Abstract
BACKGROUND:
Arsenic exposure has been related to numerous adverse cardiovascular outcomes. The aim of this study was to investigate the cross-sectional and prospective association between arsenic exposure with echocardiographic measures of left ventricular (LV) geometry and functioning.
METHODS:
A total of 1337 young adult participants free of diabetes mellitus and cardiovascular disease were recruited from the SHFS (Strong Heart Family Study). The sum of inorganic and methylated arsenic concentrations in urine (ΣAs) at baseline was used as a biomarker of arsenic exposure. LV geometry and functioning were assessed using transthoracic echocardiography at baseline and follow-up.
RESULTS:
Mean follow-up was 5.6 years, and median (interquartile range) of ΣAs was 4.2 (2.8–6.9) μg/g creatinine. Increased arsenic exposure was associated with prevalent LV hypertrophy, with an odds ratio (95% CI) per a 2-fold increase in ΣAs of 1.47 (1.05–2.08) in all participants and of 1.58 (1.04–2.41) among prehypertensive or hypertensive individuals. Measures of LV geometry, including LV mass index, left atrial systolic diameter, interventricular septum, and LV posterior wall thickness, were positively and significantly related to arsenic exposure. Among measures of LV functioning, stroke volume, and ejection fraction were associated with arsenic exposure.
CONCLUSIONS:
Arsenic exposure was related to an increase in LV wall thickness and LV hypertrophy in young American Indians with a low burden of cardiovascular risk factors. The relationship was stronger in participants with prehypertension or hypertension, suggesting that potential cardiotoxic effects of arsenic might be more pronounced in individuals already undergoing cardiovascular adaptive mechanisms following elevated systemic blood pressure.
Keywords: arsenic; blood pressure; echocardiography; heart failure; hypertension; hypertrophy, left ventricular
Inorganic arsenic is a well-established human toxic and carcinogen that can be found in groundwater, food, soil, and air.1 Chronic exposure to inorganic arsenic (iA) has been associated with an increased risk for cardiovascular disease and its risk factors, including hypertension,2 diabetes mellitus,3,4 carotid atherosclerosis,5 and peripheral artery disease.6,7 Importantly, arsenic exposure has been related to cardiovascular mortality and adverse cardiac events, particularly, ischemic heart disease and other forms of heart disease.8–12 However, the relationship of arsenic exposure with adverse cardiac outcomes is not fully understood. Inorganic arsenic is related to hypertension and diabetes mellitus, the main risk factors for the development of cardiac dys-function.13,14 It is unknown whether inorganic arsenic is related to cardiac structure and functioning or if the observed adverse outcomes are secondary to a worse cardiometabolic profile of arsenic-exposed individuals.
Cardiac geometry and functioning, notably the dimension and function of the left ventricle (LV), can be reliably and reproducibly assessed with transthoracic echocardiography (TTE).15 LV hypertrophy (LVH), LV systolic dysfunction, and LV diastolic dysfunction are strong independent predictors of survival in both individuals with a history of cardiac disease and individuals free of overt cardiovascular disease.16–18 A change in magnitude or direction of baseline values of TTE-based measures of LV mass and functioning is followed by a corresponding change in risk for fatal and nonfatal cardiovascular events.19,20 In addition, treatment targeting asymptomatic patients with LVH, LV systolic dysfunction, or LV diastolic dysfunction may slow the natural progression to heart failure and reduce subsequent morbidity and mortality.21,22 Accordingly, abnormal TTE-based measurements of cardiac geometry and function are established surrogates for heart failure and adverse cardiac outcomes. Nevertheless, the risk factors and pathophysiological mechanisms involved in the disproportionate growth of the heart and consecutive alteration in cardiac function are not fully understood.23
Inorganic arsenic has been positively related to cardiovascular surrogate end points, including subclinical atherosclerosis, QT interval prolongation, and circulating markers of endothelial dysfunction.24 In a small cross-sectional study of children in Central Mexico, arsenic exposure was associated with a higher LV mass and a lower systolic function.25 Animal studies have shown that exposure to arsenic is followed by cardiac dysfunction, including myocyte apoptosis, fibrosis, and subsequent LVH.26,27 In contrast, the potential impact of arsenic exposure on LVH, LV systolic dysfunction, and LV diastolic dysfunction in adult populations free of cardiovascular disease has not been studied before. The main objective of the present study was to evaluate the association of arsenic exposure with cardiac geometry and LV function in adolescents and young adults exposed to low-to-moderate arsenic level in drinking water from Arizona, Oklahoma, and North and South Dakota who participated in the SHFS (Strong Heart Family Study).
METHODS
Outside investigators may apply to use the data generated in this study according to the established protocols for SHS (Strong Heart Study) Resource and Data Sharing, including community approval, through a formal application process which is detailed in the SHS Website (https://strongheartstudy.org/Research/Study-Data-and-Study-Samples/Study-Data).
Study Population
The SHS is a population-based prospective cohort designed to evaluate cardiovascular disease and its risk factors in American Indians (45 to 74 years old) residing in Arizona, Oklahoma, North Dakota, and South Dakota and ongoing since 1988.28 The SHFS is an extension of the SHS that recruited 3838 men and women from 94 large families of SHS participants in 2 phases: 1998 to 1999 (SHS phase III) and 2001 to 2004 (SHS phase IV). A follow-up visit was conducted from 2007 to 2009 (SHS phase V). Although the SHS and the SHFS were not originally started to study arsenic exposure, the importance of studying arsenic was recognized over time as increasing evidence supported the role of arsenic in cardiovascular disease29 and the relatively high arsenic exposure in tribal communities compared with other general populations in the United States.30,31
In 2016, 1 community withdrew their consent to participate in further research; therefore, data from 919 participants from that community were not used for the present study, leaving a total of 2919 participants eligible for this study. At baseline, in-person interviews, physical examinations, and biological specimens were obtained. TTE was conducted at SHS phases IV and V. For this study, we a priori restricted the analyses to participants ≤50 years, free of cardiovascular disease, and free of diabetes mellitus at baseline (N=1941). We then excluded 133 participants without complete baseline data on TTE-measured variables at phase IV and 442 participants with missing urine arsenic measures at phase IV. A total of 1366 SHFS participants aged 14 to 50 years had complete data on TTE-measured variables and urine arsenic measurements at SHS phase IV. We further excluded 20 participants due to missing data on covariables of interest and 9 participants with outlier levels (defined as values ≥ 2×percentile 99th) of measured TTE variables, leaving 1337 participants for this analysis (Figure I in the Data Supplement). The present study was approved by institutional review boards from the participating academic institutions, Indian Health Service institutional review boards, and each participating tribe. At enrollment, written informed consent was obtained from all participants.
Urine Arsenic
Morning spot urine samples were collected in polypropylene tubes, frozen within 1 to 2 hours of collection, and stored at −70°C. For arsenic analyses, up to 1.0 mL from each urine sample was transported on dry ice to the Trace Element Laboratory at Graz University, Austria. Total urine arsenic concentrations were measured using inductively coupled plasma mass spectrometry. The urine concentrations of iAs (ie, arsenite plus arsenate), methylarsonate, dimethylarsinate, and arsenobetaine were measured using high-performance liquid chromatography (HPLC)–inductively coupled plasma mass spectrometry (Agilent 1100 HPLC and Agilent 7700x ICP-MS, Agilent Technologies, Waldbronn Germany). The limit of detection for the arsenic species was 0.1 μg As/L. Among the 1337 participants selected for the present study, 129 (9.6%) and 37 (2.8%) had iAs and methylarsonate concentrations below the limit of detection, respectively. The concentrations below the limit of detection were imputed as the limit of detection divided by the square root of 2. The sum of inorganic and methylated arsenic concentrations (ΣAs) in urine is an established biomarker of exposure to iA from water and food and was used as a biomarker of exposure, hereafter referred to as arsenic.32 Arsenic concentrations were divided by urine creatinine to account for urine dilution and expressed as μg/g creatinine. Prior research in the SHS population showed an intraclass coefficient of combined inorganic and methylated arsenic species of 0.64 and an average change in urine arsenic concentration between study visits spanning 10 years of −0.8 μg/g urine creatinine,30 supporting the use of urinary arsenic as a surrogate of long-term arsenic exposure. Previous studies conducted in the SHS population showed low levels of arsenobetaine, a measure of seafood arsenicals, indicating that seafood consumption was low in the community.8
Echocardiographic Measures
Transthoracic echocardiograms were performed by expert sonographers, according to standardized methods, and reviewed offline by 2 readers,33 with ≈97% of studies finally interpreted by a single highly experienced investigator, following the American Society of Echocardiography recommendations.34 Phased-array echocardiographs with M-mode, 2-dimensional and Doppler capabilities were used for the assessment of cardiac geometry and function. At least 10 consecutive beats of 2-dimensional and M-mode recordings of cardiac geometry parameters were recorded in the parasternal acoustic window at or just below the tips of the mitral leaflets in both long and short-axis views.
Cardiac geometry was assessed by the following parameters: Left atrium diameter in systole and LV internal diameter, interventricular septum, LV posterior wall thickness, and relative wall thickness were measured at end diastole. LV mass was calculated by a necropsy-validated formula35 and normalized for body surface area.36 LVH was defined as a ratio of LV mass/body surface area higher than 115 g/m2 in men and higher than 95 g/m2 in women, respectively. Cardiac systolic functioning was assessed as follows: ejection fraction was calculated from LV linear dimensions,37 and stroke volume was derived by Doppler method.38 Cardiac diastolic functioning was evaluated by Doppler interrogation. Transmitral early (E) and late (A) LV filling velocities were measured at the annular level and used to calculate the early peak rapid filling velocity to peak atrial filling velocity ratio (E/A ratio). Likewise, deceleration time of early diastolic LV filling and the atrial filling fraction were assessed. Isovolumic relaxation time (IVRT) reflects active LV relaxation and was measured between aortic valve closure and mitral valve opening.
Other Variables
The standardized questionnaire included sociodemographic data (age, sex, income), smoking history, physical activity, and medical history.39 Measurement of height, weight and blood pressure (BP), as well as collection of blood and urine, was performed by centrally trained nurses and medical assistants following standardized protocols.28 Body mass index (BMI) was calculated dividing measured weight in kilograms by measured height in meters squared. The methods of BP measurement and assessment of laboratory variables, including fasting glucose, lipoproteins, plasma creatinine, urine albumin, and urine creatinine, have been described previously.40 Prehypertension or hypertension status was defined as systolic BP ≥120 mm Hg, diastolic BP ≥80 mm Hg, or record of use of antihypertensive medications in the clinical history. Accordingly, normal pressure was defined as systolic BP <120 mm Hg and diastolic BP <80 mm Hg and never use of antihypertensive medications. Dyslipidaemia was defined as having total cholesterol ≥200 mg/dL, LDL (low-density lipoprotein)-cholesterol ≥130 mg/dL, HDL (high-density lipoprotein)-cholesterol ≤40 mg/dL, total triglycerides ≥150 mg/dL, or use of lipid-lowering medications in the clinical history. All participants were free of diabetes mellitus (following the American Diabetes Association criteria) at baseline visit due to study design. Prediabetes mellitus was defined as having fasting glucose levels ≥100 mg/dL. The glomerular filtration rate was estimated (estimated glomerular filtration rate [eGFR]) by the chronic kidney disease–Epidemiology Collaboration abbreviated formula.41 Chronic kidney disease was defined as an eGFR lower than 60 mL(min·1.73 m2) or abnormal albuminuria status (ratio of albumin to creatinine >30 mg/g). Kidney function has shown to interfere with iA excretion in urine and adjustment for eGFR is recommended in analyses of urinary arsenic.42
Statistical Analysis
Baseline participants’ characteristics, including levels on TTE-measured variables, were described by quartiles of urine arsenic levels. P values of trend of the described participant’s characteristics across arsenic quartiles were also calculated. Spearman correlation coefficients were calculated to explore the relationship between urine arsenic and each measure of cardiac geometry and functioning. Urine arsenic levels were log-transformed for the analyses to improve normality. Odds ratios (OR) of prevalent and incident LVH by arsenic levels were estimated using logistic regression models. Cox proportional hazard models were not performed for incident LVH because of lack of information on the exact time when the incident cases occurred. OR of incident LVH were further adjusted for length of follow-up in years for sensitivity analysis. For continuous measures of cardiac geometry and function, baseline mean difference, annual mean change, and mean difference at 5 years of follow-up by an increase in arsenic levels were estimated using linear mixed effect models with random intercept and slope over time. Family clustering was accounted for in both logistic and mixed effect models. Models were conducted in the overall study sample and also stratified by normal BP and prehypertension/hypertension status. Arsenic was introduced in the models as a continuous variable, and the results were per a 2-fold increase in arsenic levels (per doubling). Models were adjusted progressively. Model 1 was adjusted for age and sex. Model 2 was additionally adjusted for study site, smoking status (never, former, current), BMI, dyslipidemia, eGFR, fasting glucose, systolic BP, and hypertension treatment. Study site was included because there is some geographic variation in arsenic exposure. Smoking status and BMI were included as markers of behavioral patterns that are risk factors for the study outcomes that could be related to arsenic exposure from water and food. Dyslipidaemia, fasting glucose, systolic BP, and hypertension treatment were included as major risk factors for cardiac outcomes. eGFR was included as a risk factor for cardiac outcomes that can interfere with arsenic excretion in the urine. To allow more flexible evaluation of the dose-response between iA exposure and cardiac structure/function, we graphically described the cross-sectional and prospective mean differences of LV measurements and ORs of LVH based on restricted cubic splines of the urine arsenic distribution.
Secondary analyses were performed to explore whether the associations between arsenic exposure and the continuous measures of LV geometry and functioning were modified by sex, smoking status, BMI (<30, ≥30 kg/m2), lipid treatment (no, yes), fasting glucose (normal, impaired), and BP (normal, prehypertension, or hypertension) by including interaction terms in linear regression models. In sensitivity analyses, we also further adjusted for tungsten and uranium, metals that tend to cooccur with arsenic in drinking water31 and could be related to cardiovascular disease,43,44 with similar findings (not shown). The data were analyzed using R software (version 3.0.3; R Development Core Team 2014). A 2-sided P value of <0.05 was considered statistically significant.
RESULTS
Study Population and Cardiac Measures
Characteristics of study participants and echocardio-graphic measures at baseline are presented in Table 1. Mean follow-up during the study period was 5.6 years. Median (interquartile range) of urine arsenic at baseline was 4.24 (2.82–6.90) μg/g creatinine. Urine arsenic levels were higher in older individuals, females, smokers, and in participants with higher BMI. Higher urine arsenic levels were observed in individuals with higher LV mass index, left atrial diameter, interventricular septum thickness, LV posterior wall thickness, relative wall thickness, stroke volume, ejection fraction, and mitral A-velocity.
Table 1.
Characteristics of Study Participants at Baseline Overall and by Urinary Arsenic Levels
| Sum of Inorganic and Methylated Arsenic Species (μg/g Creatinine) | |||||||
|---|---|---|---|---|---|---|---|
| Overall (0.42–91.49) | Q1 (<2.82) | Q2 (2.82–4.24) | Q3 (4.24–6.90) | Q4 (>6.90) | P Value of Trend | ||
| N (%) | 1337 (100) | 335 (25.1) | 336 (25.1) | 332 (24.8) | 334 (25) | ||
| Female, n (%) | 811 (60.7) | 196 (58.5) | 180 (53.6) | 217 (65.4) | 218 (65.3) | 0.003 | |
| Age, y | 30.7 (10.4) | 29.6 (10) | 30.2 (10.5) | 31.5 (10.4) | 31.6 (10.4) | 0.005 | |
| Smoking, n (%) | |||||||
| Never | 565 (42.3) | 167 (49.9) | 146 (43.5) | 131 (39.5) | 121 (36.2) | 0.003 | |
| Former | 246 (18.4) | 67 (20.0) | 57 (17.0) | 60 (18.1) | 62 (18.6) | ||
| Current | 526 (39.3) | 101 (30.1) | 133 (39.6) | 141 (42.5) | 151 (45.2) | ||
| BMI, kg/m2 | 30.2 (7.4) | 29.8 (6.7) | 29.7 (6.9) | 30.1 (7.3) | 31.2 (8.3) | 0.011 | |
| Systolic BP, mmHg | 117.7 (13.2) | 117.6 (13.2) | 118.2 (13.4) | 116.4 (12.6) | 118.6 (13.5) | 0.73 | |
| Diastolic BP, mmHg | 75.3 (11) | 75.1 (11.1) | 75.1 (11.8) | 74.7 (10.9) | 76.2 (10.2) | 0.29 | |
| Hypertension, n (%) | 192 (14.4) | 46 (13.7) | 58 (17.3) | 38 (11.4) | 50 (15.0) | 0.19 | |
| Prehypertension or hypertension, n (%) | 664 (49.7) | 167 (49.9) | 166 (49.4) | 161 (48.5) | 170 (50.9) | 0.94 | |
| BP treatment, n (%) | 61 (4.6) | 18 (5.4) | 14 (4.2) | 10 (3.0) | 19 (5.7) | 0.33 | |
| Fasting glucose, mg/dL | 92 (9.4) | 91.7 (8.6) | 92.2 (9.2) | 91.7 (9.4) | 92.4 (10.3) | 0.56 | |
| Prediabetes mellitus, n (%) | 254 (19.0) | 61 (18.2) | 67 (19.9) | 63 (19.0) | 63 (18.9) | 0.95 | |
| Dyslipidaemia, n (%) | 687 (51.4) | 174 (51.9) | 176 (52.4) | 162 (48.8) | 175 (52.4) | 0.75 | |
| eGFR, mL/(min-1.73 m2) | 123.4 (15.7) | 121.4 (14.7) | 122.8 (15.3) | 123.1 (16.6) | 126.5 (15.7) | <0.001 | |
| CKD, n (%) | 106 (7.9) | 23 (6.9) | 20 (6.0) | 28 (8.4) | 35 (10.5) | 0.14 | |
| Cardiac geometry | |||||||
| Left atrium diameter, cm | 3.54 (0.44) | 3.48 (0.46) | 3.51 (0.43) | 3.56 (0.41) | 3.61 (0.46) | <0.001 | |
| LV internal diameter, cm | 5.30 (0.42) | 5.30 (0.43) | 5.32(0.41) | 5.27(0.41) | 5.30 (0.43) | 0.70 | |
| Interventricular septum, cm | 1.19 (0.12) | 1.17 (0.12) | 1.19 (0.11) | 1.18 (0.11) | 1.21 (0.13) | <0.001 | |
| LV posterior wall thickness, cm | 1.22 (0.11) | 1.19 (0.11) | 1.21 (0.10) | 1.21 (0.1) | 1.25 (0.11) | <0.001 | |
| Relative wall thickness | 0.286 (0.038) | 0.281 (0.038) | 0.284 (0.037) | 0.285 (0.04) | 0.292 (0.038) | <0.001 | |
| LV mass index, g/m2 | 76.7 (14.3) | 75.4 (14.5) | 76.6 (13.2) | 76 (14.1) | 78.6 (15.0) | 0.01 | |
| LV hypertrophy (LVMI), n (%) | 61 (4.6) | 14 (4.2) | 9 (2.7) | 13 (3.9) | 25 (7.5) | 0.021 | |
| Cardiac function | |||||||
| Heart rate, bpm | 65.9 (10.3) | 65.6 (9.2) | 66.1 (10.6) | 64.9 (10) | 67 (11.1) | 0.27 | |
| Stroke volume, mL | 81.8 (14.4) | 81 (14.7) | 81 (13.7) | 81.3 (14.4) | 84.1 (14.6) | 0.006 | |
| Ejection fraction, % | 60.0 (5.0) | 59.7 (5.2) | 59.7 (5.0) | 60.1 (4.7) | 60.6 (5.2) | 0.009 | |
| Mitral E-velocity, cm/s | 69.7 (14.1) | 69.4 (15.5) | 70.2 (14.1) | 69.4 (13.4) | 69.7 (13.3) | 0.98 | |
| Mitral A-velocity, cm/s | 51.6 (11.7) | 50.3 (11.3) | 52.4 (12.2) | 51.2 (11.9) | 52.7 (11.5) | 0.031 | |
| E/A ratio | 1.42 (0.43) | 1.45 (0.45) | 1.40 (0.41) | 1.43 (0.47) | 1.38 (0.39) | 0.11 | |
| Atrial filling fraction | 0.26 (0.08) | 0.26 (0.08) | 0.26 (0.07) | 0.26 (0.08) | 0.26 (0.08) | 0.84 | |
| Deceleration time, ms | 168.9 (34.4) | 170.4 (35) | 168.4 (31.1) | 168.8 (35.9) | 168 (35.6) | 0.41 | |
| IVRT, ms | 75.9 (10.6) | 76.9 (10.7) | 75.7 (11.0) | 75.9 (10.3) | 75.2 (10.5) | 0.06 | |
Data are mean±SD. LV hypertrophy (LVMI), LV hypertrophy category based on LVMI. Prediabetes mellitus was defined as fasting glucose levels between 110 and 126 mg/dL (participants with diabetes mellitus were excluded from the study). BMI indicates body mass index; BP, blood pressure; CKD, chronic kidney disease; E/A, early peak rapid filling velocity to peak atrial filling velocity; eGFR, estimated glomerular filtration rate; IVRT, isovolumic relaxation time; LV, left ventricular; and LVMI, LV mass index.
Association Between Arsenic Exposure and LV Geometry
The Spearman correlation coefficients of urine arsenic with each of the LV geometry measures at baseline were positive and statistically significant, except for LV internal diameter (Figure II in the Data Supplement). Overall, the prevalence of LVH was 4.6%. In fully adjusted models, the OR (95% CI) for prevalent LVH per a 2-fold increase in urinary arsenic levels were 1.47 (1.05–2.08) in all participants and 1.58 (1.04–2.41) among prehypertensive or hypertensive individuals (Table 2). Arsenic concentrations were not associated with incident LVH (Table 2; Table I in the Data Supplement).
Table 2.
Odds Ratio (95% CI) for Left Ventricular Alterations at Baseline (2001–2004) and at Follow-Up (2006–2009) Per a 2-Fold Increase in Urinary Arsenic Levels, Among All Participants and by Blood Pressure Status
| Baseline | Follow-Up | |||||
|---|---|---|---|---|---|---|
| Cases/Noncases | Prevalence OR (95% Cl) | Cases/Noncases | Incidence OR (95% Cl) | |||
| Model 1 | Model 2 | Model 1 | Model 2 | |||
| LV hypertrophy (LVMI) | ||||||
| All participants | 61/1276 | 1.37 (0.99–1.92) | 1.47 (1.05–2.08) | 28/1162 | 0.91 (0.53–1.55) | 0.95 (0.58–1.56) |
| Prehypertension/hypertension | 42/622 | 1.51 (1.02–2.23) | 1.58 (1.04–2.41) | 23/554 | 0.85 (0.48–1.54) | 0.82 (0.45–1.50) |
| Normal BP | 19/654 | 1.08 (0.61–1.91) | 1.20 (0.64–2.26) | 5/608 | 1.28 (0.68–2.38) | 1.20 (0.59–2.43) |
Model 1 adjusted for age and sex.
Model 2 additionally adjusted for region, smoking (never, former, current), body mass index (continuous), dyslipidemia (no/yes), fasting glucose level (continuous), estimated glomerular filtration rate (continuous), systolic BP (continuous), and BP treatment (no/yes). BP indicates blood pressure; LV, left ventricular; LVMI, LV mass index; and OR, odds ratio.
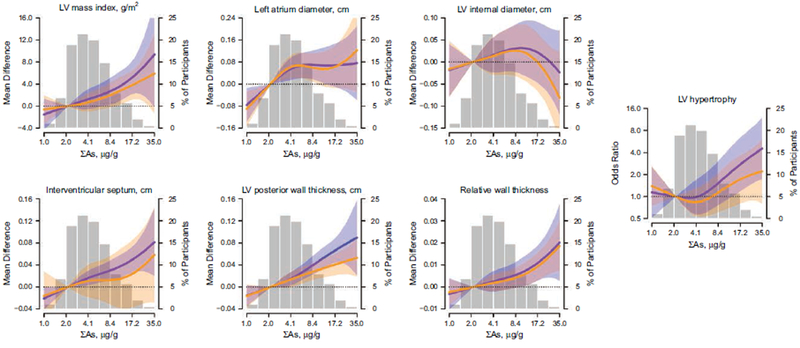
At baseline, the continuous LV geometry measures LV mass index, left atrial systolic diameter, interventricular septum, and LV posterior wall thickness were positively associated with arsenic exposure in fully adjusted models (Tables 3 and 4, Figure 1). In particular, baseline LV posterior wall thickness and inter-ventricular septum showed a positive association with arsenic exposure in the overall study population, whereas the impact of arsenic on LV mass index was observed in prehypertensive or hypertensive subjects but not in participants with normal BP when participants were stratified according to hypertension status (Table 4). Left atrial systolic diameter was not significantly related to arsenic when the study population was divided according to hypertension status. At follow-up, the associations between arsenic exposure with LV mass index and LV posterior wall thickness were somewhat attenuated but remained statistically significant. Interventricular septum thickness was not related to arsenic at follow-up. During follow-up, 23 individuals with prehypertension or hypertension and 5 participants with normal BP developed LVH. Urine arsenic was not associated with incident LVH (Table 2). LV mass index and LV posterior wall thickness decreased during follow-up compared with baseline examination (mean change, −0.58 g/m2 and −0.02 mm, respectively). Despite the negative annual change in mean values, the mean differences in LV mass index and LV posterior wall thickness at baseline and follow-up were similar per an increase in urinary arsenic levels (Table 3, Figure 1). Effect modifications of the associations were observed in some interaction analyses (Table II in the Data Supplement). In particular, participants with prehypertension/hypertension status showed a stronger association of urine arsenic with LV mass index (Geometric Mean Ratio [95% CI]: 2.43 [1.03–3.84]; P interaction=0.05) and with LV internal diameter (Geometric Mean Ratio [95% CI]: 0.03 [0.00–0.06]; P interaction=0.04). Never smokers showed a stronger association of urine arsenic with LV posterior wall thickness (Geometric Mean Ratio [95% CI]: 0.02 [0.01–0.03], P interaction=0.01) and relative wall thickness (Geometric Mean Ratio [95% CI]: 0.00 [0.00–0.01], P interaction=0.02).
Table 3.
Mean difference (95% CI) of left ventricular measurements per a 2-fold increase in urinary arsenic levels overall at baseline and at follow-up. Mean (95% CI) of annual change during follow-up for the same comparison.
| All Participants | ||||
|---|---|---|---|---|
| N | MD at Baseline | Annual Change | MD at Follow-Up | |
| LV geometry | ||||
| LV mass index, g/m2 | 1252 | 1.69 (0.88 to 2.49) | −0.10 (−0.19 to−0.01) | 1.17 (0.39 to 1.96) |
| Left atrial systolic diameter, cm | 1264 | 0.03 (0.01 to 0.05) | −0.00 (−0.00 to 0.00) | 0.02 (0.00 to 0.04) |
| LV internal diameter, cm | 1258 | 0.01 (−0.01 to 0.03) | −0.00 (−0.00 to 0.00) | −0.00 (−0.02 to 0.02) |
| Interventricular septum, cm | 1266 | 0.02 (0.01 to 0.02) | −0.00 (−0.01 to 0.00) | 0.01 (−0.00 to 0.01) |
| LV posterior wall thickness, cm | 1096 | 0.02 (0.02 to 0.03) | −0.00 (−0.00 to −0.00) | 0.01 (0.01 to 0.02) |
| Relative wall thickness | 1257 | 0.00 (0.00 to 0.01) | −0.00 (−0.00 to 0.00) | 0.00 (0.00 to 0.01) |
| LV functioning | ||||
| Heart rate, bpm | 1239 | 0.04 (−0.59 to 0.67) | 0.01 (−0.12 to 0.1 5) | 0.11 (−0.47 to 0.70) |
| Stroke volume, mL | 1228 | 1.56 (0.78 to 2.35) | −0.26 (−0.42 to-0.10) | 0.26 (−0.48 to 1.01) |
| Ejection fraction, % | 1257 | 0.35 (0.05 to 0.65) | −0.02 (−0.06 to 0.03) | 0.25 (−0.02 to 0.53) |
| Mitral E-velocity, cm/s | 1239 | −0.48 (−1.24 to 0.29) | 0.28(0.11 to 0.46) | 0.93 (0.24 to 1.62) |
| Mitral A-velocity, cm/s | 1237 | −0.40 (−1.03 to 0.24) | 0.11 (−0.03 to 0.25) | 0.14 (−0.43 to 0.72) |
| E/A ratio | 1237 | −0.00 (−0.02 to 0.02) | 0.00 (0.00 to 0.01) | 0.02 (−0.00 to 0.03) |
| Atrial filling fraction | 1184 | −0.00 (−0.01 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) |
| Deceleration time, ms | 1238 | −0.89 (−2.96 to 1.18) | 0.59 (0.09 to 1.10) | 2.07 (0.18 to 3.96) |
| Isovolumic relaxation time, ms | 1214 | −0.79 (−1.38 to-0.20) | 0.21 (0.07 to 0.34) | 0.25 (−0.28 to 0.79) |
Model was adjusted for age, sex, region, smoking (never, former, current), body mass index (continuous), dyslipidemia (no/yes), fasting glucose level (continuous), estimated glomerular filtration rate (continuous), systolic BP (continuous), and BP treatment (no/yes). BP indicates blood pressure; CI, confidence interval; E/A, early peak rapid filling velocity to peak atrial filling velocity; LV, left ventricular; and MD, mean difference.
Table 4.
Mean difference (95% CI) of left ventricular measurements per a 2-fold increase in urinary arsenic levels by blood pressure status at baseline and at follow-up. Mean (95% CI) of annual change during follow-up for the same comparison.
| Prehypertension/Hypertension | Normal Blood Pressure | |||||||
|---|---|---|---|---|---|---|---|---|
| N | MD at Baseline | Annual Change | MD at Follow-Up | N | MD at Baseline | Annual Change | MD at Follow-Up | |
| LV geometry | ||||||||
| LV mass index, g/m2 | 620 | 2.36 (1.17 to 3.56) | −0.15 (−0.28 to−0.01) | 1.64 (0.47 to 2.80) | 632 | 0.88 (−0.23 to 1.99) | −0.06 (−0.19 to 0.07) | 0.58 (−0.49 to 1.65) |
| Left atrial systolic diameter, cm | 629 | 0.03 (−0.00 to 0.06) | 0.00 (−0.00 to 0.00) | 0.03 (−0.00 to 0.06) | 635 | 0.03 (0.00 to 0.06) | −0.00 (−0.01 to 0.00) | 0.02 (−0.01 to 0.05) |
| LV internal diameter, cm | 624 | 0.03 (−0.01 to 0.06) | −0.00 (−0.00 to 0.00) | 0.02 (−0.01 to 0.05) | 634 | −0.01 (−0.04 to 0.02) | −0.00 (−0.01 to 0.00) | −0.02 (−0.05 to 0.00) |
| Interventricular septum, cm | 629 | 0.02 (0.01 to 0.03) | −0.00 (−0.01 to 0.00) | 0.01 (−0.00 to 0.02) | 637 | 0.01 (0.00 to 0.02) | −0.00 (−0.01 to 0.00) | 0.01 (−0.00 to 0.01) |
| LV posterior wall thickness, cm | 543 | 0.02 (0.02 to 0.03) | −0.00 (−0.00 to−0.00) | 0.01 (0.01 to 0.02) | 553 | 0.02 (0.01 to 0.03) | −0.00 (−0.00 to 0.00) | 0.01 (0.01 to 0.02) |
| Relative wall thickness | 623 | 0.00 (−0.00 to 0.01) | −0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.01) | 634 | 0.01 (0.00 to 0.01) | −0.00 (−0.00 to 0.00) | 0.00 (0.00 to 0.01) |
| LV functioning | ||||||||
| Heart rate, bpm | 616 | −0.57 (−1.45 to 0.32) | 0.11 (−0.04 to 0.27) | −0.01 (−0.83 to 0.82) | 623 | 0.67 (−0.24 to 1.58) | −0.06 (−0.28 to 0.17) | 0.39 (−0.45 to 1.24) |
| Stroke volume, mL | 607 | 1.89 (0.72 to 3.07) | −0.28 (−0.50 to −0.06) | 0.49 (−0.63 to 1.62) | 621 | 1.20 (0.1 5 to 2.25) | −0.24 (−0.47 to −0.00) | 0.02 (−0.97 to 1.01) |
| Ejection fraction, % | 623 | 0.25 (−0.16 to 0.67) | 0.01 (−0.06 to 0.07) | 0.29 (−0.10 to 0.68) | 634 | 0.45 (0.01 to 0.88) | −0.05 (−0.11 to 0.01) | 0.21 (−0.20 to 0.61) |
| Mitral E-velocity, cm/S | 617 | −0.37 (−1.47 to 0.73) | 0.29 (0.04 to 0.53) | 1.07 (0.07 to 2.06) | 622 | −0.68 (−1.74 to 0.38) | 0.28 (0.03 to 0.52) | 0.72 (−0.24 to 1.68) |
| Mitral A-velocity, cm/s | 616 | −0.60 (−1.47 to 0.26) | 0.19 (−0.01 to 0.39) | 0.36 (−0.42 to 1.14) | 621 | −0.21 (−1.14 to 0.72) | 0.00 (−0.19 to 0.20) | −0.20 (−1.05 to 0.65) |
| E/A ratio | 616 | 0.01 (−0.01 to 0.04) | 0.00 (−0.00 to 0.01) | 0.01 (−0.01 to 0.04) | 621 | −0.02 (−0.05 to 0.01) | 0.01 (0.00 to 0.01) | 0.02 (−0.01 to 0.05) |
| Atrial filling fraction | 589 | −0.00 (−0.01 to 0.00) | 0.00 (0.00 to 0.00) | 0.00 (−0.00 to 0.01) | 595 | −0.00 (−0.01 to 0.00) | −0.00 (−0.00 to 0.00) | −0.00 (−0.01 to 0.00) |
| Deceleration time, ms | 616 | −1.14 (−3.98 to 1.71) | 0.44 (−0.23 to 1.11) | 1.05 (−1.56 to 3.66) | 622 | −0.92 (−3.94 to 2.09) | 0.77 (0.00 to 1.54) | 2.94 (0.20 to 5.67) |
| Isovolumic relaxation time, ms | 595 | −0.76 (−1.62 to 0.09) | 0.25 (0.06 to 0.44) | 0.50 (−0.29 to 1.28) | 619 | −0.78 (−1.60 to 0.04) | 0.16 (−0.04 to 0.36) | 0.02 (−0.72 to 0.76) |
Model was adjusted for age, sex, region, smoking (never, former, current), body mass index (continuous), dyslipidemia (no/yes), fasting glucose level (continuous), estimated glomerular filtration rate (continuous), systolic BP (continuous), and BP treatment (no/yes). BP indicates blood pressure; CI, confidence interval; E/A, early peak rapid filling velocity to peak atrial filling velocity; LV, left ventricular; and MD, mean difference.
Figure 1. Cross-sectional and prospective mean differences and odds ratio of left ventricular (LV) geometry measures by urine arsenic levels.
Lines (shaded areas) represent the adjusted mean differences or odds ratios (95% CI) of left ventricular geometry measures based on restricted cubic splines for log-transformed ΣAs distribution with knots at 10th, 50th, and 90th percentiles. The reference value was set at 10th percentile. Blue lines (blue shaded areas) represent association at baseline, and orange lines (orange shaded areas) represent association at follow-up. Models were adjusted for sex, age, region, smoking (never, former, current), body mass index (continuous), dyslipidemia (no/yes), fasting glucose level (continuous), estimated glomerular filtration rate (continuous), systolic blood pressure (BP; continuous), and BP treatment (no/yes). The histograms in the background represent the distribution of ΣAs. The extreme tails of the histograms were truncated because 3 participants had ΣAs levels <1.0 μ g/g, and 6 participants had ΣAs levels >35.0 μg/g.
Association Between Arsenic Exposure and LV Function
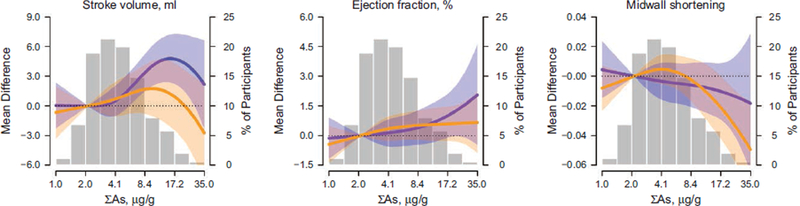
The Spearman correlation between arsenic exposure and measures of LV functioning were weak but significantly positive for stroke volume, ejection fraction, and mitral A-velocity (Figure III in the Data Supplement). Arsenic exposure was associated with systolic function at baseline (Tables 3 and 4, Figure 2). In fully adjusted models, the mean differences (95% CI) of stroke volume per a 2-fold increase in urinary arsenic levels were 1.56 mL (0.78–2.35) in all participants and 1.89 mL (0.72–3.07) in individuals with BP levels higher than 120/80 mm Hg. Arsenic was further associated with ejection fraction in all participants and individuals with normal BP. At follow-up, stroke volume and ejection fraction were not significantly related to arsenic (Figure 2). The annual change in mean stroke volume by arsenic levels was negative (Tables 3 and 4).
Figure 2. Dose-response relationships of arsenic and left ventricular functioning measures.
Lines (shaded areas) represent the adjusted mean difference (95% CI) of left ventricular function measures based on restricted cubic splines for log-transformed ΣAs distribution with knots at 10th, 50th, and 90th percentiles. The reference value was set at 10th percentile. Models were adjusted for sex, age, region, smoking (never, former, current), body mass index (continuous), dyslipidemia (no/yes), fasting glucose level (continuous), estimated glomerular filtration rate (continuous), systolic blood pressure (BP; continuous), and BP treatment (no/yes). The histograms in the background represent the distribution of ΣAs. The extreme tails of the histograms were truncated because 3 participants had ΣAs levels <1.0 μ g/g, and 6 participants had ΣAs levels >35.0 μg/g.
Regarding diastolic function, arsenic exposure was inversely associated with IVRT at baseline in fully adjusted models (Table 3, Figure 2). The relationship lost statistical significance when the study participants were stratified by BP status. At follow-up, mitral E-velocity was positively associated with arsenic in prehypertensive and hypertensive individuals, whereas deceleration time was positively related in participants with normal BP (Table 4, Figure 2). The annual change in means of mitral E-velocity and IVRT was positive (Tables 3 and 4). Mitral A-velocity, E/A ratio, and atrial filling fraction were not consistently associated with arsenic exposure. In interaction analysis, the following effect modifications were observed for the associations with urinary arsenic: by BP status for E/A ratio (P interaction=0.04); by BMI for stroke volume (P interaction=0.04) and mitral E-velocity (P interaction=0.04); by lipid treatment for mitral A-velocity (P interaction=0.01) and atrial filling fraction (P interaction=0.01); and by fasting glucose status for mitral A-velocity (P interaction=0.03) and deceleration time (P interaction<0.001; Tables III and IV in the Data Supplement).
We also conducted analyses for arsenic metabolism based on the relative percentage of each of the species over their sum (iAs%, methylarsonate%, and dimethylarsinate%) with the measures of LV geometry and LV functioning as study outcomes. The adjustments in these models were similar as in our analyses for arsenic exposure with additional adjustment for arsenic exposure levels as measured in urine. For the majority of the outcomes, the associations with arsenic metabolites were null, and although a few outcomes showed significant associations, those were inconsistent across the 3 arsenic metabolism biomarkers (Tables V, VI, and VII in the Data Supplement).
DISCUSSION
The present study conducted in young adult American Indians free of cardiovascular disease at baseline showed that low-level arsenic exposure was associated with increased LV wall thickness and LV mass. Urinary arsenic was positively related to LVH, predominantly in prehypertensive and hypertensive individuals. Moreover, a positive association between arsenic exposure with stroke volume and ejection fraction, determinants of cardiac output, was found. Regarding diastolic function, IVRT showed a negative relationship with arsenic in the cross-sectional analysis, whereas no significant association with E/A ratio was observed. At follow-up, LV geometry measures remained significantly related to urinary arsenic, although the relationship was attenuated and no significant association was observed between arsenic and incident LVH. Measures of systolic function were not related to arsenic at follow-up. In contrast, mitral E-velocity as a measure of diastolic function was positively associated with arsenic exposure.
Available evidence on the relationship between arsenic exposure and echocardiographic measures of cardiac geometry and function in humans is scarce and limited to populations of children. In Mexican children aged from 3 to 8 years (N=161), estimated lifetime arsenic exposure and total urine arsenic concentration (geometric mean concentration of arsenic in urine 59.0 [range, 5.7–370] μg/L, markedly higher than the levels in the SHFS) were associated with a higher LV mass and a lower systolic function, respectively.25 Although the authors concluded that exposure to arsenic was associated with cardiac measures of size and mass, they also found a positive relationship between urinary arsenic concentrations and systolic and diastolic BP but did not control for BP levels in multivariable regression models.25 Therefore, it remains unclear whether the impact of arsenic exposure on LV measures was independent of BP. Our exposure levels in the SHFS, while higher than in other general US populations,31 are markedly lower than the levels in the study conducted in Mexico25 or other studies in Bangladesh.10 In the SHFS, the cross-sectional association between urinary arsenic concentrations with increase in LV wall thickness and mass was significant after controlling for BP levels. Nevertheless, when the study participants were divided according to BP status, the association remained statistically significant only in individuals with prehypertension or hypertension (defined as BP levels above 120/80 mm Hg). Effect modification of prehypertension or hypertension on the association between arsenic and LV mass index was observed, suggesting that the impact of arsenic on cardiac structure is more pronounced in individuals with adaptive cardiovascular responses to increases in systemic BP.
The heart is responsive to physiological and pathological stimulants. Pressure overload in cardiac chambers due to systemic arterial hypertension is considered the main determinant of LVH.45 However, changes in cardiac form and mass are mediated by complex mechanical, neurohumoral, inflammatory, and oxidative processes that involve all cardiac cell types and ultimately lead to a disproportionate growth of cardiac chambers and altered cardiac functioning.46,47 Numerous potential cardiotoxic effects of arsenic have been described in animal and mechanistic studies. In female mice, chronic low-level arsenite exposure (average total arsenic content in drinking water 103.35 μg/L, administrated over a period of 15 weeks) lead to an increment in LV interventricular septum and LV mass of 19% and 43%, respectively, along with an increase in BP.26 Other rodent models showed extensive damage of cardiomyocytes and impaired cardiac contractility in rats treated with sodium arsenite (sodium arsenite content in drinking water 3500 μg/L, administrated over a period of 4 weeks).27 These alterations were mediated by regulatory proteins involved in calcium homeostasis, a potential target of arsenic toxicity.27 Arsenic has been shown to induce calcium overload and inhibit potassium current in cardiac muscle cells,48 leading to adverse electrophysiological effects and ultimately to apoptosis.49,50 Along with functional changes affecting ion channels, arsenic-related cardiotoxicity might be mediated by oxidative stress51 and reactive oxygen species formation.52 In addition, arsenic-induced apoptosis of cardiomyocytes via alteration of mitochondrial permeability53 and activation of MAP (mitogen-activated protein) kinases54 has been reported.
The potential mechanisms of arsenic-induced toxicity are not limited to cardiac muscle cells. In animal models, arsenic promoted collagen production and TGF (transforming growth factor)-β1 expression, resulting in fibrosis of cardiac tissue and subsequently in an increase in cardiac mass.27,55 Moreover, arsenic has been related to endothelial dysfunction via reactive oxygen species formation and accumulation in vascular smooth muscle cells, lipid peroxidation, and loss of vasodilators in numerous studies.56 In view of all potential mechanisms of arsenic-induced cardiotoxicity, it is biologically plausible that arsenic might exert adverse effects on cardiac structure and mass independent of traditional risk factors.
In the present study, the cross-sectional association between arsenic exposure with cardiac systolic functioning showed a positive relationship for stroke volume and ejection fraction. The main determinants of stroke volume and ejection fraction are preload, after-load, and cardiac contractility.57 Early adaptive mechanisms to volume or pressure overload in the heart are not limited to structural growth but include functional systemic compensations including the activation of sympathetic or renin-angiotensin-aldosterone systems to reduce LV wall stress and preserve mechanical function.58 These compensatory mechanisms have a direct impact on preload, afterload, and contractility and can initially lead to an increase in stroke volume, as well as determine measures of LV diastolic function, including IVRT and mitral E-velocity.59 Arsenic exposure can be directly related to hypertension via endothelial dysfunction, oxidative stress, and inflammatory activity, among other mechanisms that are not fully understood.60 In fact, a positive association between arsenic and systolic BP at baseline was found in sensitivity analysis of the present study.
Interestingly, we found no significant relationship between arsenic and incident cases of LVH in the present study. The number of incident cases of LVH during the follow-up (23 of the baseline prehypertensive or hypertensive participants and 5 participants with normal BP at baseline) was small. The study is likely underpowered to answer the question whether a relationship between arsenic exposure and incident LVH exists. In addition, a negative annual change in mean LV mass index and stroke volume was observed when the upper versus the lower quartile of urinary arsenic concentration was compared, whereas the means of mitral E-velocity, deceleration time, and IVRT showed a positive annual change. These findings do not necessarily reflect that the relationship between arsenic exposure and measures of LV geometry and function is inverse in prospective analysis as compared to the findings from cross-sectional analysis. For example, LV mass index and LV posterior wall thickness were lower at follow-up than at baseline in the study population. Despite the negative annual change in mean values, the differences in LV mass index or LV posterior wall thickness at baseline and follow-up were similar comparing the upper versus the lower quartile of urinary arsenic concentration (Figure 1). Urinary arsenic concentrations were available at baseline, but not at follow-up; therefore, the potential impact of changes in arsenic exposure during follow-up in the study outcomes could not be controlled for.
The present study has to be considered with its strengths and limitations. The study was performed in participants of the SHFS, a well-established cohort of American Indians with high cardiovascular risk.40 However, only subjects ≤50 years old with a relatively low burden of cardiovascular risk factors were included. Individuals with cardiovascular disease or diabetes mellitus at baseline were excluded, as both history of cardiovascular events and diabetes mellitus have shown to exert direct impact on cardiac measures performed by TTE.61,62 The prevalence of hypertension and chronic kidney disease, established risk factors for LVH, were relatively low in the investigated cohort (14.4% and 7.9%, respectively).63 Moreover, BP and eGFR were controlled for in regression models, and sensitivity and interaction analyses were performed for each cardiac measure. Stratification according to BP status is important to gain insight into the cardiovascular risk profile of hypertensive patients, which is directly related to arsenic exposure.64 However, the rates of overweight and obesity, conditions independently related to cardiac growth,65 were high (27.9% and 46.3%, respectively); nevertheless, interaction analysis showed no effect modification by BMI status. Circadian variation of BP levels, as well as changes in BP treatment and compliance, could have an impact on measures of cardiac geometry but were not available for the present study. The number of comparisons was relatively large. Due to the elevated number of interrelated outcomes (a total of 16), Bonferroni correction would be inappropriate. Several associations, however, passed the Bonferroni significance level (0.05/16=0.0031). In addition to arsenic exposure, the relationship between arsenic metabolism, which is based on the relative percentage of each of the species over their sum (iAs%, methylarsonate%, and dimethylarsinate%), and measures of cardiac geometry and functioning was investigated but largely show no significant associations. One major limitation of the present study is that measures of urinary arsenic were available at baseline but not at follow-up. Additional resources are needed to measure urinary arsenic at follow-up visits to account for changes in urinary arsenic over time in the statistical analysis and assess the short-term versus long-term impacts of arsenic exposure on cardiac geometry and function. Cross-sectional analyses are generally not free from reverse causation. The interpretation of magnitude and direction of association of OR with large CIs which span the null value has limited value due to the low precision level.
In conclusion, arsenic exposure expressed as the sum of inorganic and methylated arsenic species in urine was related to an increase in LV wall thickness and LVH in young adult American Indians with a low burden of cardiovascular risk factors. The relationship was predominantly found in participants with prehypertension or hypertension, suggesting that possible cardiotoxic effects of arsenic might be more pronounced in individuals already undergoing cardiovascular adaptive mechanisms following elevated systemic BP. Stroke volume as a measure of systolic function as well as isolated measures of diastolic function, including IVRT and mitral E-velocity, were cross-sectionally associated with arsenic exposure, which might reflect the impact of arsenic on both vascular hemodynamics and cardiac structure. In prospective analysis, the relationship of arsenic exposure with changes in cardiac measures was attenuated but remained significant. Although reported findings provide insights to the association between arsenic exposure with LV geometry and functioning, further research is needed to elucidate the causal pathways underlying this relationship and whether these associations are reversible after arsenic exposure is removed from drinking water.
Supplementary Material
CLINICAL PERSPECTIVE.
Arsenic has been related to cardiovascular outcomes and hypertension-induced target organ damage in numerous cross-sectional and prospective studies. The mechanistic pathways that explain this excess in cardiovascular risk are not fully understood. We aimed to investigate the importance of cardiac function and geometry as a relevant pathway, and we focused our research on young adults to assess the relevance of arsenic exposure in affecting the cardiovascular system before the occurrence of clinical disease. The study was conducted in participants from the SHS (Strong Heart Study), designed to investigate cardiovascular disease and its risk factors in American Indian communities. We found that arsenic exposure expressed as the sum of inorganic and methylated arsenic species in urine was related to left ventricular wall thickness and hypertrophy. This association was predominantly found in individuals with elevated blood pressure. Our findings suggest that individuals in a preclinical cardiovascular disease state might be prone to undergo cardiotoxic effects of arsenic. Low exposure to arsenic is widespread; consequently, our results may have implications for the prevention and control of cardiovascular disease in general populations.
Sources of Funding
This study was supported by the National Institute of Health Sciences (R01ES021367, R01ES025216, P42ES010349, P30ES009089), and by the National Heart, Lung, and Blood Institute (cooperative agreements grants U01-HL41642, U01-HL41652, U01-HL41654, U01-HL65520, U01-HL65521 and research grants R01-HL109315, R01-HL109301,R01-HL109284, R01-HL109282 and R01-HL109319 and R01-HL090863).
Footnotes
Disclosures
None.
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCIMAGING.119.009018.
REFERENCES
- 1.Hughes MF, Beck BD, Chen Y, Lewis AS, Thomas DJ. Arsenic exposure and toxicology: a historical perspective. Toxicol Sci. 2011;123:305–332. doi: 10.1093/toxsci/kfr184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang YK, Tseng CH, Huang YL, Yang MH, Chen CJ, Hsueh YM. Arsenic methylation capability and hypertension risk in subjects living in arseniasis-hyperendemic areas in southwestern Taiwan. Toxicol Appl Pharmacol. 2007;218:135–142. doi: 10.1016/j.taap.2006.10.022 [DOI] [PubMed] [Google Scholar]
- 3.Navas-Acien A, Silbergeld EK, Pastor-Barriuso R, Guallar E. Arsenic exposure and prevalence of type 2 diabetes in US adults. JAMA. 2008;300:814–822. doi: 10.1001/jama.300.7.814 [DOI] [PubMed] [Google Scholar]
- 4.Maull EA, Ahsan H, Edwards J, Longnecker MP, Navas-Acien A, Pi J, Silbergeld EK, Styblo M, Tseng CH, Thayer KA, Loomis D. Evaluation of the association between arsenic and diabetes: a National Toxicology Program workshop review. Environ Health Perspect. 2012;120:1658–1670. doi: 10.1289/ehp.1104579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang YL, Hsueh YM, Huang YK, Yip PK, Yang MH, Chen CJ. Uri-nary arsenic methylation capability and carotid atherosclerosis risk in subjects living in arsenicosis-hyperendemic areas in southwestern Taiwan. Sci Total Environ. 2009;407:2608–2614. doi: 10.1016/j.scitotenv.2008.12.061 [DOI] [PubMed] [Google Scholar]
- 6.Tseng CH, Huang YK, Huang YL, Chung CJ, Yang MH, Chen CJ, Hsueh YM. Arsenic exposure, urinary arsenic speciation, and peripheral vascular disease in blackfoot disease-hyperendemic villages in Taiwan. Toxicol Appl Pharmacol. 2005;206:299–308. doi: 10.1016/j.taap.2004.11.022 [DOI] [PubMed] [Google Scholar]
- 7.Newman JD, Navas-Acien A, Kuo CC, Guallar E, Howard BV, Fabsitz RR, Devereux RB, Umans JG, Francesconi KA, Goessler W, Best LT, Tellez-Plaza M. Peripheral arterial disease and its association with arsenic exposure and metabolism in the strong heart study. Am J Epidemiol. 2016;184:806–817. doi: 10.1093/aje/kww002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moon KA, Guallar E, Umans JG, Devereux RB, Best LG, Francesconi KA, Goessler W, Pollak J, Silbergeld EK, Howard BV, Navas-Acien A. Association between exposure to low to moderate arsenic levels and incident cardiovascular disease. A prospective cohort study. Ann Intern Med. 2013; 159:649–659. doi: 10.7326/0003-4819-159-10-201311190-00719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chowdhury R, Ramond A, O’Keeffe LM, Shahzad S, Kunutsor SK, Muka T, Gregson J, Willeit P, Warnakula S, Khan H, Chowdhury S, Gobin R, Franco OH, Di Angelantonio E. Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2018;362:k3310. doi: 10.1136/bmj.k3310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Graziano JH, Parvez F, Liu M, Slavkovich V, Kalra T, Argos M, Islam T, Ahmed A, Rakibuz-Zaman M, Hasan R, Sarwar G, Levy D, van Geen A, Ahsan H. Arsenic exposure from drinking water and mortality from cardiovascular disease in Bangladesh: prospective cohort study. BMJ. 2011;342:d2431. doi: 10.1136/bmj.d2431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tseng CH, Chong CK, Tseng CP, Hsueh YM, Chiou HY, Tseng CC, Chen CJ. Long-term arsenic exposure and ischemic heart disease in arseniasis-hyperendemic villages in Taiwan. Toxicol Lett. 2003;137:15–21. [DOI] [PubMed] [Google Scholar]
- 12.Hsueh YM, Wu WL, Huang YL, Chiou HY, Tseng CH, Chen CJ. Low serum carotene level and increased risk of ischemic heart disease related to long-term arsenic exposure. Atherosclerosis. 1998;141:249–257. [DOI] [PubMed] [Google Scholar]
- 13.Abhyankar LN, Jones MR, Guallar E, Navas-Acien A. Arsenic exposure and hypertension: a systematic review. Environ Health Perspect. 2012; 120:494–500. doi: 10.1289/ehp.1103988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sung TC, Huang JW, Guo HR. Association between arsenic exposure and diabetes: a meta-analysis. Biomed Res Int. 2015;2015:368087. doi: 10.1155/2015/368087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, Gottdiener J, Haluska B, Ofili E, Segers P, Senior R, Tapp RJ, Zamorano JL. recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015;28:727–754. doi: 10.1016/j.echo.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 16.Lauer MS, Evans JC, Levy D. Prognostic implications of subclinical left ventricular dilatation and systolic dysfunction in men free of overt cardiovascular disease (the Framingham Heart Study). Am J Cardiol. 1992; 70:1180–1184. [DOI] [PubMed] [Google Scholar]
- 17.Niemeijer MN, Leening MJ, van den Berg ME, Hofman A, Franco OH, Deckers JW, Rijnbeek PR, Stricker BH, Eijgelsheim M. Subclinical abnormalities in echocardiographic parameters and risk of sudden cardiac death in a general population: the rotterdam study. J Card Fail. 2016;22:17–23. doi: 10.1016/j.cardfail.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 18.Wang TJ, Evans JC, Benjamin EJ, Levy D, LeRoy EC, Vasan RS. Natural history of asymptomatic left ventricular systolic dysfunction in the community. Circulation. 2003;108:977–982. doi: 10.1161/01.CIR.0000085166.44904.79 [DOI] [PubMed] [Google Scholar]
- 19.Feinstein SB, Voci P, Pizzuto F. Noninvasive surrogate markers of atherosclerosis. Am J Cardiol. 2002;89(5A):31C–43C; discussion 43C. [DOI] [PubMed] [Google Scholar]
- 20.Anand IS, Florea VG, Fisher L. Surrogate end points in heart failure. J Am Coll Cardiol. 2002;39:1414–1421. [DOI] [PubMed] [Google Scholar]
- 21.SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 1992;327:685–691. [DOI] [PubMed] [Google Scholar]
- 22.Klapholz M Beta-blocker use for the stages of heart failure. Mayo Clin Proc. 2009;84:718–729. doi: 10.4065/84.8.718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rode-heffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. [DOI] [PubMed] [Google Scholar]
- 24.Wu F, Molinaro P, Chen Y. Arsenic exposure and subclinical endpoints of cardiovascular diseases. Curr Environ Health Rep. 2014;1:148–162. doi: 10.1007/s40572-014-0011-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osorio-Yáñez C, Ayllon-Vergara JC, Arreola-Mendoza L, Aguilar-Madrid G, Hernández-Castellanos E, Sánchez-Peña LC, Del Razo LM. Blood pressure, left ventricular geometry, and systolic function in children exposed to inorganic arsenic. Environ Health Perspect. 2015;123:629–635. doi: 10.1289/ehp.1307327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sanchez-Soria P, Broka D, Monks SL, Camenisch TD. Chronic low-level arsenite exposure through drinking water increases blood pressure and promotes concentric left ventricular hypertrophy in female mice. Toxicol Pathol. 2012;40:504–512. doi: 10.1177/0192623311432297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phan NN, Wang CY, Lin YC. The novel regulations of MEF2A, CAMKK2, CALM3, and TNNI3 in ventricular hypertrophy induced by arsenic exposure in rats. Toxicology. 2014;324:123–135. doi: 10.1016/j.tox.2014.07.010 [DOI] [PubMed] [Google Scholar]
- 28.Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, Cucchiara AJ, Savage PJ, Howard BV. The strong heart study. a study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol. 1990;132:1141–1155. [DOI] [PubMed] [Google Scholar]
- 29.Navas-Acien A, Sharrett AR, Silbergeld EK, Schwartz BS, Nachman KE, Burke TA, Guallar E. Arsenic exposure and cardiovascular disease: a systematic review of the epidemiologic evidence. Am J Epidemiol. 2005;162:1037–1049. doi: 10.1093/aje/kwi330 [DOI] [PubMed] [Google Scholar]
- 30.Navas-Acien A, Umans JG, Howard BV, Goessler W, Francesconi KA, Crainiceanu CM, Silbergeld EK, Guallar E. Urine arsenic concentrations and species excretion patterns in American Indian communities over a 10-year period: the Strong Heart Study. Environ Health Perspect. 2009;117:1428–1433. doi: 10.1289/ehp.0800509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pang Y, Peng RD, Jones MR, Francesconi KA, Goessler W, Howard BV, Umans JG, Best LG, Guallar E, Post WS, Kaufman JD, Vaidya D, Navas-Acien A. Metal mixtures in urban and rural populations in the US: The Multi-Ethnic Study of Atherosclerosis and the Strong Heart Study. Environ Res. 2016;147:356–364. doi: 10.1016/j.envres.2016.02.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Research Council; Division on Earth and Life Studies; Board on Environmental Studies and Toxicology; Committee on Inorganic Arsenic. Critical Aspects of EPA’s IRIS Assessment of Inorganic Arsenic: Interim Report. https://www.nap.edu/read/18594/chapter/1. Accessed September 17, 2018. [Google Scholar]
- 33.Devereux RB, Roman MJ, de Simone G, O’Grady MJ, Paranicas M, Yeh JL, Fabsitz RR, Howard BV. Relations of left ventricular mass to demographic and hemodynamic variables in American Indians: the Strong Heart Study. Circulation. 1997;96:1416–1423. [DOI] [PubMed] [Google Scholar]
- 34.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–367. [DOI] [PubMed] [Google Scholar]
- 35.Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. [DOI] [PubMed] [Google Scholar]
- 36.de Simone G, Kizer JR, Chinali M, Roman MJ, Bella JN, Best LG, Lee ET, Devereux RB; Strong Heart Study Investigators. Normalization for body size and population-attributable risk of left ventricular hypertrophy: the Strong Heart Study. Am J Hypertens. 2005;18(2 pt 1):191–196. doi: 10.1016/j.amjhyper.2004.08.032 [DOI] [PubMed] [Google Scholar]
- 37.Devereux RB, Roman MJ, Palmieri V, Liu JE, Lee ET, Best LG, Fabsitz RR, Rodeheffer RJ, Howard BV. Prognostic implications of ejection fraction from linear echocardiographic dimensions: the Strong Heart Study. Am Heart J. 2003;146:527–534. doi: 10.1016/S0002-8703(03)00229-1 [DOI] [PubMed] [Google Scholar]
- 38.Devereux RB, Roman MJ, Paranicas M, O’Grady MJ, Wood EA, Howard BV, Welty TK, Lee ET, Fabsitz RR. Relations of Doppler stroke volume and its components to left ventricular stroke volume in normotensive and hypertensive American Indians: the Strong Heart Study. Am J Hypertens. 1997;10:619–628. [DOI] [PubMed] [Google Scholar]
- 39.Yurgalevitch SM, Kriska AM, Welty TK, Go O, Robbins DC, Howard BV. Physical activity and lipids and lipoproteins in American Indians ages 45–74. Med Sci Sports Exerc. 1998;30:543–549. [DOI] [PubMed] [Google Scholar]
- 40.North KE, Howard BV, Welty TK, Best LG, Lee ET, Yeh JL, Fabsitz RR, Roman MJ, MacCluer JW. Genetic and environmental contributions to cardiovascular disease risk in American Indians: the strong heart family study. Am J Epidemiol. 2003;157:303–314. [DOI] [PubMed] [Google Scholar]
- 41.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zheng LY, Umans JG, Yeh F, Francesconi KA, Goessler W, Silbergeld EK, Bandeen-Roche K, Guallar E, Howard BV, Weaver VM, Navas-Acien A. The association of urine arsenic with prevalent and incident chronic kidney disease: evidence from the Strong Heart Study. Epidemiology. 2015;26:601–612. doi: 10.1097/EDE.0000000000000313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nigra AE, Howard BV, Umans JG, Best L, Francesconi KA, Goessler W, Devereux R, Navas-Acien A. Urinary tungsten and incident cardiovascular disease in the Strong Heart Study: an interaction with urinary molybdenum. Environ Res. 2018;166:444–451. doi: 10.1016/j.envres.2018.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nigra AE, Ruiz-Hernandez A, Redon J, Navas-Acien A, Tellez-Plaza M. Environmental metals and cardiovascular disease in adults: a systematic review beyond lead and cadmium. Curr Environ Health Rep. 2016;3:416–433. doi: 10.1007/s40572-016-0117-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nadruz W, Shah AM, Solomon SD. Diastolic dysfunction and hypertension. Med Clin North Am. 2017;101:7–17. doi: 10.1016/j.mcna.2016.08.013 [DOI] [PubMed] [Google Scholar]
- 46.Lazzeroni D, Rimoldi O, Camici PG. From left ventricular hypertrophy to dys-function and failure. Circ J. 2016;80:555–564. doi: 10.1253/circj.CJ-16-0062 [DOI] [PubMed] [Google Scholar]
- 47.Moreno MU, Eiros R, Gavira JJ, Gallego C, González A, Ravassa S, López B, Beaumont J, San José G, Díez J. The hypertensive myocardium: from microscopic lesions to clinical complications and outcomes. Med Clin North Am. 2017;101:43–52. doi: 10.1016/j.mcna.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 48.Chen X, Shan H, Zhao J, Hong Y, Bai Y, Sun I, Pan Z, Zhang Y, Yang B, Du Z. L-type calcium current (ICa,L) and inward rectifier potassium current (IK1) are involved in QT prolongation induced by arsenic trioxide in rat. Cell Physiol Biochem. 2010;26:967–974. doi: 10.1159/000324005 [DOI] [PubMed] [Google Scholar]
- 49.Raghu KG, Cherian OL. Characterization of cytotoxicity induced by arsenic trioxide (a potent anti-APL drug) in rat cardiac myocytes. J Trace Elem Med Biol. 2009;23:61–68. doi: 10.1016/j.jtemb.2008.10.001 [DOI] [PubMed] [Google Scholar]
- 50.Bernardi P, Rasola A. Calcium and cell death: the mitochondrial connection. Subcell Biochem. 2007;45:481–506. [DOI] [PubMed] [Google Scholar]
- 51.Muthumani M, Prabu SM. Silibinin potentially attenuates arsenic-induced oxidative stress mediated cardiotoxicity and dyslipidemia in rats. Cardiovasc Toxicol. 2014;14:83–97. doi: 10.1007/s12012-013-9227-x [DOI] [PubMed] [Google Scholar]
- 52.Zhao X, Feng T, Chen H, Shan H, Zhang Y, Lu Y, Yang B. Arsenic trioxide-induced apoptosis in H9c2 cardiomyocytes: implications in cardiotoxicity. Basic Clin Pharmacol Toxicol. 2008;102:419–425. doi: 10.1111/j.1742-7843.2007.00150.x [DOI] [PubMed] [Google Scholar]
- 53.Larochette N, Decaudin D, Jacotot E, Brenner C, Marzo I, Susin SA, Zamzami N, Xie Z, Reed J, Kroemer G. Arsenite induces apoptosis via a direct effect on the mitochondrial permeability transition pore. Exp Cell Res. 1999;249:413–421. doi: 10.1006/excr.1999.4519 [DOI] [PubMed] [Google Scholar]
- 54.Ghosh J, Das J, Manna P, Sil PC. Taurine prevents arsenic-induced cardiac oxidative stress and apoptotic damage: role of NF-kappa B, p38 and JNK MAPK pathway. Toxicol Appl Pharmacol. 2009;240:73–87. doi: 10.1016/j.taap.2009.07.008 [DOI] [PubMed] [Google Scholar]
- 55.Chu W, Li C, Qu X, Zhao D, Wang X, Yu X, Cai F, Liang H, Zhang Y, Zhao X, Li B, Qiao G, Dong D, Lu Y, Du Z, Yang B. Arsenic-induced interstitial myocardial fibrosis reveals a new insight into drug-induced long QT syndrome. Cardiovasc Res. 2012;96:90–98. doi: 10.1093/cvr/cvs230 [DOI] [PubMed] [Google Scholar]
- 56.Ellinsworth DC. Arsenic, reactive oxygen, and endothelial dysfunction. J Pharmacol Exp Ther. 2015;353:458–464. doi: 10.1124/jpet.115.223289 [DOI] [PubMed] [Google Scholar]
- 57.Vincent JL. Understanding cardiac output. Crit Care. 2008;12:174. doi: 10.1186/cc6975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dávila DF, Donis JH, Odreman R, Gonzalez M, Landaeta A. Patterns of left ventricular hypertrophy in essential hypertension: should echocardiography guide the pharmacological treatment? Int J Cardiol. 2008;124:134–138. doi: 10.1016/j.ijcard.2007.01.089 [DOI] [PubMed] [Google Scholar]
- 59.Lovic D, Narayan P, Pittaras A, Faselis C, Doumas M, Kokkinos P. Left ventricular hypertrophy in athletes and hypertensive patients. J Clin Hypertens (Greenwich). 2017;19:413–417. doi: 10.1111/jch.12977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jones MR, Tellez-Plaza M, Sharrett AR, Guallar E, Navas-Acien A. Urine arsenic and hypertension in US adults: the 2003–2008 National Health and Nutrition Examination Survey. Epidemiology. 2011;22:153–161. doi: 10.1097/EDE.0b013e318207fdf2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karas MG, Devereux RB, Wiebers DO, Whisnant JP, Best LG, Lee ET, Howard BV, Roman MJ, Umans JG, Kizer JR. Incremental value of biochemical and echocardiographic measures in prediction of ischemic stroke: the Strong Heart Study. Stroke. 2012;43:720–726. doi: 10.1161/STROKEAHA.111.631168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Marco M, de Simone G, Roman MJ, Chinali M, Lee ET, Calhoun D, Howard BV, Devereux RB. Cardiac geometry and function in diabetic or prediabetic adolescents and young adults: the Strong Heart Study. Diabetes Care. 2011;34:2300–2305. doi: 10.2337/dc11-0191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Paoletti E, De Nicola L, Gabbai FB, Chiodini P, Ravera M, Pieracci L, Marre S, Cassottana P, Lucà S, Vettoretti S, Borrelli S, Conte G, Minutolo R. As sociations of left ventricular hypertrophy and geometry with adverse outcomes in Patients with CKD and hypertension. Clin J Am Soc Nephrol. 2016;11:271–279. doi: 10.2215/CJN.06980615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nong Q, Zhang Y, Guallar E, Zhong Q. Arsenic exposure and predicted 10-year atherosclerotic cardiovascular risk using the pooled cohort Equations in U.S. hypertensive adults. Int J Environ Res Public Health. 2016;13:E1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Simone G, Pasanisi F, Ferrara AL, Roman MJ, Lee ET, Contaldo F, Howard BV, Devereux RB. Relative fat-free mass deficiency and left ventricular adaptation to obesity: the Strong Heart Study. Int J Cardiol. 2013;168:729–733. doi: 10.1016/j.ijcard.2012.09.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.