Abstract
Activation of the inflammasome is a key function of the innate immune response which regulates inflammation in response to microbial substances. Inflammasome activation by human rhinovirus (RV), a major cause of asthma exacerbations, has not been well-studied. We examined whether RV induces inflammasome activation in vivo, molecular mechanisms underlying RV-stimulated inflammasome priming and activation, and the contribution of inflammasome activation to RV-induced airway inflammation and exacerbation. RV infection triggered lung mRNA and protein expression of pro-IL-1β and NLRP3, indicative of inflammasome priming, as well as cleavage of caspase-1 and pro-IL-1β, completing inflammasome activation. Immunofluorescence staining showed IL-1β in lung macrophages. Depletion with clodronate liposomes and adoptive transfer experiments showed macrophages to be required and sufficient for RV-induced inflammasome activation. TLR2 was required for RV-induced inflammasome priming in vivo. UV-irradiation blocked inflammasome activation and RV genome was sufficient for inflammasome activation in primed cells. Naïve and house dust mite-treated NLRP3−/−and IL-1β−/−mice, as well as IL-1 receptor antagonist-treated mice, showed attenuated airway inflammation and responsiveness following RV infection. We conclude that RV-induced inflammasome activation is required for maximal airway inflammation and hyperresponsiveness in naïve and allergic mice. The inflammasome represents a molecular target for RV-induced asthma exacerbations.
Keywords: Inflammasome, IL-1β, rhinovirus, asthma, macrophage, NLRP3
Introduction
Activation of the inflammasome is a key function of the innate immune response which regulates inflammation and pyroptosis, a lytic form of cell death, in response to detected stimuli1. Inflammasomes consists of three main components: a pattern recognition receptor; an adaptor protein which consists of a pyrin domain and a caspase recruitment domain; and the cysteine protease caspase-1 as the effector. At least five pattern recognition receptors have been shown to assemble inflammasomes. Nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain containing 3 (NLRP3) detects a diverse series of agonists including pathogens (bacteria, fungi, viruses) and sterile environmental stimuli such as asbestos and silica2, 3. A twostep model has been suggested for NLRP3 inflammasome activation4. The first step, priming by extracellular inflammatory stimuli, induces NLRP3 and pro-interleukin (IL)-1β expression. The second step, which may be triggered by an array of cellular mechanisms including release of oxidized mitochondrial DNA, reactive oxygen, mitochondrial dysfunction, lysosomal rupture, intracellular calcium and potassium efflux, activates caspase-1- mediated proteolytic cleavage of pro-inflammatory IL-1 family cytokines into their bioactive forms, IL-1β and IL-18.
Evidence exists for inflammasome activation in asthma. IL-1β was increased in sputum and bronchoalveolar lavage (BAL) fluid of patients with neutrophilic5 and Th2/Th17predominant asthma6. Sputum macrophages from patients with neutrophilic asthma also showed elevated mRNA expression of NLRP3, caspase-1 and IL-1β, as well as increased NLRP3 and caspase-1 protein abundance7, evidence of NLRP3 inflammasome activation. Gene signatures of NLRP1, NLRP3 and NLRC4 were increased in sputum cells of nonsmoking patients with severe neutrophilic or eosinophilic asthma8. In contrast, compared to healthy volunteers, expression of inflammasome genes was decreased in samples of sputum inflammatory cells from patients with allergic rhinitis or asthma9. Finally, IL-1β promotes airways hyperresponsiveness in rodents sensitized to ovalbumin, a model allergen10, 11.
Human rhinovirus (RV), a member of the family Picornaviridae, genus Enterovirus, carries a single-stranded positive RNA genome, about 7.5 kb in size. Four structural proteins, VP1, VP2, VP3 and the myristoylated VP412, form the icosahedral capsid. First identified as the most common cause of upper respiratory tract infections, advances in molecular methods of viral detection have linked RV infections to exacerbations of chronic pulmonary disease, in particular asthma and COPD13, 14. RV is the most common cause of asthma exacerbation in children15, 16 and adults13, 17.
In cultured bronchial epithelial cells, RV infection induces NLRP3 and NLRC5 inflammasome activation18, 19 and IL-1β secretion20 Experimental human RV infection increases nasal IL-1β21–23. However, the association between RV-induced inflammasome activation and airway inflammation has not been established in vivo.
In this study, we examined the effects of RV infection on inflammasome activation in naïve mice as well as those with allergic airways disease. We found that RV induces inflammasome activation in vivo, and that inflammasome activation plays an essential role in RV-induced airway inflammation and hyperresponsiveness. We also identified primary roles for TLR2 activation and viral genome in inflammasome priming and activation, respectively.
Results
RV infection activates the inflammasome in vivo.
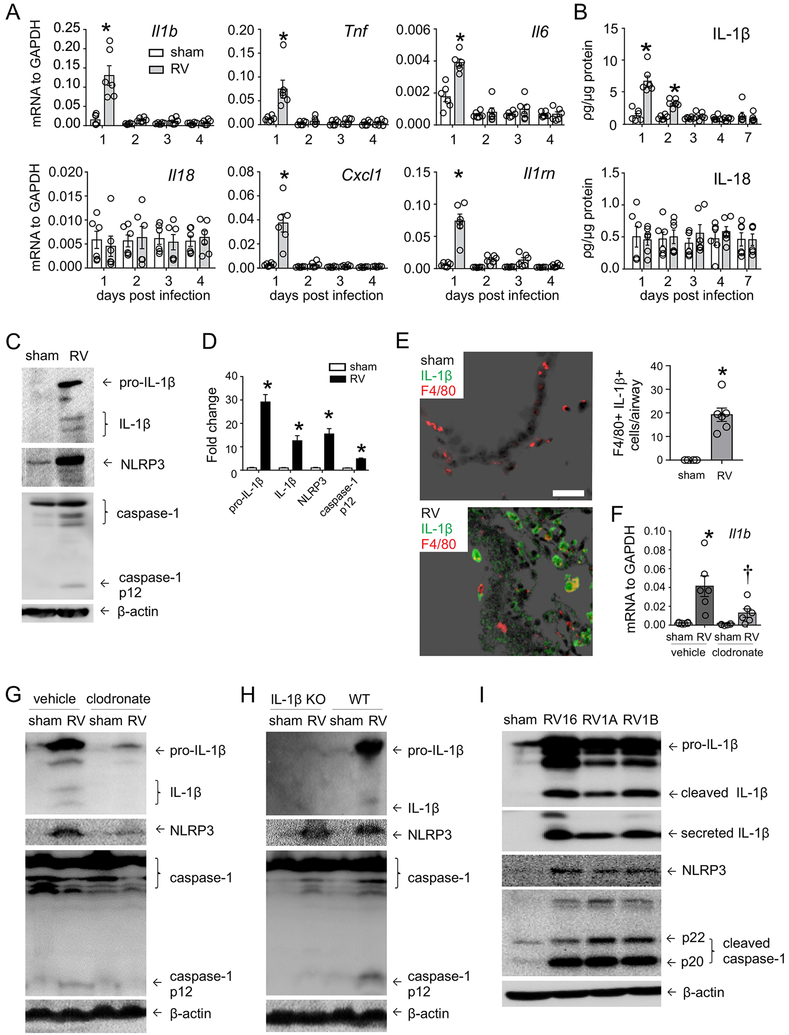
Previous studies have shown NLRP3 inflammasome activation in RV-infected bronchial epithelial cells18, 19. We employed in vivo model to determine the role of RV infection in inflammasome activation. We collected lungs from RV-infected mice and measured IL-1β and IL-18 mRNA and protein. IL-1β mRNA and protein expression, but not IL-18, was increased in RV-infected mice at early time points of infection (Fig. 1A, 1B). In addition, mRNA expression of the pro-inflammatory cytokines Cxcl1, Il6 and TNFa, and the IL-1 receptor antagonist Il1rn was increased (Fig. 1A). RV increased protein expression of NLRP3 and pro-IL-1β (Fig. 1C, 1D), indicative of the RV-induced priming step. RV also triggered cleavage of pro-IL-1β and caspase-1 and subsequent production of IL-1β and caspase-1 p12, demonstrating inflammasome activation in the lungs of RV-infected mice.
FIG 1. RV activates inflammasome in vivo.
C57BL/6 mice were inoculated with sham or RV. Lung mRNA (A) and protein (B) expression were measured 1, 2, 3, 4 or 7 days later. (N=6 from two different experiments, mean±SEM, *different from sham, p<0.05, two-way ANOVA with Tukey’s multiple comparisons test.) C. One day after infection, whole lungs were homogenized and subjected to Western blot. Anti-mouse-IL-1β recognizes pro-IL-1β and its bioactive form IL1β. Anti-mouse-caspase-1 detects both caspase-1 and its cleaved form, caspase-1 p12. D. Group mean relative expression levels were normalized to β-actin. (N=12 from six different experiments, mean±SEM, *different from sham, p<0.05, two-way ANOVA.) E. Lungs were stained for IL-1β (green), F4/80 (red) and nuclei (DAPI, black; bar, 50 μm). Average number of F4/80+ IL-1β+ cells per airway (N=6 from two different experiments, mean ±SEM, *different from sham, p<0.05, unpaired t test.) F. and G. Clodronate- or PBS-containing liposomes were delivered to mice intratracheally 24 hours before sham or RV infection. One day after infection, lungs were harvested for mRNA and Western blot (N=6 from one experiment, mean±SEM, *different from sham, p<0.05, two-way ANOVA). H. Bone marrow cells from either wild-type or IL-1β−/−mice were cultured in L929 media for 7 days. Macrophages were transferred to IL1β−/−mice intratracheally at 106 cells per mouse 24 hours before RV infection. One day after infection, lungs were harvested for Western blot analysis. (Image is representative of N=3 from one experiment.) I. Human THP-1 (106 cells) were infected with sham, RV-16, RV-1A or RV1B at an MOI of 1 for 24 hours. Both cell lysate and supernatant were collected for immunoblot assay. Anti-human-capase-1 recognizes two forms of cleaved caspase-1, p22 and p20. Antihuman-IL-1β recognizes pro-IL-1β and IL-1β. (Image is representative of N=3 from two experiments.) For clarity, individual data points are not shown for panel D.
To determine the cellular source of inflammasome activation, we examined airway IL-1β deposition by immunofluorescence. Infection with RV increased airway IL-1β expression, with the strongest signal found in subepithelial F4/80+ cells, indicative of airway macrophages (Fig. 1E). There was less IL-1β staining in the airway epithelium.
Next, we delivered clodronate- or PBS-containing liposomes to mice intratracheally to deplete macrophages as previously described24. Twenty-four hours later, mice were inoculated with sham or RV. Clodronate treatment significantly reduced whole lung IL-1β mRNA in RV-infected mice (Fig. 1F). RV-induced protein expression of NLRP3 and pro-IL-1β as well as the production of mature IL-1β and caspase-1 p12 were also reduced in clodronate-treated mice (Fig. 1G), confirming the macrophage to be major cellular source of inflammasome activation.
We tested the sufficiency of macrophages for inflammasome activation by transferring bone marrow-derived macrophages from wild-type and IL-1β−/−mice to the airways of sham-treated and RV-infected IL-1β−/−mice. IL-1β−/−mice receiving macrophages from IL-1β−/−mice showed no inflammasome activation following RV infection. However, IL-1β−/−mice receiving macrophages from wild type mice and infected with RV showed a significant increase in NLRP3, pro-IL-1β, IL-1β and caspase-1 p12 (Fig. 1H).
Finally, to test inflammasome activation by a major group RV strain, THP-1 human monocytic cells were infected with RV-16, a major group virus, and RV-1A and RV-1B, two minor group viruses. Each infection showed cleaved caspase-1 and IL-1β (Figure 1I). Secreted IL-1β was also detected in the culture supernatant of virus-infected cells, demonstrating inflammasome activation by major and minor RV strains.
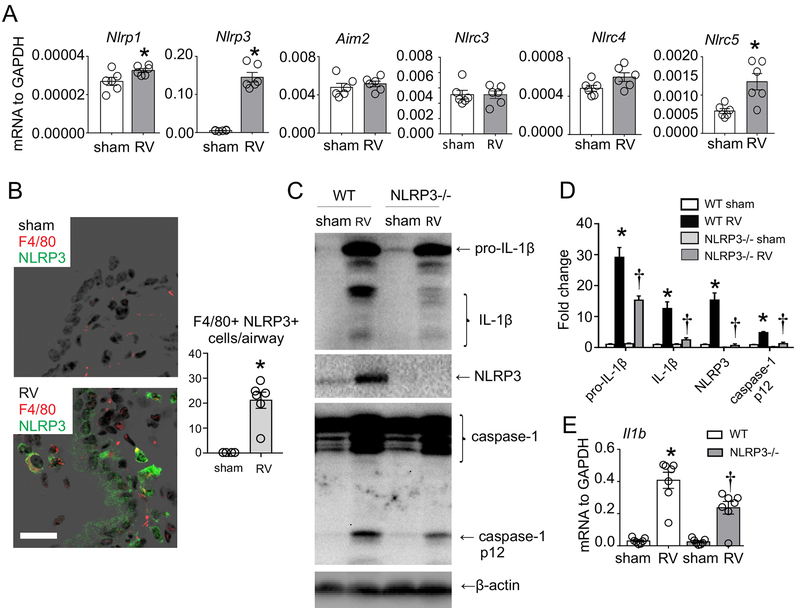
NLRP3 is required for RV induced inflammasome activation.
We examined RV-induced lung mRNA expression of different pattern recognition receptors involved in inflammasome formation. RV induced Nlrp1, Nlrp3, and Nlrc5 mRNA expression, but not Aim2, Nlrc3 or Nlrc4 (Fig. 2A). Immunoblots and immunofluorescence staining showed increased lung NLRP3 protein expression in RV-infected mice (Fig. 1C and 2B). Similar to IL-1β, large subepithelial cell F4/80 positive cells were highly positive for NLRP3 expression (Fig 2B). Again, there was less NLRP3 staining in the airway epithelium.
FIG 2. NLRP3 is required for RV-triggered inflammasome.
Wild type C57BL/6 (WT) or NLRP3−/−mice were inoculated with sham or RV for 24 hours. A. Lung mRNAs were measured by qPCR (N=6 from two different experiments, mean±SEM, *different from sham, p<0.05, unpaired t test). B. Lungs were stained for NLRP3 (green), F4/80 (red) and nuclei (DAPI, black; bar, 50 μm). Average number of F4/80+ NLRP3+ cells per airway (N=6 from one experiment, mean ±SEM, *different from sham, p<0.05, unpaired t test.) C, D. Whole lungs collected from C57BL/6 and NLRP3−/−mice were homogenized within lysis buffer and subjected to Western blot. Group mean expression levels relative to β-actin are also shown. (N=6 from three different experiments, mean±SEM, *different from sham, †different from wild type, p<0.05, two-way ANOVA.) E. Effect of NLRP3−/−on IL1b mRNA (N=7 from two different experiments, mean±SEM, *different from WT sham, †different from WT RV, p<0.05, two-way ANOVA with Tukey multiple comparisons test). For clarity, individual data points are not shown for panel D.
We examined the requirement of NLRP3 for inflammasome activation using NLRP3−/−mice. RV-infected NLRP3−/−mice showed significantly decreased caspase-1 p12 and IL-1β levels, suggesting that NLRP3 is required for the RV inflammasome activation step (Fig. 2C, 2D). NLRP3−/−also slightly reduced Il1b mRNA (Fig 2E) and pro-IL-1β protein expression (Fig 2C, 2D), consistent with previous reports of an IL-1β autocrine loop25, 26.
TLR2 is required and sufficient for the priming step of RV-induced inflammasome.
TLR2 is required for RV-induced cytokine responses in vivo27. We employed TLR2−/−mice to determine the role of TLR2 in RV-induced inflammasome activation. Compared to wild type mice, RV-induced Il1b, il1rn, Nlrp3, Nlrc5 and Tnf mRNA expression was blocked in TLR2−/−mice (Fig 3A). TLR2−/−mice also showed a reduction in RV-induced lung IL-1β protein level compared to wild type (Fig 3B). Consistent with decreased mRNA expression, TLR2−/−mice showed a reduction in RV-induced protein abundance of pro-IL1b and NLRP3, demonstrating a block in inflammasome priming (Fig 3C, 3D). Immunoblots also showed reduced caspase-1 p12 and mature IL-1β in TLR2−/−mice. We also infected bone marrow-derived macrophages isolated from wild type and TLR2−/−mice with RV. Macrophages from TLR2−/−mice showed similar results as whole lung, with attenuated RV-induced expression of pro-IL-1β, NLRP3, mature IL1β and caspase-1 p12 (Fig 3E). However, LPS, a TLR4 ligand, increased pro-IL-1β and NLRP3 in both wild type and TLR2−/−macrophages. Together, our results suggest the RV-TLR2 interaction is essential for the priming step of inflammasome activation, which in turn is necessary for inflammasome activation.
FIG 3. RV-induced inflammasome activation is TLR2 dependent.
Wild type C57BL/6 (WT) or TLR2−/−mice were inoculated with sham or RV for 24 hours. Lung mRNA (A), protein (B) and inflammasome activation (C, D) were assessed. (N= 6–7 from two different experiments, mean±SEM, *different from WT sham, †different from WT RV, p<0.05, two-way ANOVA.) E. Bone marrow-derived macrophages from C57BL/6 (WT) or TLR2−/−mice were infected with sham or RV at an MOI of 1 or 10 for 24 hours. Selected cells were primed with LPS (100 ng/ml) for 6 hours. (Image is representative of two experiments.) F. Bone marrow-derived macrophages from C57BL/6 (WT) or TLR2−/−mice were treated with recombinant MyrVP4 (500 ng/mL) for 24 hours. (Image is representative of two experiments.) For clarity, individual data points are not shown for panel D.
We have recently found that the RV-TLR2 interaction is mediated by the myristoylated viral capsid protein VP428. We treated bone marrow-derived macrophages from wild type mice with synthetic MyrVP4. Immunoblots showed increased protein abundance of pro-IL-1β (Fig 3F). However, the bioactive product IL-1β was not present, in contrast to RV-treated cells. In addition, MyrVP4-induced pro-IL-1β expression was decreased in bone marrow-derived macrophages from TLR2−/−mice. Thus, TLR2 is not only required, but also sufficient, for inflammasome priming.
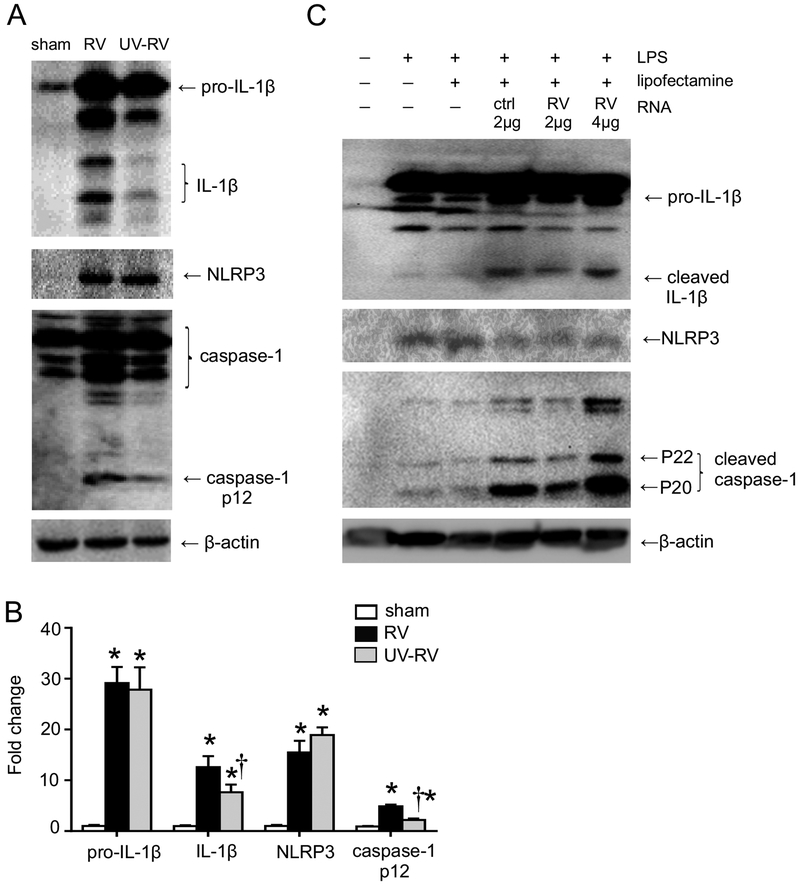
UV-irradiation attenuates inflammasome activation in RV-infected mice.
Recognition of viral RNA triggers activation of the NLRP3 inflammasome, which in return mediates innate immune responses against RNA viruses29, 30. We examined the effect of UV-irradiation (which damages the viral genome and prevents its replication) on RV-induced inflammasome priming and activation by immunoblot. C57BL/6 mice treated with UV-irradiated RV-1B showed unchanged pro-IL-1β and NLRP3 expression levels, indicating an intact priming step (Fig. 4A, 4B). However, UV irradiation of RV-1B attenuated cleavage of caspase-1 p12 and IL-1β, suggesting the essential role of viral RNA in inflammasome activation.
FIG 4. UV-irradiation impairs RV-induced inflammasome activation.
A. Wild type C57BL/6 mice were infected with sham, RV, or UV-RV for 24 hours. B. Group mean relative expression levels were normalized to β-actin. (N=6 from three different experiments, mean±SEM, *different from sham, p<0.05, †different from RV, two-way ANOVA.) C. Human THP-1 cells were pre-incubated with LPS (1 μg/mL) for 6 hours. The LPS-primed cells were then transfected with control or viral genomic single-stranded RNA for 20 hours. Whole cell lysate was assessed for inflammasome activation by immunoblot. (Image is representative of two experiments.) For clarity, individual data points are not shown for panel B.
Transfection of single-stranded RNA is sufficient for inflammasome activation.
RV induced inflammasome activation in mouse bone marrow-derived macrophages that do not support viral replication31. It is therefore plausible that single-stranded viral genomic RNA, rather than double-stranded RNA formed during viral replication, is sufficient for inflammasome activation. To test this, human THP-1 cells were primed with LPS for 6 hr and then subjected to transient transfection with control single-strand RNA or in-vitro transcribed RV-1A genomic RNA. LPS-primed THP-1 cells showed increased expression of pro-IL-1β and NLRP3, but limited mature IL-1β and caspase-1 p20 and p22 (Fig 4C). Transfection of LPS-treated cells with control single-stranded and RV-1A genomic RNA each induced increased expression of mature IL-1β and caspase-1 p20 and p22, suggesting that, in primed cells, single-stranded RNA is sufficient for inflammasome activation
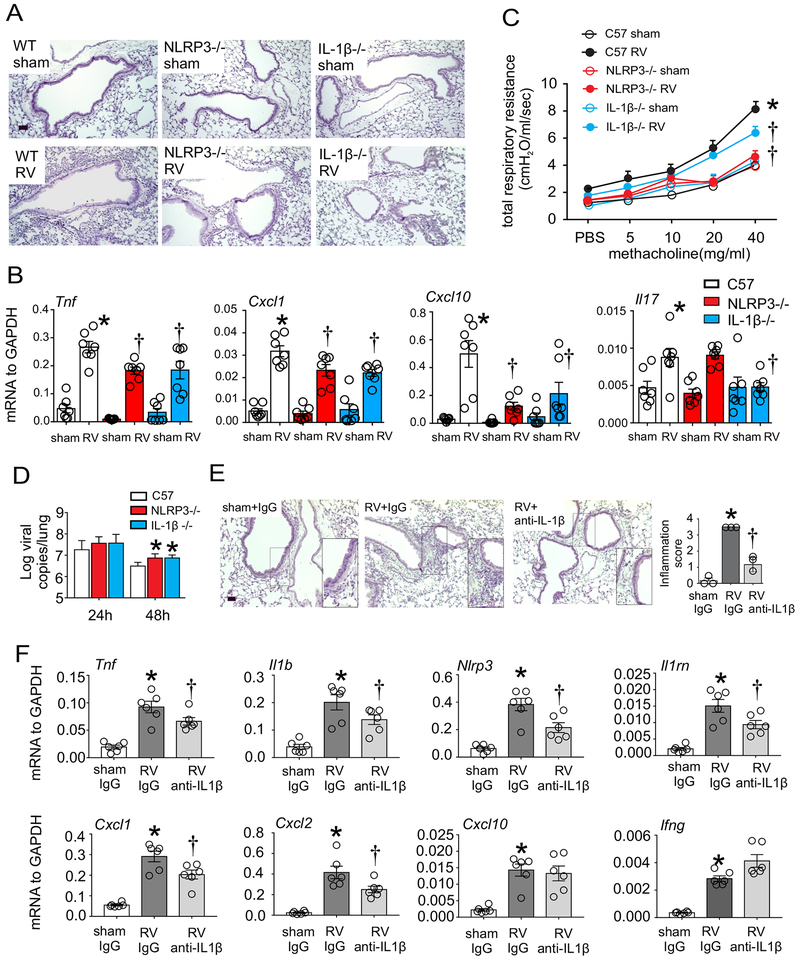
NLRP3 and IL-1β knockouts attenuate RV-induced airway inflammation in naïve mice.
We examined differences in RV response between wild type, NLRP3−/−and IL-1β−/−mice. Lungs of wild-type animals revealed peribronchial inflammatory and intraluminal infiltrates (Fig 5A). In contrast, RV-infected NLRP3−/−and IL-1β−/−mice showed minimal inflammation. BAL cell counts showed decreased numbers of total cells and neutrophils in RV infected NLRP3−/−and IL1β−/−mice (Fig 6D). Following RV infection, Cxcl1, Cxcl10, Tnf, and Il17 mRNA expression were increased significantly 24 hours post-infection of wild type C57BL/6 mice but reduced in NLRP3−/−and IL-1β−/−mice (Fig 5B). In addition, NLRP3−/−and IL-1β−/−mice showed decreased airway cholinergic responsiveness following RV infection (Fig 5C).
FIG 5. Inhibition of RV-induced airway inflammation and hyperresponsiveness in NLRP3 −/−, IL-1β−/−, and anti-IL-1β treated mice.
A, C57BL/6 (WT), NLRP3−/−or IL-1β−/−mice were intranasally infected with sham or RV. Lung sections were prepared 2 days after infection. B. Transcript levels of pro-inflammatory cytokines were assessed one day post-infection by quantitative PCR and results expressed as fold change over GAPDH (N=7 from two different experiments, mean±SEM, *different from WT sham, † different from WT RV, p<0.05, two-way ANOVA). C. Airways hyperresponsiveness was measured in sham- or RV-treated wild type, NLRP3−/−, and IL-1β−/−mice 2 days after treatment. (N=4 from two different experiments, mean±SEM, *different from WT RV, † different from WT RV, p<0.05, two-way ANOVA with Tukey multiple comparisons test.) D. RV positive strand RNA was assessed 24–48 h after infection, and presented as viral copy numbers in total lung. (N=7 from two different experiments, mean±SEM, * different from WT RV, p<0.05, two-way ANOVA with Tukey multiple comparisons test.) E and F, C57BL/6 mice were inoculated with sham + IgG, RV + IgG or RV+anti-IL-1β. Anti-IL-1β was given 1 hour before infection to selected RV-treated mice. After 24 hours, lungs were harvested for histology (E, bar is 50 μm), inflammation score (N=3 from one experiment) and mRNA expression (N=6 from two different experiments, mean±SEM, *different from sham + IgG, †different from RV + IgG, p<0.05, one-way ANOVA with Tukey’s multiple comparisons test.) For clarity, individual data points are not shown for panels C and D.
FIG 6. Inflammasome inhibition attenuates RV-induced allergic airway inflammation and type-2 immune response in HDM-sensitized mice.
Whole lungs collected from PBS-or HDMtreated wild type mice 1 day post-RV infection were subjected to Western blot (A and B) and qPCR analysis (C). (N= 7 from two different experiments, mean±SEM, *different from WT sham, †different from WT RV, p<0.05, two-way ANOVA with Tukey’s multiple comparisons test.) D. Differential immune cell counts in BAL of PBS-or HDM-sensitized and challenged, sham- or RV-treated wild type, NLRP3−/−, and IL-1β−/−mice (105 cells/ml) 2 days after treatment (N=7 from two different experiments, mean±SEM, *different from WT sham, †different from WT PBS RV or WT HDM RV, ‡ different from WT HDM sham, p<0.05, two-way ANOVA with Tukey’s multiple comparisons test). E and F. Airways responsiveness was measured in PBS-or HDM-sensitized and challenged, sham- or RV-treated wild type, NLRP3−/−, and IL-1β−/−mice 2 days after treatment. (N=4 from two different experiments, mean±SEM, *different from WT sham, †different from WT RV, p<0.05, two-way ANOVA). G. mRNA levels of type 2 cytokines in mice lungs. (N=7 from two different experiments, mean±SEM, *different from WT sham, †different from WT PBS RV or WT HDM RV, ‡ different from WT HDM sham, p<0.05 two-way ANOVA with Tukey’s multiple comparisons test). H and I. Recombinant IL-1RA (1 mg/kg body weight) was given after HDM treatment, one h before and 24 h after RV infection. BAL cell counts (H) and lung mRNA levels of type 2 cytokines (I) were measured 2 days post-RV infection. (N=7 from two different experiments, mean±SEM, *different from HDM-sham, †different from HDM RV, p<0.05, one-way ANOVA). For clarity, individual data points are not shown for panels B, F and G.
We have previously shown that inoculation of mice with RV-1B is associated with modest viral replication32, 33. Compared to wild-type C57BL/6 mice, NLRP3 −/−and IL1b −/−mice showed small (1/2 log) but statistically significant increases in viral copy number (Fig 5D).
H&E staining showed that treatment with anti-IL-1β blocked peribronchial inflammatory and intraluminal infiltrates (Fig 5E). Expression of mRNAs encoding IL-1β, IL-1RN, TNF-α, NLRP3, CXCL-1 and CXCL-2 was decreased (Fig 5F). Taken together, these results show that IL-1β plays a key role in the development of lung inflammation in RV-infected mice.
Reduction of type 2 inflammation and airway eosinophils in RV-infected HDM-sensitized and -challenged mice.
We examined whether NLRP3 and IL-1β play roles in RV-mediated exacerbation of allergic airway disease. First, we examined the effect of allergen treatment on RV-induced lung inflammasome activation. We employed a clinically relevant mouse model designed to recapitulate RV-induced asthma exacerbation, as described previously34. Wild-type C57BL/6 mice were sensitized with house dust mite (HDM) and challenged with HDM 10 and 11 days after sensitization. Mice were infected with RV one day after the last challenge. HDM treatment induced modest pro-IL-1β synthesis but no mature IL-1β synthesis (Fig 6A, 6B). RV infection increased both pro- and mature IL-1β synthesis in HDM-treated mice at day 1 post infection, evidence of inflammasome priming and activation. However, mRNA expression of IL-1β and NLRP3 and abundance of mature IL-1β and p12 caspase 1 were reduced compared to PBS-treated RV-infected mice, suggesting that allergen treatment partially attenuates inflammasome priming and activation (Fig 6A-6C).
Sham-infected house dust mite-sensitized and -challenged mice exhibited signs of allergic airway inflammation compared to sham-infected naïve controls, including increased BAL total cells, eosinophils and lymphocytes (Fig 6D, 6E). In addition, HDM-sensitized and challenged mice inoculated with RV displayed exacerbated airway inflammation compared HDM-treated mice inoculated with sham, including increased total BAL cells, neutrophils, eosinophils, lymphocytes (Fig 6D), airway responsiveness (Fig 6E) and mRNA expression of Il4, Il5, Il13, and Ccl24 (Fig 6G).
Next, we examined airway inflammation in HDM-sensitized and challenged, RV-infected, wild type, NLRP3−/−and IL-1β −/−mice. Compared to wild type, HDM-sensitized and challenged NLRP3−/−and IL-1β−/−mice showed significantly reduced RV-induced total cells, neutrophils, lymphocytes and eosinophils, as well as reduced cytokine mRNA expression (Fig 6D, 6G). HDM-treated and RV-infected NLRP3−/−and IL1β−/−mice showed reduced airways responsiveness compared to RV-infected HDM-treated wild type mice (Fig 6F).
We also examined the effects of a recombinant IL-1 receptor antagonist on RV-induced inflammation in HDM-treated mice. Recombinant IL-1RA was given after HDM treatment, one h before and 24 h after RV infection. IL-1RA significantly attenuated RV-induced eosinophilic inflammation and type 2 cytokine mRNA expression in allergen-treated mice (Fig 6H, 6I).
Discussion
RV is an important cause of asthma exacerbation. However, the precise mechanisms underlying RV-induced asthma exacerbation are uncertain. Activation of the inflammasome is a key function of the innate immune response which regulates inflammation in response to microbial substances, including viral infections. Influenza is a well-known stimulus of inflammasome activation29, 35–37. However, inflammasome activation by RV, perhaps the most common human infection, has not been well-studied. While RV has been shown to induce NLRP3 and NLRC5 inflammasome activation18, 19 and IL-1β secretion19, 20 in cultured bronchial epithelial cells, little is known about RV-induced inflammasome activation in vivo or its contribution to airway inflammation and exacerbation of allergic airways disease. Our pilot studies in children with RV infections show overexpression of IL1B, MEFV and other inflammasome-related genes. To address this in a mechanistic manner, we infected C57BL/6 mice with RV-1B, a minor group strain which replicates in mouse and human cells38. RV infection triggered inflammasome priming and activation. Lung macrophages were a major cellular source of IL-1β. TLR2 was required and myristoylated VP4, a TLR2 ligand, were sufficient for inflammasome priming. In contrast, UV-irradiation blocked RV-induced inflammasome activation and single-stranded RV genome was sufficient for this process, indicating a key role for the RV genome in inflammasome activation. Naïve NLRP3- and IL-1βdeficient mice showed attenuated RV-induced airway inflammation (fewer BAL cells and reduced lung cytokine levels), despite a slightly increased viral load. RV infection of HDM-sensitized and -challenged mice showed additive or synergistic type 2 inflammatory responses which were reduced in NLRP3 and IL-1β deficient mice, as well as wild type mice treated with IL-1 receptor antagonist. Together, these data show for the first time that inflammasome activation is required for RV-induced airway inflammation in naïve and allergen-sensitized mice.
Our data are consistent with previous work showing reduced lung inflammation in influenza-infected mice lacking the NLRP3 inflammasome29. However, in contrast to influenza-infected NLRP3-deficient mice with increased mortality, RV-infected NLRP3−/−mice showed reduced airway responsiveness. Airway inflammation and responsiveness were reduced in NLRP3- and IL-1β-deficient mice despite the fact that viral copy number was significantly higher 48 h after infection. Thus, in the context of a non-lethal lung infection, inflammasome activation was deleterious to the host, leading to an asthma exacerbation-like phenotype. While the amount of viral replication in our model is limited, these data are consistent with the notion that disproportionate inflammation, rather than viral-induced cellular damage, is the cause of RV-induced asthma exacerbation.
Previous studies have examined the role of the inflammasome products IL-1β and IL-18 in RV infection, but in a limited fashion. RV infection has been shown to induce IL-1β secretion in cultured bronchial epithelial cells19, 20. IL-1β potentiated RV-1B-induced CXCL8 production in cultured BEAS-2B airway epithelial cells39. Administration of an IL-1 receptor antagonist decreases RV-induced IL-6 and IL-8 production in primary bronchial epithelial cells40. Experimental human RV infection increases IL-1β21–23 and IL-1841 in nasal washings. However, we did not observe an increase in IL-18 mRNA in RV-infected mice, nor did we find an IL18 signal in children with natural RV infections.
While in vitro studies of RV-induced inflammasome activation have focused on airway epithelial cells18, 19, we found that subepithelial macrophages produce IL-1β in response to RV infection in vivo. Macrophages were required and sufficient for RV-induced lung inflammasome activation. These data are consistent with previous work showing that caspase-1 inflammasome activation in the hematopoietic, but not stromal, compartment was required to induce protective antiviral immunity in influenza-infected mice37. These data provide further support to the concept that airway macrophages are the main source of inflammatory cytokines following RV infection, in contrast to airway epithelial cells24, which support viral replication.
We found that TLR2 was required for RV-induced mRNA expression of pro-IL-1β and NLRP3 in C57BL/6 mice and cultured macrophages. MyrVP4 induced mRNA expression of pro-IL-1β and NLRP3 in cultured macrophages, but not the bioactive products IL-1β and caspase-1 p12. MyrVP4-induced priming was blocked in TLR2−/−cells. In contrast, inflammasome priming by LPS, a TLR4 ligand, was not blocked in TLR2−/−cells. These data show that MyrVP4/TLR2 signaling is sufficient for inflammasome priming but not activation.
In mice, intact viral RNA was required for cleavage of caspase-1 and production of mature IL-1β. The requirement of dsRNA for influenza-induced NLRP3 inflammasome activation has been shown previously29, 36, 37. However, in the present study, RV infection induced inflammasome activation in mouse bone marrow-derived macrophages which do not support viral replication31 and transient transfection of single-stranded viral RNA was sufficient for inflammasome activation in LPS-primed cells. These data provide a mechanism by which macrophages might rapidly initiate inflammasome activation in response to viral infection, without the need for viral replication.
Employing NLRP3−/−and IL-1β−/−mice as well as recombinant IL-1β receptor antagonist, we found that inflammasome activation was required for RV-induced airway eosinophilic inflammation and type 2 cytokine expression in HDM-sensitized and -challenged mice. Previous studies have examined inflammasome activation in mice with allergic airways disease, in combination with an infectious agent or other stimuli. Ovalbumin-sensitized mice infected with Chlamydia muridarum develop NLRP3 inflammasome activation and steroid-resistant allergic airway disease42. HDM-sensitized IL-1β−/−mice treated with dsRNA (to simulate a viral infection) demonstrate attenuated neutrophilic inflammation and Th2 cytokine expression, whereas caspase-1−/−mice show reduced eosinophilic inflammation and Th2 cytokine expression43, 44. However, in contrast to previous studies, we employed a physiologic pathogen that is a common cause of asthma exacerbations. To underline this point, we have found that, in bone marrow-derived macrophages, RV-induced TNF-α expression is TLR2/MyD88-dependent, in contrast to dsRNA-induced cytokine expression which is dependent on TLR331 . Thus, dsRNA may not be an accurate model of RV infection. Further, unlike previous studies, we also examined the effect of inflammasome blockade on airways responsiveness and viral load. Inflammasome activation was required for airways hyperresponsiveness and IL-1β blockade increased viral load.
Finally, while inflammasome activation was required for maximum type 2 inflammation after RV infection in allergic mice, we found that HDM in actual fact attenuated RV-induced inflammasome activation. This finding is consistent with previous data showing that inflammasome activation may be reduced in some asthmatics9. Thus, the contribution of inflammasome activation to airway inflammation may depend on the type and severity of asthma, combined with the burden of respiratory viral infection. It is also conceivable that the level of inflammasome activation, in combination with other cytokines, regulates the nature of the subsequent inflammatory response, with “high-dose” IL-1β contributing to expansion of type 1 innate lymphoid cells and IFN-γ production, and “low-dose” IL-1β contributing to expansion of type 2 innate lymphoid cells and IL-13 production45, 46.
We conclude that RV infection induces TLR2-dependent inflammasome activation in naïve mice, and also activates the inflammasome in mice with allergic airways disease. These data provide a new mechanism by which RV could contribute to the development of asthma exacerbations, and provide molecular targets of treatment.
Material and Methods
RV infection of mice.
Experiments were approved by the Institutional Animal Care and Use Committee. RV-1B (ATCC, Manassas, VA) was partially purified by ultrafiltration using a 100 kD filter and titered by plaque assay32. In some experiments. RV was inactivated by UV-light. C57BL/6, TLR2−/−(Jackson Laboratories, Bar Harbor, ME), NLRP3−/−or IL-1β −/−mice47, generally in a 1:1 male-to-female ratio, were inoculated intranasally under Forane anesthesia with 50 μl RV-1B (5×106 PFU/mouse) or sham HeLa cell lysate. Mice were sensitized and challenged by intranasal exposure to house dust mite extract (HDM, Greer Laboratories, Lenoir, NC) and infected with 50 μl RV-1B one day after exposure. Selected mice were treated intraperitoneally with 30 μg anti-IL-1β (R&D Systems, Minneapolis, MN) or 10 mg/kg IL-1 receptor antagonist (PeproTech, Rocky Hill, NJ).
Mouse model of RV-induced exacerbation of allergic airway inflammation.
Using a previously published protocol34, anesthetized mice were sensitized by intranasal exposure to house dust mite extract (HDM, 100 μg in 50 μl PBS, Greer Laboratories, Lenoir, NC). Controls received 50 μl PBS. Ten days later, mice were dosed intranasally with 10 μg of HDM in 50 μl of PBS on two consecutive days. One day after the last challenge, allergic and control mice were inoculated intranasally with 50 μl RV-1B as described above. Selected mice were treated intraperitoneally with 10 mg/kg human recombinant IL-1 receptor antagonist (PeproTech, Rocky Hill, NJ) after HDM treatment, 1 h before and 24 h after RV infection. This antagonist is effective against mouse IL-1 receptor.
Assessment of airway responsiveness.
Airway responsiveness was assessed by measuring changes in total respiratory system resistance after increasing doses of nebulized methacholine administered through an endotracheal tube39. Mechanical ventilation was conducted and total respiratory system resistance measured using a Buxco FinePointe operating system (Buxco, Wilmington, NC).
Analysis of lung inflammation.
Differential counts of BAL inflammatory cells were performed as described previously48. Lung sections were stained with H&E or Alexa Fluor-conjugated anti-mouse NLRP3 (Cell Signaling, Danvers, MA), anti-IL-1β (R&D), anti-CD68 and/or anti-F4/80 (Biolegend, San Diego, CA). Pathological categories of perivascular/peribronchiolar and alveolar inflammation were examined and scored on a scale of 0–4 (0 = no lesion, 1 = minimal: focal to multifocal infiltrates barely exceeding background; 2, mild: focal to multifocal infiltrates easily identified but of limited severity; 3 = moderate: multifocal to locally extensive infiltrates prominent but significant potential for increased severity; 4 = severe: locally extensive to diffuse infiltrates involving large portions of the section). In addition, the number of F4/80+IL-1β+ and F4/80+NLRP3+ cells in and around airways was quantified by NIH ImageJ software (Bethesda, MD). Four airways from one section per mouse were randomly selected for analysis.
After Trizol solubilization, purified RNA was processed for first strand cDNA and qPCR using reverse transcriptase and SYBR green qPCR reagents (ThermoFisher Scientific, Waltham, MA). To quantify virus particles, qPCR for positive-strand viral RNA was conducted using RV-specific primers and probes49. Primers used are described in Supplemental Table S1. IL-1β and IL-18 were measured by ELISA (R&D).
Cell culture.
Mouse bone marrow monocytes were isolated and cultured in L929 medium for 7 days as described31. Cells were infected with RV-1B at an MOI of 1 or 10, treated with 500 ng/mL synthetic myristoylated RV capsid protein VP4 (MyrVP4, GenScript, Piscataway, NJ) or primed with 100 ng/ml Escherichia coli O111:B4 LPS (Sigma-Aldrich, St. Louis). THP-1 human monocytic cells (ATCC) were infected with 1 MOI RV-1B, RV-16, RV-1A (ATCC) or transfected with full-length RV-1A genome or control single-stranded RNA using Lipofectamine (Thermo Fisher).
In-vitro RNA synthesis and transfection.
The RV infectious clone pMJ3-HRV-1A was described previously50. Full length viral RNA was generated using the MEGAScript T7 transcription kit (Thermo Fisher Scientific) and used to transfect human THP-1 cells using Lipofectamine (Thermo Fisher Scientific). A control single-stranded RNA was in-vitro synthesized using the plasmid pTRI-Xef provided in the MEGAScript T7 transcription kit. pTRI-Xef contains 1.85 kb of Xenopus elongation factor 1α gene.
Inflammasome priming and activation.
Lysates were subjected to Western blot assay using anti-mouse IL-1β (R&D), caspase-1 (Abcam, Cambridge, MA) and NLRP3 (Cell Signaling) or anti-human IL-1β (R&D) or caspase-1 (Abcam).
Macrophage depletion.
Depletion of alveolar macrophages was accomplished by intratracheal instillation of liposomes containing clodronate (dichloromethylenediphosphonic acid, disodium salt, Millipore Sigma, Burlington, MA), as previously described24. PBS-containing liposomes were used for control experiments. Liposomes were kept at 4°C under N2 until use. Depletion was performed 24 h before sham or RV infection by introducing 50 μl of clodronate- or PBS-containing liposomes intratracheally under Forane anesthesia.
Adoptive transfer of macrophages to the airways.
Mouse macrophages were isolated from either wild type or IL-1β mice and cultured in L929 medium. Macrophages were transferred to mice intratracheally at 106 cells per mouse 24 hours before rhinovirus infection27.
Data analysis.
Data are represented as mean ± standard error. Statistical significance was assessed by unpaired t-test, one-way or two-way ANOVA, as appropriate. Group differences were pinpointed by a Tukey multiple comparison test.
Supplementary Material
Acknowledgments
The authors thank Dr. Gabriel Núñez(University of Michigan, Ann Arbor, MI) for his gift of NLRP3−/−and IL1β −/−mice. This work was supported by NIH grant HL134369 (M.B.H).
Footnotes
Declarations of interest: none
References
- 1.Guo H, Callaway JB, Ting JP Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med 21, 677–687 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franchi L Eigenbrod, T., Núñez, G. Cutting Edge: TNF-α mediates sensitization to ATP and silica via the NLRP3 inflammasome in the absence of microbial stimulation. J Immunol 183, 792–796 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franchi L et al. Cytosolic double-stranded RNA activates the NLRP3 inflammasome via MAVS-induced membrane permeabilization and K+ efflux. J Immunology 193, 4214–4222 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He Y, Hara H, Núñez G Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem Sci 41, 1012–1021 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hastie AT et al. Analyses of asthma severity phenotypes and inflammatory proteins in subjects stratified by sputum granulocytes. J Allergy Clin Immunol 125,1028–1036 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu W et al. Mechanism of Th2/Th17-predominant and neutrophilic Th2/Th17-low subtypes of asthma. J Allergy Clin Immunol 139, 1548–1558 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simpson JL, Phipps S, Baines KJ, Oreo KM, Gunawardhana L, Gibson PG Elevated expression of the NLRP3 inflammasome in neutrophilic asthma. Eur Respir J 43, 1067–1076 (2014). [DOI] [PubMed] [Google Scholar]
- 8.Rossios C et al. Sputum transcriptomics reveal upregulation of IL-1 receptor family members in patients with severe asthma. J Allergy Clin Immunol 141, 560–570 (2018). [DOI] [PubMed] [Google Scholar]
- 9.Brickey WJ, Alexis NE, Hernandez ML, Reed W, Ting JP, Peden DB Sputum inflammatory cells from patients with allergic rhinitis and asthma have decreased inflammasome gene expression. J Allergy Clin Immunol 128, 900–903 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsukagoshi H, Sakamoto T, Xu W, Barnes PJ, Chung KF Effect of interleukin-1β on airway hyperresponsiveness and inflammation in sensitized and nonsensitized BrownNorway rats. J Allergy Clin Immunol 93, 464–469 (1994). [DOI] [PubMed] [Google Scholar]
- 11.Kobayashi T, Iijima K, Checkel JL, Kita H IL-1 family cytokines drive Th2 and Th17 cells to innocuous airborne antigens. Am J Respir Cell Mol Biol 49, 989–998 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliveira MA et al. The structure of human rhinovirus-16. Structure 1, 51–68 (1993). [DOI] [PubMed] [Google Scholar]
- 13.Corne JM et al. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet 359, 831–834 (2002). [DOI] [PubMed] [Google Scholar]
- 14.Greenberg SB, Allen M, Wilson J, Atmar RL Respiratory viral infections in adults with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med 162, 167–173 (2000). [DOI] [PubMed] [Google Scholar]
- 15.Johnston SL et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ 310, 1225–1229 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heymann PW et al. Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol 114, 239–247 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicholson KG, Kent J, Ireland DC Respiratory viruses and exacerbations of asthma in adults. BMJ 307, 982–986 (1993). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Triantafilou K, Kar S, van Kuppeveld FJ, Triantafilou M Rhinovirus-induced calcium flux triggers NLRP3 and NLRC5 activation in bronchial cells. Am J Respir Cell Mol Biol 49, 923–934 (2013). [DOI] [PubMed] [Google Scholar]
- 19.Shi L, Manthei DM, Guadarrama AG, Lenertz LY, Denlinger LC Rhinovirusinduced IL-1β release from bronchial epithelial cells is independent of functional P2X7. Am J Respir Cell Mol Biol 47, 363–371 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terajima M et al. Rhinovirus infection of primary cultures of human tracheal epithelium: role of ICAM-1 and IL-1beta. Am J Physiol 273, 749–759 (1997). [DOI] [PubMed] [Google Scholar]
- 21.Proud D, Gwaltney JM, Hendley JO, Dinarello CA, Gillis S, Schleimer RP Increased levels of interleukin-1 are detected in nasal secretions of volunteers during experimental rhinovirus colds. J Infect Dis 169, 1007–1013 (1994). [DOI] [PubMed] [Google Scholar]
- 22.Yoon HJ, Zhu Z, Gwaltney JM, Elias JA Rhinovirus regulation of IL-1 receptor antagonist in vivo and in vitro: A potential mechanism of symptom resolution. J Immunol 162, 7461–7469 (1999). [PubMed] [Google Scholar]
- 23.Kluijver JD et al. Interleukin‐1β and interleukin‐1RA levels in nasal lavages during experimental rhinovirus infection in asthmatic and non‐asthmatic subjects. Clin Exp Allergy 33, 1415–1418 (2003). [DOI] [PubMed] [Google Scholar]
- 24.Nagarkar DR et al. Rhinovirus infection of allergen-sensitized and -challenged mice induces eotaxin release from functionally polarized macrophages. J Immunol 185, 2525–2535(2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown GT, Narayanan P, Li W, Silverstein RL, McIntyre TM Lipopolysaccharide stimulates platelets through an IL-1β autocrine loop. J Immunol 191, 5196–5203 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Massip-Copiz M, Clauzure M, Valdivieso ÁG, Santa-Coloma TA Epiregulin (EREG) is upregulated through an IL‐1β autocrine loop in Caco‐2 epithelial cells with reduced CFTR function. J Cell Biochem 119, 2911–2922 (2018). [DOI] [PubMed] [Google Scholar]
- 27.Han M et al. Toll-like receptor 2–expressing macrophages are required and sufficient for rhinovirus-induced airway inflammation. J Allergy Clin Immunol 138, 1619–1630 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bentley JK et al. Myristoylated rhinovirus VP4 protein activates TLR2-dependent proinflammatory gene expression. Am J Physiol Lung Cell Mol Physiol doi: 10.1152/ajplung.00365.2018. (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allen IC et al. The NLRP3 inflammasome mediates in vivo innate immunity to influenza A virus through recognition of viral RNA. Immunity 30, 556–565 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chakrabarti A et al. RNase L activates the NLRP3 inflammasome during viral infections. Cell Host Microbe 17, 466–477 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saba TG, Chung Y,, Hong JY, Sajjan US, Bentley JK, Hershenson MB Rhinovirus-induced macrophage cytokine expression does not require endocytosis or replication. Am J Respir Cell Mol Biol 50, 974–984 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Newcomb DC et al. Human rhinovirus 1B exposure induces phosphatidylinositol 3kinase-dependent airway inflammation in mice. Am J Respir Crit Care Med 177, 11111121 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Q et al. MDA5 and TLR3 initiate pro-inflammatory signaling pathways leading to rhinovirus-induced airways inflammation and hyperresponsiveness. PLoS Pathog 7, e1002070 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toussaint M et al. Host DNA released by NETosis promotes rhinovirus-induced type-2 allergic asthma exacerbation. Nat Med 23, 681–691 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang H et al. AIM2 inflammasome is critical for influenza-induced lung injury and mortality. J Immunol 198, 4383–4393 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas PG et al. The intracellular sensor NLRP3 mediates key innate and healing responses to influenza A virus via the regulation of caspase-1. Immunity 30, 566–575 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ichinohe T, Lee HK, Ogura Y, Flavell R, Iwasaki A Inflammasome recognition of influenza virus is essential for adaptive immune responses. J Exp Med 206, 79–87 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tuthill TJ et al. Mouse respiratory epithelial cells support efficient replication of human rhinovirus. J Gen Virol 84, 2829–2836 (2003). [DOI] [PubMed] [Google Scholar]
- 39.Stokes CA et al. Role of interleukin-1 and MyD88-dependent signaling in rhinovirus infection. J Virol 85, 7912–7921 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Piper SC et al. The role of interleukin-1 and interleukin-18 in pro-inflammatory and anti-viral responses to rhinovirus in primary bronchial epithelial cells. PLoS One 8, e63365 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jackson DJ et al. Interleukin-18 is associated with protection against rhinovirus-induced colds and asthma exacerbations. Clin Infect Dis 60, 1528–1531 (2015). [DOI] [PubMed] [Google Scholar]
- 42.Kim RY et al. Role for NLRP3 inflammasome–mediated, IL-1β–dependent responses in severe, steroid-resistant asthma. Am J Respir Crit Care Med 196, 283–297 (2017). [DOI] [PubMed] [Google Scholar]
- 43.Mahmutovic Persson I, Menzel M, Ramu S, Cerps S, Akbarshahi H, Uller L IL-1β mediates lung neutrophilia and IL-33 expression in a mouse model of viral-induced asthma exacerbation. Respir Res 19, 16 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Menzel M, Akbarshahi H, Mahmutovic Persson I, Puthia M, Bjermer L, Uller L Caspase-1 deficiency reduces eosinophilia and interleukin-33 in an asthma exacerbation model. ERJ Open Res 3, 00047–2017 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bal SM et al. IL-1β, IL-4 and IL-12 control the fate of group 2 innate lymphoid cells in human airway inflammation in the lungs. Nat Immunol 17, 636–645 (2016). [DOI] [PubMed] [Google Scholar]
- 46.Ohne Y et al. IL-1 is a critical regulator of group 2 innate lymphoid cell function and plasticity. Nat Immunol 17, 646–655 (2016). [DOI] [PubMed] [Google Scholar]
- 47.Seo SU et al. Distinct commensals induce interleukin-1β via NLRP3 inflammasome in iInflammatory monocytes to promote intestinal inflammation in response to injury. Immunity 42, 744–755 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsai WC et al. Azithromycin blocks neutrophil recruitment in pseudomonas endobronchial infection. Am J Respir Crit Care Med 170, 1331–1339 (2004). [DOI] [PubMed] [Google Scholar]
- 49.Schneider D et al. Neonatal rhinovirus infection induces mucous metaplasia and airways hyperresponsiveness. J Immunol 188, 2894–2904 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quiner CA & Jackson WT Fragmentation of the Golgi apparatus provides replication membranes for human rhinovirus 1A. Virology 407, 185–195 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.