Abstract
Systemic lupus erythematosus (SLE) is characterized by a wide variety of manifestations and a difficult disease control in some patients. We present the case of a 51-year-old woman who presented with a flare of SLE including arthritis and pleuropericarditis that responded to neither leflunomide, methotrexate, nor high doses of prednisone. After initiating treatment with belimumab, the patient experienced a quick and notorious improvement. She remains stable to this day while continuing belimumab therapy.
Keywords: Systemic lupus erythematosus, belimumab, biological treatments, serositis, pleuropericarditis
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by a wide variety of manifestations and a great morbidity and mortality associated with its unpredictable course, uncontrolled activity, organ damage, and adverse side effects produced by its treatment, especially high doses of corticosteroids. The effective treatment of SLE still constitutes a challenge nowadays. Many studies have been conducted to find an effective biological agent to treat SLE. However, most of them have not achieved their primary endpoint and force physicians to use biological drugs as off-label agents when trying to control a refractory disease (1). Belimumab, a monoclonal humanized IgG antibody against B lymphocyte stimulator, which both decreases B cell number and modulates its function, is the first and unique biological drug approved for SLE treatment thus far (2). The exact role of belimumab in the SLE algorithm treatment is still to be determined.
Here, to the best of our knowledge, we present the first case described in the literature of SLE pleuropericarditis treated with belimumab as the first option of biological treatment. The case describes a patient with predominantly articular SLE manifestations who develops immune pleuropericarditis that remains refractory to treatment with two different immunosuppressants and high doses of corticosteroids. Belimumab is started with the resolution of serositis and the clinical and analytical improvement of SLE markers.
Case Presentation
We present the case of a 51-year-old woman diagnosed with rheumatoid arthritis in 2010 due to the presence of polyarthritis and treated with leflunomide (LEF) and low doses of prednisone. Written informed consent was obtained from the patient. In 2015, she received follow-up care in the rheumatology outpatient clinic where she was reassessed and diagnosed with SLE after fulfilling the 1982 American College of Rheumatology (ACR) criteria for SLE. The 1982 ACR criteria for SLE include arthritis, photosensitivity, oral ulcers, presence of antinuclear antibodies, anti-ds-DNA antibodies (ab), and lymphopenia <1500/mm3 on at least two occasions. She started treatment with hydroxychloroquine (HCQ) 400 mg/12 h combined with LEF 20 mg/day and low-dose prednisone with an irregular control, which justified changing the immunosuppressant therapy to methotrexate (MTX) 15 mg/week. At that time, she was also diagnosed as a carrier of antiphospholipid antibodies and received treatment with aspirin 100 mg/day.
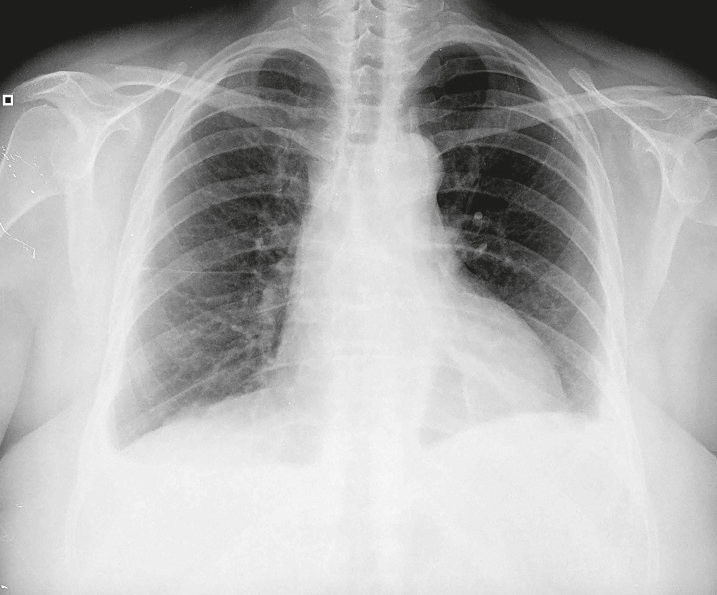
In November 2016, she presented with pleuritic chest pain, C-reactive protein (CRP) 3.08 (normal range 0.00–0.50) mg/dL, erythrocyte sedimentation rate (ESR) 42 (normal range 0–37) mm/h, and anti-ds-DNA ab 5 (normal range 0.1–4) UI/mL, with no alterations of the hemogram, the complement, or the kidney function. Her chest X-ray showed bilateral pleural effusion and an increased density in the lower left parenchyma (Figure 1). With the suspicion of pleuritis in relation to her autoimmune disease, the dose of prednisone was increased to 0.5 mg/kg/day (a total of 30 mg prednisone/day). Antibiotic treatment with amoxicillin and clavulanic acid was added. The patient evolved slowly but favorably, both clinically and analytically, with a progressive resolution of her pleuritis (CRP 3.28 mg/dL and ESR 15 mm/h).
Figure 1.
Chest X-ray showing bilateral pleural effusion
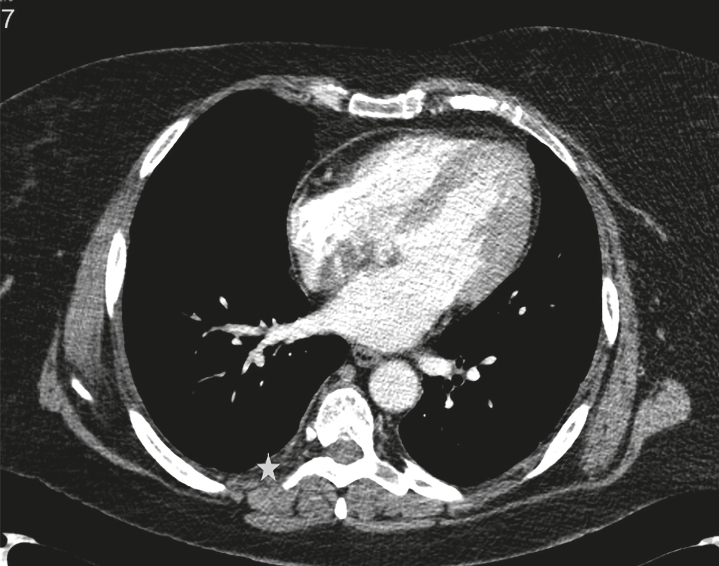
However, in January 2017, she had to be admitted to the emergency room due to a 2-day history of fever and dyspnea, as well as an increase in acute phase reactants (APR) and the presence of a new consolidation in the lower left lobe. She was diagnosed with pneumonia, and she received antibiotic treatment with levofloxacin. As part of the study, a chest computed tomography (CT) scan was performed to confirm the presence of a pneumonic consolidation in the left lower lobe, as well as mild bilateral pleural and pericardial thickening (Figure 2). Owing to only a partial improvement of symptomatology, in addition to high body mass index, lupus anticoagulant positivity, and subpleural images in the CT scan, a CT pulmonary angiography and a ventilation and perfusion lung scintigraphy were performed. Both tests ruled out pulmonary thromboembolism. Moreover, a fiberoptic bronchoscopy was performed without any signs of infection or malignancy. Infections by fungi, mycobacteria, Pneumocystis jiroveci, influenza, parainfluenza, adenovirus, enterovirus, rhinovirus, metapneumovirus, coronavirus, and bocavirus were ruled out after the analysis of bronchoalveolar lavage and diffuse bronchoscopic aspiration.
Figure 2.
Chest CT scan showing mild bilateral pleural (*) and pericardial thickening (arrow)
In April 2017, intravenous belimumab was started at a dose of 10 mg/kg/month as a corticosteroid-sparing agent in a patient with a predominantly articular SLE who had previously failed two immunosuppressants (LEF and MTX). After seven doses of belimumab, the patient improved clinically and analytically, with the disappearance of arthritis and chest pain and the complete resolution of radiological abnormalities in the chest X-ray and of pericarditis in the echocardiographic examination. Since belimumab was started, ESR and anti-ds-DNA ab levels were normal, with the persistence of CRP values only slightly above the reference range (CRP 1.51 mg/dL, ESR 5 mm/h, and anti-ds-DNA ab 3 UI/mL). SLE Disease Activity Index (SLEDAI) score decreased from 8 to 4, and a prednisone reduction from 30 mg/day to 15 mg/day was achieved. In March 2019, after 24 doses of intravenous belimumab and 1 dose of subcutaneous belimumab, the patient remains stable with no relapses of serositis symptoms during the follow-up period. In February 2018, MTX had to be restarted due to the presence of arthritis and as a corticosteroid-sparing treatment. However, after 4 months of treatment with MTX, the patient went into clinical remission and decided, on her own, to abandon MTX treatment. Currently, the patient remains asymptomatic with subcutaneous belimumab 200 mg/week and without prednisone. All markers of SLE activity remain low, with ESR 14 mm Hg, CRP 0.82 mg/dL, and anti-ds-DNA ab 2 UI/mL, and the SLEDAI score has decreased to 0.
Literature Review
Serositis, which includes both pleuritis, defined according to the 1997 ACR criteria for SLE, as a convincing history of pleuritic pain or rubbing heard by a clinician or evidence of pleural effusion, and pericarditis, defined as documented by electrocardiography, rub, or evidence of pericardial effusion, is a relatively frequent manifestation of SLE. Pleuropericarditis is considered an important SLE manifestation as proven by its inclusion in both the 1982 ACR criteria and the 2012 Systemic Lupus International Collaborating Clinics criteria for SLE diagnosis. Zhan et al. (3), and later Liang et al. (4), studied the prevalence and factors associated with serositis in patients with SLE, finding a prevalence of 16.8% and 17.9%, respectively. According to their results, serositis appears to be associated with nephropathy, interstitial lung disease, pulmonary hypertension, hypocomplementemia, leukocytopenia, thrombocytopenia, and increased anti-ds-DNA ab in the first study mentioned and with active lupus disease, fever ≥38 °C, and high D-dimer in the second study.
In our case, at the time of pleuropericarditis, the patient presented with positive anti-ds-DNA ab, increased APR, and fever associated with pneumonia. She had already received treatment with consecutive MTX and LEF together with HQC and high doses of glucocorticosteroids, with an irregular control of predominantly articular symptoms and only a discrete improvement of serositis symptomatology, with an ulterior relapse. After a thorough evaluation, belimumab was started according to the SLE guidelines, which consider that in a refractory and corticosteroid-dependent disease form, despite HCQ and at least two consecutive immunosuppressant drugs, a biological treatment could be prescribed (5). The specific use of belimumab is recommended in the absence of kidney or central nervous system involvement, requirements that our patient fulfilled (6).
After the introduction of belimumab, our results were in accordance with those of previous studies. We observed that belimumab permitted a better control of the disease activity in the short and medium term, with the negativization of anti-ds-DNA ab and APR, improvement of arthritis, disappearance of respiratory symptomatology, and resolution of radiological abnormalities. Belimumab also acted as a corticosteroid-sparing agent, with the ability to reduce corticosteroid intake to half its original dose and, later in combination with MTX, to none (2). Although in the majority of patients belimumab is used as an additional therapy to the standard one, in our particular case, the immunosuppressant therapy with MTX was discontinued when starting the biological treatment, with a good response of serositis manifestations but only a partial control of articular symptoms, which led to the restart of MTX later in combination with belimumab. However, after 4 months of treatment with MTX, the patient went into remission, and MTX was stopped again. Since then, the patient has been receiving maintenance treatment with belimumab in monotherapy for the last 9 months. Therefore, it remains unclear if antimalarials or other concomitant immunosuppressants could be withdrawn when starting belimumab, and this performance algorithm should be further studied to establish more determinant conclusions.
Predictors of response to belimumab have also been carefully evaluated and were taken into account in our case to select the better choice of treatment. They would include patients affected by an active disease with musculoskeletal and/or mucocutaneous manifestations, active serology, a disproportionate corticosteroid intake, and a relapsing–remitting course (7, 8).
There are limited cases described in the literature about the successful use of belimumab for SLE pleuropericarditis. In 2014, Jüptner et al. (9) reported two patients with active SLE pleuritis and arthritis who received off-label tocilizumab with a short and incomplete response and a subsequent flare. As a result, treatment was changed to belimumab which achieved an excellent response characterized by a normalization of complement levels, a reduction in anti-ds-DNA ab and SLEDAI values, and a nearly complete resolution of the patient’s clinical manifestations (9). In addition, Riancho-Zarrabeitia et al. (10) performed a study about their clinical experience with belimumab in a regional hospital where 11 patients with SLE were included. The clinical manifestations that the patients presented during the course of the disease were the following: joint involvement (100%), followed by cutaneous (81%), hematological (64%), renal (27%), pulmonary (9%), and cardiac (9%). Currently, to the best of our knowledge, this is the first case in the literature that described the successful use of belimumab as a first biological treatment option in SLE pleuropericarditis.
Conclusion
This case, although preliminary, appear to indicate that belimumab could have a great effect in controlling SLE activity and in allowing a reduction in corticosteroid intake. Whether this beneficial reaction remains durable in time is still to be determined. Therefore, despite the need for further studies to confirm our results, belimumab could constitute an effective alternative in the treatment of active SLE with predominant musculoskeletal manifestations and pleuropericarditis, and it should be taken into account when assessing this subgroup of patients.
Footnotes
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Design - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Supervision - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Resources - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Data Collection and/or Processing - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Analysis and/or Interpretation - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Literature Search - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Writing Manuscript - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.; Critical Review - I.C.B., T.C.S.M., S.C., F.C.D., F.O., J.M.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Gatto M, Saccon F, Zen M, Bettio S, Iaccarino L, Punzi L, et al. Success and failure of biological treatment in systemic lupus erythematosus: A critical analysis. J Autoimmun. 2016;74:94–105. doi: 10.1016/j.jaut.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 2.Tesar V, Hruskov Z. Belimumab in the management of systemic lupus erythematosus-an update. Expert Opin Biol Ther. 2017;17:901–8. doi: 10.1080/14712598.2017.1324846. [DOI] [PubMed] [Google Scholar]
- 3.Zhao J, Bai W, Zhu P, Zhang X, Liu S, Wu L, et al. Chinese SLE Treatment and Research group (CSTAR) registry VII: prevalence and clinical significance of serositis in Chinese patients with systemic lupus erythematosus. Lupus. 2016;25:652–7. doi: 10.1177/0961203315625460. [DOI] [PubMed] [Google Scholar]
- 4.Liang Y, Leng RX, Pan HF, Ye DQ. The prevalence and risk factors for serositis in patients with systemic lupus erythematosus: a cross-sectional study. Rheumatol Int. 2017;37:305–11. doi: 10.1007/s00296-016-3630-0. [DOI] [PubMed] [Google Scholar]
- 5.Calvo-Alén J, Silva-Fernández L, Úcar-Angulo E, Pego-Reigosa JM, Olivé A, Martínez-Fernández C, et al. SER consensus statement on the use of biologic therapy for systemic lupus erythematosus. Reumatol Clin. 2013;9:281–96. doi: 10.1016/j.reuma.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Kleinmann JF, Tubach F, Le Guern V, Mathian A, Richez C, Saadoun D, et al. International and multidisciplinary expert recommendations for the use of biologics in systemic lupus erythematosus. Autoimmun Rev. 2017;16:650–7. doi: 10.1016/j.autrev.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 7.van Vollenhoven RF, Petri MA, Cervera R, Roth DA, Ji BN, Kleoudis CS, et al. Belimumab in the treatment of systemic lupus erythematosus: high disease activity predictors of response. Ann Rheum Dis. 2012;71:1343–9. doi: 10.1136/annrheumdis-2011-200937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gatto M, Iaccarino L, Zen M, Doria A. When to use belimumab in SLE. Expert Rev Clin Immunol. 2017;13:737–40. doi: 10.1080/1744666X.2017.1324784. [DOI] [PubMed] [Google Scholar]
- 9.Jüptner M, Zeuner R, Schreiber S, Laudes M, Schröder JO. Successful application of belimumab in two patients with systemic lupus erythematosus experiencing a flare during tocilizumab treatment. Lupus. 2014;23:428–30. doi: 10.1177/0961203314520844. [DOI] [PubMed] [Google Scholar]
- 10.Riancho-Zarrabeitia L, Villa Blanco I, Santos-Gómez M, Aurrecoechea E. Belimumab in systemic lupus erythematosus: Experience in clinical practice settings in a regional hospital. Reumatol Clin. 2018 Mar 16; doi: 10.1016/j.reuma.2018.02.004. doi: 10.1016/j.reuma.2018.02.004. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]