Abstract
Introduction
We aimed to enhance the emergency general surgical service in our high-volume centre in order to reduce four-hour target breaches, to expedite senior decision making and to avoid unnecessary admissions.
Materials and methods
The aggregation of marginal gains theory was applied. A dual consultant on-call system was established by the incremental employment of five emergency general surgeons with a specialist interest in colorectal or oesophagogastric surgery. A surgical ambulatory care unit, which combines consultant-led clinical review with dedicated next-day radiology slots, and a dedicated working week half-day gastrointestinal urgent theatre session were instituted to facilitate ambulatory care pathways.
Results
The presence of two consultant surgeons being on call during weekday working hours decreased the four-hour target breaches and allowed consultant presence in the surgical ambulatory care clinic and the gastrointestinal urgent theatre list. Of 1371 surgical ambulatory care clinic appointments within 30 months, 1135 (82.7%) avoided a hospital admission, corresponding to savings of £309,752 . The coordinated functioning of the surgical ambulatory care clinic and the gastrointestinal urgent theatre list resulted in statistically significantly reduced hospital stays for patients operated for abscess drainage (gastrointestinal urgent theatre median 11 hours (interquartile range 3, 38) compared with emergency median 31 hours (interquartile range 24, 53), P < 0.001) or diagnostic laparoscopy/appendicectomy (gastrointestinal urgent theatre median 52 hours (interquartile range 41, 71) compared with emergency median 61 hours (interquartile range 43, 99), P = 0.005). Overnight surgery was reduced with only surgery that was absolutely necessary occurring out of hours.
Conclusion
The expansion of the ‘traditional’ on-call surgical team, the establishment of the surgical ambulatory care clinic and the gastrointestinal urgent theatre list led to marginal gains with a reduction in unnecessary inpatient stays, expedited decision making and improved financial efficiency.
Keywords: Emergency general surgery, Ambulatory clinic, Marginal gains
Introduction
The theory of the aggregation of marginal gains has been credited to Sir Dave Brailsford, who transformed British cycling and led his team to the astonishing success of 16 gold medals in two Olympic Games. The principle of the aggregation of marginal gains came from the idea that if you improve every area related to cycling by 1%, then those small marginal gains can add up to a remarkable improvement.1 This concept has the potential to be applied to any complex process within business, education and healthcare.2 The aggregation of marginal gains has been successfully employed for the refinement of enhanced recovery programs within urology and cardiac surgery.3,4 The National Enhanced Recovery Partnership consensus statement recognises the application of the aggregation of marginal gains within the entire perioperative patient journey.5
Hence, in the modern NHS, emergency surgical patients are not admitted to hospital by default but, instead, should be assessed by surgeons in the frontline, treated within ambulatory care pathways and operated in dedicated urgent theatre lists.6–9 The reorganisation of the emergency general surgical service has led to the development of consultant posts in emergency general surgery whose main focus is delivering and leading the management of the emergency general surgery service.6,10 A joint statement from the Association of Surgeons, the Association of Upper Gastro-intestinal Surgeons and the Association of Coloproctology of Great Britain and Ireland (ASGBI/AUGIS/ACPGBI) has defined eight different constituent components of the emergency surgery service.10 These eight components include a ‘front door’ senior surgeon to triage admission, ‘hot’ clinic service, assessment and care of emergency in-patients, acute abscess/appendix/biliary/laparotomy service, weekend review of complex elective in-patients and provision of specialised emergency surgery services.10
The reorganisation of the emergency general surgical service at our institution concentrated on three main refinements that provided incremental gains to all constituents of the emergency service. The changes that were implemented included the availability of two consultant surgeons being on call during weekday working hours, the set-up of a surgical ambulatory ‘hot’ clinic and a weekday half-day dedicated general surgical emergency theatre and seven-day consultant-delivered inpatient ward care.
Materials and methods
The hospital setting
Cambridge University Hospital NHS Foundation Trust is a major trauma and tertiary referral centre. The hospital offers emergency and elective surgical care in the specialist areas of colorectal, upper gastrointestinal/oesophagogastric, hepatopancreaticobiliary, transplant, vascular, urology, plastic, orthopaedic and paediatric surgery. The general surgical on-call service is provided by the colorectal and upper gastrointestinal subspecialties. The hepatopancreaticobiliary team has an independent specialist on-call resident team and rota, which provides subspecialty input for emergency patients following admission on the general surgical take, or accepts patients directly following a subspecialty regional referral.
The consultant surgeons leading and delivering emergency surgery
In our unit, five emergency general surgery consultants work in a rolling rota and provide an emergency surgery service during the day time in the working week. Initially, two consultant emergency general surgeons were employed but their number increased to five in 2018. Each of these consultants has one emergency general surgery duty week every five weeks, with the remaining four weeks spent providing specialist elective care, either in colorectal or upper gastrointestinal (including cancer multidisciplinary team work). Apart from the emergency surgery week duty, the consultants also contribute to the 1 in 14 gastrointestinal 24-hour or weekend on-call rota. Our unit is also staffed by another eight colorectal and four upper gastrointestinal consultant surgeons who participate in the emergency general surgical service cover by 24-hour on-calls during weekdays or for 48 hours at the weekends.
The daily emergency general surgical service is led by two consultant surgeons who are on duty during weekday working hours (i.e. the emergency general surgery consultant working between 7.30am and 5.30pm and the on-call consultant completing the on-call for 24 hours). As per College policy, the consultant surgeons covering the emergency general service are free of any elective commitments during their duty.11 Although there is no formal arrangement for the two consultants who are on call to be of different subspecialties, the alternating subspecialty of the 24-hour on-call consultant allows subspecialty cover for at least 50% of the working week. If, for example, there is a need for colorectal subspecialty opinion or input when there are two upper gastrointestinal consultants on call, then the colorectal consultant responsible for the ward round of the colorectal patients may provide the subspecialty input required. The employment of five emergency general surgery surgeons allowed both the reorganisation of the emergency general surgical service and the provision of subspecialty consultant ward round on a daily basis including weekends. Hence, our model meets the ASGBI/AUGIS/ACPGBI recommendation for weekend review of complex elective inpatients and provision of specialised emergency surgery services.10
The surgical ambulatory care unit
A ‘hot’ clinic service incorporating an acute abscess, appendix and biliary service has been described as one of the multiple component tasks of the emergency general surgical service.10,11 A surgical ambulatory care unit was created in January 2016 offering ‘hot clinic’ weekday appointments. The unit is based on the daycase surgical ward. It comprises a chaired waiting area, a single examination room and a clinical office shared by the consultant and a nurse. Referral to the unit is via the colorectal or upper gastrointestinal consultant on call, the emergency general surgery consultant or the surgical registrar on call. The afternoon clinic is primarily led by the emergency general surgery on-call consultant. However, should there be a need for a subspecialty opinion, the emergency general surgery consultant will liaise with the 24-hour on call consultant to achieve an efficient service with provision of subspecialty input if required.
The patients are referred to the surgical ambulatory care unit for consultant-led review with dedicated next day ultrasound slots to expedite diagnosis. Patients can be deferred from their general practitioner or the emergency department for a next-day consultant-led surgical ambulatory care unit ‘hot clinic’ or can be seen in the emergency department and discharged for ‘hot clinic’ follow-up, investigation and review. Three main pathways were initially produced, covering abscesses, right iliac fossa pain and presumed biliary disease. However, adult patients with postoperative problems, such as wound infections requiring urgent attention, non-specific abdominal pain or painful but non-obstructed hernias may also receive a timely surgical review in the unit.
The gastrointestinal urgent theatre session
A gastrointestinal urgent theatre session, which is a half-day weekday morning theatre list dedicated to general surgery, was created in 2016. The patients listed for the gastrointestinal urgent theatre session are patients who are stable and ambulatory, and have previously been assessed in the emergency department or in the surgical ambulatory care clinic and require an urgent operation. The gastrointestinal urgent theatre list may also accommodate inpatients awaiting an operation on the emergency list but not necessarily requiring the procedure to be performed overnight.
Therefore, the gastrointestinal urgent theatre list includes ambulatory urgent cases such as laparoscopic appendicectomy, abscess drainage, hernia repair and ‘hot’ laparoscopic cholecystectomy, as well as expedited specialist operations such as laparoscopic subtotal colectomy for colitis, re-look emergency/trauma laparotomy or oesophagogastric endovac therapy changes. The emergency general surgery consultant or the colorectal/upper gastrointestinal on-call consultant delivers or supervises the cases on the gastrointestinal urgent theatre list or the emergency theatre. There is no set arrangement with regards to which of the two on-call consultants operates on the emergency list or the gastrointestinal urgent theatre list. It is not uncommon that there are general surgical cases running on both the gastrointestinal urgent theatre and the emergency lists in the mornings. The on-call consultants work efficiently together as a team and allocation of cases is based on subspecialty interest.
Statistical analysis
Data analysis was performed using Microsoft Excel and Graphpad Prism version 7. Data were not normally distributed so median and interquartile ranges (IQR) were used for descriptive statistics. The Mann–Whitney U test was the non-parametric test used to assess significance of independent data with unequal variances. Two-tailed P-values were used and the significance level of P < 0.05 was set.
Results
Emergency general surgical service run by two consultant surgeons
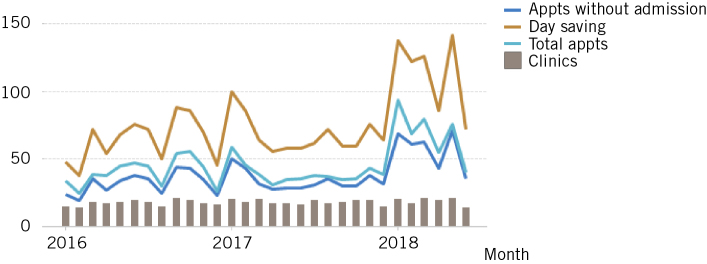
Several breaches of the four-hour emergency department target were attributed to general surgery at the beginning of 2017. As shown in Figure 1, the median value of weekly breaches was 49 (IQR 37.25, 51.75) for the first 10 weeks of 2017. During this period, one consultant general surgeon was on call with a surgical registrar, a core surgical trainee or foundation year 2 doctor, and a foundation year 1 doctor. Following the introduction of two consultant surgeons being on duty during the weekday working hours of 7.30am to 5.30pm, the weekly median number of four-hour target breaches attributed to general surgery decreased to five (IQR 3, 14.75). The reduction of emergency department breaches attributed to general surgery was a reflection of the emergency general surgical service reorganisation from March 2017 onwards. This result was not due to lower winter pressures, as the overall weekly number of emergency department attendances remained unchanged during the first 20 weeks of 2017.
Figure 1.
Emergency department four-hour target breaches attributed to general surgery on a weekly basis between January and May 2017. The change in colour of the column chart shows the time point of introduction of two consultant surgeons being on duty from week 11 in March 2017 onwards.
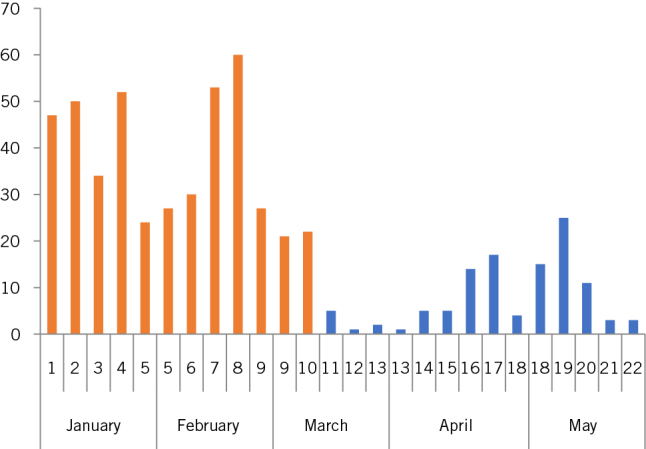
The surgical ambulatory care unit
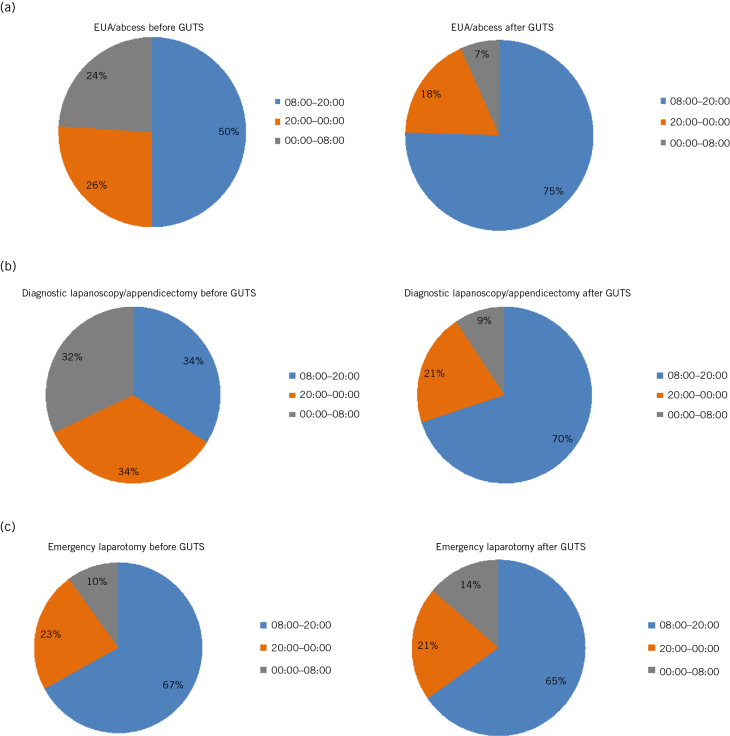
A total of 1371 clinic appointments were attended between January 2016 and June 2018 with a median of 10 (IQR 8, 14) appointments a week. A representative age distribution of the patients attending clinic in a three-month period is shown in Figure 2. The majority of the ambulatory patients had no major comorbidities and were between the ages of 20 and 40 years. Of these 1371 visits, 1135 appointments (82.7%) avoided a hospital admission (Fig 3). A total of 2498 bed days were saved over 30 months of the clinic’s operation, corresponding to savings of £309,752.
Figure 2.
Age distribution of ambulatory surgical patients attending surgical ambulatory care clinic in a three-month period. The figure that shows the majority of ambulatory patients were between the ages of 20 and 40 years.
Figure 3.
Surgical ambulatory care clinic appointments between January 2016 and June 2018. The figure shows the total number of appointments attended in the clinic on a monthly basis against the appointments avoiding admission and the total bed days saved.
The gastrointestinal urgent theatre list
The gastrointestinal urgent theatre list has operated for 24 months since its implementation, with an overall use of 73%. Some 864 general surgical cases were performed on the gastrointestinal urgent theatre list from 1 June 2016 to 31 May 2018. During the same time period, a further 1522 emergency general surgical cases were carried out within the emergency list that is shared with several other surgical subspecialties. The patient demographics and numbers of index cases, such as appendicectomy, examination of rectum under anaesthesia (EUA)/abscess drainage and laparotomy, occurring either on the gastrointestinal urgent theatre list or the emergency list are shown in Table 1. These three surgical procedures were chosen for comparison as they account for two-thirds of the total emergency workload.12
Table 1.
Demographic characteristics of surgical patients undergoing urgent or emergency operations between June 2016 and end of May 2018.
| Cases | GUTS list vs emergency list (n) | Men (n) | Women (n) | Median age (years) | |
| (n) | IQR | ||||
| Overall: | |||||
| GUTS list | 864 | 413 | 451 | 43 | (27, 60) |
| Emergency lista | 1522 | 789 | 733 | 46 | (28, 67) |
| Laparoscopy/appendicectomy: | |||||
| GUTS list | 171 | 73 | 98 | 30 | (22, 46) |
| Emergency lista | 395 | 214 | 181 | 33 | (22, 48) |
| EUA/abscess:b | |||||
| GUTS list | 145 | 90 | 55 | 34 | (24, 47) |
| Emergency lista | 181 | 112 | 69 | 31 | (23, 46) |
| Laparotomy: | |||||
| GUTS list | 50 | 23 | 27 | 58 | (45, 75) |
| Emergency lista | 444 | 234 | 210 | 65 | (47, 77) |
a Emergency cases were censored for the general surgical consultants participating in the on-call general surgical rota and did not include emergency general surgical cases of the hepatopancreaticobiliary team or paediatric cases.
b Cases of examination of rectum under anaesthetic were included, as were fistula-in-ano cases and abscesses (e.g. axillary, perianal, ischiorectal).
EUA, examination of rectum under anaesthesia; GUTS, gastrointestinal urgent theatre session; IQR, interquartile ratio.
The implementation of the gastrointestinal urgent theatre list significantly reduced the hospital stay for patients having an EUA/abscess procedure or laparoscopy/appendicectomy. A total of 85 of the 145 patients (58.6%) who had an EUA/abscess procedure on the gastrointestinal urgent theatre list were discharged home after initial assessment and returned to hospital for their operation to be performed on a dedicated gastrointestinal urgent theatre slot on a different day. In view of this, and as expected, the cases performed on the gastrointestinal urgent theatre list had a significantly higher median time from case creation to the patient arriving in the anaesthetic room compared with cases on the emergency list (Table 2). On the other hand, the median hospital stay for patients having an EUA/abscess procedure on the gastrointestinal urgent theatre list was significantly reduced compared with the main emergency list (11 vs 31 hours, P < 0.001). Of the 145 patients, 85 (58.6%) from the gastrointestinal urgent theatre list having EUA/abscess drainage were discharged within 23 hours of their admission. On the other hand, 39 of 181 patients (21.5%) who had an EUA/abscess drainage on the emergency list were discharged home within 23 hours of admission. Similarly, the hospital stay for patients having laparoscopy/appendicectomy on the gastrointestinal urgent theatre list was significantly reduced compared with the patients having the procedure on the emergency list (median 52 vs 61 hours, P = 0.005).
Table 2.
The table shows the median hospital stay and the median time from case creation to the anaesthetic room for cases performed on the GUTS or the emergency list.
| Cases | Time from case creation to anaesthetic room (hours) | P-valuea | Hospital stay (hours) | P-valuea | ||
| (median) | (IQR) | (median) | (IQR) | |||
| EUA/abscess: | ||||||
| Emergency list | 14.1 | (6.5, 20.9) | < 0.0001 | 31 | (24, 53) | < 0.001 |
| GUTS list | 19.2 | (13.3, 22) | 11 | (8, 38) | ||
| Laparoscopy/appendicectomy: | ||||||
| Emergency list | 9.7 | (5, 18.6) | 0.0013 | 61 | (43, 99) | 0.005 |
| GUTS list | 13.7 | (9, 18.2) | 52 | (41, 71) | ||
| Laparotomy: | ||||||
| Emergency list | 3 | (1.4, 8.9) | < 0.0001 | 14 | (8, 29) | 0.047 |
| GUTS list | 22.5 | (12, 33.3) | 21 | (10, 38) | ||
a The non-parametric Mann–Whitney U test was used to assess statistical significance.
EUA, examination of rectum under anaesthesia; GUTS, gastrointestinal urgent theatre session; IQR, interquartile ratio.
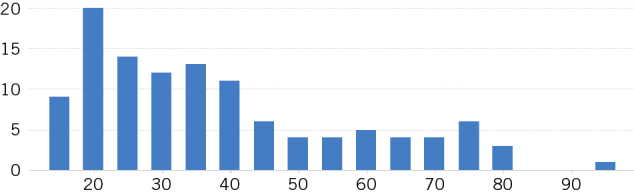
The introduction of the gastrointestinal urgent theatre list resulted in a significant reduction in unnecessary overnight operating with the majority of urgent laparoscopies/appendicectomies and abscess cases taking place during day time hours. Prior to the gastrointestinal urgent theatre list in June 2016, 50% of EUA/abscess procedures and 66% of the diagnostic laparoscopies/appendicectomies were performed between 8pm and 8am because of limited emergency daytime theatre capacity shared by several other surgical subspecialties in our high-volume centre (Figure 4a,b). With the gastrointestinal urgent theatre list, the majority of the urgent EUA/abscesses and diagnostic laparoscopies/appendicectomies (75% and 70%, respectively) were performed during the day, whereas only the cases of septic or unwell patients who really required an emergency procedure were carried out overnight. Figure 4c shows that the emergency laparotomy rates remained unchanged during the daytime or out of hours, confirming that the emergency cases needed to be performed overnight continued to take place, whereas the gastrointestinal urgent theatre list was appropriately employed for urgent cases that safely occurred during the daytime.
Figure 4.
Percentage of cases performed before and after the introduction of the gastrointestinal urgent theatre sessions (GUTS) occurring for two years prior and two years following the implementation of the list: (a) examination of rectum under anaesthesia(EUA)/abscess; (b) diagnostic laparoscopies/appendicectomies; (c) laparotomies.
Discussion
We applied the aggregation of marginal gains to enhance the emergency general surgical service at our high-volume institution. After recognising the constituent components of the emergency service,10 we proceeded with the employment of five emergency general surgery consultants, the provision of an ambulatory surgical ambulatory care clinic and the introduction of a half-day weekday dedicated urgent gastrointestinal urgent theatre list. In addition, we also incorporated seven-day consultant-delivered inpatient ward care during this time.
Anderson recognised that a single duty surgeon taking direct personal responsibility for every component of the emergency surgery service would not be reliable in high-volume units, owing to the increased workload.10 The modern NHS is calling for consultant-delivered care, which is defined as the ready availability of a consultant for direct patient care responsibility that may not necessarily equate to 24-hour consultant presence.9,13 Consultant-delivered care has been shown to promote timely surgical decision making and result in faster patient processing.7 The 2006 New Zealand junior doctors strike forced consultants to act on the front line leading to faster patient processing and reduced length of stay.14 Similarly, the implementation of an acute care emergency surgical service in Canada resulted in 15% reduction in surgical decision time and improved emergency department crowding.15 The ‘traditional’ on-call team, with one gastrointestinal consultant surgeon being on call, was not enough to provide consultant-delivered care at our high-volume centre. The reorganisation of the service led to two consultants being on duty during weekday working hours alongside an independent on-call consultant for hepatopancreaticobiliary and vascular surgery. The presence of senior surgical decision making in emergency department led to an immediate reduction of the four-hour target breaches that were attributed to general surgery.
The ASGBI/AUGIS/ACPGBI joint document on emergency surgical service advises on the importance of specialised emergency surgery services (e.g. trauma, hepatopancreaticobiliary, specialist upper gastrointestinal, specialist colorectal) for large units.10 The increase in the number of emergency general surgery consultants with subspecialist interest in either colorectal or upper gastrointestinal surgery supplemented the pool of expertise in colorectal, upper gastrointestinal or hepatopancreaticobiliary consultants already present in the provision of specialised emergency surgery and trauma services. In practice, this also led to the provision of specialist consultant daily ward rounds of surgical inpatients and the development of the acute biliary service with patients having a ‘hot’ laparoscopic cholecystectomy by specialist surgeons on the gastrointestinal urgent theatre list.
A dual consultant on-call system not only allowed front-line senior surgical decision making but also promoted the parallel running of the surgical ambulatory care clinic and the development of ambulatory patient pathways. Within 30 months of set-up, the surgical ambulatory care clinic accommodated 1371 attendances and helped to avoid 1135 (82.7%) admissions, which translates to savings of £309,752. Tierney et al have previously reported that 69% of their ambulatory clinic appointments avoided a hospital admission.8 The ambulatory clinic at the Bath Royal United Hospital reported a 25% reduction in the daily number of their acute surgical admissions with an estimated reduction in patient bed stays of 130 a month, corresponding to annual savings of approximately £500,000.9
The gastrointestinal urgent theatre list was instituted with the availability of two consultant surgeons being on duty and resulted in enhanced senior-led daytime operating. As expected, the median time from case creation to the patient arriving in the anaesthetic room was higher for the cases performed on the gastrointestinal urgent theatre list compared with those on the emergency list (Table 2), as these patients were treated in an ambulatory fashion. If there was a concern of significant pain or sepsis then the patient would remain an inpatient and surgery would be performed on the emergency list. The higher number of EUA/abscesses performed on the emergency list compared with the gastrointestinal urgent theatre list (i.e. 181 vs 145, as shown in Table 1) is largely a result of facilitating ambulatory pathways appropriately but without compromising patient safety. On the other hand, the hospital stay for patients having an EUA/abscess drainage or their laparoscopy/appendicectomy performed on the gastrointestinal urgent theatre list was significantly shorter than that of the patients having their surgery on the emergency list. In particular, 58.6% of the patients having an EUA/abscess drainage on the gastrointestinal urgent theatre list were ambulated and admitted on the day of their planned urgent operation. The same percentage of patients (but not necessarily the same patients) operated on the gastrointestinal urgent theatre list were discharged within 23 hours of admission.
Studies from the 1990s identified that up to one-third of the general surgical operations occurring overnight could be safely deferred to the daytime and advocated that dedicated daytime theatre access results in significant reduction of unnecessary overnight operating.16–18 The National Confidential Enquiry into Perioperative Deaths with the Who Operates When? audit advised on moving away from out-of-hours operating, increased consultant presence for emergency cases and higher availability of dedicated daytime emergency lists.19 The second cycle of the Who Operates When? audit showed increased consultant participation overnight (26% vs 11%) and improved availability of dedicated daytime emergency theatre lists (63% vs 51%).19 Subsequently, the ASGBI/AUGIS/ACPGBI joint document advised on defined urgent theatre slots separate from parallel emergency and elective lists to provide the consultant-delivered acute abscess/appendix/biliary service.10
As shown in Figure 4, the introduction of the gastrointestinal urgent theatre list led to a clear decrease in overnight operating. Significant numbers of emergency appendicectomies and EUA/abscesses were previously occurring after midnight in an attempt to clear the backlog of a competitive emergency list. Figures 4a and 4b show that more than two-thirds of the EUA/abscess drainages and diagnostic laparoscopies/appendicectomy previously occurred between 8am and midnight. With the gastrointestinal urgent theatre list, the same percentage of these procedures took place between the hours of 8am and 8pm. On the other hand, the results from the laparotomy cases showed no major difference in the percentages being performed overnight after the introduction of the gastrointestinal urgent theatre list. This was an expected finding because the urgency and the clinical requirement for an emergency laparotomy to happen should not be affected by the operation of the gastrointestinal urgent theatre list.
Our results are in line with those reported by other groups. An Australian group with a consultant-led emergency service reported a statistically significant increase in the appendicectomies performed within hours (64.4% vs 54.3%) with no change in hospital stay.20 A Canadian team reported 70% of emergency procedures being performed between 7.30am and 5.30pm with the implementation of an acute care model compared with 55.4% previously and a 14% reduction in overnight operating.21 A Finnish group that used three dedicated daytime operating theatres reported 85.4% emergency theatre time and a reduction in night-time operating from 27.4% to 23.5%.22
Leppaniemi argues the need for emergency surgery to be recognised as a formal specialty, but also identifies the requirement for such a specialty to be made popular enough in order to attract an adequate workforce.6 Our model of emergency general surgical care is novel and provides excellent supervised training opportunities for surgical trainees to enthuse them into the specialty. Specialist trainees can be supervised in their decision making in the frontline, their interactions with primary care, their assessment of surgical patients in the ambulatory clinic and on technical skills training within a high volume of emergency laparotomies and trauma cases. Similarly, our emergency general surgical service model promotes the continuous professional development of the emergency general surgery consultants within their subspecialty interest. This model is attractive because it not only involves being an emergency surgeon but also allows time for elective career advancement and recognition with elective work in four of five working weeks, including multidisciplinary membership. In turn, allowing the emergency general surgeons to develop a specialist elective interest can only augment the emergency service by bringing their specialist skills to potentially complex emergency work.10
Conclusion
The enhancement of our emergency general surgical service was successful following the introduction of a dual consultant daytime on call, the set-up of the surgical ambulatory care clinic and the operation of the gastrointestinal urgent theatre list. This was done in tandem with the introduction of seven-day consultant-delivered inpatient ward care. These main changes resulted in the availability of front-door senior surgical decision making, the provision of specialist input for emergency surgical patients, the daily specialist consultant ward round of surgical inpatients and the refinement of the acute abscess, biliary, appendix and emergency laparotomy services. Therefore, these initial changes provided marginal gains in all eight constituent components of the emergency surgical service as advised by the ASGBI/AUGIS/ACPGBI joint document, which led to an overall significant improvement in efficiency, as well as financial savings.
Acknowledgements
We would like to thank Mrs Gill Love, Operations Manager at Addenbrooke’s Hospital for her help and support with this service improvement project.
References
- 1.Slater M. Olympics cycling: marginal gains underpin Team GB dominance. BBC Sport, 8 August 2012 http://www.bbc.co.uk/sport/0/olympics/19174302 (cited April 2019).
- 2.Harrell E. How 1% Performance Improvements Led to Olympic Gold. Harvard Business Review 30 October 2015 https://hbr.org/2015/10/how-1-performance-improvements-led-to-olympic-gold. (cited April 2019).
- 3.Smith J, Meng ZW, Lockyer R et al. . Evolution of the Southampton Enhanced Recovery Programme for radical cystectomy and the aggregation of marginal gains. BJU Int 2014; : 375–383. [DOI] [PubMed] [Google Scholar]
- 4.Flemming IO, Garratt C, Guha R et al. . Aggregation of marginal gains in cardiac surgery: feasibility of a perioperative care bundle for enhanced recovery in cardiac surgical patients. J Cardiothorac Vasc Anesth 2016; : 665–670. [DOI] [PubMed] [Google Scholar]
- 5.NHS Improving Quality, NHS England Enhanced Recovery Care Pathway: A Better Journey for Patients Seven Days a Week and Better Deal for the NHS, Progress Review (2012/13) and Level of Ambition (2014/15). Leeds: NHS IQ; 2013. [Google Scholar]
- 6.Leppaniemi A. Organization of emergency surgery. BJS 2014; : e7–e8. [DOI] [PubMed] [Google Scholar]
- 7.Bergenfelz A, Soreide K. Improving outcomes in emergency surgery. BJS 2014; : e1–e2. [DOI] [PubMed] [Google Scholar]
- 8.Tierney GM, Tou S, Hender J, Lund JN. Pilot study of a new paradigm in the management of surgical emergencies using emergency surgery ambulatory care. Ann R Coll Surg Engl (Suppl) 2014; : 198–201. [Google Scholar]
- 9.Rance C, Richards SK, Jones AE. Front door surgeons: the rise of consultant-delivered acute surgical care. Br J Gen Pract 2016; : 234–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Association of Coloproctology of Great Britain and Ireland, Association of Upper Gastro-Intestinal Surgeons & Association of Surgeons of Great Britain and Ireland . The Future of Emergency General Surgery. A Joint Document. London: ACGBI; 2015. [Google Scholar]
- 11.Royal College of Surgeons Separating Emergency and Elective Surgical Care. London: RCS; 2007. [Google Scholar]
- 12.Faiz O, Banerjee S, Tekkis P et al. . We still need to operate at night! World J Emerg Surg 2007; : 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Academy of Medical Royal Colleges The Benefits of Consultant-Delivered Care. London: AoMRC; 2012. [Google Scholar]
- 14.Robinson G, McCann K, Freeman P, Beasley R. The New Zealand national doctors’ strike, implications for the provision of acute medical services. Clin Med 2008; : 272–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qureshi A, Smith A, Wright F et al. . The impact of an acute care emergency surgical service on timely surgical decision-making and emergency department overcrowding. J Am Coll Surg 2011; : 284–293. [DOI] [PubMed] [Google Scholar]
- 16.McKee M, Priest P, Ginzler M, Black N. Which general surgical operations must be done at night? Ann R Coll Surg Engl 1991; : 295–302. [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow AP, Wilkinson DA, Wordsworth M, Eyre-Brook IA. An emergency daytime theatre list: utilisation and impact on clinical practice. Ann R Coll Surg Engl 1993; : 441–444. [PMC free article] [PubMed] [Google Scholar]
- 18.Lovett BE, Katchburian MV. Emergency surgery: half a day does make a difference. Ann R Coll Surg Engl 1999; : 62–64. [PMC free article] [PubMed] [Google Scholar]
- 19.National Confidential Enquiry into Perioperative Deaths Who Operates When? London: NCEPOD; 2003. [Google Scholar]
- 20.Suen K, Hayes IP, Thomson BNJ, Shedda S. Effect of the introduction of an emergency general surgical service on outcomes from appendicectomy. BJS 2014; : e141–e146. [DOI] [PubMed] [Google Scholar]
- 21.Britt RC, Weireter LJ, Britt LD. Initial implementation of an acute care surgery model: implications for timeliness of care. J Am Coll Surg 2009; : 421–424. [DOI] [PubMed] [Google Scholar]
- 22.Leppaniemi A, Jousela I. A traffic-light coding system to organize emergency surgery across surgical disciplines. BJS 2014; : e134–e140. [DOI] [PubMed] [Google Scholar]