Abstract
Three-dimensional (3D) printing has recently emerged as a new technique in various liver-related surgical fields. There are currently only a few systematic reviews that summarize the evidence of its impact. In order to construct a systematic literature review of the applications and effects of 3D printing in liver surgery, we searched the PubMed, Embase and ScienceDirect databases for relevant titles, according to the PRISMA statement guidelines. We retrieved 162 titles, of which 32 met the inclusion criteria and are reported. The leading application of 3D printing in liver surgery is for preoperative planning. 3D printing techniques seem to be beneficial for preoperative planning and educational tools, despite their cost and time requirements, but this conclusion must be confirmed by additional randomized controlled trials.
Keywords: Three-dimensional printing, Three-dimensional models, Liver, Surgery, Hepatic phantom models
Core tip: Three-dimensional printing is an emerging technology that seems to have useful applications in various medical fields. The most thoroughly studied applications are in medical education and preoperative planning. However, the financial and time requirements for its use remain issues to be resolved. In this Minireview, we analyze the uses of three-dimensional printing models which are reported in the literature, with special emphasis on their role in surgical education in hepatic surgery.
INTRODUCTION
Three-dimensional (3D) printing is a rapid prototyping additive manufacturing technology that offers the opportunity to create numerous artificial parts and objects, made of different materials with various mechanical and physical properties[1,2]. The first 3D printed object was reported by Hideo Kodama in 1982. Since then, the technological aspects of 3D printing procedures have achieved an exponential development rate and, nowadays, big specialized companies, as well as individuals with their personal printers, can construct a variety of 3D objects, ranging in cost and quality depending on their intended use. 3D printing is an emerging technological achievement that could be deployed for a variety of applications in many medical fields, such as preoperative planning and medical education. This state-of-the-art technology displays certain advantages against older techniques, and seems to overcome some existing limitations, although there are still some drawbacks to be resolved[3-5]. 3D printed models seem to be capable of satisfying the needs for tactile and spatial perception of human anatomical structures[6,7]. Thus, they can be used to create 3D organ models for spatial and anatomical understanding, so that surgeons can achieve a better preoperative plan and prepare their surgical manipulations on 3D, graspable models[4,6]. 3D printing also provides optimized strategies for device testing[6] and serves educational purposes[8-10]. One of the most prominent medical applications of 3D printing is the development of medical devices and instru-mentation[4,9]. 3D printing appears to be a significantly useful and cost-effective technique compared to traditional cadaveric models. Surgeons can have an accurate optical and tactile sense of the structures, and perform complex operations on them[6,11,12]. Moreover, the use of additive manufacturing technologies in tissue engineering has been recently explored with revolutionary results. Many materials are used to fabricate a scaffold and then print functional cells onto it in order to mimic human tissue, which is a process called bioprinting[13,14].
Liver diseases, and especially those requiring surgical interventions, have led the way for the implementation of 3D printing techniques for many applications. Liver resection is the “gold standard” procedure in liver cancer that guarantees successful treatment. Despite technological improvements, liver resections remain a challenging area, especially for young surgeons. Although the knowledge of liver anatomy is essential for safe surgical resections, there are many anatomical variations. To perform an accurate hepatic resection, knowledge of the anatomical relationships among the branches of Glisson’s sheath, the hepatic veins and the tumor is crucial[15]. Magnetic resonance imaging (MRI) and computed tomography (CT) are conventional diagnostic methods that estimate the location of the lesions and their relationship with neighboring structures, and also provide 2-dimensional images. Virtual and Augmented Reality tools can possibly offer a more comprehensive alternative for 3D visualization, but still lack the ability to provide tactile feedback. Advanced navigation systems during liver resections can provide us with some help, but they demonstrate numerous limitations while maintaining a relatively high cost[16]. 3D printing techniques provide an effective solution for preoperative planning, by creating precise, patient-specific, graspable, 3D printed models of organs and lesions based on imaging data. While liver surgery can be challenging, and requires technical excellence and experience, implementation of a 3D printed pre-operative model seems to be very promising[13]. The implementation of 3D objects in medical education and surgical training also seems promising, as it provides live models that the trainees can handle and better comprehend[17,18]. In the present study, we analyze the studies that report the applications and the outcomes of 3D printing technologies in liver surgery, with special emphasis on preoperative planning and surgical education.
BASIC PRINCIPLES OF 3D PRINTING
3D printing is similar to conventional inkjet printing. It is a process of layering a material that initially has polymeric properties (or reaches a fluid state through heat), horizontally deposited and solidified, either by cooling or by ultraviolet light irradiation, to eventually create a complete 3D model. Every horizontal section of the final printed product closely resembles the way images of an axial or magnetic tomography are acquired. In 3D printing, instead of having a detection level that records the different densities corresponding to the different web structures between the irradiation head and its recorder, the print head composes an artefact in three dimensions.
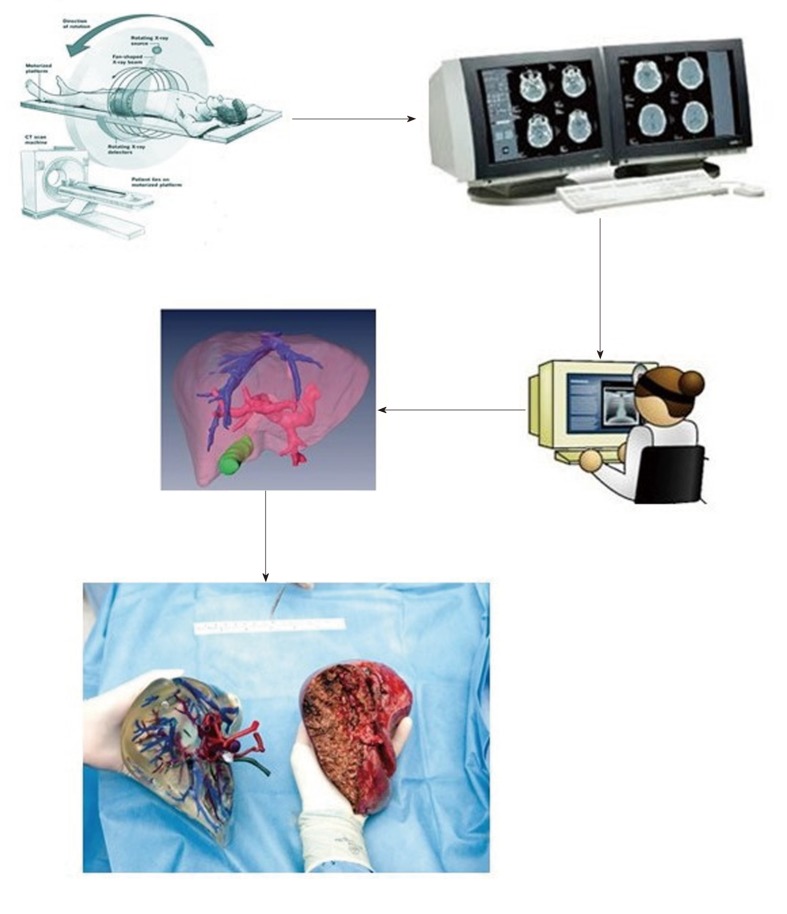
The resemblance of how a printed item is created by the process of reconstituting a CT scan helps physicians' understanding of both the printing process and its necessity in both medicine and surgery. CT and MRI scans are the most frequent preoperative examinations performed during the investigation of many pathological conditions, and guide the treating physician in finding the optimal therapeutic approach. However, the nature of CT is completely different from the 3D reality, and the physician's perception is constrained by the two-dimensional representation of sequential tomography images, which often result in the erroneous assessment of an existing disease state. CT and MRI data files (Digital Imaging and Communications in Medicine, DICOM format) were usually stored in CAD software (©Google sketchup). After isolating the relevant structures in each image set, 3-D volume reconstruction was performed. The final model was saved in the STL format. This extension STL supported the visualization of the model as a fully rotated virtual 3-D representation (360° on the x, y and z axes). A physical model of the processed 3-D digital model was created by a 3-D printer using commercially available polymeric filament materials. In all studies, “Digital Imaging and Communications in Medicine” (DICOM) files from MRI or CT tomography are reconstructed using computer-aided design (CAD) drawings software. Digital 3-D objects are sent to a 3-D printer, and 3-D models are then ready for use[3] (Figure 1).
Figure 1.
Long way from bedside to three-dimensional printed objects.
LITERATURE REVIEW
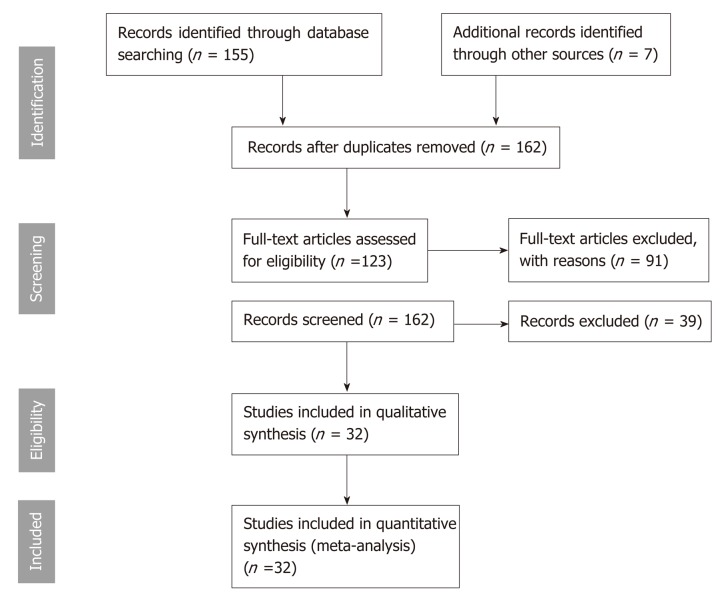
We performed a thorough review of the literature in accordance with PRISMA statement guidelines, using the PubMed, Embase and ScienceDirect indexing databases[19]. “3D printing”, “three-dimensional printing” and “rapid prototyping”, in combination with “liver”, “hepatic” or “surgical”, were used as search terms to identify relevant titles. We included only original papers written in English and published between January 2008 and August 2018. Moreover, we excluded the semantically irrelevant studies that did not refer to the use of 3D printing in liver surgery, based on the content of the abstract and the full text. The studies involving non-human subjects, as well as those referring to 3D bioprinting, were also excluded (Figure 2).
Figure 2.
PRISMA statement chart.
CURRENT STATUS AND CHALLENGES OF 3D PRINTING IN HEPATIC SURGERY
Data extraction and appraisal
The initial search retrieved 162 titles. Two expert reviewers screened the papers independently, and after the removal of studies not meeting the inclusion criteria, 32 full-text papers were included (Figure 2). All included papers refer to 3D printing applications strictly related to liver surgery. Characteristics, such as the study type, the field of application, the study setting, the clinical or practical outcome and the time and cost required, were extracted and are presented (Table 1).
Table 1.
Report of studies referring to 3D printing applications in liver diseases
| Authors[REF], year | Study type | Field of application | Imaging tools | Outcome |
| Zein et al[19], 2013 | Case series | PP | CT and MRI | Accurate in providing liver volume and size |
| measurement | ||||
| Takagi et al[20], 2014 | Case report | PP, TP | CT | Reported reproducibility of the model and possible future aid to surgical procedures |
| Igami et al[21], 2014 | Case report | PP | CT | Helpful in preoperative planning. Detects small tumors invisible with intraoperative US |
| Watson[36], 2014 | Case series | ET | CT and MRI | Ability of creating patient-simulated 3D printed |
| liver models at low cost | ||||
| Baimakhanov et al[22], 2015 | Case report | PP (transplantation) | CT | Helpful in preoperative planning and surgical training |
| Xiang et al[23], 2015 | Case report | PP (hepatectomy for tumor) | CT | Helpful in preoperative planning |
| Dhir et al[33], 2015 | Cohort study | ET, TP | MRCP | Accurate understanding liver anatomy |
| Souzaki et al[24], 2015 | Case report | PP | CT | Assists surgical planning understanding of the anatomy |
| Soejima et al[25], 2016 | Case report | PP | CT | Useful for small infants or neonates Realistic liver graft that is helpful in optimizing the procedure |
| Leng et al[26], 2016 | Case report | PP | CT | Could be useful in reducing radiation dose and detecting small liver lesions |
| Kong et al[35], 2016 | RCT, Cohort study | ET, TP | CT | Αnatomy teaching and significantly improved knowledge |
| Kong et al[34], 2016 | RCT, Cohort study | ET, TP | CT | Τeaching of hepatic segments |
| Burdall et al[41], 2016 | Cohort study | TP | CR, MRI | Scored 5.6/10 for fidelity, 6.2/10 for complexity and 7.36/10 for usefulness. All would suggest it and think it is reproducible |
| Takao et al[42], 2016 | Case series | TP | CT | High accuracy of 3D |
| Koganemaru et al[45], 2016 | Case report | PP | CT | Successful embolization and follow-up markers |
| Javan et al[37], 2016 | Case series | ET | CT | Useful in comprehending difficult anatomical structures |
| Witowski et al[12,27], 2017 | Case report | PP, ET | CT | Useful for planning procedures like hepatic resection and for educational purposes. |
| Kuroda et al[15], 2017 | Case series | PP | CT | Successful resection |
| Madurska et al[28], 2017 | Case report | PP | CT, MRI | Anatomical structures and lesions were clearly demonstrated |
| Oshiro et al[29], 2017 | Case report | PP | CT | The surgical procedure was easier, and the visibility of small tumors was improved |
| Perica et al[17,30], 2017 | Case report | PP | CT | Possible benefit in preoperative planning and intraoperative guidance |
| Andolfi et al[31], 2017` | Case report | PP ET, PE | VR | Clearer observations of the relationship between the mass and blood vessels |
| Trout et al[46], 2017 | Case series | PP | CT, MRI | A new technique to standardize hepatic sectioning was used |
| Weng et al[47], 2017 | Case report | PP, TP | CT, MRI | Positive comments from relatives and experts |
| Choi et al[43], 2017 | Cohort study | TP | CT, US | No significant difference in tumor size was found between the CT images and 3D model measured with US |
| Bücking et al[44], 2017 | Case series | TP | CT | High accuracy in fidelity |
| Igami et al[32], 2017 | Case report | PP | CT | The 3D printed model was useful in determining the resection line |
| Yang et al[48], 2018 | Cohort study | PE | CT | Parental understanding of basic liver anatomy |
| Li et al[38], 2018 | RCT | ET | CT | The 1st group, trained with the 3D printed model |
| Yang et al[39], 2018 | RCT | ET | CT | Better understanding liver anatomy |
| Javan et al[40], 2018 | Case report | ET | CT, MRI | Abscess drainage, artery embolization, and catheter placement procedures were well-exhibited |
| Tang et al[49], 2018 | Case report | VR | CT | Navigation was effective, although stability in tracking was not satisfactory |
3D: Three-dimensional; PP: Preoperative planning; ET: Education and training; PE: Patient education; TP: Evaluation of technical properties; RCT: Randomized controlled trial; CT: Computed tomography; MRI: Magnetic resonance imaging; LDLT: Living donor liver transplantation; MRCP: Magnetic resonance cholangiopancreatography; VR: Virtual reality; AR: Augmented reality; 2D: Two-dimensional; US: Ultrasound.
Preoperative planning is the leading application of 3D printing technology. Fifteen of the 32 studies refer to the utilization of 3D printed organs, based on the patients’ CT and MRI imaging data, to establish a better understanding of the lesions and the surrounding structures pre-operatively[16,20-33]. Ten studies refer to the use of 3D printed objects for educational uses[28,32,34-41], while seven studies describe and evaluate the technical properties of 3D printed models[34-36,42-45]. Other uses of 3D printing techniques account for six of the included studies[32,46-50]. Additionally, 20 of the studies were case reports, reporting the use or the properties of one 3D printed model, while seven were case series, involving more than one object. There were a limited number of cohort studies and randomized controlled trials (RCT), constituting only seven and four of the included studies, respectively. Cohort studies quantitatively explore the characteristics of a group of 3D printed models or of a cohort of patients/trainees where a 3D printing method is employed. RCTs compare the outcome (clinical or educational) of a 3D printing method to another conventional one. Some of the studies described more than one application field using different study designs, and thus are included in more than one category. The results are summarized (Table 2).
Table 2.
Cross-tabulation of the study characteristics
| Field of application |
Type of study |
Sum | |||
| Case report | Case series | Cohort studies | RCT | ||
| Preoperative planning | 13 | 2 | 0 | 0 | 15 |
| ET | 3 | 2 | 1 | 4 | 10 |
| TP | 0 | 2 | 5 | 0 | 7 |
| Other | 4 | 1 | 1 | 0 | 6 |
| Sum | 20 | 7 | 7 | 4 | |
ET: Education and training; TP: Evaluation of technical properties; RCT: Randomized controlled trial. Five of the studies belong to more than one application group, and they display different study types for each application, thus belonging to more than one cell.
Principles of function, and requirements of 3D printing
In the majority of the cases, 3D printers are “fed” with real patients’ data obtained from CT and MRI imaging files. In particular, 26 of the 32 studies used CT-derived images as the pool of data for the printer. In four of the 26 cases, the use of MRI imaging was included. One study did not clarify the source of the 3D model’s data, while the remaining five studies used alternative sources of data. The segmentation of the images, and the conversion of the data to a “3D-printer-friendly” format, is a time-consuming procedure, lasting from a few hours to a few days, and can be performed by a variety of different software systems[18]. An .STL file, which is compatible with the majority of 3D printers, is produced. The printer uses the .STL file to construct a 3D artificial object, which simulates the shape of the individual’s structures with precision. There is a variety of different 3D printers, each one compatible with specific fabrication materials, selected according to the desired application. Both conventional, personal 3D printers and professional, sophisticated 3D printing systems from big companies were used. Printing time can also be time-consuming. Different structures, such as the biliary tract, gallbladder, vessels, parenchyma and tumor, are manufactured with different materials and colored in different colors, a procedure often performed manually. In most cases, the parenchyma is transparent to allow visibility of the inner structures, while in some cases it is not printed at all. Depending on the system employed, the materials used, the size and the complexity of the printed object, the time necessary for segmentation, conversion and printing, as well as the economic cost can vary substantially[13,17,18]. Eighteen studies do not provide clues about the time required, and 14 studies do not refer to the cost of printing. Neither the cost, nor the time requirements are included in 11 of the studies. The economic data and time information from the rest of the studies are inhomogeneous and of poor quality. We can roughly say that the whole procedure time ranges from 1-3 d, although there are many factors that determine this variable, and significant deviations are observed[28,38]. The cost also displays a wide range, depending on the method used and the size of the object. Seven studies use more economical settings at a cost of around $100, four studies reach a cost of approximately $400-$600, and four studies use high accuracy materials and techniques that exceed the cost of $1000 (Table 1). However, there are also numerous factors, such as the cost of the dyes, the materials and the handmade work cost, that can drastically affect the cost and are vaguely explained in most of the studies.
Preoperative planning
Preoperative planning is the most popular application of 3D printing in liver surgery, and is referred to in 15 (47%) of the studies. The authors describe the potent use of 3D printed models of the patients’ organs in helping them better understand the lesions and the surrounding structures, as well as plan a more efficient surgical strategy. The individualized, artificially manufactured liver replicates hold many advantages, such as the tactile feedback, the ability to distinctly demonstrate the different structures by using different colors, and the ability to reveal small lesions that could be invisible intraoperatively[22]. However, there are also drawbacks regarding the cost and the time they require[13,18]. Eleven of the studies describe its use in tumor resection and partial hepatectomy, while in one of them it is mentioned that the surgery was abandoned, as the 3D printed model revealed that the tumor was unresectable[32]. One study describes the use of 3D printing for reducing the radiation dose and detecting small tumors[27], while three studies exhibit the usefulness of 3D printing in liver transplantations[20,23,26]. The majority of the studies referring to preoperative planning with 3D printing are case reports (13 of the 15 studies, 87%)[21-33], while there are also two (13%) case series, one with six subjects (three organ donors and three LDLT recipients), and the other with two[16,20].
Most of the studies report good results regarding the usefulness of 3D printing in preoperative planning, although there is no objective evidence for any significantly beneficial clinical outcome, as there are no RCTs that could compare the outcome of these applications with the more traditional ones. Zein et al[19] was the first to describe the application of 3D printing in liver surgery and the crucial field of transplantation. This study employed 3D printed models to visualize the donors’ and recipients’ livers, and used them to both identify better anatomical landmarks and optimize preoperative planning. It is mentioned that the mean errors of the measurements are < 4 mm for the whole liver and < 1.3 mm for the diameter of the vessels. In 2014 and 2015, the number of publications concerning the use of 3D printing in preoperative planning for liver surgery began to rise. There were three studies advocating the beneficial role of 3D printing in partial hepatectomy for tumor removal[21,22,24], one study testing these methods in pediatric patients with malignant tumors[25], and also one study concerning transplantation[23]. Soejima et al[25] tried to use a 3D printed model to simulate the liver of a 11-mo-old female receiving LDLT for biliary atresia after a failed Kasai procedure, as well as the liver of the donor father. The results were reported as encouraging. Leng et al[26] developed a method, involving 3D printed liver models, to reduce radiation dose and detect small liver lesions. In 2017, there were six original papers that described the beneficial effects of 3D printing in the preoperative planning of liver surgeries[16,28-32], while no similar studies were published in 2018. Although these studies clearly explain the concept of involving 3D printing in hepatic surgery, and the opinions are expressed by prominent professionals, they have been designed as case reports or case series, so it is therefore impossible to objectively compare their results to another preoperative planning method. Moreover, there is insufficient information in most of the studies concerning the time and cost requirements that would allow for the accurate evaluation of their overall efficiency in the context of these two critical factors.
Education and training
Both student education in liver anatomy and resident training in liver surgical techniques with the use of 3D printed models are the second most widely studied application. Ten studies refer to this field, five of which were designed as case reports or case series[28,32,37,38,41], one was an observational cohort study[34] and four were RCTs[35,36,39,40]. The case reports and case series state that 3D printed models could help in both the understanding of liver anatomy and surgical training, but fail to provide objective evidence. Dhir et al[33] was the first to use 3D printed liver models to train a cohort of 15 individuals in EUS-guided biliary drainage (EUS-BD) and, moreover, to measure the educational outcomes. The success rates were: 100% for needle puncture, 82.35% for wire manipulation and 80% for stent placement. However, the more experienced trainees were found to score lower in stent placement. This may be attributed to the small sample size that may not have supported safe comparison tests. Two RCTs were published in 2016[35,36], and two in 2018[39,40], comparing the educational impact of 3D printing to more conventional strategies. Kong et al[34] randomized 61 medical students into three cohorts: the 1st was trained in 3D printed models, the 2nd in 3D virtual models on computers and the 3rd in traditional anatomy atlases. The results favored both 3D printed and virtual models against the traditional atlases. However, the sample was small, and there was no cost analysis to the use of 3D printing against 3D virtual methods. In another study that same year, Kong et al[35] randomized 92 students into four groups, and trained them in different settings: The 1st was trained on a 3D printed model with hepatic segments without parenchyma, the 2nd on a 3D printed model with hepatic segments with transparent parenchyma, the 3rd on a biliary tract model with segmental partitions and the 4th on traditional anatomic atlases. In general, the 3rd group was found to have better results, although the samples in the randomized groups may also lack enough statistical power. Li et al[38] tried to use 3D printed models against virtual, computer-based 3D models in order to train 20 individuals in choledochoscopy. Although the randomized sample was also small, the design was sophisticated, and the results showed 3D printed models to be superior. Yang et al[39] evaluated the educational impact of 3D printed models against 3D virtual models and CT-based tools, and found them to be superior. These studies provide significant evidence that 3D printing could be applied in education and training in liver surgery, although they may have some methodological weaknesses.
Evaluation of technical properties
There are also a number of studies that aim to evaluate the technical properties of 3D printed models, such as their accuracy in simulating the real organ. There are seven published studies, two of which are case series[43,45] and five of which are observational cohort studies[34,36,36,42,44]. The case series mention high accuracy and fidelity of the 3D printed models when compared with the CT-derived models. Choi et al[43] printed 20 CT-based 3D livers with tumors, and measured the sizes of the anatomical structures with US. The results were not significantly different from those derived from CT, indicating high accuracy. Burdall et al[41] constructed a liver-like base with a cuboid slot in which a sponge with a green balloon, simulating the gallbladder, was placed. This setting was evaluated by ten trainees for its possible educational effect, and scored high for fidelity, complexity, usefulness and reproducibility. Dhir et al[33], Kong et al[34] and Kong et al[35], except for measuring the differences in the educational impact between the different cohorts of trainees, also employed independent teams of experts to quantitatively evaluate the settings. The results showed 3D printed models to be equal to or more satisfactory than computer-based virtual 3D models, and better than older, traditional strategies.
Additional applications
Additional uses of 3D printing in liver surgery are described in six studies. Andolfi et al[31] and Yang et al[48] describe the effect 3D printed liver models can have on patient education. They can enlighten the patients about their condition, and contribute to the facilitation of a better understanding and patient-physician collaboration. Tang et al[49] proposes the use of 3D printed models when training in AR-assisted endoscopy. Although the setting and equipment were described thoroughly, there were no quantitative variables in the study that could measure the benefit of this method. Weng et al[47] describes an alternative use of 3D printing. 3D printed objects were used to replace the heart, the kidneys and the liver of a brain-dead patient whose organs were removed for transplantation. In this study, the motives and the relevant ethical issues are explained, as well as the cost and the procedure. Koganemaru et al[45] reported the use of a CT-based, 3D printed copy of a portacaval shunt following transplantation, to better understand the complication and decide the embolization technique and material. Additionally, Trout et al[46] described a 3D printing-based technique for applying better sectioning to explants, resulting in better pathology results.
Impact of 3D printing technology in the era of hepatobiliary surgery
In this systematic review, we analyzed and reported the findings of 32 original studies concerning the role of 3D printing models in liver surgery. As indicated from the literature, 3D printing has already been applied to a variety of relevant fields, with preoperative planning as the one most commonly reported. The second most encountered application is for educational and training purposes. The remaining studies evaluate the technical aspects of 3D printed models, or refer to some less frequent uses. 3D printed models of patients’ livers have been found to be useful in preoperative planning, as they provide a more realistic view of the lesion and the surrounding anatomical structures, a conclusion shared by other reviews as well[13,15,18]. These models can also offer the ability to interact with a graspable object, so that surgical manipulations can be tested, in contrast with 3D visualizations based on a computer setting. Although virtual and augmented reality techniques can also provide tactile feedback, they lack fidelity with the current equipment available[50]. The most common type of surgery was partial hepatectomy for the resection of malignant tumors, while three studies applied 3D printing methods in LDLT[20,23,26]. The application in transplantation seems to be extremely helpful, as it can provide models for both donor and recipient livers, thus enabling the surgeon to better understand the crucial landmarks and structures, as well as better prepare for the procedure and avoid the large-for-size syndrome[26]. Education offers a great field for 3D printing applications, as the innovative technology can address the need for high quality visualization of the interior, tactile feedback and reproducible models. 3D printed copies are used both in anatomy teaching and for providing tools for training in advanced interventions, such as choledochoscopy. Some studies have evaluated the accuracy and reproducibility of 3D printed models in a positive manner. Remarkably interesting are some rarely encountered uses of 3D printing in liver surgery, such as its use in filling the hollow cavities of brain-dead patients after the removal of their organs, or its involvement in a novel technique for better sectioning of explants for pathology purposes[47,48]. These are examples of the numerous yet unknown uses of such techniques and technologies, and can lead the way for further exploration.
Although 3D printing exhibits significant advantages, there are certain drawbacks that may undermine its wide use. The large eco nomic cost and the extended time required for printing are often referred as such in the literature[13,31]. Unfortunately, these types of information are inadequately reported in the included studies, and when they do, there are numerous factors that can significantly affect these parameters, which are rarely explained. As far as the cost is concerned, the price for printing one model starts at around $100 and can exceed $1000. However, the printing technique and the printer, the fabrication materials used, and the size of the model can drastically change the cost. Moreover, in some studies, the printing is assigned to third specialized companies, which may include extra costs in the final price (branding, shipping costs) or make marketing discounts. In some studies, the lesions, biliary tract and vascular structures are printed, but not the parenchyma, not only for educational/clinical reasons (touching the structures), but also to reduce the cost. In terms of time, it seems that not only the printing procedure itself is a time-consuming process, but so are the preliminary stages of image segmentation and data conversion to a printer-compatible format. The size of the model, the desired quality and the software used determine the needed time.
Our findings are in agreement with the conclusions of other relevant reviews. According to our search, there have been four reviews analyzing the use of 3D printing in liver pathology[13,17,18,51,52]. Three of the reviews include less than or equal to 19 studies[17,18,51,52], while Witowski et al[12] also includes articles referring to 3D tissue bioprinting. One review was published in 2016, two in 2017 and two in 2018. In the current review, 32 original papers were included, which makes it the most comprehensive review in this rapidly developing field. One of the limitations of this review is that the majority of the studies included were case reports or case series, while there were only few observational cohort studies and RCTs. The observational cohort design was mainly used in studies that evaluated the technical properties of the models. In most cases, a group of experts evaluated specific variables of the models, such as their accuracy, their potential usefulness (according to the evaluators’ subjective judgement) or their reproducibility. In these studies, the scores of the various models were not compared to other standardized, gold-standard tech-niques[34-36,42,44]. On the contrary, the included RCTs evaluated the effect of 3D printed models against other conventional methods, such as 3D visualizations on computers or CT imaging, mostly in the field of educational applications[35,36,39,40]. However, even these papers, which constitute the most robustly designed studies, contain small sample sizes that fail to add statistical power to the tests used. All of the studies referring to preoperative planning are case reports or case series, reporting the subjective evaluation of the experts using these models in single cases. This can at least partly be explained by the fact that an RCT would require many different, individualized 3D printed models of the livers of the intervention cohort, which would be discouragingly costly. Moreover, even if an RCT with sufficiently large samples could show the clinical benefit of 3D printing, we would also have to assess the cost of the intervention in order to conclude, not only if it is an effective method, but also if it constitutes a cost-efficient and massively applicable one. More RCTs are needed that will show the possible superiority of 3D printing methods against more conventional ones, and will extensively report the time and cost aspects. This thorough evaluation of 3D printing technology, and its medical and surgical applications, is critical, as the key question remains whether this impressive, innovative technology will actually benefit our patients and their families. As we are at the dawn of this new technology, we expect to continue seeing new evidence and expanding our knowledge.
CONCLUSION
3D printing is a novel technique that has applications in several liver surgical conditions. Most published studies refer to its use in preoperative planning and education. Although the advantages it offers seem numerous, the cost and time required for the whole process is currently an important issue. As this technology has emerged recently, we can speculate that these drawbacks will be resolved in the future so that these methods will be widely accessible and better explored.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and Hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Conflict-of-interest statement: All authors have nothing to disclosure.
Peer-review started: February 11, 2019
First decision: April 11, 2019
Article in press: June 27, 2019
P-Reviewer: Milovanovic T, Pallav K, Guo X S-Editor: Cui LJ L-Editor: Filipodia E-Editor: Zhang YL
Contributor Information
Peter Bangeas, Department of Surgery, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece.
Vassilios Tsioukas, Department of School of Rural and Surveying Engineering, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece.
Vasileios N Papadopoulos, Department of Surgery, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece.
Georgios Tsoulfas, Department of Surgery, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece. tsoulfasg@auth.gr.
References
- 1.Takagishi K, Umezu S. Development of the Improving Process for the 3D Printed Structure. Sci Rep. 2017;7:39852. doi: 10.1038/srep39852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chua CK, Yeong WY, An J. Special Issue: 3D Printing for Biomedical Engineering. Materials (Basel) 2017:10. doi: 10.3390/ma10030243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bangeas P, Voulalas G, Ktenidis K. Rapid prototyping in aortic surgery. Interact Cardiovasc Thorac Surg. 2016;22:513–514. doi: 10.1093/icvts/ivv395. [DOI] [PubMed] [Google Scholar]
- 4.Shaheen E, Alhelwani A, Van De Casteele E, Politis C, Jacobs R. Evaluation of Dimensional Changes of 3D Printed Models After Sterilization: A Pilot Study. Open Dent J. 2018;12:72–79. doi: 10.2174/1874210601812010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sodian R, Schmauss D, Markert M, Weber S, Nikolaou K, Haeberle S, Vogt F, Vicol C, Lueth T, Reichart B, Schmitz C. Three-dimensional printing creates models for surgical planning of aortic valve replacement after previous coronary bypass grafting. Ann Thorac Surg. 2008;85:2105–2108. doi: 10.1016/j.athoracsur.2007.12.033. [DOI] [PubMed] [Google Scholar]
- 6.Lioufas PA, Quayle MR, Leong JC, McMenamin PG. 3D Printed Models of Cleft Palate Pathology for Surgical Education. Plast Reconstr Surg Glob Open. 2016;4:e1029. doi: 10.1097/GOX.0000000000001029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmauss D, Haeberle S, Hagl C, Sodian R. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-centre experience. Eur J Cardiothorac Surg. 2015;47:1044–1052. doi: 10.1093/ejcts/ezu310. [DOI] [PubMed] [Google Scholar]
- 8.Kurenov SN, Ionita C, Sammons D, Demmy TL. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J Thorac Cardiovasc Surg. 2015;149:973–9.e1. doi: 10.1016/j.jtcvs.2014.12.059. [DOI] [PubMed] [Google Scholar]
- 9.Rankin TM, Giovinco NA, Cucher DJ, Watts G, Hurwitz B, Armstrong DG. Three-dimensional printing surgical instruments: are we there yet? J Surg Res. 2014;189:193–197. doi: 10.1016/j.jss.2014.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolyva C, Biglino G, Pepper JR, Khir AW. A mock circulatory system with physiological distribution of terminal resistance and compliance: application for testing the intra-aortic balloon pump. Artif Organs. 2012;36:E62–E70. doi: 10.1111/j.1525-1594.2010.01071.x. [DOI] [PubMed] [Google Scholar]
- 11.Biglino G, Capelli C, Binazzi A, Reggiani R, Cosentino D, Migliavacca F, Bonhoeffer P, Taylor AM, Schievano S. Virtual and real bench testing of a new percutaneous valve device: a case study. EuroIntervention. 2012;8:120–128. doi: 10.4244/EIJV8I1A19. [DOI] [PubMed] [Google Scholar]
- 12.Witowski JS, Coles-Black J, Zuzak TZ, Pędziwiatr M, Chuen J, Major P, Budzyński A. 3D Printing in Liver Surgery: A Systematic Review. Telemed J E Health. 2017;23:943–947. doi: 10.1089/tmj.2017.0049. [DOI] [PubMed] [Google Scholar]
- 13.Michael S, Sorg H, Peck CT, Koch L, Deiwick A, Chichkov B, Vogt PM, Reimers K. Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures in the dorsal skin fold chamber in mice. PLoS One. 2013;8:e57741. doi: 10.1371/journal.pone.0057741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oshiro Y, Ohkohchi N. Three-Dimensional Liver Surgery Simulation: Computer-Assisted Surgical Planning with Three-Dimensional Simulation Software and Three-Dimensional Printing. Tissue Eng Part A. 2017;23:474–480. doi: 10.1089/ten.TEA.2016.0528. [DOI] [PubMed] [Google Scholar]
- 15.Kuroda S, Kobayashi T, Ohdan H. 3D printing model of the intrahepatic vessels for navigation during anatomical resection of hepatocellular carcinoma. Int J Surg Case Rep. 2017;41:219–222. doi: 10.1016/j.ijscr.2017.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang JZ, Xiong NY, Zhao LZ, Hu JT, Kong DC, Yuan JY. Review fantastic medical implications of 3D-printing in liver surgeries, liver regeneration, liver transplantation and drug hepatotoxicity testing: A review. Int J Surg. 2018;56:1–6. doi: 10.1016/j.ijsu.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Perica ER, Sun Z. A Systematic Review of Three-Dimensional Printing in Liver Disease. J Digit Imaging. 2018;31:692–701. doi: 10.1007/s10278-018-0067-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zein NN, Hanouneh IA, Bishop PD, Samaan M, Eghtesad B, Quintini C, Miller C, Yerian L, Klatte R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013;19:1304–1310. doi: 10.1002/lt.23729. [DOI] [PubMed] [Google Scholar]
- 20.Takagi K, Nanashima A, Abo T, Arai J, Matsuo N, Fukuda T, Nagayasu T. Three-dimensional printing model of liver for operative simulation in perihilar cholangiocarcinoma. Hepatogastroenterology. 2014;61:2315–2316. [PubMed] [Google Scholar]
- 21.Igami T, Nakamura Y, Hirose T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, Mori K, Nagino M. Application of a three-dimensional print of a liver in hepatectomy for small tumors invisible by intraoperative ultrasonography: preliminary experience. World J Surg. 2014;38:3163–3166. doi: 10.1007/s00268-014-2740-7. [DOI] [PubMed] [Google Scholar]
- 22.Baimakhanov Z, Soyama A, Takatsuki M, Hidaka M, Hirayama T, Kinoshita A, Natsuda K, Kuroki T, Eguchi S. Preoperative simulation with a 3-dimensional printed solid model for one-step reconstruction of multiple hepatic veins during living donor liver transplantation. Liver Transpl. 2015;21:266–268. doi: 10.1002/lt.24019. [DOI] [PubMed] [Google Scholar]
- 23.Xiang N, Fang C, Fan Y, Yang J, Zeng N, Liu J, Zhu W. Application of liver three-dimensional printing in hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: preliminary experience. Int J Clin Exp Med. 2015;8:18873–18878. [PMC free article] [PubMed] [Google Scholar]
- 24.Souzaki R, Kinoshita Y, Ieiri S, Hayashida M, Koga Y, Shirabe K, Hara T, Maehara Y, Hashizume M, Taguchi T. Three-dimensional liver model based on preoperative CT images as a tool to assist in surgical planning for hepatoblastoma in a child. Pediatr Surg Int. 2015;31:593–596. doi: 10.1007/s00383-015-3709-9. [DOI] [PubMed] [Google Scholar]
- 25.Soejima Y, Taguchi T, Sugimoto M, Hayashida M, Yoshizumi T, Ikegami T, Uchiyama H, Shirabe K, Maehara Y. Three-dimensional printing and biotexture modeling for preoperative simulation in living donor liver transplantation for small infants. Liver Transpl. 2016;22:1610–1614. doi: 10.1002/lt.24516. [DOI] [PubMed] [Google Scholar]
- 26.Leng S, Chen B, Vrieze T, Kuhlmann J, Yu L, Alexander A, Matsumoto J, Morris J, McCollough CH. Construction of realistic phantoms from patient images and a commercial three-dimensional printer. J Med Imaging (Bellingham) 2016;3:033501. doi: 10.1117/1.JMI.3.3.033501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witowski JS, Pędziwiatr M, Major P, Budzyński A. Cost-effective, personalized, 3D-printed liver model for preoperative planning before laparoscopic liver hemihepatectomy for colorectal cancer metastases. Int J Comput Assist Radiol Surg. 2017;12:2047–2054. doi: 10.1007/s11548-017-1527-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Madurska MJ, Poyade M, Eason D, Rea P, Watson AJ. Development of a Patient-Specific 3D-Printed Liver Model for Preoperative Planning. Surg Innov. 2017;24:145–150. doi: 10.1177/1553350616689414. [DOI] [PubMed] [Google Scholar]
- 29.Oshiro Y, Mitani J, Okada T, Ohkohchi N. A novel three-dimensional print of liver vessels and tumors in hepatectomy. Surg Today. 2017;47:521–524. doi: 10.1007/s00595-016-1383-8. [DOI] [PubMed] [Google Scholar]
- 30.Perica E, Sun Z. Patient-specific three-dimensional printing for pre-surgical planning in hepatocellular carcinoma treatment. Quant Imaging Med Surg. 2017;7:668–677. doi: 10.21037/qims.2017.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andolfi C, Plana A, Kania P, Banerjee PP, Small S. Usefulness of Three-Dimensional Modeling in Surgical Planning, Resident Training, and Patient Education. J Laparoendosc Adv Surg Tech A. 2017;27:512–515. doi: 10.1089/lap.2016.0421. [DOI] [PubMed] [Google Scholar]
- 32.Igami T, Nakamura Y, Oda M, Tanaka H, Nojiri M, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, Yamaguchi J, Mori K, Nagino M. Application of three-dimensional print in minor hepatectomy following liver partition between anterior and posterior sectors. ANZ J Surg. 2018;88:882–885. doi: 10.1111/ans.14331. [DOI] [PubMed] [Google Scholar]
- 33.Dhir V, Itoi T, Fockens P, Perez-Miranda M, Khashab MA, Seo DW, Yang AM, Lawrence KY, Maydeo A. Novel ex vivo model for hands-on teaching of and training in EUS-guided biliary drainage: creation of "Mumbai EUS" stereolithography/3D printing bile duct prototype (with videos) Gastrointest Endosc. 2015;81:440–446. doi: 10.1016/j.gie.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, Li J, Huang W. Do Three-dimensional Visualization and Three-dimensional Printing Improve Hepatic Segment Anatomy Teaching? A Randomized Controlled Study. J Surg Educ. 2016;73:264–269. doi: 10.1016/j.jsurg.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, Huang W, Li J. Do 3D Printing Models Improve Anatomical Teaching About Hepatic Segments to Medical Students? A Randomized Controlled Study. World J Surg. 2016;40:1969–1976. doi: 10.1007/s00268-016-3541-y. [DOI] [PubMed] [Google Scholar]
- 36.Watson RA. A low-cost surgical application of additive fabrication. J Surg Educ. 2014;71:14–17. doi: 10.1016/j.jsurg.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 37.Javan R, Herrin D, Tangestanipoor A. Understanding Spatially Complex Segmental and Branch Anatomy Using 3D Printing: Liver, Lung, Prostate, Coronary Arteries, and Circle of Willis. Acad Radiol. 2016;23:1183–1189. doi: 10.1016/j.acra.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 38.Li A, Tang R, Rong Z, Zeng J, Xiang C, Yu L, Zhao W, Dong J. The Use of Three-Dimensional Printing Model in the Training of Choledochoscopy Techniques. World J Surg. 2018;42:4033–4038. doi: 10.1007/s00268-018-4731-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang T, Lin S, Xie Q, Ouyang W, Tan T, Li J, Chen Z, Yang J, Wu H, Pan J, Hu C, Zou Y. Impact of 3D printing technology on the comprehension of surgical liver anatomy. Surg Endosc. 2019;33:411–417. doi: 10.1007/s00464-018-6308-8. [DOI] [PubMed] [Google Scholar]
- 40.Javan R, Zeman MN. A Prototype Educational Model for Hepatobiliary Interventions: Unveiling the Role of Graphic Designers in Medical 3D Printing. J Digit Imaging. 2018;31:133–143. doi: 10.1007/s10278-017-0012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burdall OC, Makin E, Davenport M, Ade-Ajayi N. 3D printing to simulate laparoscopic choledochal surgery. J Pediatr Surg. 2016;51:828–831. doi: 10.1016/j.jpedsurg.2016.02.093. [DOI] [PubMed] [Google Scholar]
- 42.Takao H, Amemiya S, Shibata E, Ohtomo K. Three-Dimensional Printing of Hollow Portal Vein Stenosis Models: A Feasibility Study. J Vasc Interv Radiol. 2016;27:1755–1758. doi: 10.1016/j.jvir.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 43.Choi YR, Kim JH, Park SJ, Hur BY, Han JK. Therapeutic response assessment using 3D ultrasound for hepatic metastasis from colorectal cancer: Application of a personalized, 3D-printed tumor model using CT images. PLoS One. 2017;12:e0182596. doi: 10.1371/journal.pone.0182596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bücking TM, Hill ER, Robertson JL, Maneas E, Plumb AA, Nikitichev DI. From medical imaging data to 3D printed anatomical models. PLoS One. 2017;12:e0178540. doi: 10.1371/journal.pone.0178540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koganemaru M, Horiuchi H, Abe T. Treatment of Hypohepatia After Transplantation of Liver From a Living Donor Liver by Transcatheter Embolization, Using a Simulated 3-Dimensional Printing Vascular Model. Gastroenterology. 2016;151:e11–e13. doi: 10.1053/j.gastro.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 46.Trout AT, Batie MR, Gupta A, Sheridan RM, Tiao GM, Towbin AJ. 3D printed pathological sectioning boxes to facilitate radiological-pathological correlation in hepatectomy cases. J Clin Pathol. 2017;70:984–987. doi: 10.1136/jclinpath-2016-204293. [DOI] [PubMed] [Google Scholar]
- 47.Weng JY, Wang CC, Chen PJ, Lim SW, Kuo JR. The Application of a Three-Dimensional Printed Product to Fill the Space After Organ Removal. World Neurosurg. 2017;107:1045.e17–1045.e19. doi: 10.1016/j.wneu.2017.07.149. [DOI] [PubMed] [Google Scholar]
- 48.Yang T, Tan T, Yang J, Pan J, Hu C, Li J, Zou Y. The impact of using three-dimensional printed liver models for patient education. J Int Med Res. 2018;46:1570–1578. doi: 10.1177/0300060518755267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tang R, Ma L, Li A, Yu L, Rong Z, Zhang X, Xiang C, Liao H, Dong J. Choledochoscopic Examination of a 3-Dimensional Printing Model Using Augmented Reality Techniques: A Preliminary Proof of Concept Study. Surg Innov. 2018;25:492–498. doi: 10.1177/1553350618781622. [DOI] [PubMed] [Google Scholar]
- 50.Pantelidis P, Chorti A, Papagiouvanni I, Paparoidamis G, Drosos C, Panagiotakopoulos T, Lales G, Sideris M. Virtual and Augmented Reality in Medical Education. In: Tsoulfas G, editor. Medical and Surgical Education-Past, Present and Future. Rijeka: InTech; 2018. pp. 77–99. [Google Scholar]
- 51.Ikegami T, Maehara Y. Transplantation: 3D printing of the liver in living donor liver transplantation. Nat Rev Gastroenterol Hepatol. 2013;10:697–698. doi: 10.1038/nrgastro.2013.195. [DOI] [PubMed] [Google Scholar]
- 52.Soon DS, Chae MP, Pilgrim CH, Rozen WM, Spychal RT, Hunter-Smith DJ. 3D haptic modelling for preoperative planning of hepatic resection: A systematic review. Ann Med Surg (Lond) 2016;10:1–7. doi: 10.1016/j.amsu.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]