Abstract
Calcaneovalgus foot deformities are present in up to 35% of patients with lumbar spina bifida. Resultant heel weight bearing causes complications include those associated with pressure ulcers. Early surgical reconstruction is advocated to prevent deformity progression and rigidity. Several surgical techniques in paediatric populations have been described, but there remains a paucity of literature regarding reconstruction of chronic calcaneovalgus feet in adults. This case report describes our experience using the Ilizarov technique in the reconstruction of an adult presenting with chronic calcaneovalgus feet. This is a 34-year-old lady with myelomeningocoele spina bifida of lumbar level 5 who presented with a history of multiple admissions for cellulitis and infections of bilateral heel pressure sores. Rigid calcaneovalgus deformities of both feet (45° on the right, 40° on the left) were noted on clinical examination and radiological investigations. Reconstruction with an Ilizarov frame allowed for gradual correction of both soft tissue and bone, correcting heel weight bearing ambulation, with the aim of preventing further complications from infected heel ulcers. While the correction of bony deformities is crucial, management of chronically contracted soft tissue must not be overlooked. An Ilizarov frame requires both an experienced surgeon and a motivated patient, but it allows for accurate reconstruction of bony deformities, while allowing management of surrounding chronic soft tissue contractures with good functional outcome.
Keywords: Ilizarov technique, Calcaneus, Foot deformities, Contracture, Meningomyelocele
Introduction
Spina bifida is a birth defect caused by failure of the foetal spinal cord to completely close. Patients with spina bifida affecting the lumbar spine develop a range of congenital and acquired orthopaedic deformities. Foot deformities are among the most common, with an incidence of over 80%.1 Calcaneovalgus foot deformities are present in up to 35% of patients with low-level spina bifida; most commonly myelomeningocoele of lumbar levels 4 and 5.1, 2 Calcaneovalgus deformity arises from weak or absent plantar flexors and invertors failing to oppose strong or spastic dorsiflexors and evertors.3, 4, 5, 6 Ability to ambulate is related to the level of the neurological lesion, with better prognoses associated with lower lying lesions; 91% of young adults with a lumbar level 5 lesions and 57% of patients with a lumbar level 4 lesions remain ambulant.7 However, calcaneovalgus deformities cause primary weight bearing on the heels, leading to complications ranging from pressure ulcers to osteomyelitis.4, 6
Early surgical reconstruction is advocated to prevent progression and rigidity of deformity.5, 6, 8 The aim of surgery is firstly to achieve a plantigrade, pain-free, stable foot amenable to bracing, and secondly to prevent secondary osseous deformities such as external tibial torsion. Several surgical techniques have been described including posterior transfer of the anterior tibialis tendon and complete anterolateral release of the extensor tendons as well as peroneus longus and brevis.5, 8 The successful use of the Ilizarov technique in a paediatric series has also been described by Kelley et al.9 All the aforementioned techniques described involved paediatric populations, and there remains a paucity of literature regarding treatment of chronic calcaneovalgus feet in adults. This case report describes our experience using the Ilizarov technique in the reconstruction of an adult presenting with chronic calcaneovalgus feet due to myelomeningocele of lumbar level 5.
Case report
A 34-year-old lady with spina bifida, specifically myelomeningocoele of lumbar level 5, presented to the outpatient specialist orthopaedic clinic with bilateral calcaneovalgus feet deformities. Although ambulant, the bilateral calcaneovalgus feet deformities had caused recurrent pressure ulcers over her heels (Fig. 1). This had led to multiple hospital admissions over the previous two years for cellulitis and infected ulcers, including two admissions for debridement of infected heel ulcers on her left, which had led to osteomyelitis. Examination of her feet revealed bilateral rigid calcaneovalgus deformities. Her left ankle was dorsiflexed to 45° and her right ankle to 40° with callosities over both her heels (Fig. 2, Fig. 3).
Fig. 1.
Clinical picture of right medial foot pre-reconstruction (A) and left foot pressure ulcers pre-reconstruction (B).
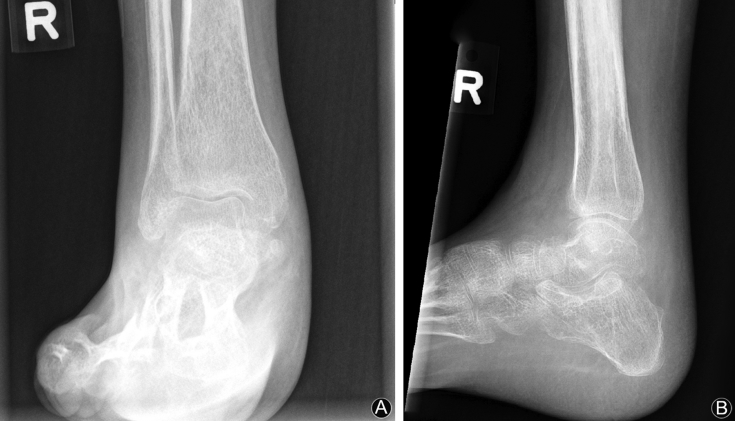
Fig. 2.
Preoperative X-ray of right foot and ankle: anteroposterior (A) and lateral (B) views.
Fig. 3.
Preoperative X-ray of left foot and ankle: anteroposterior (A) and lateral (B) views.
Management goals were discussed with the patient, and a decision was made to proceed with reconstruction of both feet using Ilizarov frames, with the aim of maintaining independent ambulation while minimising recurrent hospitalisations from pressure ulcers and infection. As the patient previously had numerous superficial skin and ulcer infections of the left foot and ankle, it was decided to proceed with reconstruction of the right foot and ankle first. This was to allow time to improve the skin condition of the left foot before reconstruction.
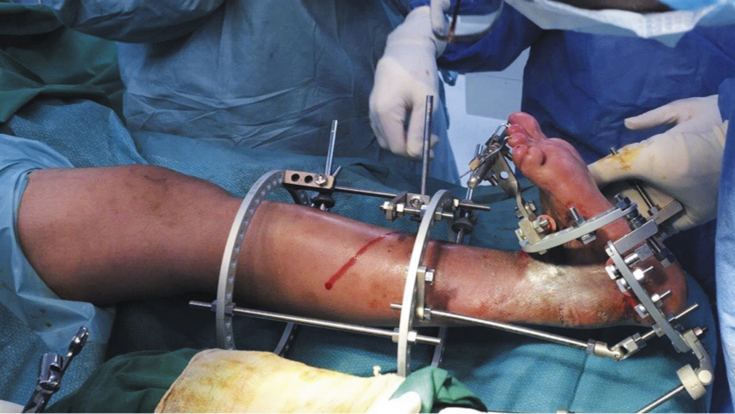
An Orthofix TL-HEX frame was used with 4 half pins inserted in the tibia supporting 2 circular rings. A third semi-circular foot ring was supported by 5 fine wires; 3 inserted into the calcaneus and 2 into the metatarsals. Finally, 2 Kirschner wires were passed through the second and third toe before attachment to the frame (Fig. 4). Minimal deformity correction was done intraoperatively to prevent excessive soft tissue trauma and stretch (Fig. 5).
Fig. 4.
Clinical picture of frame application on right foot and ankle.
Fig. 5.
Immediate postoperative X-ray of right foot and ankle: anteroposterior (A) and lateral (B) views.
Postoperative recovery was uneventful with discharge on day 3. Deformity correction was done gradually over the subsequent 4 months (Fig. 6), with fixed daily adjustments done by the patient and close weekly follow-up in clinic. The aim was for 3°–4° of correction per week, and at 4 months postoperatively, her foot was in neutral and removal of the frame was performed. A slight delay in frame removal was encountered as 3 months postoperatively it was noted her ankle was subluxing, and the frame was kept on longer following reduction of the ankle. A below knee cast was applied after removal of the frame, and full weight bearing as tolerated was allowed. Casting was kept for 6 weeks before the removal, and she was fitted with an ankle-foot orthosis. On review in clinic 4 weeks subsequently, the patient was pain-free, with a stable, plantigrade foot (Fig. 7, Fig. 8).
Fig. 6.
Four-month postoperative X-ray (before frame removal) of right foot and ankle: anteroposterior (A) and lateral (B) views.
Fig. 7.
X-ray films 3 months after frame removal of right foot and ankle: anteroposterior (A) and lateral (B) views.
Fig. 8.
Clinical pictures of right foot and ankle before (A) and 3 months after frame removal (B).
Eleven months after starting reconstruction of the right foot and ankle, reconstruction of the left foot and ankle was commenced. Again, an Orthofix TL-HEX frame was used with 4 half pins inserted in the tibia supporting 2 circular rings. The third semi-circular foot ring was supported by multiple fine wires, which were inserted in the calcaneus and metatarsals. Finally, 4 Kirschner wires were passed through the first through forth metatarsals before attachment to the frame. As with the previous reconstruction, minimal deformity correction was done intra-operatively to prevent excessive soft tissue trauma and stretch.
Postoperative recovery was uneventful. Gradual deformity correction of 4°–5° per week was maintained, with close follow-up in clinic. After 2 months, her foot was in neutral and the frame was removed. Again, a below knee cast was applied with full weight bearing as tolerated. Casting was again kept for 6 weeks before fitting of an ankle-foot orthosis.
Discussion
Management and reconstruction of chronic calcaneovalgus deformities in adults is complex, as chronicity often results in rigidity of deformities and secondary osseous deformities such as external tibial torsion. Ambulation is difficult due to crouch gait and loss of the normal toe off phase.4, 6 In the proportion of patients who remain ambulant, pressure ulcers commonly develop over the heels. The management should therefore be tailored to the needs of individual patients, but even in non-ambulant patientsreconstruction may be beneficial to allow footwear and facilitate positioning in a wheelchair. The aim of surgical reconstruction should be to achieve a plantigrade, stable, and brace-able foot.
No consensus has been established in the literature with regards to the best surgical approach. Rodrigues and Dias5 reviewed 76 patients with calcaneovalgus feet treated with either a complete anterior release (tenotomy of the tibialis anterior, extensor digitorium communis and extensor hallucis longus) or anterolateral release (associated tenotomy of the peroneus longus and brevis) for a mean of 4.66 years, with 81.5% achieving good results. Anterior tibialis tendon transfer to the calcaneus has also been described; Bliss and Meneleus8 reported on 46 such patients spanning over 12 years with only 4 feet remaining plantigrade. Park et al.6 reviewed 31 patients that underwent tibialis anterior tendon transfer, for a mean duration of 47 months. Twelve of these cases required accompanying osseous deformity correction, and there was no reported recurrence or worsening deformity noted in any of their patients.
A case series of 28 lower limb reconstructions in children and adolescents using Ilizarov frames by Kelley et al.9 reported positive results. In their series, all 19 patients with foot and ankle deformities had reconstructed feet that were plantigrade and brace-able.
The Ilizarov technique has been utilised since the 1950s to correct limb deformities. The basic components comprise of rings and connecting rods. Full rings provide the greatest degree of stability whereas half rings allow for increased access to the surgical site. The rings are connected with a minimum of four connecting rods and to the patient via at least two points of fixation.10
The Ilizarov technique provides several advantages. Firstly, correction of deformity is gradual, preventing trauma to and allowing stretch of the adjacent soft tissue, including overlying skin and neurovascular bundles. Secondly, direct access to overlying skin is possible, allowing close monitoring of the skin, which is often contracted and prone to complications in chronic deformities. In contrast, conventional surgical techniques requiring casting may result in complications such as skin necrosis, reported as high as 61%.8
In this patient, the Ilizarov technique was preferred as, in addition to the advantages listed above, it was deemed the rigidity and chronicity of deformity would not be amenable to correction purely with soft tissue release, transfer or tenotomy. The patient was also motivated, and had good social support to ensure compliance with the reconstructive process.
Pin site infections are the most common complication of Ilizarov frames, with reported rates of up to 100% in many case series.11, 12, 13, 14 Pin site and wound care is therefore essential, and resolution has been reported in up to 97% of cases with good wound care and appropriate antibiotic use.15 Additionally, the need for daily adjustment of the frame further necessitates that patients should be carefully selected, as compliance to frame adjustment and pin site care over a prolonged period of months requires a diligent patient with good support.
In the 2 years before starting the reconstructive process, the patient was admitted over 10 times for various issues involving feet ulcers and infection. Following the index surgery, no further unplanned admissions were required. The patient regained independent and pain free ambulation, and was delighted with the reconstructive result.
In conclusion, untreated and chronic severe calcaneovalgus foot deformities secondary to spina bifida rarely persist to present in adulthood in the developed world. Management and reconstruction in the adult is more complex for multiple reasons including rigidity of deformity, skin and soft tissue contractures, as well as pressure sores and infection. The Ilizarov technique offers an effective method for reconstruction of the bony deformity, while allowing gradual correction of the associated soft tissue contractures, in the adult patient. While the use of an Ilizarov frame requires a compliant patient and a competent surgeon, in the right hands it can reconstruct bony as well as soft tissue chronic deformities, and restore function in the adult patient.
Funding
Nil.
Ethical statement
Informed consent has been obtained from the patient and relatives.
Conflicts of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.04.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gunay H., Sozbilen M.C., Gurbuz Y. Incidence and type of foot deformities in patients with spina bifida according to level of lesion. Childs Nerv Syst. 2016;32:315–319. doi: 10.1007/s00381-015-2944-7. [DOI] [PubMed] [Google Scholar]
- 2.Frischhut B., Stöckl B., Landauer F. Foot deformities in adolescents and young adults with spina bifida. J Pediatr Orthop B. 2000 Jun;9:161–169. doi: 10.1097/01202412-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Westcott M.A., Dynes M.C., Remer E.M. Congenital and acquired orthopedic abnormalities in patients with myelomeningocele. Radiographics. 1992;12:1155–1173. doi: 10.1148/radiographics.12.6.1439018. [DOI] [PubMed] [Google Scholar]
- 4.Akbar M., Bresch B., Seyler T.M. Management of orthopaedic sequelae of congenital spinal disorders. J Bone Joint Surg Am. 2009;91(suppl 6):87–100. doi: 10.2106/JBJS.I.00613. [DOI] [PubMed] [Google Scholar]
- 5.Rodrigues R.C., Dias L.S. Calcaneus deformity in spina bifida: results of anterolateral release. J Pediatr Orthop. 1992;12:461–464. doi: 10.1097/01241398-199207000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Park K.B., Park H.W., Joo S.Y. Surgical treatment of calcaneal deformity in a select group of patients with myelomeningocele. J Bone Joint Surg Am. 2008;90:2149–2159. doi: 10.2106/JBJS.G.00729. [DOI] [PubMed] [Google Scholar]
- 7.Bruner J.P., Tulipan N. Tell the truth about spina bifida. Ultrasound Obstet Gynecol. 2004;24:595–596. doi: 10.1002/uog.1742. [DOI] [PubMed] [Google Scholar]
- 8.Bliss D.G., Menelaus M.B. The results of transfer of the tibialis anterior to the heel in patients who have a myelomeningocele. J Bone Joint Surg Am. 1986;68:1258–1264. [PubMed] [Google Scholar]
- 9.Kelley S.P., Bache C.E., Graham H.K. Limb reconstruction using circular frames in children and adolescents with spina bifida. J Bone Joint Surg Br. 2010;92:1017–1022. doi: 10.1302/0301-620X.92B7.22965. [DOI] [PubMed] [Google Scholar]
- 10.Spiegelberg B., Parratt T., Dheerendra S.K. Ilizarov principles of deformity correction. Ann R Coll Surg Engl. 2010;92:101–105. doi: 10.1308/003588410X12518836439326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grill F., Franke J. The Ilizarov distractor for the correction of relapsed or neglected clubfoot. J Bone Joint Surg Br. 1987;69-B:593–597. doi: 10.1302/0301-620X.69B4.3611163. [DOI] [PubMed] [Google Scholar]
- 12.Oganesian O.V., Istomina I.S. Talipes equinocavovarus deformities corrected with the aid of a hinged-distraction apparatus. Clin Orthop. 1991;266:42–50. [PubMed] [Google Scholar]
- 13.Paley D. The correction of complex foot deformities using Ilizarov's distraction osteotomies. Clin Orthop. 1993;293:97–111. [PubMed] [Google Scholar]
- 14.El-Barbary H., Abdel Ghani H., Hegazy M. Correction of relapsed or neglected clubfoot using a simple Ilizarov frame. Int Orthop. 2004;28:183–186. doi: 10.1007/s00264-004-0540-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aronson J. Experimental and clinical experience with distraction osteogenesis. Cleft Palate Craniofac J. 1994;31:473–481. doi: 10.1597/1545-1569_1994_031_0473_eacewd_2.3.co_2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.