Highlights
-
•
A good first and overall impression is key to vaccine uptake.
-
•
GP recommendation increases the likelihood of HPV vaccination.
-
•
Mothers with a higher educational level are likely to accept HPV vaccination.
-
•
Fathers taking part in the decision increases the likelihood of HPV vaccination.
-
•
Valuing news and media stories decreases the likelihood of HPV vaccination.
Keywords: Human papillomavirus vaccines, Vaccination coverage, Information, Acceptance, Decision-making, Parents
Abstract
Background
Vaccination against human papillomavirus (HPV) has been part of the Danish Childhood Vaccination Programme (CVP) since 2009 and initially had a high uptake. Following an intense public debate on the alleged side-effects to the vaccine in 2015, coverage rates declined dramatically leaving the current coverage at 54%.
The main aim of this study was to identify differences in the sources of information and factors of importance in mothers’ decision to have or not to have their adolescent daughters vaccinated against HPV.
Methods
This cross-sectional study was based on survey and register data from 3,558 mothers of daughters born in 2003 living in the Central Denmark Region. The survey examined, among others, sources of information and factors of value in the decision-making process. Socioeconomic register data were retrieved from Statistics Denmark.
Pearson's chi-squared test was used to determine differences in socioeconomic distribution between both respondents and non-respondents, and mothers who had their daughters vaccinated versus those who did not. Associations between vaccination status and various events were estimated using logistic regression.
Results
A strong association was found between vaccine uptake and general practitioner (GP) recommendation (odds ratio (OR) 0.17, 95% confidence interval (CI) 0.10; 0.30), seeking GP guidance (OR 0.63, 95% CI 0.50; 0.78) and agreeing with the daughter’s father to vaccinate (OR 0.60, 95% CI 0.37; 0.96). Inversely, vaccination decline was associated with a negative first impression of HPV vaccination (OR 4.05, 95% CI 3.28; 5.00), valuing media stories (OR 3.57, 95% CI 2.63; 4.85) and distrusting the first source of information (OR 2.49, 95% CI 1.92; 3.23).
Conclusions
The results indicate that the impression left behind by information sources is more important in determining vaccination status than the information sources themselves, indicating that mothers are liable to make healthcare decisions based on sensibility rather than sense.
1. Introduction
Despite the fact that population-based cervical cancer screening is implemented in close to all European Union (EU) member states [1], each year more than 33,000 women in the EU are diagnosed with cervical cancer and approximately 14,000 die annually of the disease [2]. Infection with human papillomavirus (HPV) is a prerequisite to the development of precancerous lesions. HPV types 16 and 18 are the most carcinogenic [3], causing 70% of all cervical cancer cases [4]; thus, vaccination may protect against the development of cervical cancer. The first vaccine against HPV was authorised for European marketing in 2006 [5]. It was tested thoroughly for both efficacy and safety [3], [6], [7] and as of 2018, all EU member states recommend HPV-vaccination [8].
HPV-vaccination coverage rates vary across the EU; in Scandinavia, HPV vaccination coverage among adolescent girls is generally high with coverage rates ranging from 70.1% in Finland [9] to 81.1% in Norway [10]. At its introduction into the Danish Childhood Vaccination Programme (CVP) in 2009, HPV vaccination coverage rates were close to 93% for initial HPV vaccination [11], [12]. The rates initially fell in 2013, but a significant drop was seen in early 2015. This decline is attributed mainly [13] to an intense public debate following a public service-funded documentary [14] on girls suffering from alleged side-effects. During 2015, the Danish Medicines Agency received almost 150% more claims of serious adverse side-effects to HPV vaccination than in the previous six years combined [15], [16], even though the fear of side-effects was unfounded according to scientific literature. Currently, in Denmark the HPV vaccination coverage rate for adolescent girls is 54%; the coverage rate for the remaining CVP is 88% [11]. Thus, a major divide between opting out of HPV-vaccination and the rest of the CVP still exists.
Internationally, aside from efficacy and safety concerns, barriers towards HPV vaccination [17] have been cost, practicality issues, lack of trust in healthcare providers and authorities, and social norms [17], [18], [19], [20], [21]. Many of these factors depend on information sources, and while this has been previously explored in the general population [22], it has been previously underexplored in mothers, which is of interest as they are often the primary health care decision makers in families [23], [24], [25].
The primary aim of this study was to identify any differences in the sources of information and factors of value during decision-making among mothers who have not had their adolescent daughters vaccinated against HPV compared with mothers who have had their daughters vaccinated. A secondary aim was to analyse if there were any socioeconomic predictors of mothers not having their daughters vaccinated against HPV.
2. Methods
2.1. Setting
Denmark has 5.8 million inhabitants divided into five geographical and administrative regions [26]. The study was conducted in the Central Denmark Region, which comprises more than 1.3 million residents living in both rural and urban areas, and contains Denmark's second largest city, Aarhus (340,000 inhabitants)[26].
HPV vaccination was introduced in Denmark in 2006 [27] and became part of the free-of-charge CVP on 1 January 2009 for girls born in 1996 and later with time-limited catch-up offers to girls born in the 1985–1995 period [28]. The CVP is managed by the family's general practitioner (GP). All Danish citizens have access to tax-funded universal healthcare.
2.2. Study design
This study was conducted as a cross-sectional study using survey and register data.
2.3. Study population
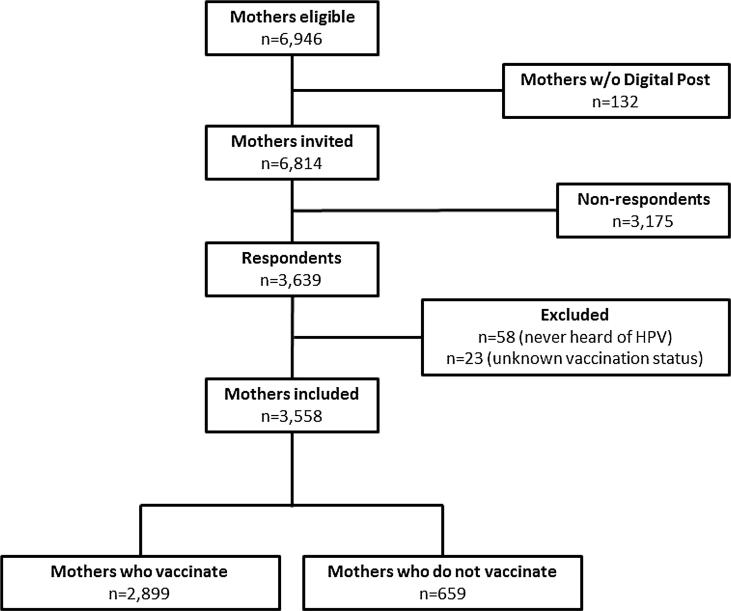
As mothers are considered the primary healthcare decision-makers in families [23], [24], [25], the study population was defined as mothers of daughters born in 2003 who were residents of the Central Denmark Region throughout the period from 1 January 2015 to 31 December 2016 to ensure that all girls had reached their 13th year of life within the study period. Inclusion into this study was performed irrespective of the girl’s vaccination status. Mothers of twins or multiple daughters born in 2003 participated as one entry. Mothers exempted from Digital Post were excluded from the study along with mothers who did not report vaccination status or who had never heard of HPV vaccination (Fig. 1). An incomplete survey response was not in itself an exclusion criterion.
Fig. 1.
Study Inclusion Flowchart.
2.4. Register data
Participants were identified through the Danish Civil Registration System (CRS) [29]. All Danish citizens are registered in the CRS with a unique 10-digit number (CPR-number), which enables individual level data linkage between registries.
Data on socioeconomic variables (educational level, annual income, occupation, ethnicity, civil status and municipal residence) and the mothers’ birthdays were obtained through Statistics Denmark's population-based databases. All socioeconomic variables were from late 2016, estimating socioeconomic status at the approximate time of decision-making.
Mothers' birthdays were used to generate their age at the end of 2003, estimating age at parturition. Disposable household income was assessed using Organisation for Economic Cooperation and Development (OECD)-modified equivalence scales [30], then categorised based on the distribution of the data into tertiles and rounded off to the nearest $100, generating the categories low (<$31,000), middle (≥$31,000–47,000) and high (≥$47,000). Area of residence was defined as (1) Densely populated area: at least 50% of the population lives in urban centres), (2) Intermediate density area: less than 50% of the population lives in rural grid cells and less than 50% of the population lives in urban centres), (3) Thinly populated area: more than 50% of the population lives in rural grid cells, according to EUROSTAT's variable DEGURBA (DEGree of URBAnisation) [31], [32]. Employing definitions used by Statistics Denmark, ethnicity was defined as Danish, Western (EU, Andorra, Australia, Canada, Iceland, Liechtenstein, Monaco, New Zealand, Norway, San Marino, Switzerland and the USA) or Non-Western (others). Marital status was categorised as married/registered partnership, cohabitating or single. Mother’s highest attained education was categorised according to the UNESCO's International Standard Classification of Education version 2011 [33] as primary education (primary and lower secondary), secondary education (upper secondary), bachelors' or vocational, or higher academic education (masters, doctoral or further degree). Occupation was grouped into self-employed/chief executive positions, employed, receiving benefits (early retirement, unemployment benefit, education grants, social security and sickness benefits) and others. Unavailable socioeconomic variables were labelled as missing.
2.5. Survey data
2.5.1. Survey development and pilot testing
A survey in Danish based on a literature review was developed by the research team. The survey was pilot tested among a convenience sample of 15 consenting mothers of daughters eligible for HPV vaccination who did not form part of the study. Subsequently, they underwent a semi-structured telephone interview individually in order to illuminate areas to improve and include any questions and answers not anticipated following the preliminary literature review.
2.5.2. Survey content
The survey consisted of eight main questions with 37 sub-questions. All respondents were to answer all main questions regardless of their response to the sub-questions, which differed depending on the answers to the main questions.
Questions sought to examine the mother’s sources of information, from whom and where she sought guidance, which factors the mother valued before deciding upon vaccination, and ultimately whether or not she had her daughter vaccinated at the time of the survey response, regardless of her intention to have her daughter vaccinated at a later time. The response options were either dichotomous ('yes/no', 'positive/negative'), Likert-scaled ('not at all/a little/a good deal/a lot') or categorical with pre-formulated answers (e.g., 'social media (Facebook, Twitter, Instagram)'). Questions with multiple answer permission were specified as such.
One question had Likert-scaled answers; viz. the question exploring if mothers found particular factors of value for her decision. This question was dichotomised as either “yes” (answer options “a little”, “a good deal”, “a lot”) or “no” (answer option “not at all”) before analysis. Questions with multiple answers were dichotomised, and each answer was analysed separately.
2.6. Data collection
Individual electronic links to the survey were sent to all participants through e-Boks in March 2018. Reminders were sent out two weeks later. e-Boks is an online email platform used by the Danish authorities and several private and public companies to contact citizens [34]. All Danish citizens are required to register for a digital signature (nemID) in order to access Digital Post through e-Boks. Exemptions from this requirement include disability (mental or physical), inability to access Digital Post (due to practicality issues or language barriers) and no permanent place of residence in Denmark (e.g., homelessness or permanent emigrant status) [35].
The survey was hosted on the online secure data management tool REDCap (version 7.4.17, © Vanderbilt University) [36], from which data were extrapolated and subsequently linked to register data using CPR-numbers.
2.6.1. Analyses
Pearson's chi-squared test for independence was used to determine differences in socioeconomic distribution between both respondents and non-respondents and between those who accepted and those who declined vaccination. We used univariate logistic regression to assess odds ratios (OR) and 95% confidence intervals (CI), estimating associations between vaccination status and exposure to different variables, including factors of value during decision-making. Vaccination status was thus the independent variable and non-vaccination being the outcome of interest (coded as 1) compared to vaccination (coded 0); therefore, ORs < 1 indicates likelihood of vaccination, whereas ORs > 1 indicates likelihood of non-vaccination. Adjustments were made for all socioeconomic variables using multivariate logistic regression.
All statistical analyses were conducted in Stata/SE 15.1 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
2.6.2. Approval
According to Danish legislation and the Central Denmark Region Committees on Biomedical Research Ethics, the study did not require ethical approval as it was based on register and survey data. The study was approved by the Danish Data Protection Agency (2012-58-0006).
3. Results
A total of 6946 mothers were eligible for inclusion of whom 6814 (98.1%) had access to Digital Post and received an invitation. 3639 (53.4%) mothers replied; of these, 58 (1.6%) had not heard of HPV vaccination and 23 (0.6%) did not report their daughter’s vaccination status. The final study population thus counted 3558 mothers of whom 651 (18.3%) had not had their daughters vaccinated (Fig. 1).
Survey respondents were statistically significantly different to non-respondents in all socioeconomic aspects with respondents more likely being older, more well-educated, of Danish ethnicity, employed, married, earning a higher income and residing in thinly populated areas than non-respondents (Table 1). Among the respondents, mothers who had their daughters vaccinated against HPV were well-educated, employed, married and had a higher income than mothers who did not have their daughters vaccinated, while there were no statistically significant differences in age, ethnicity and residence to mothers who did not have their daughters vaccinated (Table 2).
Table 1.
Indicators of socioeconomic status in the study population.
| Respondents | Non-respondents | Total | ||
|---|---|---|---|---|
| N (%)* | N (%)* | N (%)* | P value** | |
| Total | 3,639 (52.4) | 3,175 (47.6) | 6,814 (1 0 0) | |
| Age at parturition | ||||
| <20 | 13 (0.4) | 35 (1.1) | 48 (0.7) | <0.001 |
| 20–24 | 232 (6.4) | 368 (11.7) | 600 (8.8) | |
| 25–29 | 1176 (32.4) | 1090 (34.5) | 2266 (33.4) | |
| 30–34 | 1471 (40.5) | 1133 (35.9) | 2604 (38.3) | |
| 35–39 | 624 (17.2) | 461 (14.6) | 1085 (16.0) | |
| >40 | 116 (3.2) | 72 (2.3) | 188 (2.8) | |
| Educational level | ||||
| Primary education | 283 (7.8) | 470 (15.2) | 753 (11.2) | <0.001 |
| Secondary education | 1438 (39.8) | 1299 (42.0) | 2737 (40.8) | |
| Bachelor or vocational | 1423 (39.4) | 1041 (33.7) | 2464 (36.8) | |
| Higher academic education | 467 (12.9) | 284 (9.2) | 751 (11.2) | |
| Occupation | ||||
| Self-employed/executive | 217 (6.0) | 203 (6.4) | 420 (6.2) | <0.001 |
| Employed | 2935 (80.7) | 2263 (71.3) | 5198 (76.3) | |
| Receiving benefits | 440 (12.1) | 636 (20.0) | 1076 (51.8) | |
| Others | 47 (1.3) | 73 (2.3) | 120 (1.8) | |
| Annual income | ||||
| Low | 961 (26.4) | 1206 (38.0) | 2167 (31.8) | <0.001 |
| Medium | 1266 (34.8) | 1019 (32.1) | 2285 (33.6) | |
| High | 1411 (38.8) | 948 (29.9) | 2359 (34.6) | |
| Ethnicity | ||||
| Danish | 3411 (93.9) | 2657 (84.1) | 6068 (89.4) | <0.001 |
| Western | 70 (1.9) | 119 (3.8) | 189 (2.8) | |
| Non-Western | 151 (4.2) | 383 (12.1) | 534 (7.9) | |
| Civil status | ||||
| Married | 2629 (72.4) | 2161 (68.4) | 7490 (70.5) | 0.001 |
| Cohabitants | 416 (11.5) | 403 (12.8) | 819 (12.1) | |
| Single | 587 (16.2) | 595 (18.8) | 1182 (17.4) | |
| Residence | ||||
| Densely populated area | 678 (18.7) | 679 (22.1) | 1375 (20.3) | 0.002 |
| Intermediate density area | 1134 (31.2) | 968 (30.6) | 2102 (31.0) | |
| Thinly populated area | 1820 (50.1) | 1494 (47.3) | 3314 (48.8) | |
Numbers do not add up due to missing values.
P-value determined using Pearson's chi-squared test.
Table 2.
Indicators of socioeconomic status in the respondents, stratified by vaccination status.
| Mothers who had their daughters vaccinated | Mothers who did not have their daughters vaccinated | ||
|---|---|---|---|
| N (%)* | N (%)* | P-value** | |
| Total | 2899 (81.48) | 659 (18.52) | |
| Age at parturition | |||
| <20 | 8 (0.3) | 4 (0.6) | 0.08 |
| 20–24 | 160 (5.5) | 52 (7.9) | |
| 25–29 | 955 (33.0) | 206 (31.4) | |
| 30–34 | 1195 (41.3) | 251 (38.2) | |
| 35–39 | 489 (16.9) | 120 (18.3) | |
| >40 | 88 (3.0) | 24 (3.7) | |
| Educational level | |||
| Primary education | 182 (6.3) | 73 (11.2) | <0.001 |
| Secondary education | 1145 (39.7) | 271 (41.4) | |
| Bachelor or vocational | 1177 (40.2) | 231 (35.3) | |
| Higher academic education | 381 (13.2) | 79 (12.1) | |
| Occupation | |||
| Self-employed/executive | 163 (5.6) | 51 (7.7) | <0.001 |
| Employed | 2414 (83.3) | 486 (73.8) | |
| Receiving benefits | 296 (10.2) | 105 (15.9) | |
| Others | 26 (0.9) | 17 (2.6) | |
| Annual income | |||
| Low | 693 (23.9) | 211 (32.0) | <0.001 |
| Medium | 1018 (35.1) | 232 (35.2) | |
| High | 1187 (41.0) | 216 (32.8) | |
| Ethnicity | |||
| Danish | 2,765 (95.5) | 619 (94.2) | 0.37 |
| Western | 51 (1.8) | 15 (2.3) | |
| Non-Western | 79 (2.7) | 23 (3.5) | |
| Civil status | |||
| Married | 2152 (74.3) | 429 (65.3) | <0.001 |
| Cohabitants | 313 (10.8) | 96 (14.6) | |
| Single | 430 (14.9) | 132 (20.1) | |
| Residence | |||
| Densely populated area | 525 (18.1) | 126 (19.2) | 0.55 |
| Intermediate density area | 920 (31.8) | 195 (29.7) | |
| Thinly populated area | 1450 (50.1) | 336 (51.1) | |
Numbers do not add up due to missing values.
P-value determined using Pearson's chi-squared test.
Overall, 32.5% (n = 1157) of respondents reported having first heard about HPV vaccination from news media, whereas substantially fewer reported first having heard of it from social media (n = 31, 0.87%) or their GP (n = 374, 10.5%). A total of 932 mothers (26.2%) could not recall where they had first heard about HPV vaccination. A substantially larger proportion of mothers reported having heard about HPV vaccination from TV programmes (n = 2386, 67.1%), news (n = 2586, 72.2%) and social media (n = 1404, 39.5%) at a later point (Table 3).
Table 3.
The mothers’ sources of information, stratified by vaccination status. Odds ratios (OR) indicate the likelihood of not being vaccinated.
| Mothers who had their daughters vaccinated 2899 | Mothers who did not have their daughters vaccinated 659 | Unadjusted |
Adjusted* |
|||
|---|---|---|---|---|---|---|
| N (%) | N (%) | OR | CI | OR | CI | |
| Where did you first hear about HPV vaccination? | ||||||
| TV programmes & documentaries | 278 (9.6) | 82 (12.4) | 1.34 | 1.03–1.74 | 1.28 | 0.98–1.67 |
| News (TV, radio, newspapers) | 952 (32.8) | 205 (31.1) | 0.92 | 0.77–1.11 | 0.93 | 0.77–1.11 |
| Social media (Facebook etc.) | 21 (0.7) | 10 (1.5) | 2.11 | 0.99–4.51 | 2.15 | 1.00–4.61 |
| Work and social relations | 289 (13.4) | 88 (13.4) | 0.99 | 0.78–1.28 | 1.04 | 0.81–1.33 |
| General practitioner | 314 (10.8) | 60 (9.1) | 0.82 | 0.62–1.10 | 0.73 | 0.54–0.99 |
| Danish Health Authority | 131 (4.5) | 35 (5.3) | 1.19 | 0.81–1.74 | 1.19 | 0.81–1.74 |
| Do not recall | 761 (26.3) | 171 (26.0) | 0.98 | 0.81–1.19 | 1.02 | 0.84–1.24 |
| Other | 53 (1.8) | 8 (1.2) | 0.66 | 0.31–1.39 | 0.75 | 0.35–1.59 |
| Where else have you heard about the HPV vaccine? | ||||||
| TV programmes & documentaries | 1927 (66.5) | 459 (69.7) | 1.16 | 0.96–1.39 | 1.26 | 1.05–1.53 |
| News (TV, radio, newspapers) | 2099 (72.4) | 487 (73.9) | 1.08 | 0.89–1.31 | 1.16 | 0.95–1.42 |
| Social media (Facebook, etc.) | 1111 (38.3) | 293 (44.5) | 1.29 | 1.09–1.53 | 1.34 | 1.13–1.60 |
| Work and social relations | 1920 (66.2) | 430 (65.3) | 0.96 | 0.80–1.14 | 1.04 | 0.87–1.25 |
| General practitioner | 1513 (52.2) | 304 (46.1) | 0.78 | 0.66–0.93 | 0.79 | 0.66–0.93 |
| Danish Health Authority | 827 (28.5) | 212 (32.2) | 1.19 | 0.99–1.43 | 1.29 | 1.07–1.55 |
| Other | 50 (1.7) | 21 (3.2) | 1.38 | 1.08–1.77 | 1.55 | 1.20–2.00 |
| First impression | ||||||
| Positive | 1740 (60.0) | 253 (38.4) | ||||
| Negative | 394 (13.6) | 234 (35.5) | 4.08 | 3.32–5.03 | 4.05 | 3.28–5.00 |
| Missing | 765 (26.4) | 172 (26.1) | ||||
| Overall impression | ||||||
| Positive | 2501 (86.3) | 203 (30.8) | ||||
| Negative | 374 (12.9) | 449 (68.1) | 14.8 | 12.13–18.03 | 14.9 | 12.17–18.16 |
| Missing | 24 (0.8) | 7 (1.1) | ||||
Adjusted for socioeconomic values: age at daughter’s birth, educational level, annual income, occupation, ethnicity, civil status and residence.
Statistically significant differences between the information sources reported by mothers who did and mothers who did not have their daughters vaccinated were found (Table 3). Mothers who had first heard about the vaccine through social media were more likely to decline vaccination than those who had not (OR 2.15, 95% CI 1.00; 4.61), while mothers who had first heard of HPV vaccination from their GP were more likely to vaccinate than those who had not (OR 0.73, 95% CI 0.54; 0.99). Furthermore, there were associations between both a negative first and overall impression and declining vaccination (OR 4.05, 95% CI 3.28; 5.00, and OR 14.9, 95% CI 12.17; 18.16, respectively).
Mothers who were employed/self-employed/executive were more likely to vaccinate compared to mothers outside the labour market (OR 0.66, 95% CI 0.51; 0.84), and mothers who were married/reg. partnership were more likely to vaccinate compared to mothers who were single or cohabitating (OR 0.72, 95% CI 0.60; 0.88) (Table 4).
Table 4.
Likelihood of not vaccinating if exposed to various factors.
| Unadjusted |
Adjusted* |
|||
|---|---|---|---|---|
| Factor | OR | CI | OR | CI |
| Socioeconomic status | ||||
| Age > 35 years | 1.13 | 0.92–1.38 | 1.16 | 0.94–1.43 |
| High educational level | 0.76 | 0.65–0.91 | 0.86 | 0.71–1.02 |
| Employed/self-employed/executive | 0.55 | 0.44–0.69 | 0.66 | 0.51–0.84 |
| High income | 0.70 | 0.59–0.84 | 0.84 | 0.68–1.02 |
| Danish ethnicity | 0.75 | 0.52–1.08 | 0.88 | 0.60–1.30 |
| Married/reg. partnership | 0.65 | 0.54–0.78 | 0.72 | 0.60–0.88 |
| Residence in high density area | 1.04 | 0.88–1.23 | 1.02 | 0.86–1.21 |
| Searched for information on HPV | 1.22 | 0.99–1.51 | 1.33 | 1.07–1.65 |
| Searched through: | ||||
| Internet/Social media | 1.41 | 1.18–1.70 | 1.47 | 1.23–1.77 |
| Social relations | 1.25 | 1.04–1.50 | 1.31 | 1.09–1.57 |
| General practitioner/health official | 0.80 | 0.67–0.94 | 0.85 | 0.71–1.01 |
| Other | 1.66 | 1.33–2.09 | 1.89 | 1.49–2.39 |
| Reasons for searching | ||||
| Wanted to hear the other side of the matter | 1.59 | 1.33–1.89 | 1.68 | 1.40–2.00 |
| Efficacy concerns | 1.38 | 1.16–1.64 | 1.40 | 1.17–1.67 |
| Sought guidance from general practitioner | 0.61 | 0.49–0.76 | 0.63 | 0.50–0.78 |
| Did not trust first information | 2.38 | 1.84–3.07 | 2.49 | 1.92–3.23 |
| Safety concerns (side-effects) | 1.66 | 1.39–1.99 | 1.83 | 1.52–2.19 |
| Contacted by general practitioner | 1.64 | 1.37–1.97 | 1.61 | 1.34–1.94 |
| In person/by telephone | 1.30 | 0.95–1.79 | 1.20 | 0.86–1.66 |
| General practitioner recommended vaccine | 0.19 | 0.11–0.32 | 0.17 | 0.10–0.30 |
| Involved daughter's father in the decision | 0.68 | 0.56–0.82 | 0.78 | 0.63–0.95 |
| Agree on decision | 0.55 | 0.34–0.87 | 0.60 | 0.37–0.96 |
| Involved daughter in decision | 1.23 | 1.04–1.46 | 1.16 | 0.97–1.34 |
| Agree on decision | 0.35 | 0.23–0.54 | 0.34 | 0.22–0.54 |
| Previously opted out of childhood vaccination | 13.7 | 6.42–29.30 | 13.0 | 6.05–27.95 |
| Declined: | ||||
| MMR** | 12.93 | 5.44–30.71 | 12.84 | 5.36–30.75 |
| Tdap-IPV*** | 35.61 | 4.45–285.23 | 37.13 | 4.60–299.54 |
| Hib**** | 22.32 | 4.88–102.10 | 21.06 | 4.57–97.03 |
| Pneumococcal***** | 24.59 | 5.44–111.20 | 22.61 | 4.97–102.96 |
Adjusted for socioeconomic values: age at daughter’s birth, educational level, annual income, occupation, ethnicity, civil status, and residence
MMR = measles, mumps and rubella.
Tdap-IPV = tetanus, diphtheria, polio, pertussis.
Haemophilus influenzae type b.
Pneuomococcal: streptococcus pneumoniae.
Mothers who actively searched for information about HPV vaccination were more likely to decline vaccination, unless they sought guidance from their GP (OR 0.63, 95% CI 0.50; 0.78), than mothers who did not actively search for information. Mothers who sought information due to distrust in their first information source were more likely not to vaccinate than those who sought information not due to distrust (OR 2.49, 95% CI 1.92; 3.23). Mothers who reported being contacted by their GP had a higher likelihood of declining vaccination than those who reported not being contacted by their GP (OR 1.61, 95% CI 1.34; 1.94). However, those who were recommended HPV vaccination by their GP were more likely to accept vaccination than were mothers whose GP had not recommended vaccination (OR 0.17, 95% CI 0.10; 0.30). Mothers who had previously opted out of the CVP had a much higher likelihood of not vaccinating their daughter (OR 13.0, 95% CI 6.05; 27.95) (Table 4).
Mothers who involved their daughter's father in the decision-making were more likely to vaccinate their daughters than mothers who decided single-handedly (OR 0.78, 95% CI 0.63; 0.95), whereas mothers who involved their daughters showed a tendency towards declining vaccination compared to mothers who did not involve their daughters (OR 1.16, 95% CI 0.97; 1.34) (Table 4).
Lastly, mothers who valued their daughter's father's opinion (OR 0.79, 95% CI 0.63; 0.99), information from their GP (OR 0.48, 95% CI 0.39; 0.58) and information from health authorities (OR 0.49, 95% CI 0.39; 0.62) were more likely to accept vaccination, whereas mothers who valued personal knowledge (OR 1.83, 95% CI 1.52; 2.20) and media stories (OR 3.57, 95% CI 2.63; 4.85) of vaccinees with presumed side-effects were more likely to decline vaccination (Table 5).
Table 5.
Odds ratios for not vaccinating if the following factors were of value in the decision-making.
| Unadjusted |
Adjusted* |
|||
|---|---|---|---|---|
| Factor | OR | CI | OR | CI |
| Daughter's opinion of HPV | 1.12 | 0.93–1.35 | 1.07 | 0.88–1.29 |
| Daughter's father's opinion of HPV | 0.67 | 0.55–0.83 | 0.79 | 0.63–0.99 |
| Opinion of family, friends or acquaintances | 1.20 | 1.01–1.43 | 1.20 | 1.01–1.43 |
| Personal knowledge of vaccinees with presumed side-effects | 1.90 | 1.59–2.28 | 1.83 | 1.52–2.20 |
| Personal knowledge of vaccinees without presumed side-effects | 1.00 | 0.83–1.21 | 0.98 | 0.81–1.18 |
| Stories about vaccinees with presumed side-effects (documentaries, social media, etc.) | 3.55 | 2.62–4.79 | 3.57 | 2.63–4.85 |
| Stories about vaccinees without presumed side-effects (documentaries, social media, etc.) | 1.27 | 1.03–1.58 | 1.28 | 1.03–1.58 |
| Information from general practitioner | 0.48 | 0.40–0.59 | 0.48 | 0.39–0.58 |
| Information from health authorities | 0.45 | 0.36–0.57 | 0.49 | 0.39–0.62 |
Adjusted for socioeconomic values: age at daughter’s birth, educational level, annual income, occupation, ethnicity, civil status and residence.
4. Discussion
This survey-based cross-sectional study showed that a less favourable socioeconomic status, a negative first impression of the HPV vaccination, valuing social and news media and distrust in information sources were strongly associated with a higher probability of not vaccinating your daughter. Inversely, factors favourable for accepting vaccination were GP recommendation, valuing information from the GP and health authorities and involving the daughter's father. As these results show, mothers turn to the media in search for information when making healthcare decisions, and mothers who decline vaccination value media stories significantly higher than health authorities compared with mothers who accept vaccination.
The population-based study design was a strength, limiting the risk of selection bias. However, the respondents reported an 81.5% HPV vaccination initiation rate with a completion rate of 64.9%, which is higher than national accounts [11]. A recent Danish study on MMR coverage rates [37] showed that official rates are considerably lower than the true rate, indicating that self-reported survey data on vaccination status may have a higher validity than register data in a study population of this size. Thus, the high coverage found in this study may reflect both selection and information bias. Even though respondents had a more favourable socioeconomic status than non-respondents, indicating some selection bias, the differences between mothers respectfully accepted or declined vaccination are not influenced by this.
Information bias was limited by the register-based approach to socioeconomic factors; nevertheless, since the study was retrospective, the survey results may have been influenced by recall bias. Ideally, survey responses should have been collected at the height of the public debate. Additionally, the invitation letter was ambiguous regarding which daughter the survey was designed for in cases where mothers had daughters from different years, presenting another risk of information bias due to the importance of the timing of the public debate in this area of research. Finally, no information on families with male healthcare decision makers, male-male parenthoods or male single parents was obtained.
Contrary to a previous study [38], this study shows that mothers who involved their daughter's father were much more likely to vaccinate than mothers who did not. Heterosexual men have been shown to have low knowledge of HPV infection [39], but less is known about fathers’ perspectives on HPV vaccination, and further research is needed to identify how fathers respond to information provided by both health authorities and social media. The fact that alleged side-effects can influence vaccine coverage to the extent seen in Denmark is consistent with the paradigm shift seen in the post-factual context of Western society, where the approach to and interpretation of medical evidence is merely perceived as an opinion with which vaccine opposers may choose to disagree [40].
The State Serum Institute, the organisation in charge of disease and vaccine surveillance in Denmark, began sending out reminders to parents of unvaccinated children in 2014 [41]; a practice copied by many general practices. Thus, mothers contacted by their GP were most likely mothers of unvaccinated children, which may account for the conflicting finding that mothers contacted by their GP are more likely not to vaccinate, whereas mothers who search for guidance from their GP are more likely to vaccinate.
This study adds to the evidence that the mother’s decision regarding her daughter’s HPV vaccination is influenced by her beliefs, interaction with both clinicians and family members, and media exposure [42]. Media is rarely transparent, complete or correct when reporting on HPV vaccination [43], which may be attributed to the fact that media reports on health topics are rarely written by science specialists [44]. Laymen consistently testify that they trust health officers and authorities more than the media [19], [44]; yet, positive mass media coverage increases the utilisation of specific health services, whereas negative coverage discourages the use of these services regardless of official recommendations [45]. Furthermore, an increase in media debates has been shown to result in a higher level of information seeking and a higher rate of reported side-effects [46]. Additionally, negatively toned posts on social media regarding vaccination are less likely to be scientifically funded than positively toned posts, enabling like-minded individuals to disseminate rather than debate ideas [47].
Even though mothers primarily get their health information from the media, this study showed no discernible association between difference in information sources and vaccination uptake. Personal factors such as distrust in information sources, and personal relations (exemplified by the importance of GP recommendation, agreeing with the daughter’s father and valuing stories of vaccinees) were more important determinants of vaccination than the information sources themselves, indicating that mothers make healthcare decisions based on their own beliefs rather than on knowledge. Similarly, another study showed that media stories about HPV vaccine harms were especially powerful concerning vaccination decline, while there was little evidence to suggest a positive association between vaccination behaviour and stories about the positive effects of vaccination [22]. Mothers who do not vaccinate are not necessarily less informed than mothers who do; they simply place importance upon different information items based on their own personal values. Since a higher socioeconomic status is associated with a higher level of health literacy [48], socioeconomic differences between mothers may indicate that those who vaccinate are better at sorting through the available information.
The fear of side-effects to HPV vaccination is reminiscent of the MMR controversy 20 years ago, and the MMR legacy still lingers in parents' sub-consciousness when faced with new vaccination decisions [49]. Despite the fact that the producers of the Danish documentary and the broadcast channel have publicly apologised for the wrongful portrayal of the HPV vaccine [50], coverage is still trailing behind. Contemporary media reports of alleged side-effects are therefore not only harmful at the time of publication; they leave a lasting impression causing long-term damage to public health.
5. Conclusions
This study provides evidence that healthcare decision-making is often not a matter of sense but of sensibility, demonstrating that to achieve sufficient coverage and herd immunity, efforts must be made to ensure that mothers facing decision-making can do so on a well-informed and unbiased basis.
6. Abbreviations
CI: confidence interval, CRS: civil registration system, CVP: childhood vaccination programme, EMA: European Medicines Agency, EU: European Union, GP: general practitioner, HPV: human papillomavirus, MMR: measles-mumps-rubella, OR: odds ratio, SoMe: Social media.
Declaration of interests
None.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1.Ponti A, Anttila A, Ronco G, Senore C, Basu P, Sagnan N, et al. Cancer Screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. European Commission for Health and Food Safety May 2017.
- 2.Incidence and mortality 2018 [Internet]. ECIS - European Cancer Information System. European Union. [cited 25/07/2018]. Available from: <https://ecis.jrc.ec.europa.eu/index.php>.
- 3.Muñoz N., Bosch F.X., de Sanjosé S., Herrero R., Castellsagué X., Shah K.V. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348(6):518–527. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 4.Stanley M. Pathology and epidemiology of HPV infection in females. Gynecol Oncol. 2010;117(2 Suppl):S5–S10. doi: 10.1016/j.ygyno.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 5.European Medicines Agency. European public assessment report (EPAR) for Gardasil. Human papillomavirus vaccine [types 6, 11, 16, 18] (recombinant, absorbed). [14/08/2018]. Available from: <http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/000703/WC500021146.pdf>.
- 6.Haupt R.M., Sings H.L. The efficacy and safety of the quadrivalent human papillomavirus 6/11/16/18 vaccine Gardasil. J Adolescent Health: Off Publ Soc Adolescent Med. 2011;49(5):467–475. doi: 10.1016/j.jadohealth.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organisation (WHO). Global Advisory Committee on Vaccine Safety; 2007. Available from: <http://www.who.int/vaccine_safety/committee/reports/June_2007/en/>.
- 8.Human Papillomavirus Infection: Recommended vaccinations: European Centre for Disease Prevention and Control, Vaccine Scheduler Available from: <https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=38&SelectedCountryIdByDisease=-1>.
- 9.Girls' HPV vaccination coverage [Internet]. National Institute for Health and Welfare, Finland. . 2018 [cited 17/08/2018]. Available from: <https://thl.fi/roko/rokotusrekisteri/atlas/atlas-en.html?show=hpv>.
- 10.Norgeshelsa [Norhealth] [Internet]. Norwegian Institute of Public Health 2018 [cited 17/08/2018]. Available from: <www.norgeshelsa.no/norgeshelsa>.
- 11.Overvågning i tal, grafer og kort: vaccinationstilslutning [Surveillance in numbers, graphs and maps: vaccination Coverage] [Internet]. Statens Serum Institut [State Serum Institute]. 2018 [cited 17/08/2018]. Available from: <https://www.ssi.dk/Smitteberedskab/Sygdomsovervaagning.aspx>.
- 12.Slåttelid Schreiber S.M., Juul K.E., Dehlendorff C., Kjaer S.K. Socioeconomic predictors of human papillomavirus vaccination among girls in the Danish childhood immunization program. J Adolescent Health: Off Publ Soc Adolescent Med. 2015;56(4):402–407. doi: 10.1016/j.jadohealth.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Suppli C, Valentiner-Branth P. EPI-NYT Uge 41 - 2017 [EPI-NEWS Week 41 - 2017]: Statens Serum Institut [State Serum Institute]; [Available from: <https://www.ssi.dk/Aktuelt/Nyhedsbreve/EPI-NYT/2017/Uge%2041%20-%202017.aspx>.
- 14.De Vaccinerede Piger - Syge og Svigtede [The Vaccinated Girls – Ill and Betrayed]. TV2; 2015.
- 15.Lægemiddelstyrelsen [Danish Medicines Agency]. Årsrapport for overvågning af bivirkninger 2015 [Annual report for the surveillance of side effects 2015]; 2016
- 16.Lægemiddelstyrelsen [Danish Medicines Agency]. Årsrapport for overvågning af bivirkninger 2014 [Annual report on the surveillance of side effects 2014]’; 2015
- 17.Rambout L., Tashkandi M., Hopkins L., Tricco A.C. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: a systematic review. Prev Med. 2014;58:22–32. doi: 10.1016/j.ypmed.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Ferrer H.B., Trotter C., Hickman M., Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. doi: 10.1186/1471-2458-14-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mortensen G.L. Drivers and barriers to acceptance of human-papillomavirus vaccination among young women: a qualitative and quantitative study. BMC Public Health. 2010;10:68. doi: 10.1186/1471-2458-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dempsey A.F., Abraham L.M., Dalton V., Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. 2009;19(8):531–538. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lefevre H., Schrimpf C., Moro M.R., Lachal J. HPV vaccination rate in French adolescent girls: an example of vaccine distrust. Arch Dis Child. 2018;103(8):740–746. doi: 10.1136/archdischild-2017-313887. [DOI] [PubMed] [Google Scholar]
- 22.Margolis M.A., Brewer N.T., Shah P.D., Calo W.A., Gilkey M.B. Stories about HPV vaccine in social media, traditional media, and conversations. Prev Med. 2019;118:251–256. doi: 10.1016/j.ypmed.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Case A., Paxson C. Mothers and others: who invests in children’s health? J Health Econ. 2001;20(3):301–328. doi: 10.1016/s0167-6296(00)00088-6. [DOI] [PubMed] [Google Scholar]
- 24.Krawczyk A., Knauper B., Gilca V., Dube E., Perez S., Joyal-Desmarais K. Parents' decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccines Immunotherap. 2015;11(2):322–329. doi: 10.1080/21645515.2014.1004030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lutz M.E. The effects of family structure and regular places of care on preventive health care for children. Health Values. 1990;14(1):38–45. [PubMed] [Google Scholar]
- 26.Danmarks Statistik [Statistics Denmark]. Statistikbanken [Bank of Statistics]; 2018 Available from: <www.statistikbanken.dk>.
- 27.Andersen PH. EPI-NYT Uge 42/43 - 2006 [EPI-NEWS Week 42/43 - 2006]. Available from: <https://www.ssi.dk/~/media/Indhold/DK%20-%20dansk/Aktuelt/Nyhedsbreve/EPI-NYT/EPI-NYT-Arkiv/2006/2006%20PDF/EPI-NYT%20-%202006%20-%20uge%2043.ashx>.
- 28.Andersen PH. EPI-NYT Uge 35 - 2008 [EPI-NEWS Week 35 - 2008]. Available from: <https://www.ssi.dk/~/media/Indhold/DK%20-%20dansk/Aktuelt/Nyhedsbreve/EPI-NYT/2008/2008%20PDF/EPI-NYT%20-%202008%20-%20uge%2035.ashx>.
- 29.Pedersen C.B. The Danish civil registration system. Scand. J. Public Health. 2011;39(7 Suppl):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 30.OECD Project on Income Distribution and Poverty. What are equivalence scales? Available from: <http://www.oecd.org/els/soc/OECD-Note-EquivalenceScales.pdf>.
- 31.Danmarks Statistik [Statistics Denmark]. DEGURBA - DANMARKS STATISTIC VERS. 1.0; 2018. Available from: <https://www.dst.dk/da/Statistik/dokumentation/nomenklaturer/degurba---danmarks-statistik>.
- 32.DEGURBA - eurostat. European Commission; 2018 Available from: <https://ec.europa.eu/eurostat/web/gisco/geodata/reference-data/population-distribution-demography/degurba>.
- 33.UNESCO. International Standard Classification of Education (ISCED) 2011 [cited 2018 13-08]. Available from: <http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf>.
- 34.Digitaliseringsstyrelsen [The Danish Agency for Digitisation]. Om nemID [About nemID]; 2018. Available from: <https://www.nemid.nu/dk-en/about_nemid>.
- 35.Digitaliseringsstyrelsen [The Danish Agency for Digitisation]. Fritagelse fra Digital Post [Exemption from Digital Post]. Available from: <https://digst.dk/it-loesninger/digital-post/om-loesningen/fritagelse/>.
- 36.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holt N., Mygind A., Bro F. Danish MMR vaccination coverage is considerably higher than reported. Danish Med J. 2017.;64(2) [PubMed] [Google Scholar]
- 38.Berenson A.B., Laz T.H., Hirth J.M., McGrath C.J., Rahman M. Effect of the decision-making process in the family on HPV vaccination rates among adolescents 9–17 years of age. Hum Vaccines Immunotherap. 2014;10(7):1807–1811. doi: 10.4161/hv.28779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reiter P.L., Brewer N.T., Smith J.S. Human papillomavirus knowledge and vaccine acceptability among a national sample of heterosexual men. Sex Transm Infect. 2010;86(3):241–246. doi: 10.1136/sti.2009.039065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30(25):3778–3789. doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 41.Påmindelser om manglende børnevaccination [Reminders of lacking childhood vaccinations]: Statens Serum Institut [State Serum Institute]; 2017. Available from: <https://www.ssi.dk/vac>.
- 42.Griffioen A.M., Glynn S., Mullins T.K., Zimet G.D., Rosenthal S.L., Fortenberry J.D. Perspectives on decision making about human papillomavirus vaccination among 11- to 12-year-old girls and their mothers. Clin Pediatr. 2012;51(6):560–568. doi: 10.1177/0009922812443732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bodemer N., Muller S.M., Okan Y., Garcia-Retamero R., Neumeyer-Gromen A. Do the media provide transparent health information? A cross-cultural comparison of public information about the HPV vaccine. Vaccine. 2012;30(25):3747–3756. doi: 10.1016/j.vaccine.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Hargreaves I., Lewis J., Speers T. Economic and Social Research Council; Swindon: 2003. Towards a better map: science, the public and the media. [Google Scholar]
- 45.Grilli R., Ramsay C., Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database Syst Rev. 2002;1:Cd000389. doi: 10.1002/14651858.CD000389. [DOI] [PubMed] [Google Scholar]
- 46.Eberth J.M., Kline K.N., Moskowitz D.A., Montealegre J.R., Scheurer M.E. The role of media and the Internet on vaccine adverse event reporting: a case study of human papillomavirus vaccination. J Adolescent Health: Off Publ Soc Adolescent Med. 2014;54(3):289–295. doi: 10.1016/j.jadohealth.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Keelan J., Pavri V., Balakrishnan R., Wilson K. An analysis of the Human Papilloma Virus vaccine debate on MySpace blogs. Vaccine. 2010;28(6):1535–1540. doi: 10.1016/j.vaccine.2009.11.060. [DOI] [PubMed] [Google Scholar]
- 48.Sorensen K., Pelikan J.M., Rothlin F., Ganahl K., Slonska Z., Doyle G. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU) Eur J Pub Health. 2015;25(6):1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kennedy C., Gray Brunton C., Hogg R. 'Just that little bit of doubt': Scottish parents', teenage girls' and health professionals' views of the MMR, H1N1 and HPV vaccines. Int J Behav Med. 2014;21(1):3–10. doi: 10.1007/s12529-013-9356-4. [DOI] [PubMed] [Google Scholar]
- 50.Sjöberg SS. TV 2 om HPV-dokumentar: Vi er medansvarlige for at forældre undlod at vaccinere deres børn [TV2 on HPV-documentary: We share the responsibility for parents' omission of vaccinating their children]: Fyens Stifttidende; 2018. Available from: <https://www.fyens.dk/indland/TV-2-om-HPV-dokumentar-Vi-er-medansvarlige-for-at-foraeldre-undlod-at-vaccinere-deres-boern/artikel/3227673>.