Abstract
The recent reduction of live attenuated influenza vaccine (LAIV) effectiveness in multivalent formulations was particularly associated with the A(H1N1)pdm09 component. In the 2017 the WHO vaccine composition committee changed its recommendations for the A(H1N1)pdm09 component to include an A/Michigan/45/2015-like virus. We evaluated effectiveness and quality of newly developed and previous A(H1N1)pdm09 LAIV reassortants through assessment of their thermal and pH stability, receptor binding specificity and replication fitness in primary human airway epithelial cells of nasal origin (hAECN). Our analysis showed that LAIV expressed hemagglutinin (HA) and neuraminidase (NA) from an A/Michigan/45/2015-like strain A/New York/61/2015 (A/New York/61/2015-CDC-LV16A, NY-LV16A), exhibit higher thermal and pH stability compared to the previous vaccine candidates expressing HA and NA from A/California/07/2009 and A/Bolivia/559/2013 (A17/Cal09 and A17/Bol13). Reassortants A/South Africa/3626/2013-CDC-LV14A (SA-LV14A) and NY-LV16A showed preferential binding to α2,6 sialic acid (SA) receptors and replicated at higher titers and more extensively in hAECN compared to A17/Cal09 and A17/Bol13, which had an α2,3 SA receptor binding preference. Our data analysis supports selection of A/New York/61/2015-CDC-LV16A for LAIV formulation and the introduction of new assays for LAIV characterization.
Keywords: A(H1N1)pdm09 LAIV, Stability, Glycan, Replication, hAECN
1. Introduction
Live attenuated influenza vaccine (LAIV) seed viruses are reassortants containing the surface antigens hemagglutinin (HA) and neuraminidase (NA) from seasonal influenza viruses in the backbone (M, NS, NP, PA, PB1 and PB2 gene segments) of cold-adapted master donor virus (MDV). The MDV provides temperature-sensitive, cold- adapted, and attenuated phenotypes through mutations in PA, PB1, and PB2 gene segments that encode the RNA-dependent RNA polymerase, as well as some other proteins. There are currently two sets of donors of attenuation that are approved for generation of LAIV: A/Leningrad/134/17/1957 and B/USSR/60/1969 for LAIV produced in Russia, India, and China, and A/Ann Arbor/6/1960 and B/Ann Arbor/1/1966 for LAIV production in USA/Canada (FluMist) and Europe (Fluenza).
LAIVs based on Ann/Arbor MDVs are typically prepared using patented reverse genetics technology [1], [2]. LAIVs based on Len/17-MDV or B/USSR/60/69 are typically prepared by classical reassortment in embryonated chicken eggs [3]. LAIVs based on Len/17-MDV or B/USSR/60/69 have been used for decades in Russia and since 2011 in India. Vaccines generated using these two backbones have been shown to be safe and effective [3], [4], [5], [6]. In some studies, superior efficacy of LAIV over inactivated vaccines has been observed for both antigenically well-matched and drifted viruses [7]. However, lower than expected effectiveness of LAIVs based on Ann/Arbor MDV were observed in the USA in 2013–2014 and 2015–2016 seasons, leading the US Advisory Committee on Immunization Practices (ACIP) to withdraw recommendations for use of LAIV during the 2016–2017 and 2017–2018 influenza seasons within the USA [8], [9]. The decreased efficacy of LAIV in the US was correlated with lack of effectiveness against influenza A(H1N1)pdm09 vaccine component A/California/7/2009–like virus [10], [11], [12], [13]. Safety and immunogenicity studies of Len/17-MDV based LAIV containing A(H1N1)pdm09-like component were also conducted in Bangladesh and Senegal; however, the results of this studies were controversial. In Bangladesh, vaccine efficacy were estimated as 57%, while in Senegal the same lot of LAIV was ineffective [14], [15]. Several hypotheses were proposed to explain the low vaccine effectiveness of the LAIV against A(H1N1)pdm09 including poor thermal stability of the vaccine, low replicative fitness of vaccine strain; viral interference in the quadrivalent formulation and suppressed replication under preexisting influenza virus immunity [16], [17], [18].
The immunogenicity of LAIV relies on the processes of infection and replication in respiratory epithelial cells in the upper respiratory tract, particularly nasopharyngeal epithelial cells. Replication efficiency is impacted by the specific HA and (NA) proteins expressed by the LAIV, which are updated annually for use in trivalent and tetravalent vaccine compositions. Based on antigenic analysis, the A(H1N1)pdm09 vaccine component’s HA and NA gene segments remained the same from A/California/07/2009-like virus from its emergence in 2009. However, for the 2017 southern hemisphere season, the WHO vaccine composition committee updated the recommendations for the A(H1N1)pdm09 vaccine component to an A/Michigan/45/2015-like virus [19]. The potential impact of the specific HA and NA gene segments selected for vaccines, combined with increased international demand for the LAIV based on Len/17, prompted us to identify strategies to improve the assessment and/or quality control for LAIVs as part of the development process.
The goal of the current study is to characterize the new A/Michigan/45/2015-like reassortant and compare its characteristics to previously developed Len/17-MDV–based A(H1N1)pdm09 LAIV reassortants by analyzing receptor binding specificity, stability, and replication in primary human nasal cells.
2. Materials and methods
2.1. Generation of LAIV viruses
A(H2N2) A/Leningrad/134/17/57 MDV (Len/17-MDV) was provided by BioDiem (Australia). Seasonal A(H1N1)pdm09 influenza isolates, A/South Africa/3626/2013 and A/New York/61/2015, propagated in 9- to 11-day-old embryonated eggs were obtained from the Virus Reference Team, Centers for Disease Control and Prevention (CDC), Atlanta, USA. For vaccine preparation, specific pathogen-free (SPF) eggs (Charles River Laboratories Inc., USA) were used. LAIV reassortants—A17/California/2009/38 (A17/Cal09) and A17/Bolivia/2013/6585 (A17/Bol13)—were obtained from the Institute of Experimental Medicine (IEM), St. Petersburg, Russia [20]. Reassortants A/South Africa/3626/2013-CDC-LV14A (SA-LV14A) and A/New York/61/2015-CDC-LV16A (NY-LV16A) were generated by classical reassortment as described previously [21]. The HA and NA sequences of A/South Africa/3626/2013-CDC-LV14A and A/New York/61/2015-CDC-LV16A were submitted to the Global Initiative on Sharing All Influenza Data (GISAID) EpiFlu database with accession numbers EPI652003, EPI652004, EPI731788, and EPI731789.
2.2. Cells
Madin-Darby canine kidney (MDCK London) cells were maintained in DMEM High Glucose (Life Technologies, Carlsbad, CA) supplemented with 5% fetal bovine serum, 1x GlutaMAX (Life Technologies) and 40 μg/ml Neomycin (Sigma-Aldrich, St. Louis, MO). The primary human airway epithelial cells of nasal origin (hAECN) were purchased from Epithelix (Epithelix Sàrl, Switzerland) and maintained on membrane supports at the air-liquid interface in serum-free media. Fully differentiated 10-day-old cultures were used for infection with LAIV reassortants.
2.3. Two-way hemagglutination inhibition assay
All hemagglutination assays were performed using 0.5% turkey red blood cells, as these cells have both 2–3 and 2–6 SA receptors and were shown previously to be the most appropriate choice for the influenza H1N1pdm viruses [22]. Hemagglutination inhibition (HI) assays were performed to determine the antigenic relationship between the parental reference virus and the LAIV reassortants generated. Ferret antisera were raised against both parental contemporary human isolates and candidate LAIV reassortants for use in the HI analysis [23]. Reassortant viruses were considered consistent with parental isolates if the heterologous titer was within two-fold of the homologous HI titer of the parental reference isolate.
2.4. Glycan microarray binding
Glycan microarray slides were produced under contract for CDC using a glycan library by Professor James Paulson at the Scripps Research Institute (La Jolla, CA), funded (see Table Supplementary 1 for a list of glycans used for analyses). Virus preparations were diluted in phosphate-buffered saline (PBS) with 2% (wt/vol) bovine serum albumin to an HA titer of 128. Virus suspensions were applied to the slides, and the slides were incubated at 4 °C for 1.5 h. Unbound virus was washed off with brief sequential rinses in PBS with 0.05% Tween 20 (PBS-T) and PBS. The slides were then immediately incubated with ferret serum raised against A/South Africa/3626/2013 A(H1N1)pdm09 (30 min) and then with a biotinylated anti-ferret IgG antibody (Rockland) in combination with streptavidin-Alexa Fluor488 conjugate (30 min) (Thermo Fisher, Waltham, MA, USA), with brief PBS-T/PBS washes after each incubation. After the final PBS–T/PBS washes, slides were washed briefly in deionized water, dried by a gentle steam of nitrogen gas, and immediately subjected to imaging. Fluorescence intensities were detected using an Innoscan 1100AL scanner (Innopsys, Carbonne, France). Image analyses were carried out using ImaGene 9 image analysis software (BioDiscovery, El Segundo, CA, USA).
2.5. Analyses of virus thermostability
LAIV reassortants (70 μl) were dispensed into 0.2-ml thin-walled PCR tubes (USA Scientific, Ocala, FL). Tubes were placed into a BioRad 96-well thermal cycler (BioRad, Hercules, CA). The temperature range was set at 50–65.0 °C. Tubes were heated for 20 min and then transferred to ice. Control samples containing 70 μl of virus were incubated for 20 min at ambient room temperature. The virus content in each sample was determined by an HA assay. Each virus sample was analyzed in three independent experiments and average value was determined.
2.6. Analysis of virus pH stability
To measure the effect of acid exposure on the retention of infectivity, virus stocks were diluted 1/10 in PBS, then in PBS or citric acid buffers adjusted to the desired pH and incubated at 32 °C for 1 h. The infectivity of these viruses were then determined by measuring EID50: pH stability was determined as pH values that corresponded to virus inactivation by 50% (pH50-inact). The titers of low-pH–treated viruses were expressed as percentages of the titers of viruses that were incubated at pH 7.4 (PBS). Infectivity-versus-pH curves were plotted, and pH50-inact values were determined by linear interpolation.
2.7. Infection of MDCK or primary hAECN with LAIV
MDCK were seeded the day before the inoculation into 6 well plates at 106 cells/well. Confluent cell monolayers were inoculated with LAIV reassortants at multiplicity of infection (MOI) of 0.001 for 1 h at 33 °C. Then virus inoculum was removed, cells were washed twice with PBS, and media were changed to DMEM supplemented with 2% BSA, 10 µg/ml GlutaMAX, 40 μg/ml Neomycin (Sigma-Aldrich, St. Louis, MO), and 1 μg/ml of TPCK-trypsin. Supernatants of infected cells were collected at the indicated points of time and virus titers were determined as 50% tissue culture infectious dose per milliliter (TCID50/mL) in confluent MDCK cells in 96-well microtiter plates.
Primary hAECN were inoculated with LAIV reassortants at a MOI of 0. 01. For inoculation of hAECN (Epithelix), the apical surface (air interface) was washed 10 times with serum-free medium to remove accumulated mucins. Then hAECN cells were inoculated with 0.2 ml/well of virus diluted in complete MucilAir™ Culture medium (Epithelix), supplemented with growth factors. The inoculum was removed after 1 h of incubation at 33 °C and the cell culture was washed twice to remove any unbound virus particles. To collect samples to determine virus replication, 200 μl/well of PBS was added to the apical surface, incubated 15 min at 33 °C, removed, frozen at −80 and stored for subsequent titration. Samples were collected every day at the specific times post inoculation. The infectious viral titers were determined by TCID50 using MDCK cells.
2.8. Immunofluorescence analysis
Mock inoculated and inoculated primary hAECN were washed 10 times at the apical and basolateral sides with PBS, followed by fixation with freshly prepared 4% paraformaldehyde for 30 min at room temperature. The apical and basolateral sides were subsequently washed three times with 500 μl PBS, permeabilized with 0.5% Triton X-100 in PBS, blocked in 1% BSA in PBS, and incubated with primary antibodies for 2 h at room temperature, followed by incubation with Alexa Fluor secondary antibody for 30 min. The wells were washed 3 times with PBST (0.05% Tween-20 in PBS) between the incubations. The antibodies in the study were used as follows: biotinylated Sambucus Nigra Lectin (SNA) (Vector Laboratories, Burlingame, CA) used at 20 µg/ml, biotinylated Maackia Amurensis Lectin II (MAL II) and biotinylated Maackia Amurensis Lectin I (MAL I (Vector Laboratories) used at 20 µg/ml each, mouse monoclonal Anti-β-Tubulin IV antibody (Sigma) used at 1:500 dilution, and mouse anti-nucleoprotein (anti-NP) (IRR) used at 1:1000. Secondary antibody, streptavidin conjugated Alexa Fluor® 555, and goat anti-mouse IgG (H + L) Alexa Fluor 488 (Invitrogen by Thermo Fisher Scientific, Eugen, OR) were used at 1:2000 dilution. Nuclei were counterstained with Hoechst 33,342 Solution at 10 µM concentration.
Cells were visualized with an LSM 710 Zeiss inverted confocal microscope (Zeiss, Germany) with a 40× oil objective lens and processed using Zen 2012 software (Zeiss). All of the images compared were obtained using the same instrument settings. Images were collected at 0.38 µm intervals with the 488, 561, and 405 nm lasers to create a stack in the Z axis (orthogonal view) and shown as maximum intensity 3D projection (MIP) of Z-stack slices.
3. Results
3.1. Growth of A(H1N1)pdm09 reassortants in eggs
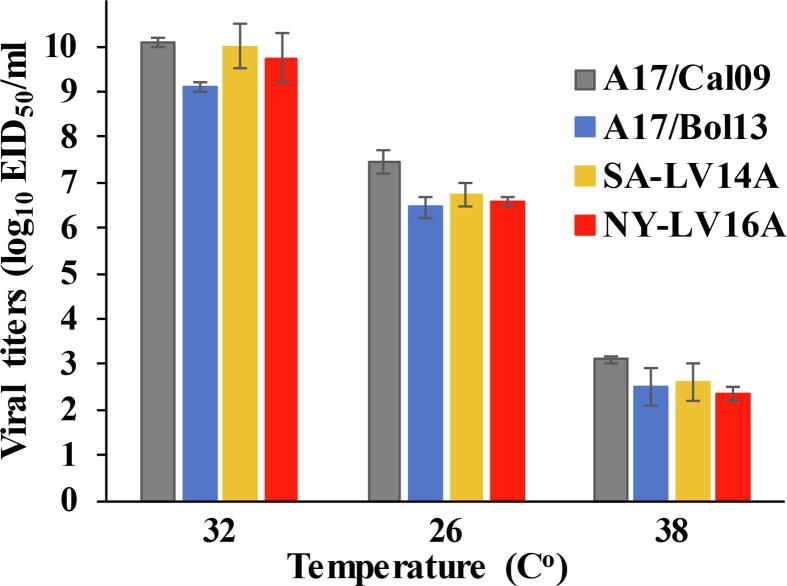
The generation of reassortants by classical reassortment requires multiple passage in eggs. This often selects for amino acid substitutions in HA that enhance replication in the avian host. Genetic sequencing and analysis revealed egg-adaptive changes in the various LAIV reassortants in HA segments as follows: A17/Cal09 acquired N156D and Q223R; A17/Bol13–Q223R and V345I, SA-LV14A–D127E, S183P, and L524V, NY-LV16A–D127E, and D222N (Table 1). The analysis of deduced NA amino acid sequence showed that A17/Bol13 acquired a D248Y substitution and SA-LV14A acquired a T135A substitution during the reassortment process, other NA sequences were identical to their cell counterparts. All LAIV reassortants had cold-adapted and temperature-sensitive phenotypes as indicated by replication to high titers of 9–10 log10 EID50/ml at the optimal temperature (32 °C), limited reduction in titers at low temperature (25 °C), and significant reductions up to 7 log10 EID50 at restrictive temperature (38 °C) (Fig. 1).
Table 1.
Amino acid substitutions in hemagglutinin (HA) of LAIV A(H1N1)pdm09 reassortants compared to cell grown A/California/07/2009 reference sequence.
 |
*Red color indicates egg- acquired HA changes compared to their respective cell isolates.
**The different amino acids between A/California/07/2009 reference sequence and cell grown viruses are shown in black.
Fig. 1.
Infectious viral titers of A(H1N1)pdm09 LAIV viruses at permissive and restrictive temperatures. Virus stocks were propagated in eggs for 2 days at the optimal temperature of 32 °C, for 6 days at the permissive temperature of 26 °C, and for 2 days at a restrictive 38 °C temperature. The bars represent virus titers at indicated temperatures and the error bars represent standard deviation.
3.2. Evaluation of A(H1N1)pdm09 reassortant virus antigenicity in ferrets
Amino acid substitutions in HA at the positions 222 and 223 are important for receptor binding preference. The substitutions impact efficient utilization of mammalian- or avian sialic acid–containing receptors and can impact antigenic properties of the virus or vaccine [24], [25], [26], [27], [28]. Polyclonal ferret antisera was raised to SA-LV14A and NY-LV16A to assess their antigenic profile. Despite the amino acid substitutions found in the HA, both SA-LV14A and NY-LV16A passed the two-way HI test (data for SA-LV14A not shown). Two-way HI cross-reactivity of NY-LV16A reassortant virus was compared to the A/New York/61/2015 reference virus (egg isolate E5 passage) and the cell-propagated A/Michigan/45/15 that was recommended as an A(H1N1)pdm09 vaccine component for 2016–2017 season. NY-LV16A was well inhibited by ferret antiserum raised to either egg- or cell-propagated reference viruses, both reference viruses were well inhibited by ferret antiserum raised to the NY-LV16A virus, indicating antigenic similarity in a two-way HI test (Table 2). Ferret antiserum raised to NY-LV16A also inhibited the majority of recently circulating viruses, with HI titers equal to or within two-fold of the homologous HI titer of the parental reference virus (Table 2) further confirming its suitability as a vaccine candidate.
Table 2.
Antigenic analysis of NY-LV16A by Two-way HI test with ferret antisera.
| Reference antigens | Reference ferret antisera |
||||||
|---|---|---|---|---|---|---|---|
| CA/7 | CA/7 | MI/45 | MI/45 | NY/61 | LV16A | Passage | |
| A/California/7/2009 | 2560 | 2560 | 1280 | 5120 | 2560 | 2560 | E3* |
| A/California/7/2009 | 2560 | 2560 | 1280 | 2560 | 2560 | 1280 | C2 |
| A/Michigan/45/15 | 2560 | 2560 | 1280 | 2560 | 2560 | 2560 | E3 |
| A/Michigan/45/15 | 2560 | 2560 | 1280 | 2560 | 2560 | 1280 | M1/C3 |
| A/New York/61/2015 | 1280 | 1280 | 640 | 2560 | 2560 | 1280 | E5 |
| A/NY- LV16A | 2560 | 2560 | 1280 | 2560 | 5120 | 2560 | E5/SPF9 |
Homologous titer of ferret antiserum to reference antigen are indicated in bold.
E-eggs, C-cells, M-MDCK cell line, SPF – specific pathogen free eggs; number denotes the passage.
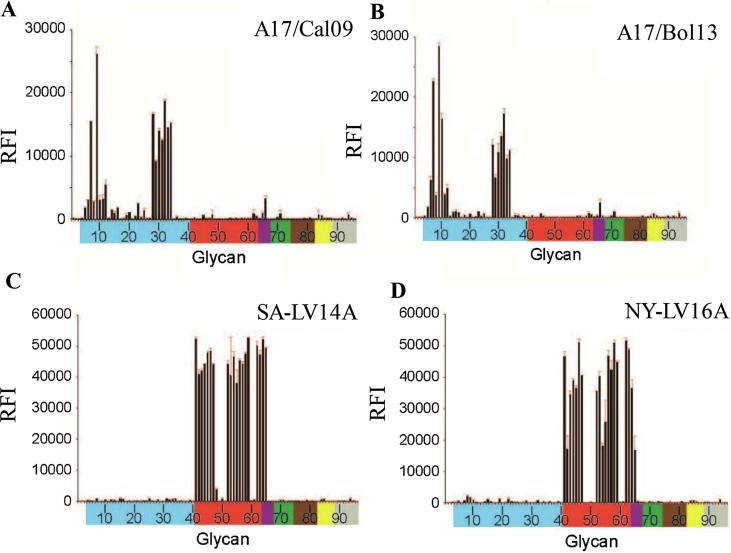
3.3. Receptor binding specificity of LAIV reassortants determined by glycan array
Glycan microarray analysis helps provide a detailed profile of influenza virus receptor specificity [29]. Sialic acid (SA) moieties found in mammals and birds are N-acetylneuraminic acid (Neu5Ac) and N-glycolylneuraminic acid (Neu5Gc). SA are bound to terminal sugars of glycoproteins and glycolipids, to the galactose carbon-6 forming an α2,6 linkage (human-like), or to galactose carbon-3 forming an α2,3 linkage (avian-like) [30]. Of the 96 glycans present on the array used in the study, 3 are sialic acids (SA), 37 have SA with α2-3 linkages to galactose, 23 have SA with α2-6 linkages, four have mixed α2-3/α2-6-linked biantennaries, seven are N-glycolylneuraminic acid-linked glycans, eight are α2-8-linked sialosides, four are β2-6-linked, two are 9-O-acetylated-linked SA, and eight are asialo-glycans (Supplementary Table 1). Viral binding can be analyzed by glycan array not only for SA linkage preference, but also for additional features such as glycan size, charge and sulfation, fucosylation, or sialylation.
Glycan-binding analyses revealed that A17/Cal09 and A17/Bol13 LAIV reassortants bound to a range of α2-3-linked sialosides (glycans 4–12 and 27–34), including linear and biantennary sialosides with or without fucosylation/sulfation, with the strongest binding to α2-3-linked glycans 7, 9 and 32 (Fig. 2). SA-LV14A and NY-LV16A LAIV reassortants showed a strong binding preference for the α2-6-linked SAs (glycans 41–47, 52–59, and 62, 63) and mixed α2–3/α2–6 branched SAs (glycans 64 and 65). Thus, the data showed that A17/Cal09 and A17/Bol13 LAIV reassortants had an avian influenza virus-like receptor binding preference while SA-LV14A and NY-LV16A reassortants had a human influenza virus-like receptor binding preference.
Fig. 2.
Receptor binding specificity of LAIV A(H1N1)pdm09 reassortants A17/Cal09 (A), A17/Bol13 (B), SA-LV14A(C) and NY-LV16A (D) identified by glycan microarray analysis. The identity of each numbered glycan (horizontal axis) is provided in Supplemental Table 1. Different categories of glycans on the array are color-coded in column 1 as follows: no color, sialic acid; blue, α2-3 sialosides; red, α2-6 sialosides, purple, mixed α2-3/α2-6 biantennaries; green, N-glycolylneuraminic acid–containing glycans; brown, α2-8 linked sialosides; yellow, β2-6 linked as well as 9-O-acetylated sialic acids; grey, asialo glycans. The vertical bars denote relative fluorescence intensity, RFI (vertical axis) and error bars indicate the standard error of the mean. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
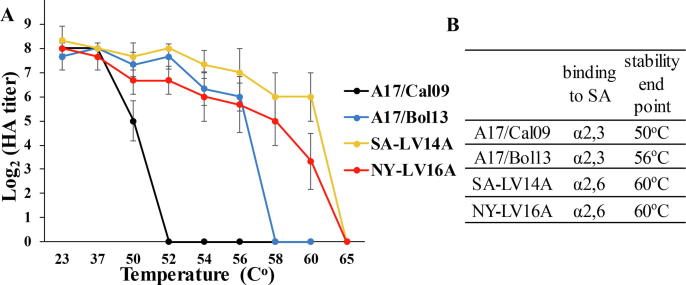
3.4. Analysis of thermal and pH stability of A(H1N1)pdm09 LAIV reassortants
HA mediates virus binding to SA receptors, followed by endocytosis and fusion of viral and endosomal membranes to release viral RNA. The low pH–triggered fusion resulted in HA conformational changes that caused irreversible virus inactivation in the absence of target membrane, providing a marker for HA stability. Exposure to high temperature results in HA conformational changes which are indistinguishable from the ones induced by acidic conditions [31] and also lead to the loss in the ability to bind to cellular receptors (hence agglutinate erythrocytes in hemmaglutination assay) and reduced infectivity. The direct correlation between loss in HA activity and viral infectivity was shown previously in the studies of H1N1pdm09 viruses stability [32], [33], [34].
To evaluate thermal stability of A(H1N1)pdm09 HA, LAIVs were incubated at temperatures between 50 °C and 65 °C for 20 min and the integrity of the HA protein was accessed by HA assay using 0.5% turkey RBC. The HA titer was measured pre- and post-incubation and HA activity threshold was determined as the lowest temperature resulted in complete loss HA activity. As expected, A17/Cal09 was the least stable, with no HA titer detected at 52 °C. A17/Bol13 was next in stability rank with a threshold point of 58 °C (Fig. 3). NY-LV16A and SA-LV14A reassortants were more thermostable, retaining high HA titers even after incubation at 60 °C (Fig. 3). The data showed that A17/Cal09 and A17/Bol13 reassortants are less heat stable compared to SA-LV14A and NY-LV16A (Fig. 3).
Fig. 3.
The effect of heat treatment on the stability of A(H1N1)pdm09 LAIV reassortants. (A) The virus stocks were incubated at indicated temperatures for 20 min and the HA titer was determined. Average values from three independent experiments with error bars as standard deviation (SD) are shown. (B) HA activity threshold was defined as the lowest temperature resulted in complete loss of HA activity.
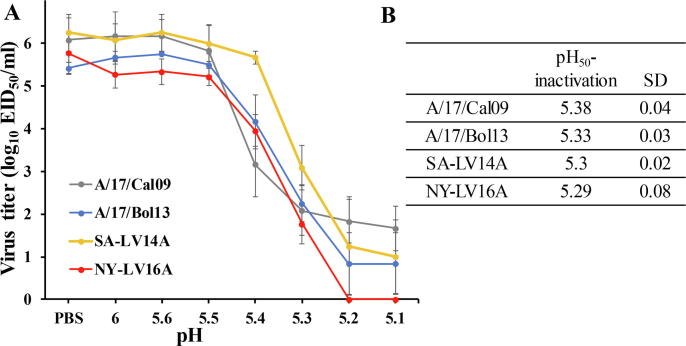
Acidic stability is important for efficient influenza infection. Viruses with higher pH of HA are less stable in the slightly acidic human nasal environment, but have a growth advantage from ability to release viral ribonucleoproteins more quickly to start replication [35]. To evaluate acidic stability, the reassortants were incubated in various pH ranging from pH 6.0 to 5.1 (citric buffers), and viral infectivity was then assessed by EID50. Infectivity was maintained at starting titers in the pH range of 6.0–5.6. In contrast, at pH 5.4, the infectious viral titers of SA-LV14A, A17/Bol13, and NY-LV16A were more than 2.0–3.0 logs higher than titers of A17/Cal/09. By pH 5.1, the infectivity of all viruses dropped below 2.0 log10 EID50/mL (Fig. 4A). The titers of low-pH-treated viruses were expressed as percentages of the titers of control viruses that were incubated in PBS, and pH stability was determined as pH values that corresponded to virus inactivation by 50%. As expected, A17/Cal09 was the least stable, with the highest pH value of 5.38; other reassortants had similar pH stability (Fig. 4B).
Fig. 4.
Loss of infectivity at acidic pH of A(H1N1)pdm09 LAIVs. (A) The virus stocks were diluted in PBS or buffers adjusted to the desired pH and incubated for 1 h. The infectivity of these viruses was then determined by EID50. (B) The titers of low-pH–treated viruses were expressed as percentages of the titers of viruses that were incubated at pH 7.0. Infectivity-versus-pH curves were plotted, and pH50-inactivation values were determined by linear interpolation. Mean values ± SD (standard deviation) from three independent experiments are shown.
3.5. Replication of LAIV A(H1N1)pdm09 reassortants in MDCK cells
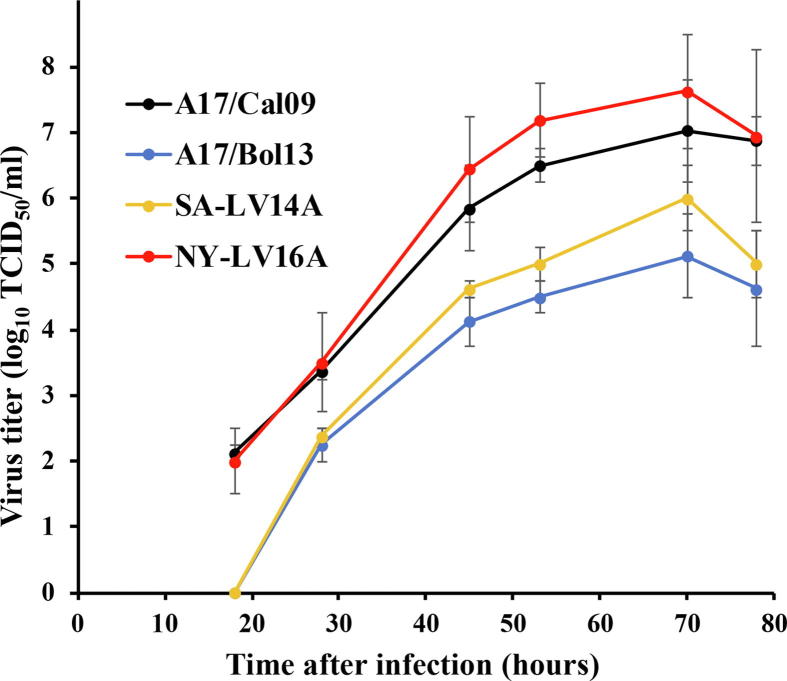
To evaluate if egg-generated LAIV reassortants replicate efficiently in cell culture, MDCK cells were infected with each A(H1N1)pdm09 reassortant at MOI of 0.001. Supernatant was sampled at various time points after infection and replication kinetics for all four reassortants were compared. NY-LV16A had consistently higher titers compared to other LAIVs starting from 28 h after infection and reaching the highest peak at 108 TCID50/ml at day 3, 70 h after infection (Fig. 5). A17/Cal09 reassortant replicated to lower titers compared to NY-LV16A, but more efficiently than A17/Bol13 or SA-LV14A, which replicated at comparable titers, reaching their highest peak of only 4.5 and 5.5 log10 TCID50/ml, respectively, at day 3 (Fig. 5). The results showed that the efficiency of LAIV reassortants replication in MDCK cells did not depend on or correlate with their receptor binding preferences.
Fig. 5.
Replication kinetics of A(H1N1)pdm09 LAIV viruses in MDCK cell cultures. Confluent MDCK monolayers were inoculated with the various A(H1N1)pdm09 viruses at an MOI of 0.001. Culture supernatants were collected at the indicated times post inoculation, and viral titers were determined by TCID50 on MDCK cells, the average titer ± SD is shown.
3.6. Characterization of primary human airway epithelial cell cultures
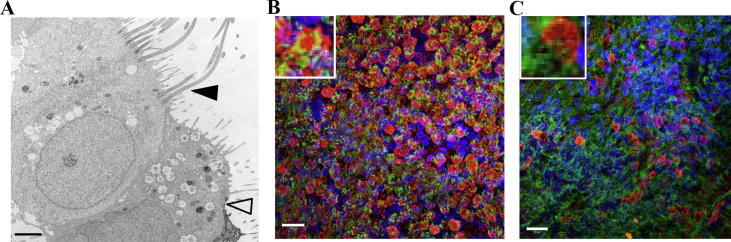
Since LAIV reassortants used for human vaccines are produced in eggs, efficient replication of LAIV in the human upper respiratory tract, including nasal epithelial cells, is important for LAIV infection and could impact vaccine performance. To determine if an in vitro system would be beneficial to analysis of candidate LAIVs, we examined if commercially available reconstituted hAECNs were susceptible to infection and could differentiate various candidates. The hAECN cultures were maintained in an air-liquid interface and were composed of a number of distinct cell types including ciliated epithelial cells, secretory goblet cells, and basal cells, which mimics the nasal cavity. The cultures even produce mucus. The presence of multiple cell types in hAECN, specifically ciliated cells and secretory cells producing mucus from the apical side of the cultures, was confirmed by transmission electron microscopy imaging (TEM) (Fig. 6A). Immunostaining with anti-tubulin IV (tubulin) antibody demonstrated ciliated cells among the total cell population (Fig. 6B and C). Ciliated cells were observed by visual inspection and represented more than 70% of the total cell population (Fig. 6B and C). To determine expression of various influenza A virus SA receptors on ciliated epithelial cells, hAECN cells were stained using lectins specific for α2,3-linked SA (Maackia amurensis tree [MAA] or α2,6-linked SA Sambucus nigra plant [SNA]). The results of confocal microscopic analysis showed that 30–40% of the cells displayed α2,3 SA residues and around half of these were ciliated cells (Fig. 6B, co-expression indicated in yellow). However, the number of α2,3-linked SAs cells detected, could be lower since recent study showed that MAL-I could also bind to nonsialylated glycans from the human lung [36]. As detected by SNA and anti-tubulin IV staining, less than 10% of the hAECN culture had α2,6 SAs and very few of them were ciliated (Fig. 6C).
Fig. 6.
Characterization of primary human epithelial cell of nasal origin (hAECN) cultures by transmission electron microscopy and immunofluorescence microscopy. (A) Multiple cell types in hAECN (TEM): filled arrow marks a ciliated cell, open arrow marks a mucus producing cell. Scale bar, 2 μm. (B and C) Immunofluorescent staining of cilia using anti-β tubulin IV antibody (tubulin) (green), lectins mixture MAA I and MAA II for α2,3-linked SA (B) or SNA lectin for α2,6-linked SA (red) and nuclei (blue, Hoechst) (C). Scale bar, 20 μm. An enlarged cell is shown in the inset on each panel. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
3.7. Replication of LAIV A(H1N1)pdm09 reassortants in hAECN cultures
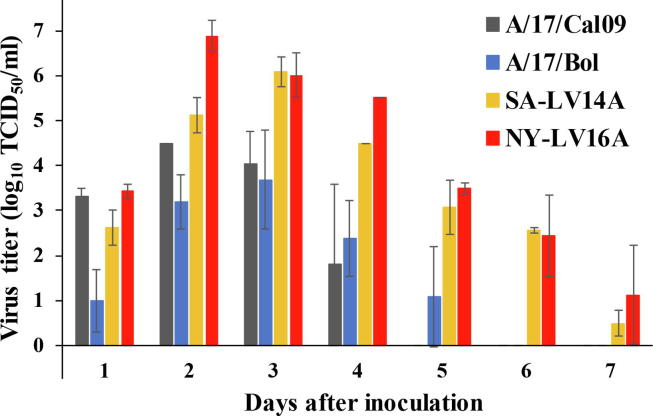
To evaluate LAIV replication in a culture system that represents the primary site for LAIV replication in humans, hAECN cultures were inoculated apically with four LAIVs (A17/Cal09, A17/Bol13, SA-LV14A, or NY-LV16A) and the replication kinetics of each virus were analyzed. Overall the LAIV viruses that preferentially bound α2,3 SA receptors (A17/Cal09 and A17/Bol13) replicated to lower titers in hAECN compared to those that showed α2,6 SA receptor preference (SA-LV14A and NY-LV16A). The NY-LV16A reached the highest titer (107 TCID50/ml) on day 2 post inoculation; titers were 10- to 1000-fold higher than the other LAIV viruses (Fig. 7). The other LAIV viruses analyzed reached their highest titers on day 3 post inoculation (106 TCID50/ml for SA-LV14A; up to 104–105 TCID50/ml for A17/Cal09 and A17/Bol13) (Fig. 7). Furthermore, the A17/Cal09 and A17/Bol13 viruses replicated less efficiently than SA-LV14A and NY-LV16A and for a shorter period of time (titer below limit of detection by day 5 or 6, respectively) (Fig. 7).
Fig. 7.
Replication of A(H1N1)pdm09 reassortants in hAECN. Cells were inoculated apically with each virus at an MOI of 0.01. Cell culture supernatants were collected at the indicated time points from the apical side of the cultures, and virus titers were determined by TCID50 using MDCK cells. The average titer of two independent experiments were calculated and error bars indicate the standard error of the mean.
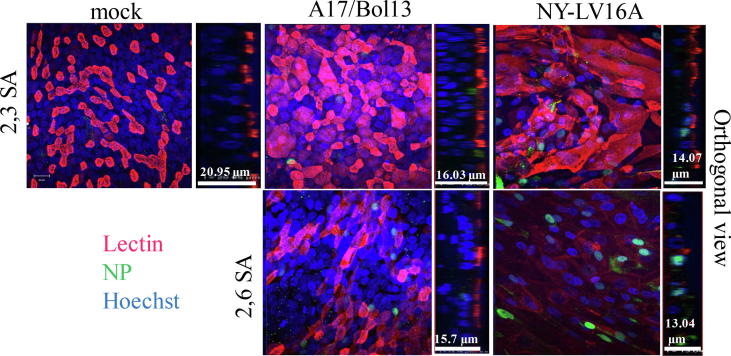
Finally, the relationships between infection and the epithelial cell culture integrity were examined at later post-inoculation times. Virus inoculation and subsequent infection did not result in death of all the cells in the cultures and infected cells (NP positive) could be detected on day 9 post inoculation (Fig. 8). Compared to mock inoculated cell cultures, infection by LAIVs resulted in significant cell morphology changes (forming stretched elongated strands) and thinning of the epithelial cell layers, as indicated by Z stack measurement, shown as the orthogonal view of depth dimension (Fig. 8). Infection by the NY-LV16A LAIV, which had the most α2,6-linked SA specificity, resulted in dramatic reduction in overall cell number and extensive loss of cells expressing α2,6-linked SA receptors (Fig. 8).
Fig. 8.
Evaluation of the integrity of the infected hAECN. The cells were inoculated with A17/Bol13 (middle panel) or NY-LV16A (right panel) virus at MOI of 0.01 and fixed at day 9 post inoculation. Uninfected or infected cells were stained to identify influenza virus nucleoprotein (NP) (green), 2,3 SA (top panel) or 2,6 SA (bottom panel) receptor bearing cells (red, MAA or SNA) and nuclei (blue, Hoechst). The images were obtained as described in Materials and Methods. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
Seasonal influenza vaccines provide protection against the strains of influenza that are predicted to circulate during a given influenza season. Antigenic match between the vaccine strain and circulating strains is an important factor for success of vaccination. Based on genetic characterization data, human serologic evidence, and A(H1N1)pdm09 vaccine effectiveness data–for the first time since the strain’s appearance in 2009 – WHO recommended changing the A(H1N1)pdm09 vaccine component in 2017 to contemporary A/Michigan/45/2015-like virus. The A/Michigan/45/2015 virus belongs to the 6B.1 genetic group, which represents the majority of circulating A(H1N1)pdm09 viruses [19]. However, egg-grown A/Michigan/45/2015 virus contained an egg-adapted change, Q223R in the HA protein, which was shown to correlate with change in virus receptor binding specificity. It was reported that amino acid residue at locations 222 and 223 of the HA of A(H1N1)pdm09 viruses impacts binding preference for either human-like (222D, 223Q) or avian-like (222G, 223R) receptors, although post-infection ferret antisera did not recognized any antigenic differences among wild type viruses, with 223Q and viruses containing 223R in HI tests [24], [27], [37].
In order to induce sufficient immune response, LAIV viruses should be able to bind to the human-like α2,6 SA receptor and replicate efficiently in the human upper respiratory tract. For this reason, one of the egg clones of A/New York/61/2015, the virus from an A/Michigan/45/2015-like A(H1N)1pdm09 6B.1 group, predicted to have human-like receptor binding specificity (222 N, 223Q of HA residues), was selected for generation of the A(H1N1)pdm09 vaccine component of LAIV in the backbone of Len/17-MDV. We analyzed the stability, receptor binding specificity, and replication fitness of new LAIV reassortant NY-LV16A in primary human nasal cells and compared it with the previously developed A(H1N1)pdm09 reassortants to justify the selection of NY-LV16A as replacement for A17/California/07/2009 in current Len/17-MDV based LAIV formulations.
All A(H1N1)pdm09 LAIV reassortants described in the present study were obtained by classical reassortment in eggs and all had egg-adaptive amino acid substitutions in the HA protein (Table 1). Most of the identified substitutions may impact receptor-binding and/or antigenicity of the HA. NY-LV16A has two additional changes, D127E and D222N, in the HA compared to the egg-grown A/New York/61/2015 isolate, which did not affect either its receptor binding specificity (detected by glycan array) (Fig. 2) or antigenicity as shown by HI tests with post-infection ferret antisera (Table 2). Moreover, as expected, reassortants possessing 223R (A17/Cal09 and A17Bol13) showed specificity to avian-like (α2,3 SA) receptors. Reassortants with 223Q (SA-LV14A and NY-LV16A) specifically bound to human-like (α2,6 SA) glycans receptors (Fig. 2), warranting further evaluation of these as suitable LAIV candidates.
It was previously reported that thermal instability of A/California/07/2009 HA might have contributed to the lack of LAIV effectiveness in the US, as a number of vaccine lots were found to have been exposed to higher than recommended temperatures during shipping and handling, and this exposure statistically correlated with lot-to-lot reduced vaccine effectiveness [17]. We addressed both the loss of infectivity at low pH of Len/17-MDV–based A(H1N1)pdm09 LAIV reassortants (pH stability) and loss of their HA titers at high temperatures (thermal stability). The ranking of stability of LAIV reassortants from most to least stable was determined as SA-LV14A > NY-LV16A > A/17/Bol13 > A17/Cal09. We thus confirmed that A17/Cal09 LAIV virus possessed thermally unstable HA, supporting its replacement in a current Len/17-MDV LAIV formulations.
By improving stability, the HA protein could be over-stabilized, compromising its activation at the low endosomal pH required for successful viral entry and effective replication. Replication efficiency of A(H1N1)pdm09 LAIV in the primary human epithelial ALI culture system was analyzed and showed that the two mostly stable reassortants, SA-LV14A and NY-LV16A, replicated to the highest levels of replication. Release of these viruses from the apical surface could be detected during the whole infection period analyzed, i.e., up to day seven after infection (Fig. 7). The replication in hAECN was also shown to correlate with the receptor binding preferences of LAIV viruses. Conversely, replication and release of LAIV with α2,3 SA preference, A17/Cal09 and A17/Bol13, was shorter and at lower titers compared to LAIVs with α2,6 SA binding preferences (Fig. 7). The confocal data of infected cells confirmed these observations: more NP-positive cells were detected in NY-LV16A infected primary epithelial cells compared to ones infected with A17/Bol13 even though overall amount of cells infected with NY-16A was greatly reduced (Fig. 8). It should be noted also that the amount of α2,3-linked SA cells detected in hAECN by MAL staining could be in fact lower, since it was reported recently that MAL-I commonly used for α2,3-linked SA detection could also bind to non-sialylated glycans from the human lung [36], specifically, to certain non-sialylated, galactose-terminating, branched complex-type N-glycans [38], [39]. Therefore, the air/liquid interface culture system revealed characteristics of LAIV infection that were different from immortalized MDCK cells. There was no receptor dependence tendency of LAIV replication in MDCK cells. NY-LV16A (α2,6 SA preference) and A17/Cal09 (α2,3 SA preference) replicated more efficiently compared to SA-LV14A (α2,6 SA preference) and A17/Bol13 (α2,3 SA preference) in MDCK cells (Fig. 5), indicating that these cells cannot be a reliable model for evaluation of human LAIV candidates replication efficiency.
The current formulation of LAIVs generated on the backbone of A/Leningrad/17/134/57 and B/USSR/60/69 are based on virus replication in eggs, EID50/ml, where each vial of single trivalent or quadrivalent LAIV dose should have not less than 107 EID50 of both A(H1N1)pdm09 and A/H3N2 strains and not less than 106.5 EID50 of B strain. This formulation does not reflect levels of LAIV replication in human nasal cells. There are no current requirements to determine the titers of LAIV in human nasal cells for LAIV properties assessment. Since effective replication of LAIV upon delivery to nasal epithelium is critical for vaccine performance, including the evaluation of replication fitness of newly developed LAIV reassortants in human primary cells of the upper respiratory tract as a quality control for LAIV characterization should be considered. Due to the importance of pH stability in the virus life cycle and thermal stability for LAIV performance, these properties should continue to be assessed during seasonal development of LAIV reassortants. Overall, the robust and durable replication of LAIV reassortant NY-LV16A in hAECN supported its selection for use in a current LAIV formulation; however, further analysis of new vaccine effectiveness in human populations is warranted.
Declaration of Competing Interest
The authors declared that there is no conflict of interest.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. We thank BioDiem (Australia) for providing MDV A/Leningrad/134/17/57. We thank Elisabeth Blanchard, Priya Budhathoki, and Xiyan Xu for providing A(H1N1)pdm09 influenza egg-grown isolates, ferret serum preparation, and HI tests. We thank Hui Zeng for technical advice and help with confocal microscopy of primary cells.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jvacx.2019.100031.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Jin H., Chen Z., Liu J., Kemble G. Genetic engineering of live attenuated influenza viruses. Methods Mol Biol. 2012;865:163–174. doi: 10.1007/978-1-61779-621-0_10. [DOI] [PubMed] [Google Scholar]
- 2.Jin H., Subbarao K. Live attenuated influenza vaccine. Curr Top Microbiol Immunol. 2015;386:181–204. doi: 10.1007/82_2014_410. [DOI] [PubMed] [Google Scholar]
- 3.Rudenko L., Yeolekar L., Kiseleva I., Isakova-Sivak I. Development and approval of live attenuated influenza vaccines based on Russian master donor viruses: Process challenges and success stories. Vaccine. 2016;34:5436–5441. doi: 10.1016/j.vaccine.2016.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudenko L.G., Lonskaya N.I., Klimov A.I., Vasilieva R.I., Ramirez A. Clinical and epidemiological evaluation of a live, cold-adapted influenza vaccine for 3–14-year-olds. Bull World Health Organ. 1996;74:77–84. [PMC free article] [PubMed] [Google Scholar]
- 5.Nigwekar P.V., Kumar A., Padbidri V.V., Choudhury A., Chaudhari A.B., Kulkarni P.S. Safety of russian-backbone trivalent, live attenuated seasonal influenza vaccine in healthy subjects: open-label, non-randomized phase 4 study. Drug Saf. 2017 doi: 10.1007/s40264-017-0605-3. [DOI] [PubMed] [Google Scholar]
- 6.Kulkarni P.S., Agarkhedkar S., Lalwani S., Bavdekar A.R., Jog S., Raut S.K. Effectiveness of an Indian-made attenuated influenza A(H1N1)pdm 2009 vaccine: a case control study. Human Vaccines Immunother. 2014;10:566–571. doi: 10.4161/hv.27490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belshe R.B., Edwards K.M., Vesikari T., Black S.V., Walker R.E., Hultquist M. Live attenuated versus inactivated influenza vaccine in infants and young children. N Eng J Med. 2007;356:685–696. doi: 10.1056/NEJMoa065368. [DOI] [PubMed] [Google Scholar]
- 8.Grohskopf L.A., Sokolow L.Z., Broder K.R., Olsen S.J., Karron R.A., Jernigan D.B. Prevention and control of seasonal influenza with vaccines. MMWR Recomm Rep. 2016;65:1–54. doi: 10.15585/mmwr.rr6505a1. [DOI] [PubMed] [Google Scholar]
- 9.Grohskopf L.A., Sokolow L.Z., Broder K.R., Walter E.B., Bresee J.S., Fry A.M. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices - united states, 2017–18 influenza season. MMWR Recomm Rep. 2017;66:1–20. doi: 10.15585/mmwr.rr6602a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedman N., Drori Y., Pando R., Glatman-Freedman A., Sefty H., Bassal R. A(H1N1)pdm09 influenza infection: vaccine inefficiency. Oncotarget. 2017;8:32856–32863. doi: 10.18632/oncotarget.16459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gaglani M., Pruszynski J., Murthy K., Clipper L., Robertson A., Reis M. Influenza vaccine effectiveness against 2009 pandemic influenza A(H1N1) virus differed by vaccine type during 2013–2014 in the United States. J Infect Dis. 2016;213:1546–1556. doi: 10.1093/infdis/jiv577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puig-Barbera J., Guglieri-Lopez B., Tortajada-Girbes M., Lopez-Labrador F.X., Carballido-Fernandez M., Mollar-Maseres J. Low influenza vaccine effectiveness and the effect of previous vaccination in preventing admission with A(H1N1)pdm09 or B/Victoria-Lineage in patients 60 years old or older during the 2015/2016 influenza season. Vaccine. 2017;35:7331–7338. doi: 10.1016/j.vaccine.2017.10.100. [DOI] [PubMed] [Google Scholar]
- 13.Caspard H., Mallory R.M., Yu J., Ambrose C.S. Live-attenuated influenza vaccine effectiveness in children from 2009 to 2015–2016: a systematic review and meta-analysis. Open Forum Infect Dis. 2017;4:ofx111. doi: 10.1093/ofid/ofx111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brooks W.A., Zaman K., Lewis K.D., Ortiz J.R., Goswami D., Feser J. Efficacy of a Russian-backbone live attenuated influenza vaccine among young children in Bangladesh: a randomised, double-blind, placebo-controlled trial. Lancet Glob Health. 2016;4:e946–e954. doi: 10.1016/S2214-109X(16)30200-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Victor J.C., Lewis K.D., Diallo A., Niang M.N., Diarra B., Dia N. Efficacy of a Russian-backbone live attenuated influenza vaccine among children in Senegal: a randomised, double-blind, placebo-controlled trial. Lancet Glob Health. 2016;4:e955–e965. doi: 10.1016/S2214-109X(16)30201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ambrose Christopher S, Bright Helen, Mallory Raburn. Letter to the editor: Potential causes of the decreased effectiveness of the influenza A(H1N1)pdm09 strain in live attenuated influenza vaccines. Euro Surveill. 2016;21(45) doi: 10.2807/1560-7917.ES.2016.21.45.30394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caspard H., Coelingh K.L., Mallory R.M., Ambrose C.S. Association of vaccine handling conditions with effectiveness of live attenuated influenza vaccine against H1N1pdm09 viruses in the United States. Vaccine. 2016;34:5066–5072. doi: 10.1016/j.vaccine.2016.08.079. [DOI] [PubMed] [Google Scholar]
- 18.Singanayagam A., Zambon M., Lalvani A., Barclay W. Urgent challenges in implementing live attenuated influenza vaccine. Lancet Infect Dis. 2017 doi: 10.1016/S1473-3099(17)30360-2. [DOI] [PubMed] [Google Scholar]
- 19.Recommended composition of influenza virus vaccines for use in the 2017 southern hemisphere influenza season. Wkly Epidemiol Rec. 2016;91:469–84. [PubMed]
- 20.Aleksandrova G.I. Use of the genetic recombination method for obtaining vaccinal strains of the influenza virus. Vopr Virusol. 1977;4:387–395. [PubMed] [Google Scholar]
- 21.Shcherbik S., Pearce N., Kiseleva I., Larionova N., Rudenko L., Xu X. Implementation of new approaches for generating conventional reassortants for live attenuated influenza vaccine based on Russian master donor viruses. J Virol Methods. 2016;227:33–39. doi: 10.1016/j.jviromet.2015.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ovsyannikova I.G., White S.J., Albrecht R.A., Garcia-Sastre A., Poland G.A. Turkey versus guinea pig red blood cells: hemagglutination differences alter hemagglutination inhibition responses against influenza A/H1N1. Viral Immunol. 2014;27:174–178. doi: 10.1089/vim.2013.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO . WHO Press; 2011. WHO Global Influenza Surveillance Network. Manual for the laboratory diagnosis and virology surveillance of influenza. [Google Scholar]
- 24.Chen Z., Wang W., Zhou H., Suguitan A.L., Jr., Shambaugh C., Kim L. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J Virol. 2010;84:44–51. doi: 10.1128/JVI.02106-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicolson C., Harvey R., Johnson R., Guilfoyle K., Engelhardt O.G., Robertson J.S. An additional oligosaccharide moiety in the HA of a pandemic influenza H1N1 candidate vaccine virus confers increased antigen yield in eggs. Vaccine. 2012;30:745–751. doi: 10.1016/j.vaccine.2011.11.081. [DOI] [PubMed] [Google Scholar]
- 26.Robertson J.S., Nicolson C., Harvey R., Johnson R., Major D., Guilfoyle K. The development of vaccine viruses against pandemic A(H1N1) influenza. Vaccine. 2011;29:1836–1843. doi: 10.1016/j.vaccine.2010.12.044. [DOI] [PubMed] [Google Scholar]
- 27.Suptawiwat O., Jeamtua W., Boonarkart C., Kongchanagul A., Puthawathana P., Auewarakul P. Effects of the Q223R mutation in the hemagglutinin (HA) of egg-adapted pandemic 2009 (H1N1) influenza A virus on virus growth and binding of HA to human- and avian-type cell receptors. Acta Virol. 2013;57:333–338. [PubMed] [Google Scholar]
- 28.Raymond D.D., Stewart S.M., Lee J., Ferdman J., Bajic G., Do K.T. Influenza immunization elicits antibodies specific for an egg-adapted vaccine strain. Nat Med. 2016;22:1465–1469. doi: 10.1038/nm.4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stevens J., Blixt O., Glaser L., Taubenberger J.K., Palese P., Paulson J.C. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol. 2006;355:1143–1155. doi: 10.1016/j.jmb.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki Y., Ito T., Suzuki T., Holland R.E., Jr., Chambers T.M., Kiso M. Sialic acid species as a determinant of the host range of influenza A viruses. J Virol. 2000;74:11825–11831. doi: 10.1128/jvi.74.24.11825-11831.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carr C.M., Chaudhry C., Kim P.S. Influenza hemagglutinin is spring-loaded by a metastable native conformation. PNAS. 1997;94:14306–14313. doi: 10.1073/pnas.94.26.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cotter C.R., Jin H., Chen Z. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 2014;10:e1003831. doi: 10.1371/journal.ppat.1003831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Donnell C.D., Vogel L., Matsuoka Y., Jin H., Subbarao K. The matrix gene segment destabilizes the acid and thermal stability of the hemagglutinin of pandemic live attenuated influenza virus vaccines. J Virol. 2014;88:12374–12384. doi: 10.1128/JVI.01107-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wen F., Li L., Zhao N., Chiang M.J., Xie H., Cooley J. H1N1 influenza A virus in cells. J Virol. 2009;2018:92. doi: 10.1128/JVI.01621-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sieczkarski S.B., Whittaker G.R. Differential requirements of Rab5 and Rab7 for endocytosis of influenza and other enveloped viruses. Traffic. 2003;4:333–343. doi: 10.1034/j.1600-0854.2003.00090.x. [DOI] [PubMed] [Google Scholar]
- 36.Byrd-Leotis L., Jia N., Dutta S., Trost J.F., Gao C., Cummings S.F. Influenza binds phosphorylated glycans from human lung. Sci Adv. 2019;5:eaav2554. doi: 10.1126/sciadv.aav2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koel B.F., Burke D.F., Bestebroer T.M., van der Vliet S., Zondag G.C., Vervaet G. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science. 2013;342:976–979. doi: 10.1126/science.1244730. [DOI] [PubMed] [Google Scholar]
- 38.Wang L., Cummings R.D., Smith D.F., Huflejt M., Campbell C.T., Gildersleeve J.C. Cross-platform comparison of glycan microarray formats. Glycobiology. 2014;24:507–517. doi: 10.1093/glycob/cwu019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geisler C., Jarvis D.L. Effective glycoanalysis with Maackia amurensis lectins requires a clear understanding of their binding specificities. Glycobiology. 2011;21:988–993. doi: 10.1093/glycob/cwr080. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.