revised trauma score, TRISS: trauma revised injury severity score.
In the end, all variables with a significant effect on risk of death were entered simultaneously into the regression model; the final model is presented in Table 4. As can be observed in the table, as risk of death increases by 6% for each year increase in age (OR = 1.06, 95% CI: 1.023–1.10), a statistically finding. Each unit increase in heart rate at the time of admission would increase the risk of fatality by 5%; this observation has statistical significance. Patients with injuries to the head and neck were 3.5 times more at risk of mortality; however, this increased risk wasn't statistically significant. Eventually, we found that each unit increase in TRISS would cause a 20% reduction in risk of death; this finding was statistically significant.
Table 4.
Multivariate logistic regression for estimation of risk of death due to trauma.
| Variables | Adjusted OR | 95% CI for OR |
p value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.06 | 1.023 | 1.10 | 0.002 |
| Occupation | ||||
| Unemployed | – | |||
| Public | 0.05 | 0.004 | 0.88 | 0.59 |
| Self-employed | 4.04 | 0.95 | 17.25 | 0.36 |
| TRISS | 0.82 | 0.71 | 0.88 | <0.001 |
| Heart Rate >100 | 1.05 | 1.02 | 1.08 | <0.001 |
| Head-and-neck injury | 3.55 | 1.05 | 12.32 | |
| Hypertension | 6.07 | 1.26 | 29.2 | 0.024 |
OR: odds ratio, CI: confidence interval, TRISS: trauma revised injury severity score.
Discussion
The present study made an evaluation of risk factors associated with mortality in trauma patients referred to Shahid Rajaee hospital during a period of 6 months in 2017 (February–July). Of the 849 patients under study, 10.4% had passed away, which is a higher rate comparing to reports from other Iranian cities.19, 20, 21, 22, 23, 24 Considering that in most developing countries, more than 70% of trauma-related fatalities occur in the pre-hospital stage,25 the higher rate of mortality in this study could be related to the fact that our study considered pre-hospital deaths as well, while other studies had only paid attention to deaths occurring in the hospital. Individual errors and lack of adherence to safety protocols were the main causes of pre-hospital fatality. Increased awareness of the society toward adherence to safety guidelines and improvement of pre-hospital emergency services can minimize the mortality caused by trauma throughout the world, especially in lower middle-income countries such as Iran, which has a very high rate accidents and trauma.26, 27 Technically, pre-hospital care involves provision of medical services to patients at the site of accident and on the way to the hospital by the emergency unit, which is considered the first interaction with the patients before admission.28 By true detection of triage level, optimize patient screen time, improve patient care can decrease in-hospital mortality of trauma patients. According to our study results, men had experienced more fatalities due to trauma compared to women, which is consistent with results from previous studies.20, 21, 29 Also, results revealed that most trauma patients were males, which is consistent with the findings of most studies.22, 30, 31, 32, 33, 34, 35 This is caused by the fact that men are more prone to accidents than women. Moreover, considering the socioeconomic and cultural state of our society (women mostly being housewives and higher involvement of men in the transportation sector), this finding is explainable. The patients had a mean age of about 39 years in this study and the age-group of 15–39 had the highest frequency, it shows that most trauma patients were in the working ages, a finding consistent with most studies in Iran.36, 37 Furthermore, a study in Singapore and a study by Worley et al. both showed similar results.38, 39 Our results showed that in trauma patients, ISS scores would increase by aging; previous studies have reported the same results.40, 41 It was also determined that aging would lead to increased TRISS, GCS and RTS. In terms of occupation, self-employed individuals are at a higher risk of death than the unemployed by 4 times and civil servants are 95% less at risk of death compared to unemployed individuals. It seems that there isn't sufficient research in regard to the circumstances of trauma occurrence, which requires further study in various regions. In all possibility, increasing workplace safety and paying attention to the nature of recreational activities would place the population of this study at a lower risk of traumatic incidents, which would consequently lead to a reduced rate of mortality. Therefore, an assessment is needed in order to improve the preventive measures and create safer conditions, as well as to provide respective training with consideration to the epidemiological trends in our country. From the results, over 81% of the patients had been transferred to the hospital by public ambulances and only 14% had used personal vehicles to get to hospital. This indicates that the quality of emergency services has improved. Results from various studies showed the increasing usage of ambulances for patient transfer during the past years, in a study in Tehran in 1999, 7.2% of the patients were transferred to the hospital by public ambulances, while this rate was close to 50% in a study conducted in Isfahan in 2014.42 As previously witnessed, the rate of ambulance usage has increased significantly in the present study. Mean patient transfer time equaled to 30 min in this study; this variable is technically the average time it takes from occurrence of accident until transfer to hospital. Most patients had been transferred to the hospital in 30 min; however, for about 7% of them, it had taken more than an hour to get to hospital. This period was around 27 min in a study by Zamani et al.,23 which is close to our findings. In study of Newgard et al.,43 median patient transfer time was between 28.1 and 42.1 min, this value varies from different states in the United States. The findings reveal that road traffic accidents as the leading cause of trauma and falls from heights held the second rank, which is consistent with results from other studies24, 33, 35, 44; however, certain studies didn't report similar findings.26, 42 The most common site of injury was the head-and-neck region in our study, and the extremities had the highest frequency following that, which is justifiable considering the high prevalence of motor-vehicle accidents and falls from height. Some studies showed different results in this relation, which could be as a result of social and cultural differences in other communities. Approximately 46% of the deceased patients had been hospitalized for longer than 48 h; previous studies have presented consistent reports in this regard.21 In regard to ISS, GCS, RTS and TRISS, our results showed that all these indices had a significant effect on risk of death due to trauma. In this regard, risk of death increases by 10% for each unit increase in ISS, and for each unit increase in the indices of GCS, RTS and TRISS, risk of death would decrease by 40%, 80% and 10%, respectively. The present study reports a mean ISS of 8.9, which is lower comparing to scores provided by other studies45, 46; this could be resulted by the fact that ISS is not determined in the cases of pre-hospital fatality. Furthermore, a regression analysis conducted by Ay et al.47 revealed that ISS had significant effects on the mortality of trauma patients; several other studies, as well, have significantly determined increased ISS as an effective factor for mortality in trauma cases.48, 49, 50, 51 However, certain studies reported that ISS is not an independent risk factor in relation to mortality.52, 53 Results from a study by Philip et al.45 showed an ISS of lower than 14 in 3.5% of the fatality cases, and a GCS of between 3 and 4 in about 46% of them; both indices had an impact on risk of death. Overall, ISS, GCS, RTS and TRISS all can be used independently as predictors of mortality. These indices, used together or along with other triage indices, can become a more powerful, useful tool to estimate risk of death in trauma patients. As previously witnessed, results from our logistic regression analysis indicated the influence of TRISS on trauma-induced mortality; the analysis showed that TRISS can be an appropriate predictor of mortality in combination with increased heart rate and high blood pressure.
Our study strengths included a large sample size and three sets of demographic variables related to accident and clinical factors in a level one trauma center of south of Iran. Despite these advantages, there were certain limitations to our research as well. First of all, patients were not followed up after discharging from hospital. Secondly, the study only focused on the initial stage of clinical evaluations, and lastly, our study didn't include pediatric trauma patients. In this regard, the risk factors for mortality could be insignificant in relation to children and infants. Moreover, duration of screening of patients is too weak to summarize the risk factors in trauma patients, so, a study with a higher follow-up duration seems to have better achievement.
Based on our results, accident mortality rate can be decreased by more attention in injured patients with history of risk factors such as hypertension, heart disease, diabetes and priority to care of patients with triage level 1, higher injury severity score. In addition, in-hospital death due to accidents are also reduced by increasing pre-hospital actions. Therefore, we suggest that future studies widen their research by focusing on multiple centers, also, not limiting the evaluations to the admission stage and involving the pediatric trauma patients would be of obvious value.
According to our results, increasing in the ISS index increases the risk of death in trauma patients, but increasing the GCS, RTS and TRISS indices reduces the risk of death in trauma patients. It was also found that the TRISS index was better predictor of death for traumatic patients than other indicators. Therefore, we must admit that trauma-related mortality can be reduced through improvement of preventive measures for accidents, especially road-traffic accidents, increased safety of roads, The importance of giving emergency care to the pre-hospital, better exertion of control by the traffic police and improvements in pre-hospital and hospital care by proper training of the emergency personnel.
Funding
This research has been supported with grant number of 98-01-38-19738 by Shiraz University of Medical Sciences in Shiraz, Iran.
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.01.012.
Ethical statement
This project has been approved by the research ethic committee by Shiraz University of Medical Sciences in Shiraz, Iran.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Curtis K., Caldwell E., Delprado A. Traumatic injury in Australia and New Zealand. Australas Emerg Nurs J. 2012;15:45–54. doi: 10.1016/j.aenj.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Myburgh J.A., Cooper D.J., Finfer S.R. Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. J Trauma. 2008;64:854–862. doi: 10.1097/TA.0b013e3180340e77. [DOI] [PubMed] [Google Scholar]
- 3.Karbakhsh M., Zandi N., Rouzrokh M. Injury epidemiology in Kermanshah: the national trauma project in Islamic Republic of Iran. East Mediterr Health J. 2009;15:57–64. [PubMed] [Google Scholar]
- 4.Lopez A.D., Mathers C.D., Ezzati M. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 5.Mohammad A., Branicki F., Abu-Zidan F.M. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: a systematic review. World J Surg. 2014;38:322–329. doi: 10.1007/s00268-013-2294-0. [DOI] [PubMed] [Google Scholar]
- 6.Peden M., McGee K., Krug E. World Health Organization; Washington, DC: 2002. Injury: A Leading Cause of the Global Burden of Disease, 2000. [Google Scholar]
- 7.Araqi E., Vahedian M. Study on susceptible and damages from motorcycle accidents in Mashhad in 2005. Gonabad Univ Med Sci Health Serv. 2007;13:34–39. [Google Scholar]
- 8.Sanaei-Zadeh H., Vahabi R., Nazparvar B. An epidemiological study and determination of causes of traffic accident-related deaths in Tehran, Iran (during 2000–2001) J Clin Forensic Med. 2002;9:74–77. doi: 10.1054/jcfm.2002.0547. [DOI] [PubMed] [Google Scholar]
- 9.Khatami S., Tarighi P., Rezai Y. Epidemiology of trauma baqiatallah hospital: a one-Year Prospective study. J Mil Med. 2003;5:13–19. [Google Scholar]
- 10.Mock C., Lormand J.D., Goosen J. World Health Organization; Geneva: 2004. Guidelines for Essential Trauma Care. [Google Scholar]
- 11.Magruder K.M., Kassam-Adams N., Thoresen S. Prevention and public health approaches to trauma and traumatic stress: a rationale and a call to action. Eur J Psychotraumatol. 2016;7:19715. doi: 10.3402/ejpt.v7.29715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alimohammadi H., Bidarizerehpoosh F., Mirmohammadi F. Cause of emergency department mortality; a case-control study. Emerg (Tehran) 2014;2:30–35. [PMC free article] [PubMed] [Google Scholar]
- 13.Paydar S., Moghaninasab A., Asiaei E. Outcome of patients underwent emergency department thoracotomy and its predictive factors. Emerg (Tehran) 2014;2:125–129. [PMC free article] [PubMed] [Google Scholar]
- 14.Rao D., Sood D., Pathak P. Causes of sudden cardiac death on autopsy findings; a four-year report. Emerg (Tehran) 2014;2:12–17. [PMC free article] [PubMed] [Google Scholar]
- 15.Sim J., Lee J., Lee J.C. Risk factors for mortality of severe trauma based on 3 years' data at a single Korean institution. Ann Surg Treat Res. 2015;89:215–219. doi: 10.4174/astr.2015.89.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers A., Rogers F.B., Schwab C.W. Increased mortality with undertriaged patients in a mature trauma center with an aggressive trauma team activation system. Eur J Trauma Emerg Surg. 2013;39:599–603. doi: 10.1007/s00068-013-0289-z. [DOI] [PubMed] [Google Scholar]
- 17.Sasser S.M., Hunt R.C., Faul M. Guidelines for field triage of injured patients: recommendations of the national expert panel on field triage, 2011. MMWR Recomm Rep. 2012;61:1–20. [PubMed] [Google Scholar]
- 18.Lakeh M.M., Banihashemi S.T., Kia G.V. Comparison of trauma scoring systems for prediction of patient's prognosis. Razi J Med Sci. 2002;9:129–137. [Google Scholar]
- 19.Fazel M.R., Fakharian E., Mahdian M. Demographic profiles of adult trauma during a 5 Year period (2007-2011) in kashan, IR Iran. Arch Trauma Res. 2012;1:63–66. doi: 10.5812/atr.6770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rasouli M.R., Saadat S., Haddadi M. Epidemiology of injuries and poisonings in emergency departments in Iran. Public Health. 2011;125:727–733. doi: 10.1016/j.puhe.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Yadollahi M., Anvar M., Ghaem H. Logistic regression modeling for evaluation of factors affecting trauma outcome in a level I trauma center in Shiraz. Iran Red Crescent Med J. 2017;19:33559. [Google Scholar]
- 22.Yadollahi M., Paydar S., Jahromi G.S. Types and causalities in dead patients due to traumatic injuries. Arch Trauma Res. 2015;4 doi: 10.5812/atr.26028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zamani M., Esmailian M., Mirazimi M.S. Cause and final outcome of trauma in patients referred to the emergency department: a cross sectional study. Iran J Emerg Med. 2014;1:7–22. [Google Scholar]
- 24.Zargar M., Motamedi S.M.R.K., Karbakhsh M. Trauma care system in Iran. Chin J Traumatol. 2011;14:131–136. [PubMed] [Google Scholar]
- 25.Mock C.N., Jurkovich G.J., Arreola-Risa C. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44:804–812. doi: 10.1097/00005373-199805000-00011. discussion 812-814. [DOI] [PubMed] [Google Scholar]
- 26.Haghparast-Bidgoli H., Hasselberg M., Khankeh H. Barriers and facilitators to provide effective pre-hospital trauma care for road traffic injury victims in Iran: a grounded theory approach. BMC Emerg Med. 2010;10:20. doi: 10.1186/1471-227X-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mina M., Tahereh K.M., Ehsan K.L. Epidemiologic survey of trauma and associated factors in Guilan. Iran J Crit Care Nurs. 2014;7:41–50. [Google Scholar]
- 28.Von Elm E., Schoettker P., Henzi I. Pre-hospital tracheal intubation in patients with traumatic brain injury: systematic review of current evidence. Br J Anaesth. 2009;103:371–386. doi: 10.1093/bja/aep202. [DOI] [PubMed] [Google Scholar]
- 29.Bhalla K., Naghavi M., Shahraz S. Building national estimates of the burden of road traffic injuries in developing countries from all available data sources: Iran. Inj Prev. 2009;15:150–156. doi: 10.1136/ip.2008.020826. [DOI] [PubMed] [Google Scholar]
- 30.Azizi A., Abdoli G. Mortality rates in Kermanshah province–2000. J Kerman Univ Med Sci. 2003;7 [Google Scholar]
- 31.Goel A., Kumar S., Bagga M.K. Epidemiological and Trauma Injury and Severity Score (TRISS) analysis of trauma patients at a tertiary care centre in India. Natl Med J India. 2004;17:186–189. [PubMed] [Google Scholar]
- 32.Murlidhar V., Roy N. Measuring trauma outcomes in India: an analysis based on TRISS methodology in a Mumbai university hospital. Injury. 2004;35:386–390. doi: 10.1016/S0020-1383(03)00214-6. [DOI] [PubMed] [Google Scholar]
- 33.Solagberu B., Adekanye A., Ofoegbu C. Epidemiology of trauma deaths. W Afr J Med. 2003;22:177–181. doi: 10.4314/wajm.v22i2.27944. [DOI] [PubMed] [Google Scholar]
- 34.Yadollahi M., Anvar M., Ghaem H. Epidemiologic study of trauma patients admitted to a level 1 trauma center in Shiraz: one year survey. Razavi Int J Med. 2015;3 [Google Scholar]
- 35.Zafar H., Rehmani R., Raja A. Registry based trauma outcome: perspective of a developing country. Emerg Med J. 2002;19:391–394. doi: 10.1136/emj.19.5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farzandipour M., Ghattan H., Mazrouei L. Epidemiological study of traumatic patients referred to neghavi hospital of kashan. J Kerman Univ Med Sci. 2007;11 [Google Scholar]
- 37.Yousefzadeh S., Dafchahi M.A., Maleksari H.M. Epidemiology of injuries and their causes among traumatic patients admitted into Poursina hospital, Rasht. J Kerman Univ Med Sci. 2007;11 [Google Scholar]
- 38.Wong Z.H., Chong C.K., Tai B.C. A review of fatal road traffic accidents in Singapore from 2000 to 2004. Ann Acad Med Singapore. 2009;38:594–596. [PubMed] [Google Scholar]
- 39.Worley H. 2006. Road Traffic Accidents Increase Dramatically Worldwide. Population Reference Bureau.https://www.prb.org/roadtrafficaccidentsincreasedramaticallyworldwide/ [Google Scholar]
- 40.Caterino J.M., Valasek T., Werman H.A. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med. 2010;28:151–158. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 41.Kuhne C.A., Ruchholtz S., Kaiser G.M. Mortality in severely injured elderly trauma patients—when does age become a risk factor? World J Surg. 2005;29:1476–1482. doi: 10.1007/s00268-005-7796-y. [DOI] [PubMed] [Google Scholar]
- 42.Amani F., Habibzadeh S., Rostami K. Specifications of traumatized patients referring to Fatemi hospital of Ardabil, 2007-8. J Ardabil Univ Med Sci. 2009;9:13–22. [Google Scholar]
- 43.Newgard C.D., Schmicker R.H., Hedges J.R. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55:235–246. doi: 10.1016/j.annemergmed.2009.07.024. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mohseni M., Khaleghdoost M.T., Adib M. 2015. Surveying the Condition of Pre-hospital Emergency and Factors Associated to it in Traumatic Patients Were Transported.http://www.investigacionencuidados.es/investen/2015/posteres/193.pdf [Google Scholar]
- 45.Schluter P.J. The trauma and injury severity score (TRISS) revised. Injury. 2011;42:90–96. doi: 10.1016/j.injury.2010.08.040. [DOI] [PubMed] [Google Scholar]
- 46.Thanapaisal C., Saksaen P. A comparison of the acute physiology and chronic health evaluation (APACHE) II score and the trauma-injury severity score (TRISS) for outcome assessment in Srinagarind intensive care unit trauma patients. J Med Assoc Thail. 2012;95:S25–S33. [PubMed] [Google Scholar]
- 47.Ay N., Alp V., Aliosmanoğlu İ. Factors affecting morbidity and mortality in traumatic colorectal injuries and reliability and validity of trauma scoring systems. World J Emerg Surg. 2015;10:21. doi: 10.1186/s13017-015-0014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.AlEassa E.M., Al-Marashda M.J., Elsherif A. Factors affecting mortality of hospitalized chest trauma patients in United Arab Emirates. J Cardiothorac Surg. 2013;8:57. doi: 10.1186/1749-8090-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hasler R., Exadaktylos A., Lecky F. Systolic blood pressure below 110 Mmhg is associated with increased mortality in major trauma patients. Acad Emerg Med. 2012;19:712–713. doi: 10.1016/j.resuscitation.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 50.Lichtveld R.A., Panhuizen I.F., Smit R.B. Predictors of death in trauma patients who are alive on arrival at hospital. Eur J Trauma Emerg Surg. 2007;33:46–51. doi: 10.1007/s00068-007-6097-6. [DOI] [PubMed] [Google Scholar]
- 51.Sarani B., Temple-Lykens B., Kim P. Factors associated with mortality and brain injury after falls from the standing position. J Trauma. 2009;67:954–958. doi: 10.1097/TA.0b013e3181ae6d39. [DOI] [PubMed] [Google Scholar]
- 52.Brattström O., Granath F., Rossi P. Early predictors of morbidity and mortality in trauma patients treated in the intensive care unit. Acta Anaesthesiol Scand. 2010 Sep;54(8):1007–1017. doi: 10.1111/j.1399-6576.2010.02266.x. [DOI] [PubMed] [Google Scholar]
- 53.Ulvik A., Wentzel-Larsen T., Flaatten H. Trauma patients in the intensive care unit: short-and long-term survival and predictors of 30-day mortality. Acta Anaesthesiol Scand. 2007;51:171–177. doi: 10.1111/j.1399-6576.2006.01207.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.