Abstract
Introduction
Surgical site infections are associated with increased morbidity and mortality in patients. The Getting It Right First Time surgical site infection programme set up a national survey to review surgical site infection rates in surgical units in England. The objectives were for frontline clinicians to assess the rates of infection following selected procedures, to examine the risk of significant complications and to review current practice in the prevention of surgical site infection.
Methods
A national survey was launched in April 2017 to assess surgical site infections within 13 specialties: breast surgery, cardiothoracic surgery, cranial neurosurgery, ear, nose and throat surgery, general surgery, obstetrics and gynaecology, ophthalmology, oral and maxillofacial surgery, orthopaedic surgery, paediatric surgery, spinal surgery, urology and vascular surgery. All participating trusts prospectively identified and collected supporting information on surgical site infections diagnosed within the six-month study period.
Results
Data were received from 95 NHS trusts. A total of 1807 surgical site infection cases were reported. There were variations in rates reported by trusts across specialties and procedures. Reoperations were reported in 36.2% of all identified cases, and surgical site infections are associated with a delayed discharge rate of 34.1% in our survey.
Conclusion
The Getting It Right First Time surgical site infection programme has introduced a different approach to infection surveillance in England. Results of the survey has demonstrated variation in surgical site infection rates among surgical units, raised the importance in addressing these issues for better patient outcomes and to reduce the financial burden on the NHS. Much work remains to be done to improve surgical site infection surveillance across surgical units and trusts in England.
Keywords: Surgical wound infection, Infection control, Population surveillance, Postoperative care
Introduction
Surgical site infections are associated with increased morbidity and mortality in surgical patients. The management of a surgical site infection can involve prolonged hospitalisation, readmission and reoperation, and can be associated with increased diagnostic and treatment costs.1 The importance of monitoring and reducing rates of surgical site infection is therefore widely acknowledged.
In the UK, Public Health England (PHE) runs a surgical site infection surveillance service, which broadly covers eight surgical specialties across hospitals in England; this is mandatory for four orthopaedic procedures and voluntary in a further 13 categories of surgical procedures.2 The National Joint Registry and National Institute for Cardiovascular Outcomes Research also routinely collect data on surgical site infection rates following orthopaedic and cardiac surgeries, respectively. Despite the work of these programmes, the national review of all surgical departments by the Getting It Right First Time (GIRFT) programme has revealed a lack of awareness of surgical site infection rates by both units and individual clinicians.3–5 Furthermore, specialties such ear, nose and throat surgery, ophthalmology, oral and maxillofacial surgery and urology were omitted from these surveillance programmes.
There is a concern at the ability of surgeons to carry out truly informed consent for surgical procedures when they are not aware of the infection rate of their unit. GIRFT has received data from NHS Resolution identifying 383 medical negligence claims related to surgical site infections notified to NHS trusts in England between April 2012 and March 2017, which are estimated to cost £35.2million.6 Clearly, surgeons should have access to accurate information on their unit’s infection rates when consenting patients for operations, both to improve shared decision making but also to decrease the cost of potential litigation against the NHS.
The GIRFT surgical site infection programme set up a national survey to review infection rates in surgical units in England. The objectives were for frontline clinicians to assess the rates of surgical site infection following selected procedures, to examine the risk of significant complications associated with surgical site infections, as well as to review current practice in the prevention of surgical site infections for the specified procedures.
Materials and methods
Designing the survey
The GIRFT surgical site infection programme assessed infections within 13 surgical specialties: breast surgery, cardiothoracic surgery, cranial neurosurgery, ear, nose and throat surgery, general surgery, obstetrics and gynaecology, ophthalmology, oral and maxillofacial surgery, orthopaedic surgery, paediatric surgery, spinal surgery, urology and vascular surgery. The survey was designed in consultation with the respective GIRFT-appointed national clinical leads for each of the 13 specialties. The type of procedures selected, data requested and the metrics developed were those deemed most significant in both improving patient outcomes and in supporting local improvement efforts to reduce the rates and impact of surgical site infections following consultations with the respective clinical leads.
Data collection
A national survey was launched in April 2017 and letters were sent to all hospital trusts in England, requesting data on surgical site infections associated with 65 categories of surgical procedures. All participating trusts were asked to undertake a six-month exercise to prospectively identify and collect supporting information on infections diagnosed between 1 May 2017 and 31 October 2017. A retrospective data collection exercise in relation to infections diagnosed between 1 November 2016 and 30 April 2017 was also planned, but recommended only for those units with an established surgical site infection surveillance system in place and with an accessible list of cases.
Within each participating unit, ‘audit leads’, were appointed to oversee the survey. Data collection packs containing instructions for data collection, definitions of surgical site infection and other diagnoses (e.g. sepsis) and, where relevant, OPCS Classification of Interventions and Procedures (OPCS-4) and International Classification of Diseases, tenth edition (ICD-10) codes were provided to all participants (Appendices 1,2 and 3). For the prospective part of the survey, participants were advised to identify eligible cases at the point of diagnosis/presentation with surgical site infection (e.g. postoperatively during the initial admission, in unplanned readmissions or in outpatient clinics). The local ‘audit leads’ were advised to liaise with relevant healthcare professionals within such settings (e.g. wound clinic, acute surgical admission clinics, specialty wards) to facilitate the identification of cases. Methods for identification of cases and data collection may vary depending on local arrangements and participants were expected to design their own strategies to suit their local set-up. Standardised Microsoft Excel templates were used for data collection (Appendix 5, online only). Each surgical unit was requested to provide information on the existence of a surgical site infection prevention bundle and antibiotic prophylaxis guidelines specific to the specialty and, where available, whether previous audits have been performed to assess for local compliance. For each case identified, data requested included the type of infection and the development of any complication (e.g. reoperation, delayed discharge, readmission, sepsis and mortality).
A webinar was hosted prior to the data collection period to address any potential queries. Any enquires regarding the survey were directed to the GIRFT Surgical Site Infection Audit Team throughout the data collection period via email.
Definitions
For the majority of specialties, a surgical site infection was defined as superficial, deep or organ/space infection, based on the definitions used by the PHE surveillance service and the US Centres for Disease Control and Prevention (CDC).7,8 The definitions of different types of surgical site infection were included in the briefing pack for all participants to maximise standardisation of identification across trusts (Appendix 3, online only). Broadly speaking, we define a surgical site infection as one that occurs within 30 days of surgery (without implants) and within one year of surgery if there is an implant in place.
Some exceptions to the definitions used were made in cardiothoracic surgery, cranial neurosurgery, ophthalmology and urology; deep sternal wound infection, infective endocarditis, craniotomy infection, meningitis, ventriculitis, cerebrospinal fluid (CSF) shunt-related infection, endophthalmitis, epididymitis and urinary tract infection were used to define surgical site infection in these specialties.
Analyses
Anonymised data were collected from all participating units at the end of the survey period by submission of the completed excel templates to our designated NHS.net email account. Additional data were also obtained from the Hospital Episode Statistics (HES) database, which provided the denominators used to calculate infection rates. For the analysis of infection rates, data from trusts with a low volume of work (defined as number of procedures less than 10) were suppressed and were not presented. All analyses were performed centrally by the national GIRFT surgical site infection audit team. Once all hospitals had submitted their data, our analyst from the national GIRFT surgical site infection programme validated the submitted data to ensure that they were complete and were accurate to the best of our knowledge.
Results
A letter of invitation to participate in the survey was sent to all hospital trusts in England. A total of 861 healthcare professionals, mostly doctors in training, registered to take part in the survey. Data were received from 95 NHS trusts, encompassing 198 surgical units in England. A total of 1807 individual cases of surgical site infection were reported.
Rates of infection
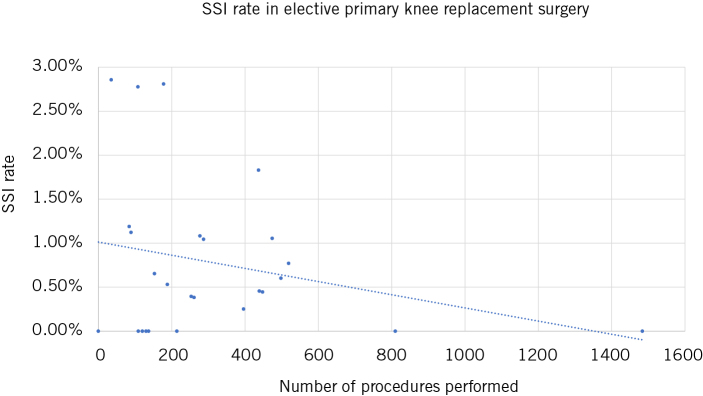
There were variations in infection rates reported by trusts across specialties and procedural types (Table 1). For example, in breast surgery procedures requiring a flap, a mean deep or organ/space infection rate of 8.9% was reported by trusts; a rate of 74.4% was reported by the surgical unit with the highest infection rate, while other breast surgical units did not report any infection during the survey period. We also observed variations within general surgery, the reported rates of deep or organ/space infection following emergency appendicectomy ranged from 0% to 47.8%. A trend towards higher infection rates being reported by trusts with lower activity levels was noted in most procedures, including in orthopaedic procedures such as elective primary knee replacement surgery (fig 1).
Table 1.
Surgical site infection rates by specialty and procedure.
| Specialty/procedurea | Surgical site infection (n) | Procedures performed (n) | Surgical site infection rate (%) | ||
| Mean | Minimum | Maximum | |||
| Breast surgery (n = 38) | 148 | 1614 | 9.2 | 0.0 | 61.1 |
| Breast implant procedures | 76 | 466 | 16.3 | 0.0 | 53.9 |
| Procedures requiring a flap | 41 | 463 | 8.9 | 0.0 | 74.4 |
| Level 2 mammoplasty: therapeutic or symmetrising | 31 | 685 | 4.5 | 0.0 | 61.1 |
| Cardiothoracic surgery (n = 8) | 109 | 13177 | 0.8 | 0.0 | 2.9 |
| Cardiac surgery: isolated CABG procedure | 37 | 4990 | 0.7 | 0.0 | 1.4 |
| Cardiac surgery: valve surgery ± combined procedure | 36 | 3150 | 1.1 | 0.0 | 3.7 |
| Cardiac surgery: other (exclude transplantation) | 5 | 608 | 0.8 | 0.0 | 4.2 |
| Thoracic surgery: lung resection | 17 | 2819 | 0.6 | 0.0 | 2.5 |
| Thoracic surgery: other (exclude transplantation) | 14 | 1610 | 0.9 | 0.0 | 3.7 |
| Cranial neurosurgery (n = 6) | 88 | 2061 | 4.3 | 1.0 | 14.0 |
| Cranial procedure for benign brain tumour | 25 | 295 | 8.5 | 0.0 | 18.4 |
| Cranial procedures for malignant brain tumour | 24 | 489 | 4.9 | 0.0 | 11.1 |
| Cranial procedure for trauma | 0 | < 10 | – | – | – |
| Brain shunt procedure | 6 | 315 | 1.9 | 0.0 | 4.4 |
| Insertion of external ventricular drain | 17 | 324 | 5.2 | 0.0 | 38.9 |
| Procedure performed for subarachnoid haemorrhage | 10 | 182 | 5.5 | 0.0 | 31.6 |
| Procedure performed for subdural haematoma | 6 | 456 | 1.3 | 0.0 | 3.8 |
| Ear, nose and throat (n = 14) | 29 | 2525 | 1.1 | 0.0 | 3.6 |
| Resections in head and neck cancer | 16 | 1059 | 1.5 | 0.0 | 17.2 |
| Bone anchored hearing aid surgery | 0 | < 10 | – | – | – |
| Cochlear implant procedures | 1 | 131 | 0.8 | 0.0 | 2.9 |
| Parotidectomy | 4 | 462 | 0.9 | 0.0 | 4.3 |
| Submandibular salivary gland removal | 0 | 20 | 0.0 | 0.0 | 0.0 |
| Thyroid surgery procedures | 8 | 853 | 0.9 | 0.0 | 4.0 |
| General surgery (n = 24) | 318 | 23085 | 1.4 | 0.0 | 14.5 |
| Elective cholecystectomy | 50 | 7099 | 0.7 | 0.0 | 2.9 |
| Elective gastrointestinal resection | 157 | 3629 | 4.3 | 0.0 | 18.0 |
| Elective hernia repair (incisional) | 20 | 1058 | 1.9 | 0.0 | 20.0 |
| Table 1 (continued) | |||||
| Elective hernia repair (inguinal) | 13 | 6310 | 0.2 | 0.0 | 2.0 |
| Emergency appendicectomy | 57 | 3639 | 1.6 | 0.0 | 47.8 |
| Emergency cholecystectomy | 18 | 1334 | 1.3 | 0.0 | 9.5 |
| Emergency laparotomy | 3 | 16 | 18.8 | 0.0 | 18.8 |
| Obstetrics and gynaecology (n = 20) | 294 | 18798 | 1.6 | 0.0 | 4.7 |
| Abdominal hysterectomy | 43 | 2544 | 1.7 | 0.0 | 7.3 |
| Caesarean section | 251 | 16214 | 1.5 | 0.0 | 7.1 |
| Ophthalmology (n = 18) | 33 | 68404 | 0.05 | 0.00 | 0.10 |
| Cataract surgery total | 18 | 60193 | 0.0 | 0.0 | 0.1 |
| Intravitreal Injection | 15 | 8211 | 0.2 | 0.0 | 2.8 |
| Oral and maxillofacial surgery (n = 7) | 48 | 8783 | 0.5 | 0 | 2.6 |
| Head and neck cancer surgery | 11 | 290 | 3.8 | 0.0 | 8.6 |
| Dentoalveolar surgery | 26 | 7731 | 0.3 | 0.0 | 2.7 |
| Surgery following trauma | 11 | 762 | 1.4 | 0.0 | 2.1 |
| Orthopaedic surgery (n = 29) | 130 | 20343 | 0.6 | 0.0 | 12.1 |
| Elective primary elbow replacement | 0 | 78 | 0.0 | 0.0 | 0.0 |
| Elective primary shoulder replacement | 6 | 888 | 0.7 | 0.0 | 3.6 |
| Elective primary hip replacement | 52 | 8603 | 0.6 | 0.0 | 17.4 |
| Elective primary knee replacement | 52 | 8968 | 0.6 | 0.0 | 2.9 |
| Elective primary ankle replacement | 0 | 93 | 0.0 | 0.0 | 0.0 |
| Elective revision elbow replacement | 0 | < 10 | – | – | – |
| Elective revision shoulder replacement | 0 | 47 | 0.0 | 0.0 | 0.0 |
| Elective revision hip replacement | 10 | 1028 | 1.0 | 0.0 | 5.3 |
| Elective revision knee replacement | 10 | 638 | 1.6 | 0.0 | 8.9 |
| Elective revision ankle replacement | 0 | <10 | – | – | – |
| Paediatric surgery (n = 7) | 27 | 563 | 4.8 | 1.5 | 15.4 |
| Emergency appendicectomy | 27 | 563 | 4.8 | 1.5 | 15.4 |
| Spinal surgery (n = 7) 23 | 2287 | 1.0 | 0.0 | 3.0 | |
| Posterior cervical spine decompression and instrumented fusion | 3 | 170 | 1.8 | 0.0 | 8.1 |
| Posterior correction of adolescent idiopathic scoliosis | 0 | < 10 | – | – | – |
| Single level discectomy or decompression (unilateral or bilateral) | 8 | 1674 | 0.5 | 0.0 | 1.6 |
| Single level instrumented posterior fusion (including interbody fusion) | 12 | 443 | 2.7 | 0.0 | 7.7 |
| Urology (n = 11) | 98 | 5410 | 1.8 | 0.0 | 15.1 |
| Artificial urinary sphincter surgery | 0 | < 10 | – | – | – |
| Cystoscopy | 44 | 2276 | 1.9 | 0.0 | 11.9 |
| Laser prostectomy | 0 | 33 | 0.0 | 0.0 | 0.0 |
| Penile prostheses surgery | 0 | 21 | 0.0 | 0.0 | 0.0 |
| Sacral nerve stimulation surgery | 0 | 56 | 0.0 | 0.0 | 0.0 |
| Transurethral resection of bladder tumours | 23 | 1256 | 1.8 | 0.0 | 11.9 |
| Transurethral resection of the prostate | 13 | 894 | 1.5 | 0.0 | 6.0 |
| Urinary tract stone surgery (litholapaxy) | 1 | 198 | 0.5 | 0.0 | 4.0 |
| Urinary tract stone surgery (ureteroscopy) | 15 | 594 | 2.5 | 0.0 | 10.0 |
| Urinary tract surgery (percutaneous nephrolithotomy) | 2 | 82 | 2.4 | 0.0 | 16.7 |
| Table 1 (continued) | |||||
| Vascular surgery (n = 9) | 116 | 4695 | 2.5 | 0.8 | 5.3 |
| Procedures for abdominal aortic aneurysm | 12 | 721 | 1.7 | 0.0 | 7.1 |
| Carotid endarterectomy | 1 | 412 | 0.2 | 0.0 | 2.5 |
| Lower-limb angioplasty | 3 | 1960 | 0.2 | 0.0 | 3.3 |
| Lower-limb bypass | 39 | 1133 | 3.4 | 1.9 | 5.5 |
| Lower-limb surgery for peripheral arterial diseaseb | 61 | 469 | 13.0 | 1.9 | 42.4 |
an = number of participating trusts.
b Except lower limb bypass.
Figure 1.
Deep or organ/space surgical site infection (SSI) rates following elective primary knee replacement surgery by number of procedures performed per trust.
Complications of surgical site infection
In the survey, reoperations were reported in 36.2% of all cases of surgical site infection identified. The rate of reoperation was highest in spinal and orthopaedic surgery, where rates of 84.6% and 82.6% were reported, respectively (Table 2). Highest implant removals were seen in breast surgery, orthopaedic and spinal surgery, with a respective rate of 52.8%, 32.2% and 10.5%. Sepsis was reported in almost 50% of the cases of infections that developed following urological procedures, and a mortality rate of 11.3% was reported to be associated with a surgical site infection developing after vascular surgery. The latter was largely following lower-limb procedures (mortality rates of 33.3%, n = 1; 10.5%, n = 4; and 9.8% n = 6, respectively, following lower-limb angioplasty, lower-limb bypass and lower-limb surgery for peripheral arterial disease, excluding bypass).
Table 2.
Rates of complications following surgical site infection, by specialty.
| Specialtya | Cases with complication (%) | |||
| Reoperation | Implant removalb | Sepsis | Mortality | |
| Breast surgery | 45.2 | 52.8 | 12.4 | 0.0 |
| Cardiothoracic surgery | 42.5 | 9.6 | 41.4 | 6.8 |
| Cranial neurosurgery | 69.6 | 60.9 | 31.1 | 7.6 |
| Ear, nose and throat | 30.3 | 7.1 | 12.1 | 0.0 |
| General surgery | 29.3 | 5.4 | 37.8 | 2.9 |
| Obstetrics and gynaecology | 6.4 | – | 18.0 | 0.0 |
| Oral and maxillofacial surgery | 34.4 | 41.2 | 12.5 | 0.0 |
| Orthopaedic surgery | 82.6 | 32.2 | 16.7 | 4.7 |
| Paediatric surgery | 25.9 | – | 14.8 | 0.0 |
| Spinal surgery | 84.6 | 10.5 | 23.1 | 0.0 |
| Urology | 4.8 | 8.6 | 47.2 | 4.8 |
| Vascular surgery | 49.1 | 23.1 | 28.3 | 11.3 |
| Total | 36.2 | 25.5 | 26.9 | 3.2 |
a Implant removal based on total number of cases where implants were inserted during primary surgery.
b no complications reported in ophthalmology.
Surgical site infection led to delayed discharges in 34.1% of all cases surveyed. The mean length of stay was 12.1 days during the primary admission when diagnosed with an infection. In 49.7% of cases of surgical site infection, readmissions with a mean length of stay of 9.8 days were also reported (Table 3).
Table 3.
Delayed discharges, readmissions and lengths of stay associated with surgical site infection, by specialty.
| Specialtya | Delayed discharge (%) | Length of stay | ||
| Primary admission (days) | Readmission (%) | Readmission (days) | ||
| Breast surgery | 6.0 | 2.7 | 56.0 | 5.0 |
| Cardiothoracic surgery | 43.8 | 17.0 | 58.2 | 16.5 |
| Cranial neurosurgery | 45.1 | 19.9 | 55.1 | 17.4 |
| Ear, nose and throat | 45.5 | 12.5 | 46.9 | 5.5 |
| General surgery | 48.0 | 18.0 | 46.0 | 7.2 |
| Obstetrics and gynaecology | 19.5 | 3.4 | 40.2 | 3.3 |
| Oral and maxillofacial surgery | 27.0 | 14.4 | 28.1 | 3.6 |
| Orthopaedic surgery | 32.7 | 11.5 | 71.3 | 17.6 |
| Paediatric surgery | 29.6 | 8.8 | 69.2 | 4.4 |
| Spinal surgery | 61.5 | 13.2 | 69.2 | 14.6 |
| Urology | 19.2 | 4.6 | 45.8 | 6.1 |
| Vascular surgery | 55.7 | 23.1 | 54.3 | 16.3 |
| Total | 34.1 | 12.1 | 49.7 | 9.8 |
a No admission reported in ophthalmology.
Use of local guidelines
A total of 82.7% of trusts confirmed the existence of local antibiotic prophylaxis guidelines, while a surgical site infection prevention bundle was reported to be in place in 50.3% of surgical units. Where present, audits to assess compliance with antibiotic guidelines and surgical site infection prevention bundle had been undertaken in only 34.0% and 40.2% of trusts, respectively (Table 4).
Table 4.
Trusts with local antibiotic prophylaxis guidelines and surgical site infection (SSI) prevention bundle, by specialty.
| Specialty | Trusts with local antibiotic prophylaxis guidelines (%) | Audit against antibiotic guidelines performed (%) | Trusts with local SSI prevention bundle (%) | Audit against SSI prevention bundle performed (%) |
| Breast surgery | 72.2 | 26.9 | 51.4 | 61.1 |
| Cardiothoracic surgery | 100.0 | 75.0 | 75.0 | 100.0 |
| Cranial neurosurgery | 80.0 | 50.0 | 20.0 | 100.0 |
| Ear, nose and throat | 69.2 | 12.5 | 8.3 | 50.0 |
| General surgery | 90.5 | 22.2 | 33.3 | 11.1 |
| Obstetrics and gynaecology | 73.7 | 33.3 | 55.0 | 23.1 |
| Ophthalmology | 83.3 | 31.3 | 83.3 | 40.0 |
| Oral and maxillofacial surgery | 87.5 | 42.9 | 57.1 | 0.0 |
| Orthopaedic surgery | 96.0 | 58.3 | 64.0 | 60.0 |
| Paediatric surgery | 66.7 | 28.6 | 16.7 | 20.0 |
| Spinal surgery | 71.4 | 20.0 | 66.7 | 33.3 |
| Urology | 90.9 | 10.0 | 20.0 | 0.0 |
| Vascular surgery | 100.0 | 25.0 | 62.5 | 16.7 |
| Total | 82.7 | 34.0 | 50.3 | 40.2 |
Discussion
Surveillance of surgical site infection with appropriate and timely feedback of data to clinicians is crucial in supporting strategies to reduce the burden of infection within the health system.9,10 A successful surgical site infection surveillance programme is said to require standardised definitions of infection, an effective surveillance methodology, adequate case risk stratification and timely feedback of results to surgeons and other key stakeholders.11
Promoting hospital participation in infection surveillance
In England, national surveillance of surgical site infections was established in 1997, with mandatory surveillance of infections in orthopaedic surgery introduced in 2004.7 Between 2016 and 2017, data for 17 surgical categories were captured from 201 NHS hospitals and 8 treatment centres by the PHE surveillance service. However, the majority of participants provided only data for the mandatory segment of the programme.2 For the non-mandatory surgical categories, the number of participating hospitals ranged from 7 (bile duct, liver or pancreatic surgery) to a maximum of 53 hospitals (large-bowel surgery). Furthermore, some specialties such as ear, nose and throat surgery, ophthalmology, oral and maxillofacial surgery and urology were not included.
Similar to the PHE national surveillance programme, the level of participation in the GIRFT surgical site infection survey was variable, but encouraging for a programme in its first year of implementation. The level of uptake may be attributable to the GIRFT methodology. The direct recruitment of doctors in training and other frontline healthcare professionals and support from specialty associations and senior clinical leadership at national and local trust levels have contributed to drive participation in the survey.
Unlike the PHE surveillance programme, GIRFT survey does not require participating hospitals to carry out active surveillance of surgical site infections. Rather, the GIRFT survey relies on participants reporting infections prospectively on diagnosis during clinical practice. One of the limitations of such approach is a possible lower case-finding sensitivity, probably more noticeable in superficial infections. However, the GIRFT methodology allows trusts to collect data more efficiently and is less resource intensive. The GIRFT methodology placed emphasis on creating a sense of ownership of the surveillance initiative among surgical staff, which can encourage cooperation in the subsequent use of data to drive improvements.11 Furthermore, there has also been a good level of uptake among specialties that are not currently included in other surveillance programmes, suggesting a previously unmet demand for infection surveillance within these specialties.
Data collection
Standardising definitions is undoubtedly one of the most crucial aspects in surgical site infection surveillance, ensuring that data captured are reliable and comparable between trusts to allow for the monitoring of trends. Surveillance has traditionally been led by infection control team with the deployment of specialist nurses. However, identification of surgical site infections following hospital discharge can be challenging. Methods of surveillance that have been described to identify infections include detection during post-discharge follow-up (e.g. patients attending wound clinics, reviewed at pre-arranged postoperative outpatient clinic appointments or in the community by health care professionals), as well as patient-reported infections captured in post-discharge wound-healing questionnaires.7 Routine prearranged postoperative outpatient clinic appointments are resource intensive, but patient-reported infections might not be identified consistently, depending on the return rate of the questionnaires.
During the development of the survey, it became apparent that surgeons may be unfamiliar with the PHE/CDC definitions of superficial, deep or organ/space identification and were more comfortable referring to specific types of infection (e.g. meningitis and ventriculitis in cranial neurosurgery and endocarditis in cardiothoracic surgery). This led to some exceptions being made in the terminology and definitions used in the GIRFT survey. It is important to ensure that infection surveillance results are relatable and meaningful to frontline clinicians. We suggest that improving education and increasing involvement of frontline clinicians in surveillance work is required and, indeed, such a move has been promoted in the GIRFT surgical site infection work.
Variations in clinical practice, infection rates and outcomes
Results of the GIRFT survey have identified variations in infection rates among trusts, both at specialty and procedural levels. When infection rates are presented at a specialty level, a high rate in one procedure may be offset by a lower rate in another procedure. It is therefore important for national surveillance programmes to present results at a procedural level, to avoid any masking of information.
Some types of variation are warranted and expected. It is recognised that differences in the practice of identification and reporting of infections can lead to variation in the rates reported by trusts.11 Furthermore, trusts employing high-quality post-discharge surveillance programmes may erroneously appear to be performing less well compared with trusts with low-quality surveillance leading to missed diagnoses of infections.13 It is important to understand that results from the GIRFT survey, while designed to provide trusts with benchmarking information, are not meant to penalise. Instead, the data are intended to provide information to support trusts in reviewing local practice and question the presence and cause of any unwarranted variation. For example, a general surgical unit reporting a high infection rate in elective hernia repairs (incisional) compared with the unit in a neighbouring trust may have a low compliance with local antibiotic guidelines and surgical site infection prevention bundle, which should prompt improvement efforts.
The importance of units auditing their own performance was demonstrated by the Department of Breast Surgery at the Royal Devon and Exeter NHS Foundation Trust, which conducted an audit in 2014 and identified an implant loss rate of 17%, compared with the national best practice rate of less than 5% at three months.14 Following a review, a protocol, developed in collaboration with their infection control and microbiology team to minimise points of infection in the implant reconstruction pathway, was introduced and successfully reduced the department’s implant loss rate to 0% at three months.14
While reviewing their own practice, surgical team should refer to the National Institute for Health and Care Excellence (NICE) guidelines on the prevention and treatment of surgical site infections, to consider evidence-based recommendations for pre-, peri- and postoperative interventions to minimise the risk of infection.15 In 2017, Guys and St Thomas’ NHS Foundation Trust shared their success with reductions of avoidable infections across their surgical specialties, following the implementation of surgical site infection surveillance and targeted interventions in line with NICE guidelines. In paediatric cardiac surgery, the infection rate decreased from 12.1% in 2009 to 0.7% in 2016. A similar reduction in rate was seen in adult gastrointestinal surgery, from 10.4% in 2009 to 3% in 2016.16
The observed trend towards higher infection rates reported by trusts performing lower volume work would support GIRFT’s call for introducing minimum critical volumes in surgery and regional planning to allocate low volume, complex cases to the most appropriate surgeon.5
The survey has demonstrated significant complications arising from surgical site infections, including reoperations, removals of implant, sepsis and even mortality. Delayed discharges and readmissions from infection can also lead to increased expenses for trusts, not to mention the emotional and financial cost to patients and staff of complaints, serious incidents, inquests and litigation which can arise. Guys and St Thomas’ NHS Foundation Trust estimated significant cost savings in excess of £1 million since the commencement of their surgical site infection programme, but it must be stressed that improving patient experience and quality of life is priceless.16 Similarly, it becomes unacceptable for a surgical unit to be unaware its own infection rate, depriving its patients of truly informed decision making when consenting for a procedure and its surgical team of the opportunity to improve patient care and reduce costs.
Limitations
The results of the GIRFT Surgical Site Infection Survey only reflect data submitted to us by participating trusts. Subjectivity in the interpretation of definitions and differences in methodology employed by local leads may influence the capture of data. Surgical site infection case-finding sensitivity may also be lowered due to the passive surveillance methodology employed by the GIRFT survey. Depending on the local set-up, cases may be missed (e.g. a patient admitted as an outlier rather than to the surgical ward or where patients presented to another trust not involved in the primary surgery).
Moreover, this survey was based at acute hospital trusts, there will be a selection bias of deep or organ/space surgical site infections over superficial infections, owing to the nature of patient presentation. Patients with superficial infections who present to local general practitioners or out-of-hours treatment centres and not reported back to the ‘primary operating trust’ may be missed. This highlights the importance of a more integrated care system between primary and secondary care. In order to provide better data sharing and learning opportunities to drive improvement in our services, a robust mechanism should be in place to ensure that trusts receive feedback regarding surgical site infection rates from the community.
HES data were used as a measure of activity and have been selected based on the procedural code and specialty code assigned by each trust. Inaccurate coding will have affected the denominator used for calculating infection rates. In addition, a proxy denominator was used, based on HES data for the survey period. This was to account for the complexity of retrospective data collection, due to the variable lag phase between infection developing and the date of the primary procedure. By doing so, we assumed that trust activity levels did not change significantly over the time period concerned, and that any trend in surgical activity was consistent nationally. We envisage that this issue can be resolved by the implementation of a robust system to collect local surgical site infection data prospectively.
Conclusion
The GIRFT surgical site infections programme has introduced a different approach to infection surveillance in England, extending surveillance to 13 surgical specialties and transferring ownership of surveillance work to frontline clinicians. Results of the survey has demonstrated variation in surgical site infection rates among surgical units. Much work remains to be done to improve surveillance across surgical units and trusts in England. Future efforts should include a move to integrate existing surveillance programmes; and promoting active surgical site infection surveillance such that it becomes routine business and the responsibility of all.
References
- 1.Badia JM, Casey AL, Petrosillo N et al. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 2017; : 1–15. [DOI] [PubMed] [Google Scholar]
- 2.Public Health England Surveillance of Surgical Site Infections in NHS Hospitals in England, 2016 to 2017. London: PHE; 2017. [Google Scholar]
- 3.National Joint Registry Reports. http://www.njrreports.org.uk (cited April 2019).
- 4.NICOR: The National Institute for Cardiovascular Outcomes Research. https://www.nicor.org.uk (cited April 2019).
- 5.Briggs T. Getting it Right First Time: A national review of adult elective orthopaedic services in England. London: British Orthopaedic Association; 2015. [Google Scholar]
- 6.NHS Resolution. Claims Management. https://resolution.nhs.uk/services/claims-management (cited April 2019).
- 7.Public Health England Protocol for the Surveillance of Surgical Site Infection. Version 6, June 2013. London: PHE; 2013. [Google Scholar]
- 8.Horan TC, Gaynes RP, Martone WJ et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am J Infect Control 1992; : 271–274. [DOI] [PubMed] [Google Scholar]
- 9.Rioux C, Grandbastien B, Astagneau P. Impact of a six-year control programme on surgical site infections in France: results of the INCISO surveillance. J Hosp Infect 2007; : 217–223. [DOI] [PubMed] [Google Scholar]
- 10.Haley RW, Culver DH, White JW et al. The efficacy of infection surveillance and control program preventing nosocomial infections in US hospitals. Am J Epidemiol 1985; : 182–205. [DOI] [PubMed] [Google Scholar]
- 11.Smyth ET, Emmerson AM. Surgical site infection surveillance. J Hosp Infect 2000; : 173–184. [DOI] [PubMed] [Google Scholar]
- 12.Singh S, Davies J, Sabou S et al. Challenges in reporting surgical site infections to the national surgical site infection surveillance and suggestions for improvement. Ann R Coll Surg Engl 2015; : 460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanner J, Padley W, Kiernan M et al. A benchmark too far: findings from a national survey of surgical site infection surveillance. J Hosp Infect 2013; : 87–91. [DOI] [PubMed] [Google Scholar]
- 14.Youssef MMG, Rees-Lee J, Burden M et al. Re: Infection prevention in implant surgery: a review of the surgical evidence, guidelines and a checklist. Eur J Surg Oncol 2016; : 591–603. [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence Surgical Site Infections: Prevention and Treatment. (Clinical Guideline CG74). London: NICE; 2008. [PubMed] [Google Scholar]
- 16.Guys and St Thomas’ NHS Foundation Trust Successful implementation of NICE guidance and quality standard for prevention and treatment of surgical site infection. https://www.nice.org.uk/sharedlearning/successful-implementation-of-nice-ssi-guidance-and-quality-standard (cited April 2019).