Abstract
An 83‐year‐old woman was admitted with empyema. Pneumococcal rapid urinary antigen testing on admission showed a positive result, but culture of pleural effusion yielded only Streptococcus intermedius. S. intermedius is a member of the anginosus group and a component of the regular flora of the oral cavity and gastrointestinal tract. As a human pathogen, this species has gained notoriety for abscess formation in the liver and brain but has also been reported recently as a major agent causing pulmonary abscesses or empyema, and the number of affected patients is increasing with the aging of society. We present the first case of a false‐positive pneumococcal rapid urinary antigen test in empyema caused by S. intermedius.
Keywords: Empyema, pneumococcal rapid urinary antigen test, Streptococcus intermedius
Introduction
Streptococcus intermedius is a member of the anginosus group along with Streptococcus anginosus and Streptococcus constellatus. This species is a component of the regular flora of the oral cavity and gastrointestinal tract. As a human pathogen, it has been notorious for forming abscesses in the liver and brain. However, S. intermedius has also recently been reported as a causative pathogen in 13–44% of cases of pulmonary abscesses/empyema 1, and the prevalence of this disease is increasing with the aging of society. The pneumococcal rapid urinary antigen test is widely used to diagnose pneumococcal infection with high specificity. However, organisms such as Streptococcus mitis and Streptococcus oralis have been reported to cause false‐positive results. We present the first case of a false‐positive pneumococcal rapid urinary antigen test in empyema caused by S. intermedius.
Case Report
An 83‐year‐old woman was admitted with a seven‐day history of fatigue and right‐sided chest pain and a three‐day history of dyspnoea and appetite loss. Her past medical history included osteoporosis, left femoral fracture, and chronic tobacco use (62 pack‐years). She had not previously received any pneumococcal vaccines. She had been living indoors and alone. Vital signs on admission were: blood pressure 120/80 mmHg; heart rate 98 beats/min; respiratory rate 24 breaths/min; oxygen saturation 92% on oxygen at 3 L/min through nasal cannula; and body temperature 37.1°C. Her oral hygiene was poor. Breath sounds were decreased over the right hemithorax. Chest X‐ray showed massive right pleural effusion (Fig. 1A). Blood test results showed severe inflammation (white blood cells 28,600/μL; C‐reactive protein 24.5 mg/dL; procalcitonin 4.6 ng/mL), dehydration (blood urea nitrogen 80 mg/dL; creatinine 1.1 mg/dL), and malnutrition (albumin 1.9 mg/dL). Serum glucose and HbA1c levels were 144 mg/dL and 6.2%, respectively. The pneumococcal rapid urinary antigen test (BinaxNOW; Abbott, Japan) showed a positive result. computed tomography (CT) showed a large loculated pleural effusion in the right lung (Fig. 1B,c). Passive atelectasis was identified, but no pulmonary parenchymal disease suggestive of pneumonia was evident. Diagnostic bedside thoracentesis was performed. Since pus was obtained, a chest tube was inserted for drainage. Laboratory analysis of the pleural fluid documented: glucose <1 mg/dL; total protein 4.3 g/dL; and lactate dehydrogenase 3395 IU/L. The leukocyte count in pleural effusion was 4825/μL, with 99% neutrophils. Ceftriaxone (CTRX) at 2 g q24 h and clindamycin (CLDM) at 800 mg q8 h were started intravenously. Intrapleural installation of fibrinolytic agents and pleural lavage with saline were continued daily up to hospital days 3 and 10, respectively. The patient subsequently improved and was afebrile by day 3. Sputum culture yielded Enterobacter aerogenes, Klebsiella pneumoniae, α‐Streptococcus, and Candida albicans on day 4. S. intermedius was identified from a culture of pleural fluid on day 7. Blood cultures were negative. The S. intermedius was found to be sensitive to penicillin in susceptibility testing on day 10. Then CTRX and CLDM were switched to ampicillin/sulbactam at 3 g q6 h. Treatment was continued up to day 35 and repeated chest CT demonstrated complete resolution of the empyema after completing treatment. She was transferred to a rehabilitation centre on day 37.
Figure 1.
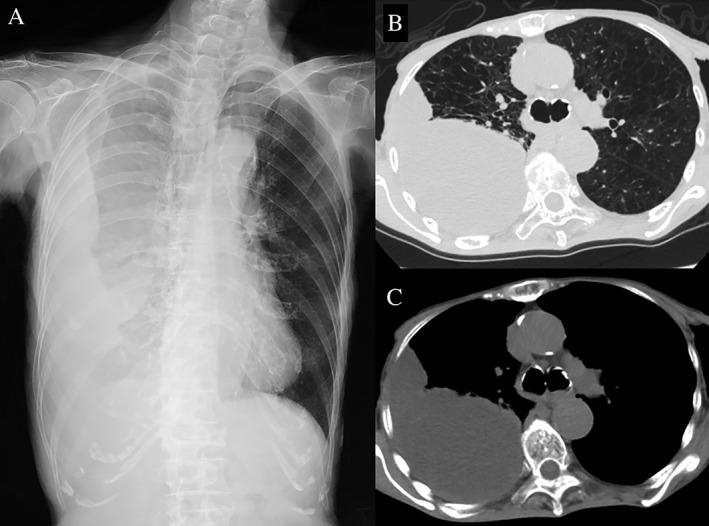
Chest X‐ray (A) and computed tomography (B, C) on admission showed a large loculated pleural effusion in the right lung.
Discussion
This is the first report of a false‐positive result for a pneumococcal rapid urinary antigen test in empyema caused by S. intermedius. The test detects the pneumococcal antigen with 74% sensitivity and 94% specificity among adults according to a recent systematic review 2. Since S. mitis and S. oralis have the same cell wall C‐polysaccharide antigen as pneumococcus, false‐positive results with BinaxNOW by their infection have been reported 3, 4. False‐positive results with S. intermedius from BinaxNOW have not been reported before; however, the package insert of RAPIRUN Pneumococcus (Otsuka Pharmaceutical, Tokyo, Japan) which detects pneumococcal cell wall C‐polysaccharide antigen refers to not 3.5 × 107 colony‐forming units (CFU)/mL, but rather 7.0 × 107 CFU/mL of S. intermedius showing false‐positive results due to cross‐reaction. In our case, we considered that false‐positive results due to pneumococcus, S. mitis, or S. oralis were ruled out, since she had never received the pneumococcal vaccine before, had not experienced pneumonia recently, had not been in contact with children, the number of α‐Streptococcus colonies cultured from sputum was small, and only S. intermedius was isolated from pleural effusion. There were 12 cases of empyema caused by S. intermedius in our hospital from April 2010 to April 2019. BinaxNOW was used in five cases among these, with only this present case showing a false‐positive result. We made an extract from 109 CFU/mL culture aliquots of S. intermedius isolated from another patient and applied the BinaxNOW, but the result was negative. The probable reason for our false‐positive result in BinaxNOW was that S. intermedius infected our patient had cell wall C‐polysaccharide antigen which cross‐reacted with pneumococcal antibodies in the BinaxNOW, and the amount of the antigen in her urine on admission was enough to cause a positive result because the number of S. intermedius in her empyema was very high. A repeat BinaxNOW performed on day 18 showed a negative result.
S. intermedius is reportedly a causative pathogen in only 2–5% of cases of bacterial pneumonia, but in 13–44% of pulmonary abscesses/empyema 1, especially, is the most common causative organism in primary empyema (empyema not accompanied by pneumonia) along with Fusobacterium nucleatum 5. Since S. intermedius tends to form abscesses, a longer duration of antibiotic administration than regular could be considered. Interventions for improving oral health are also desirable. For physicians, the possibility of false‐positive results for pneumococcal rapid urinary antigen test needs to be considered in empyema patients with S. intermedius infection.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Acknowledgments
We thank for the cooperation of the bacteria laboratory of Tokyo Saiseikai Central Hospital.
Takahashi, S , Ishitsuka, T , Namatame, K , Nakamura, M . (2019) A false‐positive pneumococcal rapid urinary antigen test in Streptococcus intermedius infection. Respirology Case Reports, 7(7), ;e00466. 10.1002/rcr2.466
Associate Editor: Bei He
References
- 1. Noguchi S, Yatera K, Kawanami T, et al. 2014. Pneumonia and empyema caused by Streptococcus intermedius that shows the diagnostic importance of evaluating the microbiota in the lower respiratory tract. Intern. Med. 53:47–50. [DOI] [PubMed] [Google Scholar]
- 2. Boulware DR, Daley CL, Merrifield C, et al. 2007. Rapid diagnosis of pneumococcal pneumonia among HIV‐infected adults with urine antigen detection. J. Infect. 55:300–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.BinaxNOW Pneumococcal. 2018 Abbott. http://www.info.pmda.go.jp/tgo/pack/21600AMY00094000_A_01_06/.
- 4. Nakanishi M, Fujimoto Y, Inaba T, et al. 2014. A case of Streptococcus oralis, Granulicarella adiacens, aspirarion pneumonia and bacteremia with positive pneumococcal urinary antigen. Ann. Japan. Resp. Soc. 3:133–136. [Google Scholar]
- 5. Iskandar SB, Al Hasan MA, Roy TM, et al. 2006. Streptococcus intermedius: an unusual cause of a primary empyema. Tenn. Med. 9:37–39. [PubMed] [Google Scholar]


