Abstract
Several companies in Japan introduced early working conditions (including recommendations on early morning work and prohibitions on nighttime overtime work) to decrease the number of long working hours at night. Nevertheless, individuals possess their own chronotype, i.e., their behavioral timing preference—be it morning or evening—that is associated with worker health.
The purpose of this study was to investigate the influence of chronotype and working conditions on sleep and health related quality of life (HRQOL) using 126 daytime office workers who were classified as morning or evening type by their Morningness-Eveningness Questionnaire scores. We then compared morning and evening type workers’ sleep variables (sleep onset/offset time and total sleep time), sleep quality (using the Japanese version of the Pittsburgh Sleep Quality Index), and HRQOL scores. Additionally, we compared the same sleep variables, sleep quality, and HRQOL scores of each chronotype category of worker under early and normal working conditions.
As the results, evening type workers had late sleep onset/offset time, poor sleep quality, and low HRQOL (role-social component) compared to morning type workers. Furthermore, the evening type workers under early working conditions had earlier sleep onset/offset time and poorer sleep quality compared to those workers under normal working conditions.
These results suggest that evening type workers in general have poor sleep and low HRQOL and those same workers under early working conditions, in particular, are associated with poor sleep quality. Therefore, in order to optimize worker health, we suggest that working conditions should be taken account of individual chronotypes.
Keywords: Chronotype, Working condition, Sleep, Health related quality of life, Workers
INTRODUCTION
Long working hours are wide spread in Japan. Unfortunately, this working style increases the risk of many health problems including stroke [11], coronary heart disease [26], depression [27], sleep problems [15], and poor Health-Related Quality of Life (HRQOL) [31]. To reduce the number of long working hours, several companies recently introduced early working conditions that set earlier work start times and reduced overtime work at night.
Although these working conditions were intended to benefit the overall well-being of workers, it is well known that every individual has a chronotype [12]. Chronotype refers to the individual preference of behavioral timing and biological characteristic in one’s circadian rhythm [19,30]. For example, morning type individuals prefer to sleep early and be active from early morning, while evening type individuals prefer to be active during the evening and go to sleep late at night, and typically have difficulty waking up early in the morning [32]. Chronotype is influenced by many biological factors, including circadian gene Period 3 [17,24], age, and gender [20]. Previous studies have reported that evening type individuals experience poor sleep quality [28,33,35] and are more vulnerable to metabolic disorders [34].
As mentioned above, several studies revealed an association between chronotype and health problems. However, no studies have investigated the influence of chronotype and working conditions, such as early working conditions and normal working conditions, on worker’s health. Thus, the first objective of this study was to compare morning and evening chronotype workers’ sleep status and HRQOL. The second objective of this study was to compare the sleep and HRQOL of morning and evening chronotype workers under both early and normal working conditions.
MATERIALS AND METHODS
Participants and study protocol
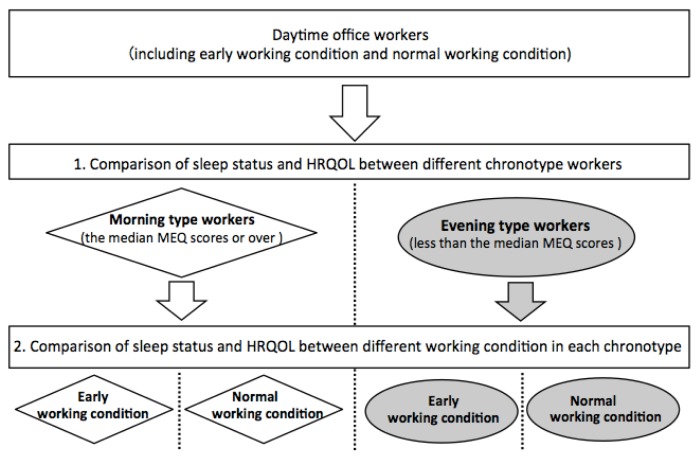
The 162 study participants were daytime office workers aged 22–54 years in different companies. These companies employed two different working conditions. One Company employed early working condition, and the other companies employed normal working condition. All participants worked five days a week—Monday to Friday. None of the participants were shift workers or physical laborers. The study was divided into two parts: first, we compared morning and evening chronotype workers’ sleep status (sleep variables and sleep quality) and HRQOL; second, we compared the sleep status and HRQOL of both morning and evening chronotype workers under the early working conditions and normal working conditions (Figure 1).
Figure 1.
The study design
First, we compared the sleep status (sleep variables and sleep quality) and HRQOL between morning and evening types. Second, we compared the sleep status and HRQOL between early working condition (the working style involved pre-determined working hours from 09:00 to 17:15 hrs, recommended early morning work from 05:00 to 08:00 hrs, and a prohibition of overtime work after 20:00 hrs) and normal working condition (the working style involved pre-determined working hours from 09:15 to 17:30 hrs, from 09:00 to 17:30 hrs or from 09:00 to 17:45 hrs and permitted overtime work after 20:00 hrs) in each chronotype.
MEQ, the Morningness-Eveningness Questionnaire; HRQOL, health related quality of life.
The first part of the study involved a cross sectional comparison of the morning and evening type groups. We determined the chronotype of all participants using the Morningness-Eveningness Questionnaire (MEQ), and categorized them into morning type (defined as the median MEQ scores or over) and evening type (defined as less than the median MEQ scores) individuals following the method of the previous study [14]. Then, we compared sleep variables between morning and evening type workers. Sleep variables included sleep onset/offset time and total sleep time. Moreover, we also compared subjective sleep quality and HRQOL of both the groups by using a subjective sleep questionnaire—the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J), and a HRQOL questionnaire—the Japanese MOS Short-Form 36-Item Health Survey ver2 (SF-36v2).
The second part of the study involved a cross sectional comparison of the impact of two conditions — early working conditions and normal working conditions — on each chronotype workers. The early working conditions involved pre-determined working hours from 09:00 to 17:15 hrs, recommended early morning work from 05:00 to 08:00 hrs, and a prohibition of overtime work after 20:00 hrs to decrease overtime work at night and long working hours. The normal working condition (i.e., the ordinary working style of many office workers) involved pre-determined working hours from 09:15 to 17:30 hrs, from 09:00 to 17:30 hrs or from 09:00 to 17:45 hrs and permitted overtime work after 20:00 hrs. These working conditions were already in place before we commenced our research regardless of the intension of the worker. We compared the sleep status and HRQOL of both the type of workers in early and normal working conditions using the above mentioned questionnaires.
The study protocol was in accordance with the guidelines of the Declaration of Helsinki and was reviewed and approved by the Ethics Committee of the Graduate School of Health Sciences at Kobe University. All participants gave their written informed consent after the study was explained to them.
Chronotype questionnaire
We used the Morningness-Eveningness Questionnaire (MEQ) to evaluate chronotype of participants [8,9]. The MEQ scores ranged from 16 to 86, where the higher scores are indicative of morning type and lower scores are indicative of evening type individuals.
Sleep variables and subjective sleep questionnaire
First, participants recorded their sleep onset/offset time and total sleep time for a month. In addition, the subjective sleep quality of the participants was evaluated via the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) [3,4,5].
The PSQI-J is commonly used to assess subjective sleep quality of healthy people and patients with various diseases. The sleep quality is evaluated comprehensively by asking questions related to sleep efficiency, daytime sleepiness, sleep duration, and other sleep statuses. The PSQI-J score ranged from 0 to 21, with the higher score representing lower sleep quality.
Health-related quality of life questionnaire
Participants also answered the Japanese MOS Short-Form 36-Item Health Survey ver2 (SF-36v2) to measure their HRQOL [6,7,29]. SF-36v2 is a self-administered questionnaire used to assess HRQOL for healthy people and various patients. In addition, three summary indices—the Physical component summary (PCS), the Mental component summary (MCS), and the Role-social component summary (RCS) [23]—can be calculated from eight subscales. Higher the score of a particular component, better is the HRQOL with regard to that component.
Statistical analysis
All data were expressed as mean ± standard deviation (SD) for normally distributed data or median (25–75 percentile) for non-normally distributed data. To compare all data, the two-sample t-test or Mann-Whitney U test was performed after the Shapiro-Wilk test. For gender, the χ2-test was used; p < 0.05 (two-sided) was accepted as statistically significant. All analyses were performed using the SPSS statistical software (SPSS2.0 for Windows; IBM Japan, Co. Ltd., Tokyo, Japan).
RESULTS
Our final sample included 126 participants, excluding those with data errors found in their questionnaires from 162 participants in this study. The median (25–75 percentile) age in these participants was 29.0 (26.0–36.0) years. This sample consisted of 65 men and 61 women. The median MEQ value was 53.0. We defined morning type as participants with MEQ scores ≥ 53.0 (n=69) and evening type as participants with MEQ scores < 53.0 (n=57). There were no significant differences in age and gender between morning and evening type individuals. The MEQ scores of evening type individuals were significantly lower than that of morning type individuals (evening type, 47.0 (42.0–50.0) vs. morning type, 57.0 (55.0–62.0), p < 0.001) (Table I).
Table I.
General characteristics.
| Morning type (n = 69) | Evening type (n = 57) | p - value | |
|---|---|---|---|
| Age (years)a) | 31.0 (27.0 – 37.0) | 29.0 (26.0 – 34.0) | 0.136 |
| Genger (Men/Women)b) | M41/W28 | M24/W33 | 0.053 |
| MEQ (scores)a) | 57.0 (55.0 – 62.0) | 47.0 (42.0 – 50.0) | < 0.001** |
All values expressed as median (25 – 75 percentile). ** p < 0.01 by using Mann-Whitney U testa) and χ2-testb). MEQ, the Morningness-Eveningness Questionnaire
Table II shows the comparison of sleep variables, sleep quality, and HRQOL between morning and evening type individuals. In sleep variables, the sleep onset/offset times were significantly later in the evening type compared to the morning type individuals (sleep onset time: evening type, 0:15 (0:00–1:00) hrs vs. morning type, 0:00 (23:00–0:10) hrs, p = 0.019; sleep offset time: evening type, 6:45 (6:20–7:00) hrs vs. morning type, 6:00 (5:30–6:30) hrs, p < 0.001). The PSQI-J score was significantly higher in evening type than in the morning type individuals (evening type, 6.0 (4.0–7.0) vs. morning type, 4.0 (3.0–6.0), p = 0.038). In the SF-36v2, the RCS scores of evening type individuals were significantly lower than those of morning type individuals (evening type, 48.3 (37.4–55.0) vs. morning type, 51.8 (45.6–56.6), p = 0.043). The other variables were not significantly different.
Table II.
Comparison of sleep status and health related quality of life between Morning and Evening type.
| Morning type (n = 69) | Evening type (n = 57) | p - value | |
|---|---|---|---|
| Sleep variables | |||
| Sleep onset time (h:mm)a) | 0:00 (23:30 – 0:10) | 0:15 (0:00 – 1:00) | 0.019* |
| Sleep offset time (h:mm)a) | 6:00 (5:30 – 6:30) | 6:45 (6:20 – 7:00) | < 0.001** |
| Total sleep time (h)a) | 6.5 (5.5 – 6.8) | 6.5 (6.0 – 7.0) | 0.135 |
| PSQI-J (scores)a) | 4.0 (3.0 – 6.0) | 6.0 (4.0 – 7.0) | 0.038* |
| SF-36v2 | |||
| PCS (scores)c) | 57.1 ± 6.4 | 57.6 ± 6.1 | 0.668 |
| MCS (scores)a) | 49.1 (45.5 – 54.1) | 49.6 (42.7 – 52.8) | 0.654 |
| RCS (scores)a) | 51.8 (45.6 – 56.6) | 48.3 (37.4 – 55.0) | 0.043* |
All values expressed as mean ± SD or median (25 – 75 percentile). * p < 0.05 and ** p < 0.01 by using Mann-Whitney U testa) and two sample t-testc). PSQI-J, the Japanese version of the Pittsburg Sleep Quality Index; SF-36v2, the Japanese MOS Short-Form 36-Item Health Survey ver2; PCS, Physical component score; MCS, Mental component score; RCS, Role-social component score
We also compared sleep variables and HRQOL of both type of individuals in the early working conditions and normal working conditions. Table III shows the comparison of sleep variables and HRQOL in morning type individuals. Among the morning type individuals (n=69), 37 participants worked under early working conditions and 32 participants under normal working conditions. The workers who worked under early working conditions had a median age of 32.0 (29.0–36.0) years old, included 22 men and 15 women, and had a median MEQ score (25–75 percentile) of 58.0 (56.0–62.0); while the workers who worked under normal working conditions had a median age (25–75 percentile) of 29.0 (25.0–39.3) years, included 19 men and 13 women, and had a median MEQ scores (25–75 percentile) of 56.5 (55.0–59.0). The age, gender, and MEQ scores were not significantly different in the two conditions. In sleep variables, the sleep offset time of individuals working under early working conditions was significantly earlier than those under normal working conditions (early working condition, 5:54 ± 0:43 hrs vs. normal working condition, 6:24 ± 0:43 hrs, p = 0.006). There were no significant differences in PSQI-J and SF-36v2 scores between the two conditions.
Table III.
Comparison of sleep status and health related quality of life in Morning type.
| Early working condition (n = 37) | Normal working condition (n = 32) | p - value | |
|---|---|---|---|
| Age (years)a) | 32.0 (29.0 – 36.0) | 29.0 (25.0 – 39.3) | 0.563 |
| Gender (Men/Women)b) | M22/W15 | M19/W13 | 0.994 |
| MEQ (scores)a) | 58.0 (56.0 – 62.0) | 56.5 (55.0 – 59.0) | 0.116 |
| Sleep variables | |||
| Sleep onset time (h:mm)a) | 0:00 (23:00 – 0:00) | 0:00 (0:00 – 0:30) | 0.055 |
| Sleep offset time (h:mm)c) | 5:54 ± 0:43 | 6:24 ± 0:43 | 0.006** |
| Total sleep time (h)c) | 6.2 ± 1.0 | 6.3 ± 1.0 | 0.593 |
| PSQI-J (scores)a) | 4.0 (3.0 – 5.0) | 4.5 (2.8 – 7.0) | 0.589 |
| SF-36v2 | |||
| PCS (scores)c) | 57.0 ± 7.4 | 57.2 ± 5.2 | 0.900 |
| MCS (scores)a) | 48.5 (45.3 – 53.8) | 49.9 (46.4 – 55.0) | 0.427 |
| RCS (scores)a) | 50.8 (46.1 – 57.6) | 51.8 (45.2 – 55.7) | 0.674 |
All values expressed as mean ± SD or median (25 – 75 percentile). ** p < 0.01 by using Mann-Whitney U testa), χ2- testb) and two sample t-testc). MEQ, the Morningness-Eveningness Questionnaire; PSQI-J, the Japanese version of the Pittsburg Sleep Quality Index; SF-36v2, the Japanese MOS Short-Form 36-Item Health Survey ver2; PCS, Physical component score; MCS, Mental component score; RCS, Role-social component score
Table IV shows the comparison of sleep variables and HRQOL in evening type individuals. The evening type individuals (n=57) consisted of 28 participants working under early working conditions and 29 participants under normal working conditions. Those working under early working conditions had a median age of 28.5 (25.8–34.3) years, included 10 men and 18 women, and had an average MEQ score of 44.5 ± 5.5; while those working under normal working conditions had a median age (25–75 percentile) of 29.0 (26.0–33.0) years, included 14 men and 15 women, and had an average MEQ score of 46.7 ± 4.4. The age, gender, and MEQ scores were not significantly different in the two conditions. The sleep onset/offset times of those under early working conditions were significantly early compared to those under normal working conditions (sleep onset time: early working condition, 0:00 (23:22–0:30) hrs vs. normal working condition, 0:30 (0:00–1:00) hrs, p = 0.003; sleep offset time: early working condition, 6:31 ± 0:45 hrs vs. normal working condition, 6:52 ± 0:28 hrs, p = 0.045). The PSQI-J scores of those under early working conditions were significantly higher than those under normal working conditions (early working condition, 6.2 ± 2.4 vs. normal working condition, 5.0 ± 2.1, p = 0.047). The other variables of SF-36v2 did not differ significantly.
Table IV.
Comparison of sleep status and health related quality of life in Evening type.
| Early working condition (n = 28) | Normal working condition (n = 29) | p - value | |
|---|---|---|---|
| Age (years)a) | 28.5 (25.8 – 34.3) | 29.0 (26.0 – 33.0) | 0.707 |
| Gender (Men/Women)b) | M10/W18 | M14/W15 | 0.337 |
| MEQ (scores)c) | 44.5 ± 5.5 | 46.7 ± 4.4 | 0.096 |
| Sleep variables | |||
| Sleep onset time (h:mm)a) | 0:00 (23:22 – 0:30) | 0:30 (0:00 – 1:00) | 0.003** |
| Sleep offset time (h:mm)c) | 6:31 ± 0:45 | 6:52 ± 0:28 | 0.045* |
| Total sleep time (h)a) | 6.5 (6.4 – 7.0) | 6.3 (5.8 – 7.0) | 0.093 |
| PSQI-J (scores)c) | 6.2 ± 2.4 | 5.0 ± 2.1 | 0.047* |
| SF-36v2 | |||
| PCS (scores)c) | 58.7 ± 6.6 | 56.5 ± 5.5 | 0.163 |
| MCS (scores)a) | 49.3 (37.7 – 51.8) | 50.2 (43.6 – 53.1) | 0.444 |
| RCS (scores)c) | 43.7 ± 11.8 | 48.3 ± 9.6 | 0.115 |
All values expressed as mean ± SD or median (25 – 75 percentile). * p < 0.05 and ** p < 0.01 by uing Mann-Whitney U testa), χ2- testb) or two sample t-testc). MEQ, the Morningness-Eveningness Questionnaire; PSQI-J, the Japanese version of the Pittsburg Sleep Quality Index; SF-36v2, the Japanese MOS Short-Form 36-Item Health Survey ver2; PCS, Physical component score; MCS, Mental component score; RCS, Role-social component score
DISCUSSION
In this study, we found that later the sleep onset/offset time, higher the PSQI-J scores and lower the RCS scores of SF-36v2 in evening type individuals in comparison to the morning type. Moreover, in the comparison of impact of working conditions on each type of individuals, we found no significant difference in sleep quality and HRQOL among morning type individuals under early and normal working conditions. On the other hand, poorer sleep quality, indicated by high PSQI-J scores, were observed in evening type workers under early working conditions than in those under normal working conditions. Moreover, the sleep onset/offset times of evening type workers under early working conditions were earlier than that of evening type workers under normal working conditions.
In the first part of the study, evening type workers went to sleep later (later sleep phase) and had poorer sleep quality compared to morning type workers. These results correspond with previous studies that revealed that evening type individuals had poorer sleep [28,33,35] and a later sleep phase [19] compared to morning type individuals. Additionally, the RCS scores of SF-36v2 of evening type workers were significantly low compared to morning type workers in this study. The RCS score is thought to define the social relationship of HRQOL, because RCS is the summary score associated with subscales of physical role, emotional role, and social functioning of SF-36v2 [23]. Therefore, we clarified not only the association between chronotype and sleep quality but also the association between chronotype and the social relationship of HRQOL. Also, previous studies had reported an association between evening type and depression [1,2,13,25]. The poor sleep quality or low HRQOL of the evening type workers in this study might be related to the prospective risk of depression; future studies should clarify the existence and extent of this association.
In the second part of the study, morning type workers under early working conditions had no difference in sleep quality and HRQOL compared to those workers under normal working conditions. In contrast, evening type workers under early working conditions had earlier sleep phases and poorer sleep quality compared to those under normal working conditions. This poor sleep quality in evening type workers under early working conditions might be due to the social jet lag caused by the time lag between evening preference of evening type workers and the earlier sleep phase of early working conditions. Social jet lag is the misalignment between individual chronotype and one’s social schedule specified by school or work [30]. Evening type individuals, in particular, commonly experience social jet lag because they prefer to be active in the evening phase according to their biological rhythm but they are forced to work during the early phase on working days. Juda et al. reported that social jet lag was associated with sleep disturbance in shift workers [10]. Additionally, social jet lag is associated with obesity [21] as well as the risk of cardiovascular diseases [22] and metabolic syndrome [18]. Thus, the social jet lag of evening type workers under early working conditions might be associated with future diseases. However, the early working conditions, which include the early work start time and decreased long working hours at night, are thought to be effective for decreasing the number of long working hours [16]. The morning type workers under early working conditions had no problem with sleep quality and HRQOL because their early sleep offset time matched their chronotype, while evening type workers under early working conditions had poor sleep quality. Therefore, taken together, this fact suggested that it is important to consider workers’ individual chronotype when new working styles are introduced.
This study has some limitations. First, we did not evaluate objective sleep status by using sleep devices like Actiwatch. Nevertheless, PSQI-J is a very popular method for evaluating sleep status and its reliability and validity have been established [4]. Secondly, we did not evaluate the working variables (clock in/out time and working hours) since this study focused on sleep status of workers engaged in different working conditions. Future studies should examine other working variables to offer detailed discussions on how working style influences workers’ sleep. Although this study had some limitations, it is the first of its kind to show the association between sleep and HRQOL in both morning and evening chronotype workers who are working under both early and normal working conditions.
In summary, based on the results of our study, we observe that evening type workers had poorer sleep status and lower social relationship scores of HRQOL compared to morning type workers. Further, evening type workers under early working conditions had poor sleep quality. Therefore, our study suggests that in order to improve each worker’s health, his or her working condition should be suited to his or her individual chronotype.
ACKNOWLEDGEMENTS
We acknowledge the support of all participants in this study. The authors reported no conflicts of interest.
REFERENCES
- 1.Alvaro PK, Roberts RM, Harris JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. 2014;15:934–941. doi: 10.1016/j.sleep.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BW. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33:75–83. doi: 10.1002/da.22422. [DOI] [PubMed] [Google Scholar]
- 3.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 4.Doi Y, Minowa M, Okawa M, Uchiyama M. Development of the Japanese version of the Pittsburgh Sleep Quality Index. Japanese Journal of Psychiatry Treatment. 1998;13:755–763. (in Japanese). [Google Scholar]
- 5.Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, Kamei Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–172. doi: 10.1016/s0165-1781(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 6.Fukuhara S, Ware JE, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol. 1998;51:1045–1053. doi: 10.1016/s0895-4356(98)00096-1. [DOI] [PubMed] [Google Scholar]
- 7.Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–1044. doi: 10.1016/s0895-4356(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 8.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 9.Ishihara K, Miyashita A, Inugami M, Fukuda K, Yamazaki K, Miyata Y. The results of investigation by the Japanese version of Morningness-Eveningness Questionnaire. Shinrigaku Kenkyu. 1986;57:87–91. doi: 10.4992/jjpsy.57.87. [DOI] [PubMed] [Google Scholar]
- 10.Juda M, Vetter C, Roenneberg T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J Biol Rhythms. 2013;28:141–151. doi: 10.1177/0748730412475042. [DOI] [PubMed] [Google Scholar]
- 11.Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet. 2015;386:1739–1746. doi: 10.1016/S0140-6736(15)60295-1. [DOI] [PubMed] [Google Scholar]
- 12.Knutson KL, von Schantz M. Associations between chronotype, morbidity and mortality in the UK Biobank cohort. Chronobiol Int. 2018;35:1045–1053. doi: 10.1080/07420528.2018.1454458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levandovski R, Dantas G, Fernandes LC, Caumo W, Torres I, Roenneberg T, Hidalgo MP, Allebrandt KV. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol Int. 2011;28:771–778. doi: 10.3109/07420528.2011.602445. [DOI] [PubMed] [Google Scholar]
- 14.Müller MJ, Olschinski C, Kundermann B, Cabanel N. Patterns of self-reported depressive symptoms in relation to morningness-eveningness in inpatients with a depressive disorder. Psychiatry Res. 2016;239:163–168. doi: 10.1016/j.psychres.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Nakashima M, Morikawa Y, Sakurai M, Nakamura K, Miura K, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Nakagawa H. Association between long working hours and sleep problems in white-collar workers. J Sleep Res. 2011;20:110–116. doi: 10.1111/j.1365-2869.2010.00852.x. [DOI] [PubMed] [Google Scholar]
- 16.Odaira H. “Chiho komuin no jikangai kinmu ni kannsuru jittai chosa kekka” ni tsuite. Chiho komuin geppo. 2017;(646):56–73. (in Japanese) [Google Scholar]
- 17.Osland TM, Bjorvatn BR, Steen VM, Pallesen S. Association study of a variable-number tandem repeat polymorphism in the clock gene PERIOD3 and chronotype in Norwegian university students. Chronobiol Int. 2011;28:764–770. doi: 10.3109/07420528.2011.607375. [DOI] [PubMed] [Google Scholar]
- 18.Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, Caspi A. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes (Lond) 2015;39:842–848. doi: 10.1038/ijo.2014.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 20.Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, Merrow M. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11:429–438. doi: 10.1016/j.smrv.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 22.Rutters F, Lemmens SG, Adam TC, Bremmer MA, Elders PJ, Nijpels G, Dekker JM. Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile? J Biol Rhythms. 2014;29:377–383. doi: 10.1177/0748730414550199. [DOI] [PubMed] [Google Scholar]
- 23.Suzukamo Y, Fukuhara S, Green J, Kosinski M, Gandek B, Ware JE. Validation testing of a three-component model of Short Form-36 scores. J Clin Epidemiol. 2011;64:301–308. doi: 10.1016/j.jclinepi.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi M, Tahara Y, Tsubosaka M, Fukazawa M, Ozaki M, Iwakami T, Nakaoka T, Shibata S. Chronotype and social jetlag influence human circadian clock gene expression. Sci Rep. 2018;8:10152. doi: 10.1038/s41598-018-28616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vetter C, Chang SC, Devore EE, Rohrer F, Okereke OI, Schernhammer ES. Prospective study of chronotype and incident depression among middle- and older-aged women in the Nurses’ Health Study II. J Psychiatr Res. 2018;103:156–160. doi: 10.1016/j.jpsychires.2018.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Virtanen M, Ferrie JE, Singh-Manoux A, Shipley MJ, Vahtera J, Marmot MG, Kivimäki M. Overtime work and incident coronary heart disease: the Whitehall II prospective cohort study. Eur Heart J. 2010;31:1737–1744. doi: 10.1093/eurheartj/ehq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Virtanen M, Stansfeld SA, Fuhrer R, Ferrie JE, Kivimäki M. Overtime work as a predictor of major depressive episode: a 5-year follow-up of the Whitehall II study. PLoS One. 2012;7:e30719. doi: 10.1371/journal.pone.0030719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vitale JA, Roveda E, Montaruli A, Galasso L, Weydahl A, Caumo A, Carandente F. Chronotype influences activity circadian rhythm and sleep: differences in sleep quality between weekdays and weekend. Chronobiol Int. 2015;32:405–415. doi: 10.3109/07420528.2014.986273. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 31.Wu S, Zhu W, Li H, Yu IT, Lin S, Wang X, Yang S. Quality of life and its influencing factors among medical professionals in China. Int Arch Occup Environ Health. 2010;83:753–761. doi: 10.1007/s00420-009-0496-4. [DOI] [PubMed] [Google Scholar]
- 32.Yadav A, Singh S. Relationship of chronotype to sleep pattern in a cohort of college students during work days and vacation days. Indian J Exp Biol. 2014;52:569–574. [PubMed] [Google Scholar]
- 33.Yazdi Z, Sadeghniiat-Haghighi K, Javadi AR, Rikhtegar G. Sleep quality and insomnia in nurses with different circadian chronotypes: morningness and eveningness orientation. Work. 2014;47:561–567. doi: 10.3233/WOR-131664. [DOI] [PubMed] [Google Scholar]
- 34.Yu JH, Yun CH, Ahn JH, Suh S, Cho HJ, Lee SK, Yoo HJ, Seo JA, Kim SG, Choi KM, et al. Evening chronotype is associated with metabolic disorders and body composition in middle-aged adults. J Clin Endocrinol Metab. 2015;100:1494–1502. doi: 10.1210/jc.2014-3754. [DOI] [PubMed] [Google Scholar]
- 35.Yun JA, Ahn YS, Jeong KS, Joo EJ, Choi KS. The Relationship between Chronotype and Sleep Quality in Korean Firefighters. Clin Psychopharmacol Neurosci. 2015;13:201–208. doi: 10.9758/cpn.2015.13.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]