Abstract
Purpose
Trauma is a major health problem in developing countries and worldwide which requires many resources and much time in an emergency department (ED). Although Advanced Trauma Life Support (ATLS) is the gold standard, operator dependence can affect the quality of care. The objective was to identify differences in numbers and time to lifesaving interventions, investigation, ED length of stay, and mortality between an in-house protocol and conventional practice.
Methods
This was a single-center prospective non-randomized study for adult trauma patients in the ED. The trauma protocol was developed from the recent ATLS guideline.
Results
Thirty-two and 41 cases were in the in-house protocol group and conventional practice group, respectively. Endotracheal intubation was done more frequently in the in-house protocol group (84% vs. 59%, p = 0.03). Intercostal drainage tube insertion was done faster (6–26 min, median 11 min vs. 15–84 min, median 35 min, p = 0.02) and pre-arrival notification by emergency medical service increased in the in-house protocol group (66% vs. 30%, p = 0.01). Hypothermia in the operating room was found only in the conventional practice group (62% vs. 0, p = 0.007) and a warm blanket was used significantly more often in the in-house protocol group (25% vs. 0, p < 0.001). A directed acyclic graph with multivariate analysis was used to identify confounders. Time to Focused Assessment Sonography in Trauma was significantly shorter in the in-house protocol group (6.5–15.6 min, median 11 min, p = 0.019).
Conclusion
In addition to the ATLS guideline, the trauma protocol could improve trauma care by reduced time to investigation, early notification of the trauma team in pre-hospital situations, reduced incidence of hypothermia in the operating room, and increased use of a warm blanket.
Keywords: Advanced trauma life support care, Protocol, Emergency department
Introduction
Trauma is a major health problem in developing countries and worldwide which requires many resources and much time in an emergency department (ED). Resources and time can be reduced by improvements in trauma care.1, 2, 3
Nowadays, Advanced Trauma Life Support (ATLS) is the gold standard and universal guideline for management in trauma patients who usually present at the ED.4 Although ATLS is the standard guideline, there are some issues that can present problems in the quality of care. Operator dependence may delay the time to intervention and diagnosis because of a lack of clinical experience.5, 6
Previous studies showed that using a trauma protocol can significantly reduce time to initiation of lifesaving interventions and reduce mortality.7, 8 Some studies also showed that using a trauma protocol decreased ED length of stay.9, 10 One study reported that using a checklist improved the frequency and speed of the primary and secondary surveys.11
In Thailand, there is no trauma protocol in the ED. Therefore, we aimed to develop an ED trauma protocol to assess the clinical outcomes and reduce the time to lifesaving interventions, investigations, and shorten the length of stay in the ED.
The primary objective was to identify differences in the numbers and time to lifesaving interventions. The secondary objective was to identify time to investigation, intervention, ED length of stay, and mortality. Both objectives compared the in-house protocol with conventional practice.
Methods
Study design and setting
This was a single-center prospective non-randomized comparison study conducted in the ED at Songklanagarind Hospital which is a university-based level 1 trauma center on the campus of Prince of Songkla University in southern Thailand. The ED treats approximately 50,000 patients including 10,000 traumatic patients per year. The institutional review board of the Faculty of Medicine, Prince of Songkla University approved this study (EC 60-219-20-4).
Selection of participants
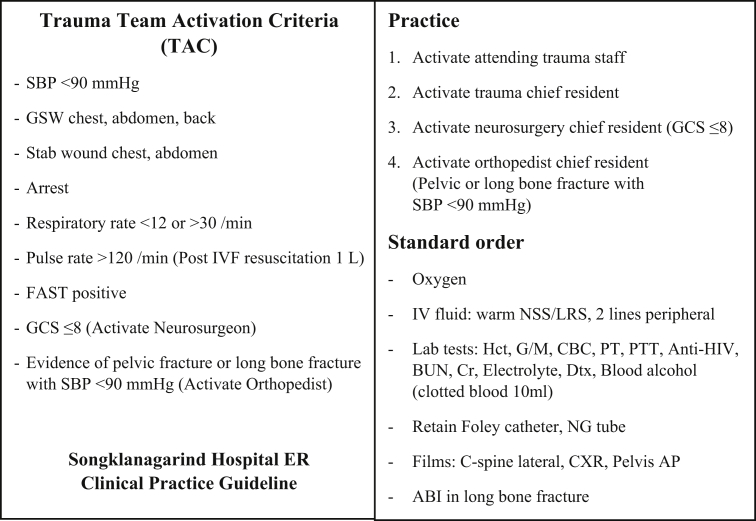
Our center utilizes trauma activation criteria (TAC) for early notification of the trauma surgeon when the criteria are met (Fig. 1). The inclusion criteria for this study were traumatic adult patients (≥15 years old) who visited the ED at Songklanagarind Hospital between February and November 2018 and met the TAC. Patients included in the study were managed using the in-house protocol sheet or conventional practice depending on physician preference. Referred patients, pregnant patients, and patients who did not meet the TAC were excluded.
Fig. 1.
Trauma activation criteria.
Intervention and development of an in-house trauma protocol sheet
A trauma protocol based on the recent ATLS guideline and other evidence-based practices was developed by the author and a colleague under the supervision of a certified trauma surgeon. A feasibility test and public hearing were used during development of the protocol to obtain the final version: Trauma Protocol V.2 Emergency Department Songklanagarind Hospital (Appendix A. Supplementary data).
Measurements
Data were collected between February and November 2018 from the Hospital Information System, Picture Archiving and Communication System, trauma registry, and the ED registry. All data were recorded in a case record form.
Outcomes
The primary outcomes of this study were the number of interventions and the time to lifesaving interventions. The secondary outcomes were the time to investigation and intervention, ED length of stay, and mortality.
Analysis
All data were entered into EpiData Manager (version 4.4.2.1) and the statistical analysis was performed using R software (version 3.5.1). Continuous variables are reported as mean or median using the unpaired t-test or Wilcoxon Rank-Sum test while categorical variables are reported as percentage using Pearson's Chi-squared test or Fisher's exact test. A directed acyclic graph was used to identify what needed to be controlled in a multivariate analysis. A p value < 0.05 was considered statistically significant.
Results
Characteristics of the study subjects
Eighty-nine cases were initially included in the study but 16 cases were excluded. Of the excluded cases the attending physician did not activate the trauma team or TAC in 12 cases, there were missing records in three cases, and in 1 case the TAC was cancelled. Finally, 73 cases were enrolled. Thirty-two cases were in the group that used the in-house protocol and 41 cases were in the conventional practice group. There were no significant differences in the demographic and baseline characteristics between the two groups except in head injury which was more severe in the in-house protocol group (Table 1).
Table 1.
Demographic and baseline characteristics of the patients.
| Demographics | Conventional group | In-house protocol | p value |
|---|---|---|---|
| (n = 41) | (n = 32) | ||
| Age (year), median (IQR) | 30 (21, 46) | 40 (28, 50) | 0.144 |
| Sex | 0.388 | ||
| Male | 30 (73) | 27 (84) | |
| Female | 11 (27) | 5 (16) | |
| Glasgow coma scale score | 0.038 | ||
| ≤8 | 25 (61) | 26 (81) | |
| 9-12 | 0 (0) | 1 (3) | |
| 13-15 | 16 (39) | 5 (16) | |
| Mechanism of injury | 0.673 | ||
| Motor vehicle collision | 29 (71) | 24 (75) | |
| Car crash | 2 (5) | 3 (9) | |
| Pedestrian | 0 (0) | 1 (3) | |
| Fall from height | 3 (7) | 2 (6) | |
| Penetrating injury | 5 (12) | 2 (6) | |
| Injury Severity Score, median (IQR) | 21 (10, 29) | 17 (14, 25) | 0.737 |
| Trauma and Injury Severity Score, median (IQR) | 0.95 (0.6, 1) | 0.73 (0.1, 1) | 0.126 |
| Systolic blood pressure <90 mmHg | 5 (12) | 2 (6) | 0.057 |
| Cardiac arrest | 8 (20) | 12 (38) | 0.148 |
| Focused Assessment Sonography in Trauma | 40 (98) | 30 (94) | 0.578 |
| Chest radiography | 34 (83) | 25 (78) | 0.828 |
| Cranial computed tomography | 27 (66) | 19 (59) | 0.745 |
Data are presented as n (%) unless indicated otherwise.
IQR: interquartile range.
Main results
Among the primary outcomes, endotracheal intubation (ETI) was performed significantly more frequently in the group that used the protocol (84% vs 59%, p = 0.03). Also, the time to ETI tended to be faster but the results were not significant (3–15 min, median 6 min vs. 5–13 min, median 8 min, p = 0.575). Intercostal drainage (ICD) tube insertion was also done significantly faster in the group that used the protocol (6–26 min, median 11 min vs. 15–84 min, median 35 min, p = 0.02). Other lifesaving interventions between the two groups were not significantly different (Table 2).
Table 2.
Primary outcome: time to lifesaving intervention.
| Intervention | Conventional group | In-house protocol | p value |
|---|---|---|---|
| Endotracheal intubation, n (%) | 24 (59) | 27 (84) | 0.033 |
| Median (IQR) in minutes | 8 (5, 13) | 6 (3, 15) | 0.575 |
| Oxygen therapy, n (%) | 2 (5) | 0 | 0.501 |
| Needle decompression, n (%) | 2 (5) | 1 (3) | 1 |
| ICD tube insertion, n (%) | 14 (34) | 15 (47) | 0.389 |
| Median (IQR) in minutes | 35 (15, 84) | 11 (6, 26) | 0.021 |
| ED-thoracotomy, n (%) | 0 | 2 (6) | 0.189 |
| Minutes | – | 9 | – |
| PRC transfusion, n (%) | 5 (12) | 6 (19) | 0.518 |
| Operation, n (%) | 10 (24) | 9 (28) | 0.927 |
| Mean ± SD in minutes | 129 ± 41 | 141 ± 28 | 0.483 |
Mean or median = duration from arrival to complete intervention.
IQR: interquartile range, SD: standard deviation.
Among the secondary outcomes, time to Focused Assessment Sonography in Trauma (FAST) tended to be performed faster (4–12 min, median 8 min vs. 7–27 min, median 10 min, p = 0.056) in the protocol group but the difference was not significant. Initial ED hypothermia was not significantly different (20% vs. 8%, p = 0.49) but hypothermia in the operating room was found only in the conventional practice group (62% vs. 0, p = 0.007) and a warm blanket was used significantly more often in the protocol group (25% vs. 0, p < 0.001). There were no significant differences in time to other investigations that included plain radiograph (eg, chest X-rays), computed tomography, arterial blood gas, and electrocardiography. In the process of care, there was a significant increase in pre-arrival notification by the emergency medical service in the group that used the in-house protocol (66% vs 30%, p = 0.01). There were no significant differences in time to activate the TAC, time to the operating room, time to intensive care unit admission or ED length of stay. There were no significant differences in the percentages of missed diagnoses or the 24 h, 72 h, and 28 day mortality rates in the ED. The clinical performance scores at discharge were also not significantly different. There were no further statistically significant results in the subgroup analysis of primary and secondary outcomes according to the Injury Severity Score of ≤15, 16–24, or ≥25 between the in-house protocol group and conventional group.
We used a directed acyclic graph to identify potential confounders (Fig. 2). The outcomes that were initially significant and of interest were ETI, ICD, FAST, and chest X-rays. In the multivariate analysis, the non-concealed pathways between use of the in-house protocol and outcomes were blocked by adjusting for cardiac arrest (for outcome of ICD), cardiac arrest, and severe head injury (for outcome of ETI). Finally, time to FAST was the only outcome that was significantly shorter (6.5–15.6 min, median 11 min, p = 0.019) in the in-house protocol group. The results and the adjusted odds ratios for those results were not significant (Table 3).
Fig. 2.
Directed acyclic graph.
Table 3.
Adjusted outcome and odds ratios of in-house protocol group vs. conventional group.
| Outcome | Time (minutes) |
||||
|---|---|---|---|---|---|
| Median difference (IQR)a | p value | Crude odds ratio | Adjusted odds ratioa | p value | |
| ETI | −2.9 (−7.4, 1.6) | 0.522 | 3.83 (1.22–11.94) | 2.92 (0.22–39.11) | 0.403 |
| ICD | −18.5 (−40.3, 3.3) | 0.407 | 1.7 (0.66–4.39) | 1.24 (0.43–3.59) | 0.695 |
| FAST | −11 (−15.6, −6.5) | 0.019 | 0.38 (0.03–4.33) | 0.416 | |
| CXR | 6.1 (1.1, 11.1) | 0.229 | 1.36 (0.42–4.37) | 0.606 | |
ETI: endotracheal tube insertion; ICD: intercostal drainage tube insertion; FAST: focused assessment sonography in trauma; CXR: chest X-ray.
According to directed acyclic graph using multivariate analysis.
Discussion
Early diagnosis, management, and resuscitation in multiple-severe trauma patients are the keys to improved outcomes. A trauma protocol was first developed and used at the University of Heidelberg, Germany, in 2006. Since then, a few published articles reported improved process and results in trauma care including time to lifesaving intervention, ED length of stay, and mortality. Our in-house trauma protocol titled Trauma Protocol V.2 Emergency Department Songklanagarind Hospital was developed according to the most recent ATLS guideline and other evidence that matched our trauma workflow. The results showed that application of the trauma protocol in the ED improved the outcomes in time to investigation. This protocol had the effect of shortening the time to FAST. Our results were consistent with that of Bernhard (2006).7 There were no differences in the lifesaving interventions as reported by Kesinger (2014).8 Unlike other studies, we did not find any significant difference in ED length of stay or mortality.7, 8, 9, 10 But the protocol showed that pre-arrival notification improved significantly which resulted in early notification of the trauma team when the TAC criteria were met. The incidence of hypothermia in the operating room was greater in the conventional practice group and a warm blanket was used only in the in-house protocol group.
Our study has some limitations. First, it was a single-center study in an academic tertiary medical center which possibly limited the generalizability of our results due to limitations of health care in smaller hospitals. Second, the number of patients was small which possibly diminished the significance of the results. Some relevant data were not recorded. Last, the patients were not randomized because not all ER physicians were familiar with the protocol. These limitations can be addressed by conducting a multi-center prospective trial with a longer study period and uniform use of the protocol in the ED.
To sum up, in addition to the ATLS guideline, a trauma protocol can improve trauma care by reduced time to investigation, early notification of the trauma team in pre-hospital situations, reduced incidence of hypothermia in the operating room, and increased use of warm blankets.
Funding
Nil.
Acknowledgments
The authors thank Kingkarn Waiyanak for article searches and retrieval, Glenn K. Shingledecker for his help in editing the manuscript, Alan Frederick Geater, Nannapat Pruphetkaew and Walailuk Jitpiboon in the Epidemiology Unit for the statistical assistance and the Faculty of Medicine for funding this research.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.04.003.
Ethical statement
The institutional review board of the Faculty of Medicine, Prince of Songkla University approved this study (EC 60-219-20-4).
Conflicts of interest
The authors declare no conflicts of interest.
Author contributions
Wainik Sookmee performed the literature search, study design, data collection, data analysis, data interpretation, and writing the manuscript. Siriporn Damnoi performed development of the protocol in addition to the feasibility test, data collection, and data analysis. Prasit Wuthisuthimethawee did the literature search, study design, and critical revision.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO Injuries and violence: the facts 2014. WHO Int. 2014 https://apps.who.int/iris/handle/10665/149798 Available from: [Google Scholar]
- 2.Mock C., Joshipura M., Arreola-Risa C. An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg. 2012;36:959–963. doi: 10.1007/s00268-012-1459-6. [DOI] [PubMed] [Google Scholar]
- 3.American College of Surgeons Committee on Trauma . Resources for optimal care of the injured patient 2006. In: Vincent J.L., Hall J.B., editors. Encyclopedia of Intensive Care Medicine. Springer; Berlin, Heidelberg: 2006. [DOI] [Google Scholar]
- 4.American College of Surgeons Committee on Trauma . tenth ed. American College of Surgeons; Chicago: 2018. Advance Trauma Life Support: Student Manual. [Google Scholar]
- 5.Hashmi Z.G., Haider A.H., Zafar S.N. Hospital-based trauma quality improvement initiatives: first step toward improving trauma outcomes in the developing world. J Trauma Acute Care Surg. 2013;75:60–68. doi: 10.1097/TA.0b013e31829880a0. [DOI] [PubMed] [Google Scholar]
- 6.Ali J., Adam R., Butler A.K. Trauma outcome improves following the advanced trauma life support program in a developing country. J Trauma. 1993;34:890–898. doi: 10.1097/00005373-199306000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Bernhard M., Becker T.K., Nowe T. Introduction of a treatment algorithm can improve the early management of emergency patients in the resuscitation room. Resuscitation. 2007;73:362–373. doi: 10.1016/j.resuscitation.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Kesinger M.R., Puyana J.C., Rubiano A.M. Improving trauma care in low- and middle-income countries by implementing a standardized trauma protocol. World J Surg. 2014;38:1869–1874. doi: 10.1007/s00268-014-2534-y. [DOI] [PubMed] [Google Scholar]
- 9.Cornwell E.E., 3rd, Chang D.C., Phillips J. Enhanced trauma program commitment at a level I trauma center: effect on the process and outcome of care. Arch Surg. 2003;138:838–843. doi: 10.1001/archsurg.138.8.838. [DOI] [PubMed] [Google Scholar]
- 10.Wurmb T.E., Frühwald P., Knuepffer J. Application of standard operating procedures accelerates the process of trauma care in patients with multiple injuries. Eur J Emerg Med. 2008;15:311–317. doi: 10.1097/MEJ.0b013e3283036ce6. [DOI] [PubMed] [Google Scholar]
- 11.Kelleher D.C., Carter E.A., Waterhouse L.J. Effect of a checklist on advanced trauma life support task performance during pediatric trauma resuscitation. Acad Emerg Med. 2014;21:1129–1134. doi: 10.1111/acem.12487. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.