Highlights
-
•
Demographic/social factors, vaccine beliefs, and vaccination status were captured.
-
•
Most parents are supportive of vaccination.
-
•
Many parents incorrectly reported their child as fully vaccinated.
-
•
Incomplete vaccination was associated with demographic and socio-economic factors.
Keywords: Childhood vaccination, Vaccine status, Attitudes, Beliefs, Risk-factors
Abstract
Background and aims
We aimed to understand the risk factors associated with incomplete vaccination, which may help to identify and prioritise opportunities to intervene.
Methods
Consenting parents of children <6 years old attending an outpatient clinic completed a questionnaire, which captured demographic information and their level of agreement with belief statements about vaccination using a 7-point Likert scale. Vaccination status was determined from the Australian Childhood Immunisation Register and deemed either “complete” (no doses overdue) or “incomplete” (1 or more doses overdue) at the time of questionnaire completion.
Results
Of 589 children of respondents, 116 (20%) had an incomplete vaccination status. Of these, nearly two-thirds (63%) of parents believed that their child was, in fact, fully-vaccinated. Compared to those with a complete vaccine status, children with an incomplete vaccine status were more likely to be born overseas (p < 0.001), have a larger family size (p = 0.02) and to have parents with lower educational attainment (p = 0.001). Parents of children with an incomplete status reported more doubt about the importance of vaccination and greater concern about vaccine safety, compared to parents of children with a complete status.
Conclusion
Most parents are supportive of vaccination. Sociodemographic factors may contribute more to the risk of incomplete vaccination than attitudes or beliefs. Some parents are unaware of their child’s vaccination status, suggesting that simple and modern reminders may assist parents to keep up to date.
1. Introduction
Many Australian children are not up to date with vaccines recommended by the National Immunisation Program schedule. In the state of Western Australia, the proportion of children reported as fully-vaccinated on the Australian Childhood Immunisation Register (ACIR) at 12–15 months old (93.6%) and at 60–63 months old (92.5%) are the lowest of any Australian jurisdiction [1].
An understanding of the modifiable factors contributing to incomplete vaccination may help inform strategies to improve vaccine coverage [2]. Previous studies have identified determinants of incomplete vaccination in international contexts; these are variable across settings and include sociodemographic factors and parental beliefs and attitudes. For example, high socio-economic status is associated with high vaccine coverage in some settings but is a risk factor for incomplete vaccination in others [3]. Large family size (e.g. ≥4 children) has been identified as a risk factor for incomplete vaccination in studies conducted in the United States [4], [5]. The influence of beliefs and attitudes have been examined among populations with vaccine hesitancy and reduced vaccine uptake; concerns about the adequacy of vaccine safety testing, side-effects and efficacy are more prevalent in these populations compared to pro-vaccine or fully-vaccinated populations [3], [6], [7].
Data on risk factors for incomplete vaccination specific to the Australian context are limited. A recent analysis from the Longitudinal Survey of Australian Children found that poor timeliness of vaccination was associated with low socio-economic factors [8]. However, this study was based on data collected in 2003-4. Another recent study obtaining prospective coverage focused on hesitancy and decision-related variables [9].
We aimed to identify sociodemographic and belief risk factors for incomplete vaccination in Perth, Western Australia (WA) by surveying parents of young children attending outpatient clinics at the state’s only tertiary children’s hospital.
2. Materials and methods
Parents or guardians of children younger than 6 years old attending outpatient clinics at Princess Margaret Hospital in Perth, WA, were invited to participate in a survey of beliefs concerning vaccination from August 2014 to May 2015. Parents/guardians were ineligible to participate if they normally resided outside of WA or if they lacked verbal and/or written English competency.
With informed parental consent, the child’s demographic and relevant clinical history was obtained from paper and electronic health records, including vaccination status. Parents also responded to a written questionnaire that gathered their own demographic data, explored their attitudes and beliefs towards vaccination and vaccine-preventable diseases, perceived barriers to vaccination, and opinions on potential strategies to increase vaccine coverage. Paper questionnaires were completed by parents while waiting for outpatient appointments in the presence of research staff but were given full privacy to enter responses. The questionnaire (see supplementary file Appendix A) was developed based on previously validated surveys, principally the national survey of attitudes towards childhood vaccination [10] and the 2012 New South Wales Population Health Survey [11]. Four principal domains were identified as being most relevant from these two surveys. These were perceived access to vaccination services, beliefs about the necessity of vaccination, beliefs about vaccine safety, and parental perception about availability and quality of information on vaccination. Pilot questions addressing each of these domains were selected, with a focus on questions assessing factors that might be addressed by real world interventions.
The pilot questionnaire was assessed for content validity by independent experts in the field of vaccination, vaccine uptake and public health. Face and internal validity of the pilot questionnaire was tested on a convenience sample of community representatives, stakeholders and parents of young children. Answers to questions pertaining to the same construct were assessed for correlation of within person answers. The questionnaire was finalised based on these pilot data, with at least three questions from each domain included, and with the aim of a questionnaire completion time of 10–15 min.
Parental attitudes and beliefs were measured using a 7-point Likert scale from ‘Strongly Disagree’ to ‘Strongly Agree’. Vaccination status was verified using the Australian Childhood Immunisation Register, a comprehensive population-based register of all childhood immunisations delivered under the National Immunisation Program (NIP). The register is electronically populated by vaccine providers who record for each child the date and vaccine type of any NIP vaccine delivered. All NIP vaccines are delivered at approximately 2, 4, 6, 12, and 18 months with a preschool booster at 4 years old. All NIP vaccines are delivered without cost, and at the time of the survey some tax benefits were contingent on dependent children being fully-vaccinated according to the register unless a parent was formally registered as conscientious objector; so, there was an incentive for parents to ensure their child’s vaccinations were up to date and recorded. Additional information about the register and NIP can be found in the supplementary file (Appendix B).
2.1. Statistical analysis
Children were categorised as either having a complete or incomplete vaccination status based on whether children had received all eligible vaccine doses on the day of survey participation, allowing no grace period but ignoring rotavirus and birth-dose hepatitis B vaccine status which are not eligible for catch-up vaccination. Survey responses among parents of children with complete vaccination were compared to parents of children with an incomplete status using Fisher’s exact test for categorical variables, and either the two-sample t-test or exact Wilcoxon Rank Sum test for continuous variables with symmetric and asymmetric distributions, respectively.
Determinants of incomplete vaccination status were analysed using multivariable logistic regression, including the reported beliefs and demographic variables of survey participants and their child’s demographic variables as explanatory variables. Graphical visualisation tools and backwards stepwise elimination were used to select the most parsimonious multivariable model. The odds ratios of incomplete vaccination status and associated 95% confidence intervals were estimated. A sensitivity analysis was performed using multiple imputation to account for missing questionnaire data; based on ten imputed datasets using the bootstrap EM algorithm (without priors) on incomplete data, where minimum and maximum chain lengths were restricted to 500.
Data were manually entered from paper questionnaires into a custom electronic database, and full quality-assurance procedures were undertaken to ensure the integrity and accuracy of the data. Sensitive patient data was anonymised prior to statistical analysis. Analysis was performed in R (Version 3.3.0, 2016-05-03). The study and questionnaire were approved by the Princess Margaret Hospital Human Research Ethics Committee (Ref: 2013115EP).
3. Results
A total of 857 parents were approached to participate in the survey. Of these, 125 parents declined to participate and 137 parents were ineligible. There were 595 questionnaire respondents, of whom 589 (99%) were included in the analysis; six were excluded as the age of the child was ≥ 6 years old or was not given. Survey respondents were predominantly women (90%; 530/589) and aged between 20 and 67 years (Mean(SD): 33.4 (6.5) years); their children were aged between 2 months and 6.8 years (Mean(SD): 2.4 (1.7) years). Evidence of complete vaccination was identified from the register for 473 children (80%); the remaining 116 respondents (20%) had children with an incomplete vaccination status. This included 13 children who were completely absent from the register and a further seven who appeared on the register but without documentation of any vaccine receipt. Respondent and child demographics are summarised in Table 1.
Table 1.
Survey respondent and child demographics.
| Total n = 589 |
Complete vaccination n = 473 |
Incomplete vaccination n = 116 |
P-value | |
|---|---|---|---|---|
| Sex of parent (female) | 378/420 (90%) Not recorded = 169 |
303/340 (89%) | 75/80 (94%) | 0.3 |
| Age of parent (years): Mean (SD) | 33.4 (6.5) Not recorded = 185 |
33.4 (6.7) Not recorded = 152 |
33.3 (6.1) Not recorded = 33 |
0.97 |
| Age of child (years): Mean (SD) | 2.4 (1.7) Not recorded = 0 |
2.4 (1.7) | 2.45 (1.6) | 0.79 |
| Child born overseas | 24/508 (5%) Not recorded = 81 |
12/408 (3%) | 12/100 (12%) | <0.001 |
| Children in household (≤4) | 469/482 (97%) Not recorded = 107 |
382/389 (98%) | 87/93 (94%) | 0.02 |
| Public transport use for vaccination appointments | 14/475 (3%) Not recorded = 114* |
7/386 (2%) | 7/89 (8%) | 0.007 |
| Highest education level of parent (<Year 10 high school) | 43/490 (9%) Not recorded = 99 |
24/393 (6%) | 19/97 (20%) | 0.001 |
| Healthcare professional advised parent to not vaccinate child (Yes) | 43/501 (9%) Not recorded = 88 |
24/405 (6%) | 19/96 (20%) | <0.001 |
Includes at least 9 respondents for whom there were no previous vaccination visits.
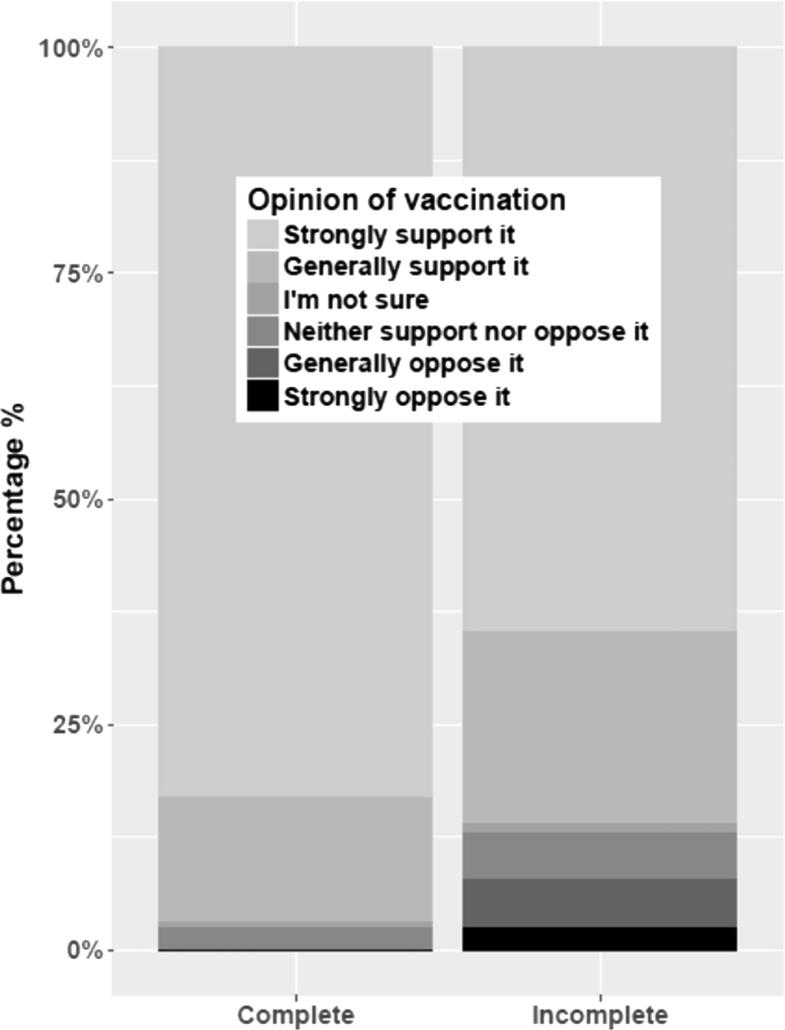
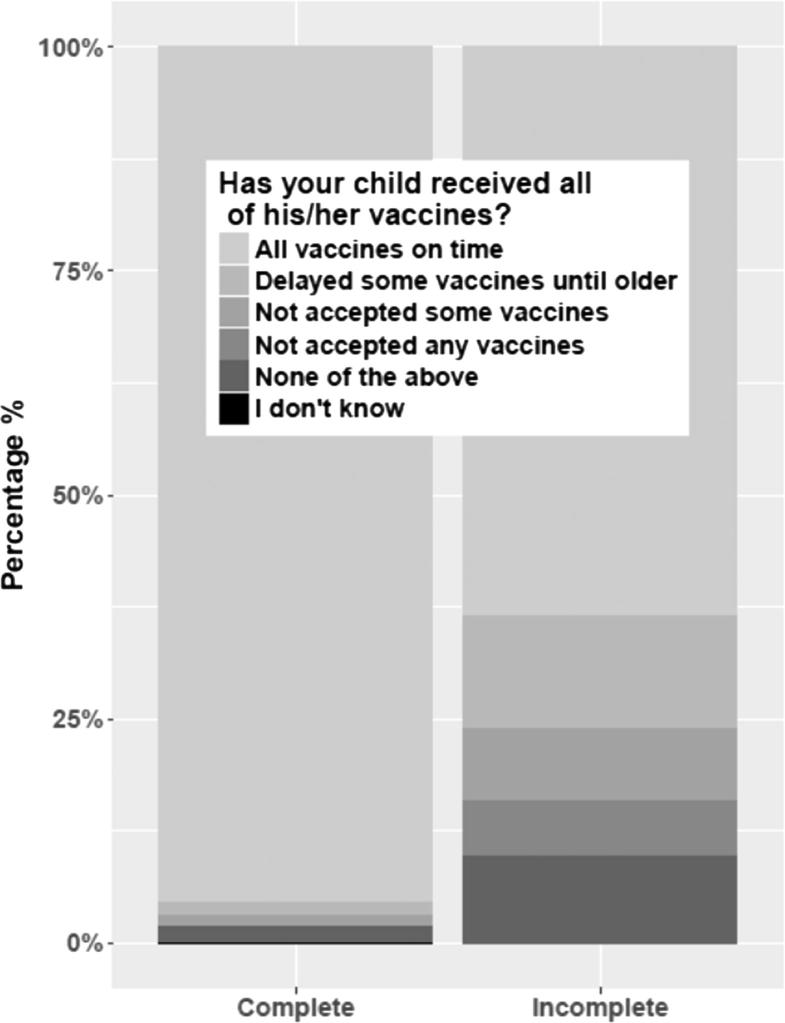
Irrespective of vaccination status, most parents were strongly or generally supportive of vaccination (97% versus 86% of parents with children who had complete and incomplete vaccination, respectively). Parents of children with incomplete vaccination were less likely to report strong support for vaccination (65% compared to 83% for parents of children with complete vaccination, p < 0.001) (Fig. 1). Among parents of children with complete vaccination, 95% reported that their child had received all vaccines on time compared to 63% of parents of children with incomplete vaccination (p < 0.001) (Fig. 2). Response proportions for opinion and parent-reported vaccination status and other explored variables that were not found to be important can be accessed in the supplementary file Appendix C.
Fig. 1.
Parental opinion of vaccination according to child vaccination status.
Fig. 2.
Parent-reported vaccination status in children with complete and incomplete vaccination.
In univariate analyses, small differences in vaccine beliefs were detected between parents with children who had complete and incomplete vaccination. Parents of children with incomplete vaccination were more likely to report concerns that vaccines were ‘unsafe’ (p = 0.03), ‘inadequately tested’ (p = 0.007), ‘too numerous in the current schedule’ (p = 0.03) and ‘too many being added’ (p = 0.009) compared to parents of fully-vaccinated children. They were also more likely to report doubts that vaccines were important (p = 0.02), a belief that vaccines ‘weaken the immune system’ (p = 0.006), and that vaccines do not protect their child (p = 0.02) or their community (p = 0.02). Compared to parents of children with complete vaccination, parents of children with an incomplete status reported less confidence in the information about vaccines that they received from their medical professional (p = 0.04) and a belief that government payments are a strong incentive for parents to complete vaccination (p = 0.02). However, these associations between participant beliefs and the completeness of their child’s vaccine status were no longer apparent in the multivariable analysis after adjusting for parental education, family size, use of public transport, overseas birth and recommendation for delayed or non-vaccination by a healthcare professional.
Irrespective of their child’s recorded vaccination status, most parents reported attending a general practice for previous vaccinations (71%; 335/474), and receiving information about vaccines from their general practitioner (91%) or nurse (53%). Compared to parents of children with complete vaccination, parents of children with incomplete vaccination were more likely to report their child as born overseas (OR: 3.52, 95% CI: 1.54 to 8.05), to report receiving a recommendation from a healthcare professional to delay or not complete vaccination (OR: 4.25, 95% CI: 2.07 to 8.69), to report non-completion of high school (OR: 2.92, 95% CI: 1.34 to 6.39 compared to university-level education), to report use of public transport for attending their child’s previous vaccination appointment (OR: 2.11, 95% CI: 0.78 to 5.71), and to report a larger family size (OR: 1.39 per one child increase in family size, 95% CI: 1.03 to 1.87), after imputation for missing values.
4. Discussion
Our study focused on a broad range of potential determinants of vaccination status, noting recent analyses that suggests a range of factors influencing uptake [12]. This study was also informed by the Health Belief Model [13] which theorises that sociodemographic factors, perceived risk of vaccine preventable diseases, benefits and risks of vaccination, and trustworthiness of medical providers, might all influence vaccine behaviour [6]. We found that most parents express support for vaccination irrespective of whether their children have complete or incomplete vaccination. This is consistent with previous studies, which suggest that only a small minority of Australian parents harbour strong objections to vaccination [10], [12]. In our sample, while parents of children with incomplete vaccination were less likely to express strong support for vaccination than those of children with complete vaccination, overall differences in beliefs and attitudes were small and no longer apparent after adjusting for differences in demographic factors.
Some identified risk factors for incomplete vaccination suggest that sociodemographic factors may be more important determinants of vaccine completeness than beliefs or attitudes. Reliance on public rather than private transport to attend for healthcare and low parent educational attainment, for example, are more likely to occur among low income groups in our setting. Large family size was also identified as a risk factor, which has been found in other studies [8], [14], [15], [16]. This is likely related to a higher parent workload in larger families or that vaccination timeliness reduces for high birth-order children.
We noted a marked discrepancy between parent-reported vaccination status and the recorded vaccination status on the immunisation register; more than half of parents who had children with incomplete vaccine records reported their child as up-to-date and on time with vaccinations. This suggests that many parents are unaware of their child’s true vaccination status, or that the national immunisation register is not always an accurate record of vaccination status. The latter may be particularly true for the minority of children born overseas who were over-represented among the group with incomplete vaccination and for whom prior vaccination records may not have been transferred to the register. We considered a child incompletely vaccinated if any eligible doses were due or overdue at the time of the survey, without allowing for any grace period. We note that because we sampled parents of children of all ages up to 6 years, there were few children sampled who were within 1 month of a vaccine due date, so allowing for a grace period of 1 month is unlikely to have materially affected the results.
Compared to the general population, our sample may under-represent parents of children of high socio-economic status, who may be more likely to access private rather than public health services. Our sample may also under-represent fathers, parents of ethnic backgrounds due to exclusion because of English language barriers, and/or parents with strong objections to vaccination who may have declined to participate due to their beliefs. Although respondents were informed their answers would be confidential and would not affect medical care, respondents were not anonymous to the research team member administrating the survey and they may therefore have been reluctant to disclose beliefs perceived to be undesirable. While the immunisation schedule is largely consistent across Australian jurisdictions, there are some differences in the implementation, particularly with respect to the proportion of vaccines delivered in primary care practices versus dedicated immunisation clinics; risk factors for incomplete vaccination might therefore vary across jurisdictions.
It is possible that enrolment of survey respondents from a hospital setting may have resulted in over-representation of children not up-to-date with vaccination due to recurrent sickness, or due to actual or misperceived contraindications to vaccination. We tried to minimise this bias by targeting general medical and surgical clinics rather than clinics for children with cancer, immunodeficiency, or other established contra-indications to vaccination. While some parents reported that their healthcare professional advised them to delay or not complete their child’s vaccines, this information could not be verified. We note that true medical contraindications to routine immunisation (e.g. severe immunodeficiency or allergy to vaccine components) are very rare.
Lastly, a limitation of our statistical analysis is that it assumes that the studied factors apply any influence directly on vaccination status. It is more likely that some factors act indirectly. For example, it is not possible to know how the observed sociodemographic risk factors might impart their influence on vaccination status; our multivariable analysis suggests these do not act via differences in beliefs and attitudes toward vaccination, although this cannot be excluded. Analytic methods which explore causal pathways rather than simple associations might help determine which factors are the most influential drivers of vaccination, and therefore, those which could be targeted for intervention.
5. Conclusion
We found that sociodemographic factors appeared to have greater independent influence on the vaccination status of young children than parental beliefs and attitudes toward vaccination in this sample. Even among parents of children with incomplete vaccination, most expressed general or strong support. While concerns about vaccination were more common in the incomplete vaccination group, these differences were relatively small and were no longer apparent after adjusting for differences in demographic factors. As such, campaigns promoting the importance of vaccination might do little to improve the completeness and timeliness of vaccination in our setting, although enhanced motivation (demand) may nonetheless assist by helping to overcome practical barriers. The fact that more than half of parents of children with incomplete vaccination reported that their child was up-to-date suggest that alternative strategies, such as implementation of vaccine text message reminders, may have greater impact in the short term.
Acknowledgments
Acknowledgements
The authors would like to thank all parents who participated, and Harold Willaby for his advice on developing the study questionnaire.
Funding
Funding was received from the WA Department of Health.
Declaration of interest
The authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jvacx.2019.100010.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Commonwealth of Australia. Immunise - Australian Immunisation Registry - Current Data. 2018 (updated 03/18; cited 1/06/18). Available from: https://health.gov.au/topics/immunisation/childhood-immunisation-coverage-in-australia/current-data-all-children.
- 2.Cooper Robbins S.C., Leask J., Booy R. Parents' attitudes towards the influenza vaccine and influencing factors. J Paediatr Child Health. 2011;47:419–422. doi: 10.1111/j.1440-1754.2010.01993.x. [DOI] [PubMed] [Google Scholar]
- 3.Prislin R., Dyer J.A., Blakely C.H., Johnson C.D. Immunization status and sociodemographic characteristics: the mediating role of beliefs, attitudes, and perceived control. Am J Public Health. 1998;88:1821–1826. doi: 10.2105/ajph.88.12.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dombkowski K.J., Lantz P.M., Freed G.L. Risk factors for delay in age-appropriate vaccination. Public Health Rep. 2004;119:144–155. doi: 10.1177/003335490411900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gust D., Strine T.W., Maurice E., Smith P., Yusuf H. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–e22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 6.Smith P.J., Humiston S.G., Marcuse E.K., Zhao Z., Dorell C.G., Howes C. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheeler M., Buttenheim A.M. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vacc Immunotherap. 2013;9:1782–1789. doi: 10.4161/hv.25959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Homel J., Edwards B. Factors associated with delayed infant immunization in a nationally representative cohort study. Child Care Health Dev. 2018;44:583–591. doi: 10.1111/cch.12560. [DOI] [PubMed] [Google Scholar]
- 9.Corben P., Leask J. Vaccination hesitancy in the antenatal period: a cross-sectional survey. BMC Public Health. 2018;18:566. doi: 10.1186/s12889-018-5389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chow M., Danchin M., Willaby H.W., Pemberton S., Leask J. Parental attitudes, beliefs, behaviours and concerns towards childhood vaccinations in Australia: A national online survey. Aust Fam Physician. 2017;46:145–151. [PubMed] [Google Scholar]
- 11.Centre for Epidemiology and Evidence, NSW Ministry of Health. New South Wales Population Health Survey: 2012 Questionnaire. Available from: http://www.health.nsw.gov.au/surveys/Documents/Questionnaire-2012.pdf [cited 1/08/18].
- 12.Beard F., Hull B., Leask J., Dey A., McIntyre P. Trends and patterns in vaccination objection, Australia, 2002–2013. Med J Aust. 2016;204:275. doi: 10.5694/mja15.01226. [DOI] [PubMed] [Google Scholar]
- 13.Becker M. The health belief model and personal health behavior. Health Edu Monogr. 1974;2:324–508. [Google Scholar]
- 14.Bond L., Nolan T., Lester R. Immunisation uptake, services required and government incentives for users of formal day care. Aust NZ J Public Health. 1999;23:368–376. doi: 10.1111/j.1467-842x.1999.tb01277.x. [DOI] [PubMed] [Google Scholar]
- 15.Pearce A., Marshall H., Bedford H., Lynch J. Barriers to childhood immunisation: Findings from the Longitudinal Study of Australian Children. Vaccine. 2015;33(29):3377–3383. doi: 10.1016/j.vaccine.2015.04.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haynes K., Stone C. Predictors of incomplete immunisation in Victorian children. Aust NZ J Public Health. 2003;28:72–79. doi: 10.1111/j.1467-842x.2004.tb00636.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.