Abstract
Kneeling ability is consistently the poorest patient-rated outcome after total knee replacement (TKR), with 60–80% of patients reporting difficulty kneeling or an inability to kneel.
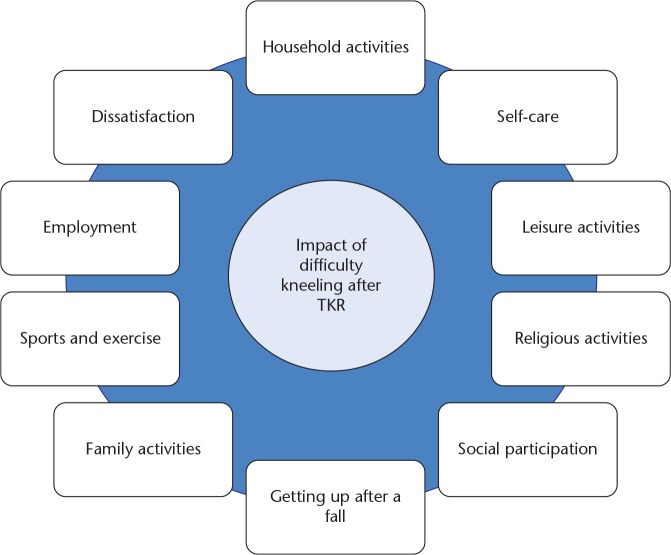
Difficulty kneeling impacts on many activities and areas of life, including activities of daily living, self-care, leisure and social activities, religious activities, employment and getting up after a fall. Given the wide range of activities that involve kneeling, and the expectation that this will be improved with surgery, problems kneeling after TKR are a source of dissatisfaction and disappointment for many patients.
Research has found that there is no association between range of motion and self-reported kneeling ability. More research is needed to understand if and how surgical factors contribute to difficulty kneeling after TKR.
Discrepancies between patients’ self-reported ability to kneel and observed ability suggests that patients can kneel but elect not to. Reasons for this are multifactorial, including knee pain/discomfort, numbness, fear of harming the prosthesis, co-morbidities and recommendations from health professionals. There is currently no evidence that there is any clinical reason why patients should not kneel on their replaced knee, and reasons for not kneeling could be addressed through education and rehabilitation.
There has been little research to evaluate the provision of healthcare services and interventions for patients who find kneeling problematic after TKR. Increased clinical awareness of this poor outcome and research to inform the provision of services is needed to improve patient care and allow patients to return to this important activity.
Cite this article: EFORT Open Rev 2019;4:460-467. DOI: 10.1302/2058-5241.4.180085
Keywords: kneeling, outcomes, total knee replacement
Introduction
The primary reasons that patients elect to undergo total knee replacement (TKR) are to gain improvements in pain and walking ability.1 However, patients often have high expectations of the outcome of their TKR and want more from their operation than pain relief and improvement in basic mobility.2 This includes a return to important higher function activities, such as kneeling.1–3 The majority of patients expect to be able to kneel after TKR,2,4,5 however, these expectations are frequently not met,1,6 with between 50% and 80% of patients reporting that they have difficulty kneeling or do not kneel in the months and years after TKR.7–14 An inability to kneel can have a detrimental impact on many activities and areas of life and is a source of dissatisfaction. Despite this, kneeling ability after TKR is an underacknowledged outcome, and has received little attention in the research literature. The aim of this instructional review article is to raise awareness of this problematic outcome and provide a comprehensive overview of prevalence, impact, aetiology, management and directions for future research.
Prevalence
Kneeling is considered as one of the most important but also most difficult to do activities for patients with TKR,7,15–19 and is the poorest patient-rated outcome after TKR.8,20-23 An overview of cohort studies assessing the prevalence of kneeling difficulties after TKR is provided in Table 1. Prior to TKR surgery, the majority of patients experience difficulty kneeling on their osteoarthritic knee,9–11,24 and post-operative improvements in kneeling ability are rarely achieved for most patients.9 These problems with kneeling continue for many years after surgery, with 67% of patients reporting difficulty with kneeling at five years post-operatively.11 Compared to older people with no knee disorders, significantly more people with TKR have difficulty kneeling.15 Therefore, kneeling difficulty is the most prevalent poor patient-reported outcome after TKR.
Table 1.
Overview of prevalence of kneeling difficulties after total knee replacement from cohort studies
| Study and country | Numbers of patients and post-operative time point(s) | Kneeling assessment | Findings |
|---|---|---|---|
| Artz et al, 20159
UK |
196 patients at 1 year 184 patients at 2 years |
OKS kneeling question | 63% extreme difficulty or impossible at 1 year 65% extreme difficulty or impossible at 2 years |
| Baker et al, 20078
UK |
8231 patients at ⩾ 1year | OKS kneeling question | 57% much difficulty or impossible |
| Benfayed et al, 201714
UK |
251 patients at 1 year | Difficulty performing four kneeling positions | Upright kneeling on operated knee: 63% extreme difficulty or impossible Upright kneeling on both knees: 67% extreme difficulty or impossible Kneeling at full flexion: 87% extreme difficulty or impossible Kneeling with hands on ground: 74% extreme difficulty or impossible (estimated from graph) |
| Dawson et al, 199823
UK |
87 patients at 6 months | OKS kneeling question | 62% extreme difficulty or impossible at 6 months |
| Hassaballa et al, 200310
UK |
109 TKRs at 1 year 75 TKRs at 2 years |
OKS kneeling question | 58% extreme difficulty or impossible at 1 year 56% extreme difficulty or impossible at 2 years |
| Roos et al, 200313
Sweden |
97 patients at 6 months |
KOOS kneeling question | 74% patient did not kneel at 6 months |
| Sharkey et al, 201112
USA |
49 patients at 3 weeks to 5 years | Single question on presence of kneeling difficulties | 82% difficulty kneeling |
| Weiss et al, 20027
USA |
176 patients ⩾ 1year post-op | Question within Knee Function Survey | 72% had some knee symptoms when kneeling |
| Wylde et al, 201711
UK |
245 patients at 3 months 236 patients at 1 year 219 patients at 2 years 231 patients at 3 years 210 patients at 5 years |
Single item question on difficulty kneeling | 58% much difficulty or impossible at 3 months 65% much difficulty or impossible at 1 year 69% much difficulty or impossible at 2 years 69% much difficulty or impossible at 3 years 67% much difficulty or impossible at 5 years |
Notes. OKS, Oxford Knee Score; KOOS, Knee injury and Osteoarthritis Outcome Score
Although it is evident from the existing literature that kneeling difficulties are highly prevalent after TKR, there are complexities and variability in kneeling ability which are often not captured. The majority of studies assess self-reported kneeling, commonly by using the kneeling question on the Oxford Knee Score which asks about the amount of difficulty experienced with kneeling down and getting up again afterwards.23 This provides a basic estimate of kneeling difficulty but does not account for factors that can affect a persons’ kneeling ability, such as kneeling position, duration and surface being knelt upon. There are a number of different positions of kneeling and these have been illustrated previously.14,25–28 For example, a person may be able to kneel at 90o flexion on a soft mat transiently to pick up an item off the floor but would experience much difficulty in participating in prolonged kneeling at full flexion on a hard surface e.g. for prayer. A more comprehensive assessment of kneeling ability, in conjugation with an evaluation of expectations, motivations, purpose and importance of kneeling, would provide further understanding of this problem.
Impact
Kneeling is important for many activities and areas of life and is considered a valued activity for most patients with TKR.5,7,13 In one study with patients who were 12 months post TKR, 63% of patients had needed to kneel in the past four weeks but only 14% of patients were able to kneel easily.29 Given the wide range of activities that involve kneeling, and the expectation that this will be improved with surgery, problems kneeling after TKR are a source of dissatisfaction and disappointment for many patients.5,6 The impact of difficulty kneeling on specific areas of life is discussed below and summarized in Figure 1.
Fig. 1.
Impact of difficulty kneeling after total knee replacement.
Daily activities
Difficulty kneeling after TKR can impact on a number of daily household and self-care activities, including cleaning, reaching items from low cupboards or picking them up from the floor, decorating, and getting out of the bath.30 In Middle Eastern and Eastern cultures, kneeling can be an integral part of many daily activities, including when eating meals.19,25 These limitations can be disruptive to patients’ daily lives and many patients adapt their activities to minimize the impact, as is a common approach to managing chronic musculoskeletal conditions.31 Examples include sitting on a stool for household chores like low-level cleaning, using assistive devices such as grabbers, and home modifications such as conversion of a bath to a shower.30 However, despite these adaptions, some patients are unable to continue with some of their usual daily activities because of problems kneeling. In such cases assistance is often needed from friends or family members, or patients may need to employ others to complete these tasks on their behalf.30 Consequently, patients may experience a lack of independence and control due to being unable to perform basic household and self-care tasks because of their difficulty with kneeling, which can lead to distress and frustration.24 Catering for these limitations may also pose a financial burden on patients and social services, and/or a caring burden on family members.
Social participation
Assessment of the success of TKR is often focused on pain relief and improvement in the ability to carry out basic activities of daily living. However, enabling patients to engage in leisure activities and social participation is increasingly being recognized as a core aim of elective operations such as TKR.18,32 Difficulties with kneeling can adversely impact on a number of leisure, family and social activities.30 For example, gardening is an important leisure activity for many patients with TKR18 which is negatively affected by difficulty kneeling.30 Exercise and sports, playing with grandchildren, and volunteering activities can also be negatively affected by problems with kneeling.30 Religious activities often involve praying, requiring prolonged periods of kneeling, particularly in Middle Eastern and Asian cultures. For example, Muslims may pray up to five times a day, requiring full-flexion kneeling.25 In a study involving female Korean patients, 54% of patients knelt for religious reasons before surgery but only 1% of patients could perform this activity after TKR.19 The limitations imposed on people’s ability to participate in valued social and leisure activities due to kneeling may be a contributing factor to social isolation and loneliness after TKR.33
Employment
In the NHS, approximately 14% of TKRs are performed in patients < 65 years old.34 The demand for TKR in younger patients has been predicted to increase in the future35 and hence the ability to return to work is an increasingly important outcome of TKR. The majority of patients who are employed before TKR do return to work post-operatively.36 However, in those who are unable to return to work, a combination of patient, healthcare professional and workplace factors have been found to influence inability to participate in employment.37 Kneeling is the work-related activity that is least improved by TKR and restrictions in kneeling have been found to lead to difficulties in returning to more physically demanding jobs.37–39 Kneeling is an important activity for a number of occupations, including floor laying, roofing, joinery, nursery teaching, painting and decorating, plumbing and cleaning.40 Systematic reviews have found evidence that occupational kneeling is a risk factor for osteoarthritis, suggesting that kneeling ability may be a particularly important occupational factor for patients after TKR.41,42
Falls
Falls are a common problem in older adults, with one in three community-dwelling adults aged 60 years or over falling each year.43 The majority of falls result in no injury or minor injury only44 and therefore being able to get up independently after a fall is important. Kneeling is an intermediate position to enable people to get up after a fall, particularly in people with physical limitations.27 Being unable to kneel and therefore rise from the floor after a fall can have a negative impact on people’s confidence and independence, particularly when doing outdoor activities alone, such as walking the dog, gardening or fishing.30 Nervousness and fear of being unable to get up after a fall can cause people to self-impose restrictions on their activities, leading to physical deconditioning, psychological distress and social isolation.45
Aetiology
Understanding the underlying factors contributing to the difficulty that patients experience with kneeling after TKR is key to designing interventions to improve this important outcome. Research has established that there are discrepancies between a patient’s perceived ability to kneel and their observed ability. In one of the first studies focusing on kneeling after TKR, 56% of patients perceived they were unable to kneel but 80% could kneel easily when observed.46 Similar observations have been found in subsequent studies.26,47 This suggests that patients can kneel but elect not to.26,46,47
Several studies have evaluated the relationship between surgical factors and post-operative kneeling ability. Type of implant and whether the patellar has been resurfaced have been found to not be associated with kneeling ability.9,10,47,48 Research has found that there is no relationship between knee flexion and self-reported kneeling ability.9,47 The amount of knee flexion reported to be required for upright kneeling is 90o and 110–111o is needed for kneeling at full flexion.47 It has been shown that mean flexion of 114o can be achieved by three months post-operatively and further small increases can occur between three months and 12 months post-operatively.49,50 In another study, the mean range of motion was 114o in patients who were able to kneel and 110o in patients unable to kneel,47 highlighting that flexion is not an important cause of kneeling problems. However, flexion is an important outcome after TKR and innovations in implant design which aim to increase flexion have been evaluated. For example, numerous trials have been conducted to evaluate high-flexion TKRs, although synthesis of the evidence suggests that they provide similar flexion to standard TKRs.51 However, there is some preliminary evidence to suggest that modern implant design features which reduce patellofemoral joint forces, such as sided patellofemoral groove, flared posterior condyles and a single radius of curvature, can lead to better flexion.52
Skin incision has been found to be associated with numbness and kneeling ability. In one small non-randomized study, patients reported that discomfort on kneeling was lower in patients with a lateral incision compared with a midline incision.53 A randomized controlled trial (RCT) found that patients who received an anterolateral skin incision had a smaller area of cutaneous hypesthesia and better observed kneeling ability compared to patients with an anteromedial skin incision.54 The findings from these studies indicate that skin incision may have an impact on kneeling ability through numbness. Many studies have compared the clinical outcome of fixed vs mobile-bearing TKR designs; however, few studies have evaluated kneeling ability, and those that have report conflicting results.9,48 More research is needed to understand whether and how surgical factors contribute to difficulty kneeling after TKR.
Given that patients’ self-perception of kneeling ability is poorer than their observed ability, it is important to evaluate patients’ reasons for their limitations. Studies that have asked patients why they have difficulty kneeling have found that the reasons are multifactorial, including knee pain/discomfort, numbness, fear of harming the prosthesis, co-morbidities and recommendations from health professionals.14,26,29,30,46,47,55 Self-reported kneeling ability has been found to be associated with knee pain severity, numbness and hypersensitivity.9,29,55,56 Patients’ reports of sensations on kneeling can range from mild discomfort to severe pain.30 Pain is often associated with tissue damage, and therefore patients are concerned that they are causing damage to their TKR by kneeling. This misconception can be reinforced by advice from third parties, including surgeons, healthcare professionals, friends and families. One study found that a range of healthcare professionals advised patients not to kneel, most commonly nurse practitioners, followed by orthopaedic consultants, general practitioners and physiotherapists.14 Although the reasons for this have not been fully investigated, they are likely to be related to concerns regarding the safety of kneeling. In terms of kinematics, kneeling generates external load over the patella and tibial tubercle. This loading on the anterior aspect of the knee can displace the tibia in a posterior direction with respect to the femur. However, research that has evaluated the displacement of the femoral component relative to the tibial component with a range of TKR implant designs has found that the femorotibial anteroposterior articulation remains within the intended articular range of the implants, and subluxation and dislocation are highly unlikely.57–60 Also, no association between high-flexion activities, including kneeling, and aseptic loosening of the femoral component have been found.61 Therefore, there is currently no evidence that there is any clinical reason why patients should not kneel on their replaced knees, as long as kneeling on a rough or uneven surface is avoided as this could lead to damage of the overlying skin and the introduction of bacteria and potential for infection of the knee prosthesis. This is supported by the advice from Versus Arthritis, the largest charity for people with musculoskeletal disorders in the United Kingdom, who recommend that patients can try kneeling on a soft surface from three months post-operatively.62
Healthcare services and unmet need
There has been little research to evaluate the provision of healthcare services and interventions for patients who find kneeling problematic after TKR. One study found that most patients do not speak to healthcare professionals about their difficulties kneeling.30 Reasons for non-disclosure include that they do not think that their limitations are sufficiently severe to seek healthcare, that it is normal to not be able to kneel, and that nothing that can be done to improve their kneeling ability. In the context of being satisfied with other aspects of their outcome, some patients appear willing to accept not being able to kneel. For those patients who do raise their problems kneeling with a healthcare professional, they perceive a lack of interest from the healthcare professionals and few patients receive advice about how to improve their kneeling ability. This highlights a clear unmet need among patients for education and rehabilitation aimed at improving their kneeling ability after TKR.
The James Lind Alliance Priority Setting Partnership identifies research questions which have direct relevance and benefit to patients and the clinicians who treat them. One of the James Lind Alliance top 10 priorities for research into hip and knee replacement is ‘What is the most effective pre and post-operative patient education support and advice for improving outcomes and satisfaction for people with osteoarthritis following hip/knee replacement?’.63 Despite the prevalence and impact of kneeling problems after TKR, there has been limited research to evaluate whether patient education and rehabilitation could benefit patients.
A study published in 2004 involving patients with TKR, unicompartmental knee replacement (UKR) or patellar resurfacing asked patients whether they could kneel and then a healthcare professional observed them kneeling, followed by a questionnaire six months later.26 Of the patients who perceived they could not kneel but actually could kneel when observed, 80% reported that they could kneel with little or no difficulty six months later. This suggests that the encouragement and opportunity to practice kneeling with a healthcare professional was enough for many patients to continue with this activity. Four years later, an RCT involving 60 patients with UKR was published. This RCT found that a 30-minute physiotherapy intervention designed to provide verbal and written information on kneeling delivered at six weeks post-operatively improved patient-reported kneeling ability at one year after surgery compared to usual care.64 However, patients often report a quicker recovery and better outcomes for kneeling after UKR compared to TKR.5 As the authors of the trial concluded, further randomized evaluations of interventions to improve kneeling for patients with TKR are needed. However, no RCTs involving patients with TKR have evaluated the effectiveness of interventions specifically aimed at improving kneeling ability. A cohort study has investigated whether providing pre-operative patient education about kneeling improves patient-reported kneeling ability up to one year after surgery.55 Before surgery, patients were advised that they may have discomfort or pain on kneeling and that this would not damage their replaced knee and then a nurse demonstrated a safe kneeling technique. By 12 months post-operatively, 72% of patients reported that they could kneel, which is higher than reported in other cohort studies (overview provided in Table 1). While these findings are promising, this was a cohort study with no comparator group, and therefore the conclusions that can be drawn are limited. There is a clear need for further research to develop an intervention to improve kneeling after TKR and evaluate whether it is clinically and cost-effective.
Implications for clinical practice and directions for future research
The first step to improving care for patients is to promote clinical awareness of this poor outcome after surgery and its importance to patients, and to empower patients to feel that this long-term problem is recognized. For this to happen, healthcare professionals need to recognize that kneeling is the most unsatisfactory patient-reported outcome after TKR and that problematic kneeling can have a considerable negative impact on health-related quality of life. Informing patients of this prior to surgery would enable patients to set realistic expectations of their post-surgical outcome. An RCT is currently ongoing to evaluate whether providing patients with additional education prior to surgery to set realistic expectations, including regarding kneeling ability, can improve satisfaction at 12 months post-operatively.65 However, more research is needed to provide healthcare professionals with an evidence base to guide their discussions with patients and provision of healthcare services. Further research to understand more about the surgical and implant-related factors that are associated with kneeling ability could inform shared decision-making about surgical options with patients for whom kneeling is a particularly important outcome, e.g. for return to work. More research is also needed to design and evaluate interventions to improve kneeling. This would need to address the multifactorial reasons for which patients have difficulty kneeling after TKR, and patients have identified that they would like more information before surgery about post-operative kneeling ability, a more holistic approach to account for their other co-morbidities, use of kneeling demonstrations and provision of advice that kneeling is safe and will not damage their prosthesis.30 Such an intervention could give patients the knowledge and confidence to return to kneeling activities and enable them to feel more in control and independent after their TKR. Alongside generating evidence on the effectiveness of interventions, work is needed to understand healthcare professionals’ perceptions on kneeling to inform the implementation of research findings into clinical practice.
Conclusions
Patients have growing expectations of being able to return to a full and active lifestyle after their TKR. To meet these expectations, research is needed to evaluate how to optimize higher-function activities such as kneeling. The majority of patients experience difficulty kneeling after TKR, which can have a detrimental impact on many activities and areas of life and is a source of dissatisfaction. Increased clinical awareness of this poor outcome and research to inform the provision of services is needed to improve patient care and allow patients to return to this important activity.
Footnotes
ICMJE Conflict of interest statement: VW and AWB declare institutional grant funding from Stryker for activity outside of the submitted work. NH declares receiving funding for providing educational activities as faculty on courses for Stryker and Smith and Nephew.
Funding statement
This article was supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
References
- 1. Tilbury C, Haanstra TM, Leichtenberg CS, et al. Unfulfilled expectations after total hip and knee arthroplasty surgery: there is a need for better preoperative patient information and education. J Arthroplasty 2016;31:2139–2145. [DOI] [PubMed] [Google Scholar]
- 2. Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br 2012;94:974–981. [DOI] [PubMed] [Google Scholar]
- 3. Ghomrawi HMK, LY Lee, Nwachukwu BU, et al. Preoperative expectations associated with postoperative dissatisfaction after total knee arthroplasty: a cohort study. J Am Acad Orthop Surg 2019: 11 June; Epub ahead of print. Available from https://journals.lww.com/jaaos/Abstract/publishahead/Preoperative_Expectations_Associated_With.99348.aspx (date last accessed 18 June 2019). [DOI] [PMC free article] [PubMed]
- 4. Clement ND, MacDonald D, Patton JT, Burnett R. Post-operative Oxford knee score can be used to indicate whether patient expectations have been achieved after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:1578–1590. [DOI] [PubMed] [Google Scholar]
- 5. Barker KL, Hannink E, Pemberton S, Jenkins C. Knee arthroplasty patients’ predicted versus actual recovery: what are their expectations about time of recovery after surgery and how long before they can do the tasks they want to do? Arch Phys Med Rehabil 2018;99:2230–2237. [DOI] [PubMed] [Google Scholar]
- 6. Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 2014;21:180–184. [DOI] [PubMed] [Google Scholar]
- 7. Weiss JM, Noble PC, Conditt MA, et al. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res 2002;404:172–188. [DOI] [PubMed] [Google Scholar]
- 8. Baker PN, van der Meulen JH, Lewsey J, Gregg PJ; National Joint Registry for England and Wales; Data from the National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement. J Bone Joint Surg Br 2007;89:893–900. [DOI] [PubMed] [Google Scholar]
- 9. Artz NJ, Hassaballa MA, Robinson JR, Newman JH, Porteous AJ, Murray JR. Patient reported kneeling ability in fixed and mobile bearing knee arthroplasty. J Arthroplasty 2015;30:2159–2163. [DOI] [PubMed] [Google Scholar]
- 10. Hassaballa MA, Porteous AJ, Newman JH, Rogers CA. Can knees kneel? Kneeling ability after total, unicompartmental and patellofemoral knee arthroplasty. Knee 2003;10:155–160. [DOI] [PubMed] [Google Scholar]
- 11. Wylde V, Dixon S, Miller LL, Whitehouse MR, Blom AW. 5 year outcomes and survivorship of the triathlon total knee replacement: a cohort study. Acta Orthop Belg 2017;83:259–267. [PubMed] [Google Scholar]
- 12. Sharkey PF, Miller AJ. Noise, numbness, and kneeling difficulties after total knee arthroplasty: is the outcome affected? J Arthroplasty 2011;26:1427–1431. [DOI] [PubMed] [Google Scholar]
- 13. Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS): validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 2003;1:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Benfayed R, Moran M, Simpson AH, MacDonald D. Perceptions of kneeling ability After TKA. Orthop Muscular Syst 2017;6. [Google Scholar]
- 15. Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res 2005; 431:157–165. [DOI] [PubMed] [Google Scholar]
- 16. Wright JG, Santaguida PL, Young N, Hawker GA, Schemitsch E, Owen JL. Patient preferences before and after total knee arthroplasty. J Clin Epidemiol 2010;63:774–782. [DOI] [PubMed] [Google Scholar]
- 17. Wylde V, MacKichan F, Bruce J, Gooberman-Hill R. Assessment of chronic post-surgical pain after knee replacement: development of a core outcome set. Eur J Pain 2015;19:611–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wylde V, Livesey C, Blom AW. Restriction in participation in leisure activities after joint replacement: an exploratory study. Age Ageing 2012;41:246–249. [DOI] [PubMed] [Google Scholar]
- 19. Kim TK, Kwon SK, Kang YG, Chang CB, Seong SC. Functional disabilities and satisfaction after total knee arthroplasty in female Asian patients. J Arthroplasty 2010;25:458–464. [DOI] [PubMed] [Google Scholar]
- 20. Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford Knee Score following total knee replacement. Bone Joint J 2013;95-B:45–51. [DOI] [PubMed] [Google Scholar]
- 21. Rothwell AG, Hooper GJ, Hobbs A, Frampton CM. An analysis of the Oxford Hip and Knee Scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br 2010;92:413–418. [DOI] [PubMed] [Google Scholar]
- 22. Pynsent PB, Adams DJ, Disney SP. The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg Br 2005;87:241–248. [DOI] [PubMed] [Google Scholar]
- 23. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 1998;80:63–69. [DOI] [PubMed] [Google Scholar]
- 24. Usiskin IM, Yang HY, Deshpande BR, et al. Association between activity limitations and pain in patients scheduled for total knee arthroplasty. BMC Musculoskelet Disord 2016;17:378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Acker SM, Cockburn RA, Krevolin J, Li RM, Tarabichi S, Wyss UP. Knee kinematics of high-flexion activities of daily living performed by male Muslims in the Middle East. J Arthroplasty 2011;26:319–327. [DOI] [PubMed] [Google Scholar]
- 26. Hassaballa MA, Porteous AJ, Newman JH. Observed kneeling ability after total, unicompartmental and patellofemoral knee arthroplasty: perception versus reality. Knee Surg Sports Traumatol Arthrosc 2004;12:136–139. [DOI] [PubMed] [Google Scholar]
- 27. Ulbrich J, Raheja A, Alexander NB. Body positions used by healthy and frail older adults to rise from the floor. J Am Geriatr Soc 2000;48:1626–1632. [DOI] [PubMed] [Google Scholar]
- 28. Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res 2001;24:191–198. [DOI] [PubMed] [Google Scholar]
- 29. Blackburn J, Wylde V, Greenwood R, Blom AW, Levy A. The effect of numbness on outcome from total knee replacement. Ann R Coll Surg Engl 2017;99:385–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fletcher D, Moore AJ, Blom AW, Wylde V. An exploratory study of the long-term impact of difficulty kneeling after total knee replacement. Disabil Rehabil 2019; 41;820–825. [DOI] [PubMed] [Google Scholar]
- 31. Moore AJ, Richardson JC, Sim J, Bernard M, Jordan KP. Older people’s perceptions of remaining physically active and living with chronic pain. Qual Health Res 2014;24:761–772. [DOI] [PubMed] [Google Scholar]
- 32. Davis AM, Perruccio AV, Ibrahim S, et al. The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthritis Cartilage 2011;19:1413–1421. [DOI] [PubMed] [Google Scholar]
- 33. Smith TO, Dainty JR, MacGregor AJ. Changes in social isolation and loneliness following total hip and knee arthroplasty: longitudinal analysis of the English Longitudinal Study of Ageing (ELSA) cohort. Osteoarthritis Cartilage 2017;25:1414–1419. [DOI] [PubMed] [Google Scholar]
- 34. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 15th annual report. Hemel Hempstead: NJR Centre, 2018. [Google Scholar]
- 35. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009;467:2606–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tilbury C, Schaasberg W, Plevier JW, Fiocco M, Nelissen RG, Vliet Vlieland TP. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology (Oxford) 2014;53:512–525. [DOI] [PubMed] [Google Scholar]
- 37. Bardgett M, Lally J, Malviya A, Kleim B, Deehan D. Patient-reported factors influencing return to work after joint replacement. Occup Med (Lond) 2016;66:215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kievit AJ, van Geenen RC, Kuijer PP, Pahlplatz TM, Blankevoort L, Schafroth MU. Total knee arthroplasty and the unforeseen impact on return to work: a cross-sectional multicenter survey. J Arthroplasty 2014;29:1163–1168. [DOI] [PubMed] [Google Scholar]
- 39. Scott CEH, GS Turnbull, MacDonald D, Breusch J. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J 2017;99-B:1037–1046. [DOI] [PubMed] [Google Scholar]
- 40. Ditchen DM, Ellegast RP, Gawliczek T, Hartmann B, Rieger MA. Occupational kneeling and squatting: development and validation of an assessment method combining measurements and diaries. Int Arch Occup Environ Health 2015;88:153–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Verbeek J, Mischke C, Robinson R, et al. Occupational exposure to knee loading and the risk of osteoarthritis of the knee: a systematic review and a dose-response meta-analysis. Saf Health Work 2017;8:130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McWilliams DF, Leeb BF, Muthuri SG, Doherty M, Zhang W. Occupational risk factors for osteoarthritis of the knee: a meta-analysis. Osteoarthritis Cartilage 2011;19:829–839. [DOI] [PubMed] [Google Scholar]
- 43. Gale CR, Cooper C, Aihie Sayer A. Prevalence and risk factors for falls in older men and women: The English Longitudinal Study of Ageing. Age Ageing 2016;45:789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993;137:342–354. [DOI] [PubMed] [Google Scholar]
- 45. Delbaere K, Close JC, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 2010;341:c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schai PA, Gibbon AJ, Scott RD. Kneeling ability after total knee arthroplasty: perception and reality. Clin Orthop Relat Res 1999;367:195–200. [PubMed] [Google Scholar]
- 47. Palmer SH, Servant CT, Maguire J, Parish EN, Cross MJ. Ability to kneel after total knee replacement. J Bone Joint Surg Br 2002;84:220–222. [DOI] [PubMed] [Google Scholar]
- 48. Kim TW, Park SH, Suh JT. Comparison of mobile-bearing and fixed-bearing designs in high flexion total knee arthroplasty: using a navigation system. Knee Surg Relat Res 2012;24:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zhou Z, Yew KS, Arul E, Chin PL, Tay KJ, Lo NN, et al. Recovery in knee range of motion reaches a plateau by 12 months after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:1729–1733. [DOI] [PubMed] [Google Scholar]
- 50. Mehta S, Rigney A, Webb K, et al. Characterizing the recovery trajectories of knee range of motion for one year after total knee replacement. Physiother Theory Pract 2018;1–10. [DOI] [PubMed] [Google Scholar]
- 51. Jiang Y, Yao JF, Xiong YM, Ma JB, Kang H, Xu P. No superiority of high-flexion vs standard total knee arthroplasty: an update meta-analysis of randomized controlled trials. J Arthroplasty 2015;30:980–986. [DOI] [PubMed] [Google Scholar]
- 52. Hamilton DF, Burnett R, Patton JT, et al. Implant design influences patient outcome after total knee arthroplasty: a prospective double-blind randomised controlled trial. Bone Joint J 2015;97-B:64–70. [DOI] [PubMed] [Google Scholar]
- 53. Calvert N, Milne L, Kuster M. A comparison of kneeling ability after lateral or midline incisions in total knee arthroplasty. Eur J Orthop Surg Traumatol 2016;26:915–919. [DOI] [PubMed] [Google Scholar]
- 54. Tsukada S, Kurosaka K, Nishino M, Hirasawa N. Cutaneous hypesthesia and kneeling ability after total knee arthroplasty: a randomized controlled trial comparing anterolateral and anteromedial skin incision. J Arthroplasty 2018;33:3174–3180. [DOI] [PubMed] [Google Scholar]
- 55. White L, Stockwell T, Hartnell N, Hennessy M, Mullan J. Factors preventing kneeling in a group of pre-educated patients post total knee arthroplasty. J Orthop Traumatol 2016;17:333–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hassaballa M, Artz N, Weale A, Porteous A. Alteration in skin sensation following knee arthroplasty and its impact on kneeling ability: a comparison of three common surgical incisions. Knee Surg Sports Traumatol Arthrosc 2023;20:1983–1987. [DOI] [PubMed] [Google Scholar]
- 57. Incavo SJ, Mullins ER, Coughlin KM, Banks S, Banks A, Beynnon BD. Tibiofemoral kinematic analysis of kneeling after total knee arthroplasty. J Arthroplasty 2004;19:906–910. [DOI] [PubMed] [Google Scholar]
- 58. Coughlin KM, Incavo SJ, Doohen RR, Gamada K, Banks S, Beynnon BD. Kneeling kinematics after total knee arthroplasty: anterior-posterior contact position of a standard and a high-flex tibial insert design. J Arthroplasty 2007;22:160–165. [DOI] [PubMed] [Google Scholar]
- 59. Barnes CL, Sharma A, Blaha JD, Nambu SN, Carroll ME. Kneeling is safe for patients implanted with medial-pivot total knee arthroplasty designs. J Arthroplasty 2011;26:549–554. [DOI] [PubMed] [Google Scholar]
- 60. Nakamura S, Sharma A, Kobayashi M, et al. 3D in vivo femoro-tibial kinematics of tri-condylar total knee arthroplasty during kneeling activities. Knee 2014;21:162–167. [DOI] [PubMed] [Google Scholar]
- 61. Ha CW, Ravichandran C, Lee CH, Kim JH, Park YB. Performing high flexion activities does not seem to be crucial in developing early femoral component loosening after high-flexion TKA. BMC Musculoskelet Disord 2015;16:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Versus Arthritis. Knee replacement surgery, 2018. https://www.versusarthritis.org/about-arthritis/treatments/surgery/knee-replacement-surgery/ (date last accessed 18 June 2019).
- 63. James Lind Alliance Priority Setting Partnership. Hip and knee replacement for osteoarthritis, 2014. http://www.jla.nihr.ac.uk/priority-setting-partnerships/hip-and-knee-replacement-for-osteoarthritis/ (date last accessed 18 June 2019).
- 64. Jenkins C, Barker KL, Pandit H, Dodd CA, Murray DW. After partial knee replacement, patients can kneel, but they need to be taught to do so: a single-blind randomized controlled trial. Phys Ther 2008;88:1012–1021. [DOI] [PubMed] [Google Scholar]
- 65. Tolk JJ, Janssen RPA, Haanstra TM, Bierma-Zeinstra SMA, Reijman M. The EKSPECT study: the influence of Expectation modification in Knee arthroplasty on Satisfaction of PatiEnts: study protocol for a randomized Controlled Trial. Trials 2018;19:437. [DOI] [PMC free article] [PubMed] [Google Scholar]