After announcement and implementation of the Medicare Hospital Readmissions Reduction Program (HRRP), 30-day readmissions declined rapidly among seniors with heart failure (HF) while 30-day mortality rose (3). This raised questions about whether the policy is responsible, since lower HF readmission rates have historically been associated with higher mortality (4). Because penalized hospitals faced more pressure to reduce readmissions and exhibited larger declines, we compared trends in HF mortality at penalized and non-penalized hospitals nationally (2).
We performed interrupted time-series analyses of risk-adjusted 30-day all-cause mortality and unplanned readmission rates during “pre-HRRP” (1/2007–3/2010), “anticipation” (4/2010–9/2012), and “penalty” (10/2012–1½014) periods. Subjects included Medicare beneficiaries age ≥65 with index discharges for HF, with HRRP exclusions. Study hospitals were eligible for the HRRP in FY2013 or FY2014. Data sources included 2007–2014 Medicare Provider and Analysis Review, Master Beneficiary Summary, Provider of Services, and HRRP payment adjustment datasets (1). The unit of analysis was an index discharge. We used regression models to estimate changes in outcomes under the HRRP relative to a linear pre-HRRP time trend, allowing changes in outcomes and pre-HRRP trends to differ by penalty status. Models controlled for patient characteristics, season, and hospital fixed effects, and accounted for clustering within hospitals.
To test whether outcomes changed under the HRRP, we used the regression estimates to compare observed and projected outcomes (Δ) at penalized and non-penalized hospitals during the penalty period. To assess whether changes differed between penalized and non-penalized hospitals, we compared their observed-to-projected differences (ΔΔ). These comparisons are a robust way of testing whether the slope and intercept of time trends changed at any point after the pre-HRRP period.
Among 3,256 eligible hospitals, 2,214 (68.00%) incurred penalties in FY2013. Of 3,009,296 index discharges across the study periods, 2,248,665 (74.72%) occurred at penalized hospitals. The Figure displays regression estimates graphically, plotting observed risk-adjusted outcomes along with projections of what outcomes would have been during anticipation and penalty periods without the HRRP.
Figure 1. Observed and Projected Rates by Hospital Penalty Status.
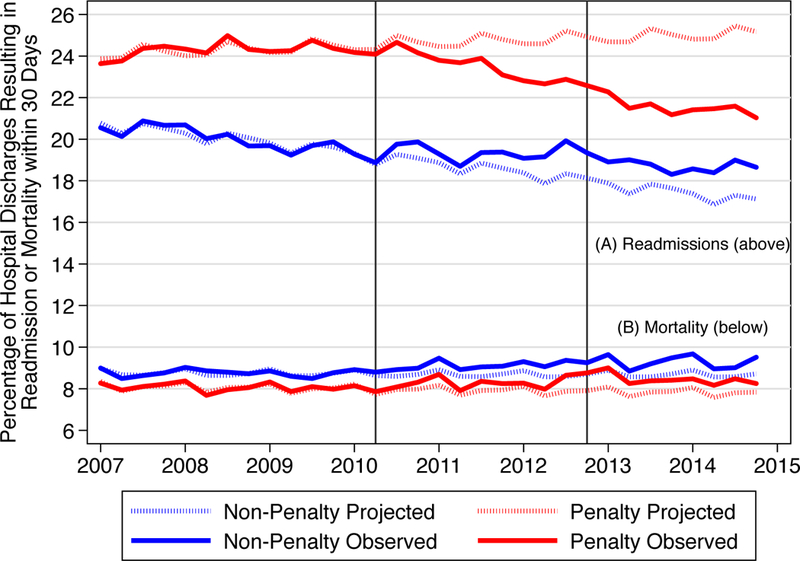
A Readmissions
B Mortality
Figure 1 plots observed risk-adjusted HF readmission rates (Panel A) and mortality rates (Panel B) by quarter-year as well as projected rates that were estimated using regression models to represent trends in the absence of the HRRP. Rates are displayed separately for penalty and non-penalty hospitals. Results show divergent readmission trends by penalty status, with decreased readmissions at penalized hospitals and increased readmissions at non-penalized hospitals. In contrast, mortality trends were similar at penalized and non-penalized hospitals. These findings suggest that factors other than the HRRP may have contributed to rising mortality during this period, particularly at non-penalized hospitals.
Mortality:
Pre-HRRP rates were 8.08% at penalized hospitals and 8.76% at non-penalized hospitals. After announcement of the HRRP, observed mortality rates rose relative to pre-HRRP trends, exceeding projections by 0.62 percentage points (Δ, 95% CI 0.30 to 0.94, P<0.001) at penalized hospitals and 0.60 points (Δ, 95% CI 0.01 to 1.19, P=0.047) at non-penalized hospitals by the penalty period. Increases were similar at penalized and non-penalized hospitals (ΔΔ 0.02 percentage points, 95% CI −0.65 to 0.70, P=0.949).
Readmissions:
Pre-HRRP rates were 24.26% and 20.07% at penalized and non-penalized hospitals, respectively. After announcement of the HRRP, observed readmission rates declined relative to pre-HRRP trends at penalized hospitals, reaching 3.35 percentage points (Δ, 95% CI 3.90 to 2.81, P<0.001) below projections by the penalty period. At non-penalized hospitals, rates decreased during the pre-HRRP period and stabilized during the anticipation period, such that by the penalty period, readmissions exceeded projections by 1.27 percentage points (Δ, 95% CI 0.44 to 2.10, P=0.003). Declines relative to projections were 4.62 percentage points (ΔΔ, 95% CI 5.62 to 3.63, P<0.001) larger at penalized than non-penalized hospitals.
The fact that HF readmissions declined at penalized hospitals but did not decline at non-penalized hospitals suggests that they responded differently to the HRRP. By contrast, mortality rose similarly at penalized and non-penalized hospitals. Effective responses to the HRRP, such as improving transition-related care, could reduce both readmissions and mortality. Ineffective responses may create barriers to inpatient care, decreasing readmissions but potentially increasing mortality.
It’s tempting to attribute rising HF mortality to the HRRP. However, the similarity in mortality trends at penalized and non-penalized hospitals does not support the hypothesis that the HRRP led to increased mortality, given the divergent trends in readmissions. In this context, any conclusion that the HRRP increased mortality at penalized hospitals is speculative.
A secular shift in the HF population, not fully accounted for by standard risk-adjustment techniques, could be contributing to parallel increases in mortality at penalized and non-penalized hospitals. Age-adjusted mortality rates in patients with HF increased sharply from 2012 to 2014, irrespective of setting, and more of these deaths were from non-cardiovascular causes (5). The causes of rising mortality among recently discharged patients with HF warrant further investigation.
Acknowledgements:
Margaret Kelley, MSEd, Cedars-Sinai Medical Center; Jillian Wallis, PhD, University of Southern California; and Zhiyou Yang, BS, University of Minnesota, contributed to the research effort.
Funding Source: The Agency for Healthcare Research and Quality (R01 HS024284) and National Institute of Aging (R01AG046838)
Abbreviations:
- HF
heart failure
- HRRP
Hospital Readmissions Reduction Program
Footnotes
Disclosures: The authors have no conflicts of interest related to this work.
References
- 1.Centers for Medicare & Medicaid Services, Hospital Readmissions Reduction Program. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed 09/28, 2017.
- 2.Desai NR, Ross JS, Kwon JY, et al. Association between Hospital Penalty Status under the Hospital Readmission Reduction Program and Readmission Rates for Target and Nontarget Conditions. JAMA. 2016;316(24):2647–2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Allen LA, Bhatt DL, et al. Association of the Hospital Readmissions Reduction Program Implementation with Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiology. 2018;3(1):44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between Hospital Readmission and Mortality Rates for Patients Hospitalized with Acute Myocardial Infarction, Heart Failure, or Pneumonia. JAMA. 2013;309(6):587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ni H, Xu J. Recent Trends in Heart Failure-Related Mortality: United States, 2000–2014. NCHS Data Brief. 2015(231):1–8. [PubMed] [Google Scholar]


