Abstract
Background:
Pregnancy in a woman's life is associated with many physiological changes in the body due to alterations in the hormone levels. These altered hormonal levels are associated with many systemic diseases. The incidence of oral diseases in general and periodontal diseases in particular are higher in pregnant women, with gingivitis and periodontitis being the most common. Furthermore, it has been evidenced in literature that periodontal diseases are associated with adverse pregnancy outcomes such as preterm low birth weight and preeclampsia.
Aims and Objectives:
The aim of this study was to evaluate the oral health knowledge among pregnant women visiting and not visiting a dental professional.
Materials and Methods:
The study was a survey-based one with a sample size of 260. The study population was divided into two groups based on their visits to a dentist. A questionnaire comprising 20 questions has been used to assess their awareness and attitude towards oral health.
Results:
The awareness regarding oral health and association with adverse pregnancy outcomes among the study population was very low, irrespective of their dental visit. Furthermore, majority of the study population in neither of the groups were aware that dental treatment was safe during pregnancy.
Conclusion:
The results of the study clearly reflected that the awareness levels among the pregnant women regarding this association were low. Hence, more collective efforts are required from dental and medical professionals to improve the oral and periodontal health outcomes during pregnancy.
Keywords: Estrogen, periodontal diseases, pregnancy, preterm low birth weight, progesterone
INTRODUCTION
Health of the oral cavity is an essential and integral part of general health, which can be substantiated with the statement that oral cavity should be considered as a “window” through which external microorganisms interact with the host.1 In recent ages, it has been well documented that an impact of various systemic diseases exhibit their effect on the oral health of an individual.2 Furthermore, a strong association was evidenced in the literature with regard to periodontal diseases and systemic conditions such as cardiovascular diseases, diabetes, and preterm low birth weight.3
Pregnancy, a dynamic and most important phase, in a woman's life is markedly characterized by altered hormonal levels of estrogen and progesterone, which was associated with significant oral changes.4 High hormone levels during this period are known to increase the incidence of diseases, such as gestational diabetes, hypertension, preeclampsia, and periodontitis.
Among the various oral diseases associated with pregnant patients, periodontal diseases have the most common occurrence, and the prevalence rate of periodontal diseases ranges from 30% to 100%.5,6 Periodontal diseases are inflammatory conditions associated with destruction of supporting structures, resulting in bone and attachment loss which might be as a result of hormonal changes altering the vascular supply and tissue response of the host.7 High hormone levels when accompanied with periodontal diseases are known to cause many adverse pregnancy outcomes, such as preterm birth, low birth weight, and preeclampsia.8 These are the major causes of maternal morbidity and mortality.9,10 These adverse outcomes can be successfully prevented by maintaining proper oral hygiene, and hence, maintenance of proper oral health during pregnancy plays a key role in the health of pregnant women.
Oral health can be achieved by personal oral hygiene maintenance and regular visits to a dentist. Even though awareness of patients regarding oral diseases has increased in the present scenario, awareness regarding periodontal diseases among the pregnant women is not up to the expected level.11 Periodic visits to a dentist can help in diagnosing many of the oral diseases such as caries, periodontitis, and malocclusion, which when detected early can be treated with better prognosis.12 Intervention of a disease at appropriate time can prevent adverse outcomes such as loss of tooth which greatly affects the social, psychological, and physical aspects of a patient. Furthermore, these visits are more so important during sensitive periods such as pregnancy and lactation as the health of both mother and child are at risk, and simple basic preventive procedures can prevent the occurrence of any of these adverse outcomes. These visits also increase the awareness regarding oral diseases and their prevention which reinforces positive attitude among the individuals.13
Although there are many studies regarding the awareness about the importance of oral health among the pregnant women, no studies in the literature have assessed the awareness levels based on dental visits. Hence, this study aims to assess the oral health knowledge among pregnant women based on their visit to a dentist.
MATERIALS AND METHODS
As a dire need exists among the dental professionals to have sufficient knowledge on the association of altered hormonal levels during pregnancy and periodontitis, the concerned medical specialists such as gynecologists should also be emphasized on their role regarding the issue. Hence, the present study was a questionnaire-based survey which was designed to assess the awareness and attitude towards oral health among pregnant women attending the gynecology hospitals in and around Bimavaram from March to August 2018. The sample size was set to be 260 using descriptive analysis.
The inclusion criteria were pregnant women attending hospitals for their routine checkup. The exclusion criteria were nonpregnant women and women who did not provide consent. In this study, the population was divided into two groups based on their visit to dentist. Group A consisted of 130 individuals who visited a dentist, and Group B consisted of 130 subjects who never visited a dentist in their lifetime. The questionnaire was verbally explained to the participants, and their answers for the questions were recorded manually.
The individuals were informed regarding the purpose of the study, and information was collected only from those who gave consent. Ethical clearance was obtained from the Ethical Committee of Vishnu Dental College, Bhimavaram.
A self-based validated questionnaire comprising 22 questions was used in our study. The questionnaire comprised three sections, wherein the first part was designed to record the sociodemographic data such as patients’ name, age, occupation, and address. The second section was designed to assess their knowledge regarding the awareness levels about the relationship between periodontal health and maternal health. The third part aimed to assess the attitude of patients towards oral health with questions such as their last dental visit, their perception towards oral hygiene, dental visits, and dental treatment during pregnancy.
RESULTS
In this study, most of the participants were under the age groups of 17–25 years and were divided into two groups based on their visits to a dentist atleast once in their lifetime.
The results of the study were subjected to descriptive analysis. When questioned regarding the importance of mouth rinsing and brushing, 93.3% of Group A and 90.7% of Group B individuals responded that they were aware of the importance of oral hygiene measures in maintaining oral health. Moreover, 100% of the study population in both the groups was well acquainted with the safe usage of medication during pregnancy.
There was an indisputable agreement among all the study participants (100%) that oral health is an integral and important part of general health. It was observed that 76.5% of Group A and 84.5% of Group B individuals were of the opinion that dental treatment is not safe during pregnancy [Figures 1 and 2]. Among the participants, 48.2% and 51.8% of the respective groups felt that dental treatment is contraindicated during pregnancy.
Figure 1.
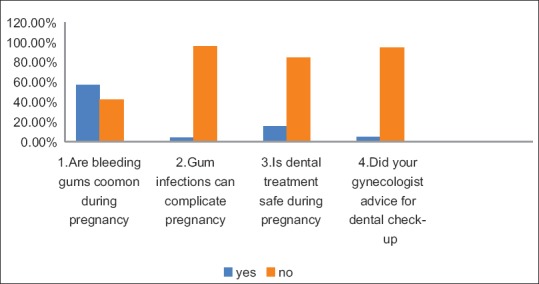
Women who visited a dental professional
Figure 2.
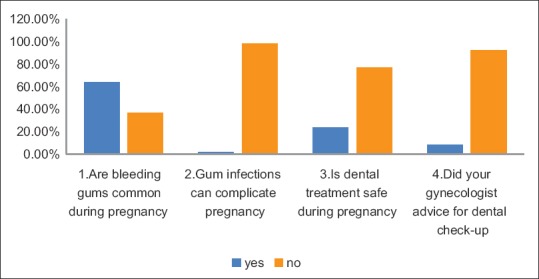
Women who never visited a dental professional
Among the study participants, only 3.96% of Group A and 1.93% of Group B were aware about the association between periodontal diseases and adverse pregnancy outcomes such as preterm low birth weight. When these individuals were questioned regarding advice from a gynecologist for a dental checkup, only 7.97% and 4.92% of the respective groups responded positively.
It can be observed from the results that 57.4% of Group A and 63.6% of Group B individuals responded that red bleeding gums were a common finding during pregnancy. Furthermore, when the study participants were asked about their opinion on changes in periodontal tissues, 50% and 59.7% of both the groups responded that the changes disappear after childbirth.
DISCUSSION
When individuals were questioned regarding the safety of drug usage during pregnancy, the results showed a positive response among the participants and these results were similar to a study done by Noha, wherein 760 pregnant women were analyzed for safety usage of drugs and most of the participants responded positively.14 It can also be observed in our results that all the participants (100%) were aware regarding the importance of oral hygiene. This showed that irrespective of a dental visit, most of the study population was well aware of the importance of basic oral hygiene measures in maintaining good oral health.
On the other hand, all the study participants (100%) in both the groups were aware of the importance of the oral health in overall general health during pregnancy. The results were comparable to a study by Sajjan et al., in which 81.50% of the study individuals felt that importance should be given for oral health as a part of general health during pregnancy.15
When individuals were assessed regarding their knowledge about the association between periodontal disease and adverse pregnancy outcomes, only very few individuals (3.96% and 1.93%) in both groups responded positively. When a similar kind of study was conducted by Boggess et al. on 599 individuals, the results showed that pregnant women have little knowledge on oral health association with pregnancy, which varied according to maternal race or ethnicity.16 A study done by Gupta et al. stated that the level of awareness is very low (60%) irrespective of education and age.17 Another study done by Nagi et al. showed similar results, wherein 75% of the individuals had no knowledge regarding the periodontal complications.18
On the other hand, very few individuals (7.97% and 4.92%) in the respective groups were advised for a dental checkup. These inferences were comparable to a study reported by Rogers, wherein it was concluded that only 25% of the patients had received advice from the gynecologist concerning dental visit.19,20 It can be understood from the above findings that gynecologists are unaware of the consequences such as premature delivery, preterm low birth weight, and preeclampsia due to periodontal diseases. It clearly reflected that although there is substantial evidence regarding the association of periodontal diseases and adverse pregnancy outcomes, the awareness levels among the population and gynecologists are low.
More than half of the participants in either of the groups felt that treatment should not be done during pregnancy, which clearly reflected the lack of awareness regarding the safety of dental treatment which happened to be the cause for many people not coming forward for dental treatment.
It was observed in our study that most of the individuals stated that it is normal to experience bleeding gums during pregnancy. Moreover, majority of the participants felt that the changes occurring in gums during pregnancy would subside by itself after delivery. These negative attitudes of the participants indicated that knowledge and practices of pregnant women towards oral health need to be greatly improved. Expecting mothers should be instructed regarding the self-care practices and educated about the importance of periodontal health. Thus, at this point, it can be emphasized that gynecologists play a role in identifying the oral changes at an early stage, thereby helping a dental professional in preventing adverse pregnancy outcomes.
However, this study is not without limitations. The major imitation is the self-reported data, which can always be biased. Furthermore, parameters such as education and social status may influence and alter the results. However, this study strongly supports the existing evidence on the lack of awareness among pregnant women regarding the importance of oral health. Hence, more coordinated efforts from dentists and gynecologists are required for ensuring maternal health and a safe pregnancy.
CONCLUSION
As gynecologists are the frontiers in treating female section of the society, their knowledge towards overall oral health in general and periodontal health in particular is pivotal in providing better pregnancy outcomes. Hence, gynecologists should play a pivotal role in referring pregnant patients to visit a dental professional. In this way, they can be facilitators in improving the awareness among pregnant females, thereby ensuring a total safe and healthy pregnancy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kane SF. The effects of oral health on systemic health. Gen Dent. 2017;65:30–4. [PubMed] [Google Scholar]
- 2.Nagpal R, Yamashiro Y, Izumi Y. The two-way association of periodontal infection with systemic disorders: An overview. Mediators Inflamm. 2015;2015:793898. doi: 10.1155/2015/793898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Umeizudike KA, Iwuala SO, Ozoh OB, Ayanbadejo PO, Fasanmade OA. Association between periodontal diseases and systemic illnesses: A survey among internal medicine residents in Nigeria. Saudi Dent J. 2016;28:24–30. doi: 10.1016/j.sdentj.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R, Acharya AK. Oral health status and treatment needs among pregnant women of Raichur district, India: A population based cross-sectional study. Scientifica (Cairo) 2016;2016:9860387. doi: 10.1155/2016/9860387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasson E. Pregnancy gingivitis. Harefuah. 1960;58:224–6. [PubMed] [Google Scholar]
- 6.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 7.Ramamurthy J, Fathima I. Assessment of knowledge and awareness about periodontal oral health among pregnant women – A questionnaire study. Int J Curr Res Rev. 2017;9:9–12. [Google Scholar]
- 8.Offenbacher S, Katz V, Fertik G, Collins J, Boyd D, Maynor G, et al. Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol. 1996;67:1103–13. doi: 10.1902/jop.1996.67.10s.1103. [DOI] [PubMed] [Google Scholar]
- 9.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 10.Shennan AH. Recent developments in obstetrics. BMJ. 2003;327:604–8. doi: 10.1136/bmj.327.7415.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martelli ML, Brandi ML, Martelli M, Nobili P, Medico E, Martelli F. Periodontal disease and women's health. Curr Med Res Opin. 2017;33:1005–15. doi: 10.1080/03007995.2017.1297928. [DOI] [PubMed] [Google Scholar]
- 12.Singh S, Dagrus K, Kariya PB, Singh S, Darmina J, Hase P. Oral periodontal health knowledge and awareness among pregnant females in Bangalore, India. Int J Dent Med Res. 2015;1:7–10. [Google Scholar]
- 13.Thomson WM, Williams SM, Broadbent JM, Poulton R, Locker D. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89:307–11. doi: 10.1177/0022034509356779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaki NM, Albarraq AA. Use, attitudes and knowledge of medications among pregnant women: A Saudi study. Saudi Pharm J. 2014;22:419–28. doi: 10.1016/j.jsps.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sajjan P, Pattanshetti JI, Padmini C, Nagathan VM, Sajjanar M, Siddiqui T. Oral health related awareness and practices among pregnant women in Bagalkot district, Karnataka, India. J Int Oral Health. 2015;7:1–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Boggess KA, Urlaub DM, Moos MK, Polinkovsky M, El-Khorazaty J, Lorenz C. Knowledge and beliefs regarding oral health among pregnant women. J Am Dent Assoc. 2011;142:1275–82. doi: 10.14219/jada.archive.2011.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta S, Jain A, Mohan S, Bhaskar N, Walia PK. Comparative evaluation of oral health knowledge, practices and attitude of pregnant and non-pregnant women, and their awareness regarding adverse pregnancy outcomes. J Clin Diagn Res. 2015;9:ZC26–32. doi: 10.7860/JCDR/2015/13819.6756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagi R, Sahu S, Nagaraju R. Oral health, nutritional knowledge, and practices among pregnant women and their awareness relating to adverse pregnancy outcomes. J Indian Acad Oral Med Radiol. 2016;28:396–402. [Google Scholar]
- 19.Rogers SN. Dental attendance in a sample of pregnant women in Birmingham, UK. Community Dent Health. 1991;8:361–8. [PubMed] [Google Scholar]
- 20.Patil SN, Kalburgi NB, Koregol AC, Warad SB, Patil S, Ugale MS. Female sex hormones and periodontal health-awareness among gynecologists – A questionnaire survey. Saudi Dent J. 2012;24:99–104. doi: 10.1016/j.sdentj.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


