Abstract
The Usutu virus (USUV) is a flavivirus that is drawing increasing attention because of its potential for emergence. First isolated in Africa, it was introduced into Europe where it caused significant outbreaks in birds, such as in Austria in 2001. Since then, its geographical distribution has rapidly expanded, with increased circulation, especially in the last few years. Similar to West Nile virus (WNV), the USUV enzootic transmission cycle involves Culex mosquitoes as vectors, and birds as amplifying reservoir hosts, with humans and other mammals likely being dead-end hosts. A similarity in the ecology of these two viruses, which co-circulate in several European countries, highlights USUV’s potential to become an important human pathogen. While USUV has had a severe impact on the blackbird population, the number of human cases remains low, with most infections being asymptomatic. However, some rare cases of neurological disease have been described, both in healthy and immuno-compromised patients. Here, we will discuss the transmission dynamics and the current state of USUV circulation in Europe.
Keywords: USUV, Usutu, WNV, flavivirus, emergence
1. Introduction
The dramatic outbreaks and global spread of the chikungunya virus (CHIKV) and the Zika virus (ZIKV) illustrate the danger that emerging arboviruses represent. Given the plethora of mosquito-transmitted viruses, which have been identified to date, and the known ability of RNA viruses to mutate rapidly to adapt to new environments, it is likely that other arboviruses will emerge in the next decades. The Usutu virus (USUV), an arbovirus from the Flaviviridae family, genus Flavivirus, has recently garnered a great deal of attention from the scientific community, particularly since its emergence in Europe. Similar to other flaviviruses, its (+)-strand RNA genome of 11,064 nucleotides encodes a single polyprotein of 3,434 amino acids that is subsequently cleaved into structural (C, prM and E) and non-structural (NS1, NS2A, NS2B, NS3, NS4A, NS4B and NS5) proteins. The natural life cycle of USUV involves Culex mosquitoes as its main vector, and multiple bird species as a natural viral reservoir. To date, USUV has been mostly associated with disease in birds, with spectacular episodes of mass mortality occurring in Central Europe; but it can also infect humans, and in some rare cases, it can be associated with neurological complications.
In this review, we will summarize the current knowledge on USUV, with particular emphasis on the increased circulation in Europe in recent years, the dynamics of transmission, and the human clinical cases described to date.
2. Introduction of USUV in Europe and Genetic Diversity
USUV belongs to the Japanese encephalitis virus (JEV) antigenic complex, together with West Nile virus (WNV) and Murray Valley encephalitis virus (MVEV). It was isolated for the first time in 1959 from a Culex neavei mosquito caught near the Usutu river in Swaziland [1]. Since then, the virus has continuously circulated within Africa, having been detected in Senegal, Uganda, Central African Republic, Nigeria, Burkina Faso, and Côte d’Ivoire (reviewed in [2]). USUV was observed in Europe for the first time in Vienna in 2001 [3], where it was responsible for massive outbreaks in blackbirds (Turdus merula) and gray owls (Strix nebulosa). A retrospective study analyzing dead birds conducted in the Tuscany region of Italy showed that USUV has been circulating in Europe since 1996 [4].
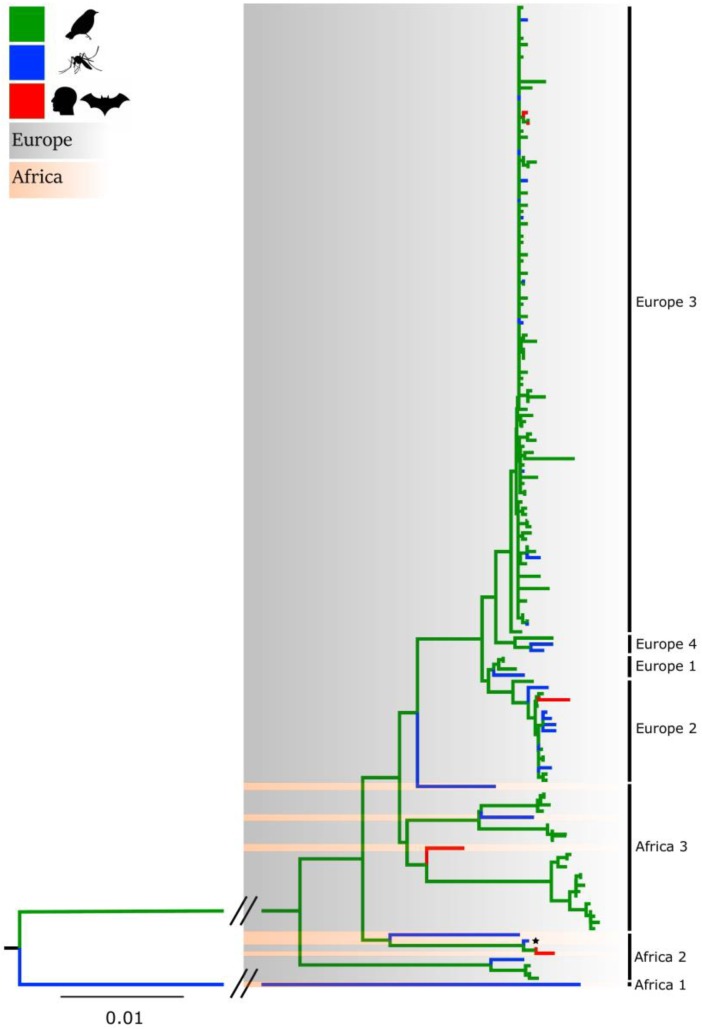
The genetic variability of USUV has been explored through phylogenetic studies performed over full-length sequences, as well as the envelope and NS5 genes [5,6,7,8,9]. These analyses cluster USUV sequences into distinct lineages which are designated on the basis of their geographic origin of isolation: Africa 1, 2 and 3 and Europe 1, 2, 3 and 4 (Figure 1). A recent phylogenetic study focused on partial NS5 gene sequences (265 bp) revealed a novel lineage (Europe 5) composed of strains isolated from birds in Germany in 2016 [8]. The prototype African strain SAAR-1776 (represented with a star in Figure 1) is distantly related to the European lineages. In addition to these genetic differences, SAAR-1776 differs from other USUV strains in that it was generated by intracerebral inoculation of newborn mice [1].
Figure 1.
Maximum-likelihood phylogenetic tree analysis of the NS5 gene of USUV strains (n = 158) circulating worldwide. Strains isolated from birds, mosquitoes and mammals are indicated in green, blue and red, respectively. African and European variants are shaded in pink and gray, respectively. The prototype SAAR-1776 strain is indicated by a star. The bar at the bottom of the tree denotes evolutionary distance, as number of base substitutions per site. The interrupted branches (indicated by oblique lines) were shortened by 50% for better graphic representation. The list of USUV strains used to generate the tree are provided in Supplemental Materials: Table S1.
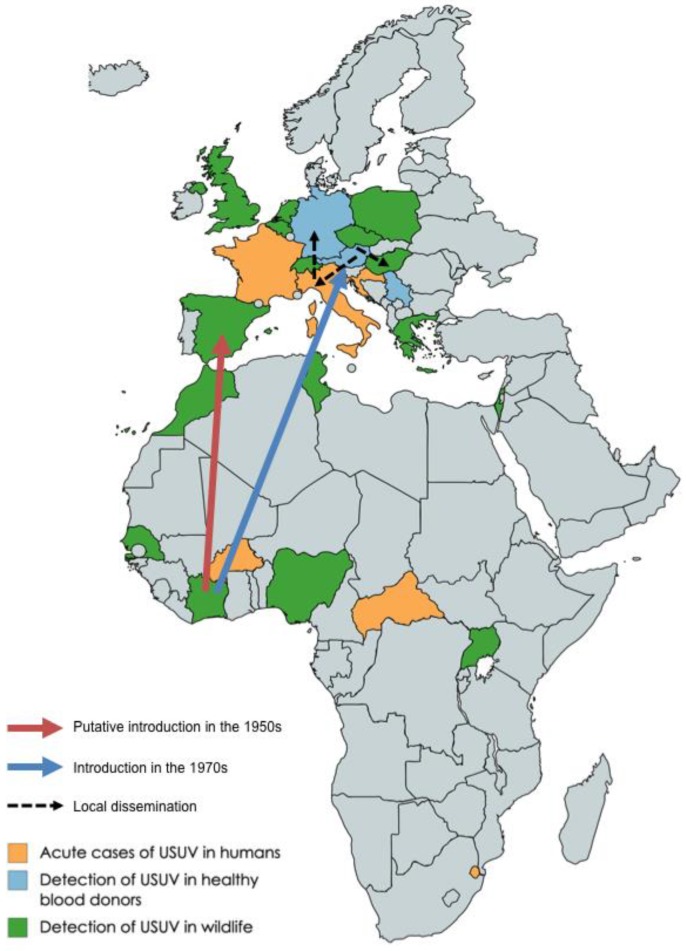
USUV is thought to have been introduced in Europe multiple times through bird migration, starting in the 1950s [7]. The Europe 1 lineage is thought to derive from a virus in Senegal that reached Spain, and is likely the origin of the first epizoosis in Central Europe. According to the same study, the Europe 2 and 3 lineages probably originated in Austria in 1993, and in Italy in 2007, respectively (Figure 2). Since these introductions, the virus has spread rapidly around the Mediterranean basin and Central Europe, reaching Tunisia [10], Morocco [11], Israel [12], Greece [13], France [14], Spain [15], Poland [16], Hungary [17], Czech Republic [18], Serbia [5], the United Kingdom [19], Croatia [20], the Netherlands [21], Switzerland [22], Italy [23], where it gave rise to the Europe 4 lineage, and Germany [24], where 3 different lineages have been recently shown to co-circulate [25]. Recent evidence suggests that introduction events into Europe from Africa are still happening. Indeed, viruses from African lineages were recently detected in Germany [26] and in the Camargue area of France [14].
Figure 2.
Geographical distribution of USUV. Countries where USUV was detected in wildlife (birds, mosquitoes, horses, etc.) are indicated in green; countries where USUV was detected in healthy blood donors are represented in blue; and countries where USUV caused symptomatic, acute infections are shown in orange. The arrows represent the presumed bird migration event that led to introduction of USUV in Europe, according to Engel et al. [7].
The viral or immunological determinants responsible for USUV adaptation to birds and humans remain unclear. Similar to other arboviruses alternating between the insect vector and mammalian host species, evidence of strong purifying selection was detected across the entire viral genome [7]. In the case of USUV, European lineages seem to be subjected to a stronger negative selection than African lineages [7]. Nevertheless, one position in the viral polymerase gene NS5 (amino acid 898) evolved under significant positive selection, possibly reflecting an ongoing host/pathogen evolutionary conflict. Interestingly, another substitution in the NS5 gene has been observed in the Bologna/09 viral strain [27] derived from an USUV-positive patient recovering from orthotropic liver transplant [28]. As more viral sequences are made available, the viral determinants influencing USUV pathogenesis may be identified, as well as whether or not other factors such as evasion from the IFN response participate in this process.
3. Transmission Dynamics
3.1. WNV and USUV Co-Circulation and Co-Infection Dynamics
The transmission dynamics of arboviruses are generally influenced by biological and environmental factors, such as the identity and population density of vector and reservoir species, the extrinsic incubation period, humidity, temperature, host immunity, etc. In this regard, USUV shares a few common features with WNV: both viruses are mainly transmitted by Culex mosquitoes, with migratory birds acting as the major amplifying host (Table 1). Therefore, it is not surprising that in Europe, where WNV has also recently re-emerged, the two viruses co-circulate in 10 European countries and in 34 species of birds [29], as well as in horses [10]. Furthermore, 9 cases of birds [19,30] and 3 cases of humans [31,32] with positive serology for both viruses have been reported to date. This may be the result of local co-circulation of WNV and USUV, although cross-reactivity of antibodies complicates interpretation of results. Indeed, the envelope protein of USUV shares some structural features with the WNV envelope [33,34], and antibody cross-reactivity has been observed [35]. Thus, serological tests, such as ELISAs, cannot always distinguish USUV from WNV, which has led to the hypothesis that USUV circulation may be underestimated [36]. Other assays, such as protein microarray based on NS1 [37] or quantitative multiplex real-time RT-PCR [38], have been developed in recent years.
In one human case, viral RNA was detected simultaneously for both viruses [31,32], confirming that co-infection does occur. How significant USUV and WNV co-circulation and co-infections are at the population level, and whether a previous flavivirus infection influences subsequent WNV or USUV infections, remain to be determined. An in vivo study suggested that the immunization of mice with recombinant WNV particles induced low levels of antibodies cross-reacting with USUV [39]. Similarly, a previous infection with USUV was shown to reduce the susceptibility of adult mice to WNV [40]. Future work should determine whether such processes of cross-protection, or in the opposite sense, whether antibody enhancement of infection, may occur and be relevant for USUV transmission in birds and humans.
3.2. Vector Species for USUV
While USUV has been detected in a wide range of mosquitoes, it seems to be most frequently associated with Culex pipiens [41,42], which is thought to be the main vector for USUV in Europe. Indeed, competence studies have shown that Culex pipiens supports high levels of USUV infection [43,44,45,46]. Notably, competence of Culex pipiens for USUV and WNV is comparable at 18 °C and 23 °C, but not at 28 °C, where mosquitoes had higher susceptibility for USUV [43]. This may indicate some interesting temperature-related differences in the ability of the two viruses to overcome anatomical barriers and bottlenecks. As noted for other arboviruses, there may be some variation in the ability of USUV to infect different Culex pipiens populations. Indeed, the prototype strain SAAR-1776 could only infect one of the two Culex pipiens colonies from the United Kingdom [44], suggesting that host factors or genetics may restrict infection in these mosquitoes. Whether this is specific to the SAAR-1776 strain, or whether this happens with European USUV strains, remains to be established.
Other species of Culex have been described to be competent for USUV: for instance, both Culex neavei and Culex quinquefasciatus show high infection and dissemination rates [45,47]. USUV has been detected in pools of Aedes albopictus [41,48,49], an invasive mosquito species involved as an alternative vector for the transmission of many arboviruses, such as CHIKV. This prompted further investigation into Aedes albopictus competence for USUV. The results indicated that Aedes albopictus exhibits a lower competence for USUV [45], although the virus can replicate in the body and escape the midgut barrier [50]. In more rare cases, USUV was also detected in other mosquito species such as Aedes japonicus, Aedes vexans, Anopheles maculipennis, Anopheles plumbeus, Coquillettidia richiardii, Culiseta annulata, and some Ochlerotatus species [41,42,46]. USUV has never been detected in ticks, even in areas such as Italy where USUV circulation is known to be significant [51,52]. Since a single mutation was required for CHIKV adaptation to Aedes albopictus [53], sustained surveillance efforts may be required to rapidly detect potential adaptation of USUV to new vector species, which may allow viral dissemination into new geographic regions.
3.3. Reservoir of USUV
The main USUV natural hosts are birds, with infection being reported to date in 93 different species belonging to 35 families [54]. USUV is particularly pathogenic in a few species such as blackbirds (Turdus merula), gray owls (Strix nebulosa), and house sparrows (Passer domesticus) [17,55]. In these birds, systemic USUV replication is likely the cause of the severe pathogenesis, as the virus was detected in many organs such as the liver, heart, brain, and spleen [56]. Necrotic lesions were noted in these organs [57]. It is currently not known whether USUV can infect American robins (Turdus migratorius), a bird species that was critical for WNV dissemination across the US [58]. However, USUV potently infects its European counterpart Turdus merula, and many other Passeriformes birds known to be susceptible to WNV, such as the common starling (Sturnus vulgaris) or the house sparrow [29].
USUV induced mass mortality in blackbirds and grey owls in Austria [57], Germany [56], France [59], and the Netherlands [21], with dramatic consequences on bird populations. For instance, in Germany, the blackbird population declined by 15% within 5 years of USUV’s arrival [8]. In Austria, however, bird mortality sharply dropped after 2004, while the number of infected birds with low viral titers increased [17]. This may have resulted from the acquisition of herd immunity: in owls and birds of prey, the proportion of seropositive birds reached levels above 50% [60]. Interestingly, only a relatively low number of bird species have been subjected to large die-off episodes, and in some avian species such as chickens or geese, experimental inoculation of USUV only caused mild pathogenicity [61,62]. The basis for these species-specific differences in pathogenicity is currently unknown. The co-infection of birds with USUV and other pathogens may increase disease severity: for instance, co-infection of birds with USUV and Plasmodium spp. can lead to a more severe outcome than when they carry only one of these pathogens [21,63]. Future investigation will help determine which virological and immunological factors influence USUV pathogenesis and co-morbidities.
3.4. Other Dead-End Hosts
Beyond infection of birds and humans, USUV has been detected in many mammalian species considered to be dead-end hosts. As is the case with WNV, horses are considered to be a sensitive host for USUV: viral circulation has been detected in Tunisia [10], Spain [64], Serbia [65], Poland [16] and Croatia [20]. USUV can also infect dogs [66,67], dear [68] and wild boars [69]. USUV was also detected in bats [70], squirrels [71] and rodents [72], in which the virus did not seem to cause the same severe pathogenicity as it does in birds, raising concerns that these species could act as secondary reservoirs. Whether USUV can reach a viremia in these animals to sustain a new mosquito infection cycle is unclear. The expanding range of wild animals susceptible to USUV highlights its potential as an important emerging pathogen.
4. Human Clinical Cases and Disease
The first human cases of USUV infection were described in Central African Republic and Burkina Faso in the 1980s and in 2004, respectively, with mild symptoms such as fever and rash [2]. To date, a total of 28 acute USUV infections have been reported in humans [73], including some serious complications such as meningoencephalitis [28,74] and facial paralysis [75]. Seroprevalence studies suggested that USUV infections in humans may have been largely underestimated, and many of them may be asymptomatic. Indeed, antibodies against USUV were detected in the blood of 0.01% to 1% of healthy blood donors in Germany and Italy, respectively [49,76,77]. Higher seroprevalence was detected in serum samples collected from healthy individuals in Serbia (7.5%) [78] and from forestry workers in Italy (18%) [79]. A large retrospective study, conducted on over 900 patients, of which about a third were suspected for encephalitis or meningoencephalitis, found a prevalence of 6.5% [80]. In contrast, two studies failed to detect USUV in the cerebrospinal fluid of patients with encephalitis in Italy and Switzerland [81,82]. These studies indicate that USUV already circulates to significant levels in human populations, although it is rarely associated with neurological complications.
While most USUV infections are mild or asymptomatic, neurotropism represents a growing concern for human health, especially since two immuno-compromised patients tested positive for USUV. One of them was recovering from a liver transplant [28], and the other was diagnosed with a B cell lymphoma [74]: both showed signs of neuropathogenesis that were thought to be caused by USUV. Both survived the infection. USUV RNA was also detected by RT-PCR in cerebrospinal fluid of patients suffering from meningoencephalitis, suggesting that the virus may establish an infection in the brain [83]. Several other lines of evidence suggest that USUV can be neurotropic. First, this virus was detected in the brains of dead bats and birds in the wild [57,70]. Furthermore, experimental infection of 1-week-old suckling mice leads to paraplegia and paralysis, and is associated with apoptosis and demyelination of neuronal and glial cells [84]. Moreover, the USUV virus isolated from a patient diagnosed with facial paralysis could infect primary astrocytes [75]. An in vitro study confirmed these findings and demonstrated that USUV can establish productive infection and induce apoptosis in a wide range of neural cells such as neurons, astrocytes, microglial cells and neuronal stem cells [85]. USUV was even shown to be associated with levels of infection and apoptosis in neuronal cells that were higher than ZIKV, suggesting that USUV may potentially cause significant neurological defects [85].
5. Cellular Responses to USUV Infection
USUV infection triggers the induction of pro-inflammatory and antiviral responses, including cytokine secretion. In primary human nasal epithelial cells, USUV induces a modest expression of IL6, IL8 and IP10, albeit to lower levels than JEV [86]. In dendritic cells (DCs), USUV induces high levels of TNF-α [87], and of both IFN-α and IFN-β [87,88], leading to the expression of Interferon Stimulated Genes (ISGs). Interestingly, cells infected by USUV induce IFN to higher levels than cells infected by WNV (10- to 100-fold, depending on the multiplicity of infection and time point considered) [88]. USUV is also very sensitive to the antiviral effect of IFN: in A549 cells, USUV replication is restricted 10 times more potently than WNV by a wide variety of IFN-I and IFN-III subtypes [88]. Consistent with these findings, while adult Swiss mice are highly susceptible to WNV infection, they are not to USUV [40]. In contrast, USUV infection induced high mortality rates in suckling mice, which have not yet developed a functional IFN response [40,84], or in AG129 mice, knocked-out for the IFN-α and IFN-γ pathways [89]. Taken together, these results suggest that USUV is potently controlled by the IFN response, which may account (at least in part) for its low viral pathogenicity in humans.
Conversely, USUV may also hijack cellular responses to its advantage: for instance, it triggers the autophagy pathway in infected cells, stimulating viral replication [90]. The interplay between autophagy and flaviviruses, which has been described before [91], could be particularly interesting, since it may provide cellular drug targets. Indeed, the autophagy inhibitors 3-methyladenine and wortmanin significantly reduced USUV replication in Vero cells (from 3-fold to 5-fold) [90]. Host lipid biosynthesis pathways are also required for the production of infectious viral particles: inhibition of the acetyl-CoA carboxylase (ACC) enzyme by two different drugs very potently (up to 3 logs) inhibited WNV and USUV [92]. Finally, favipiravir, a broad-spectrum viral RNA polymerase inhibitor, has shown some efficacy in restricting USUV replication in the AG129 model [89].
6. USUV Circulation in the Future: Surveillance and Mathematical Modeling
The circulation of USUV in bird and human populations is already solidly established in Europe, as evidenced by the massive decline in blackbird populations [8] and the significant levels of seroconversion in human blood donors [76,77,78,79,80]. However, the extent of USUV circulation in 2018 is unprecedented [93]. In France, USUV was detected from dead birds in 46 administrative districts, versus only 4 in 2017 (Cécile Beck, personal communication). In Austria, 18 blood donors (16 of them asymptomatic) tested positive for USUV, while only 6 did in 2017 [32]. According to the European Centre for Disease Prevention and Control (EDCC), WNV circulation also reached historically high levels in Europe in 2018, with 2083 human cases, representing a 7-fold increase compared to 2017. Some countries, such as Bulgaria (15-fold increase), France (13.5-fold increase) and Italy (11-fold increase) were particularly impacted by the uptick in WNV circulation. A likely hypothesis for this is that some environmental and ecological factors influencing both USUV and WNV account for the exceptional levels of viral circulation in 2018. However, the possibility that viral adaptation may have contributed to this increased circulation of USUV cannot be ruled out. Therefore, surveillance of USUV circulation, as well as monitoring USUV evolution, will be crucial to try to prevent future outbreaks. This goal remains difficult to achieve, notably because of the lack of large-scale cohort studies and the absence of commercially available diagnostic reagents for USUV. In this context, mathematical modeling can help estimate the potential levels of USUV circulation. Habitat models have recently been used to predict the number of USUV cases in under-sampled areas [94]. Two models have been developed to study USUV transmission dynamics: a mechanistic epidemiological model, aimed at estimating USUV transmission in Austria [95,96]; and a correlation-based environmental model, based on data collected in Germany [8]. Both models were used in a recent study to generate risk maps for USUV [97]. Large areas of Central and Western Europe including northern Italy, Austria, southern France, and a large area spanning the North East of France, Belgium, and the North West of Germany, were predicted as suitable for USUV replication. As temperatures are likely to increase in Europe because of the effects of climate change, these risk maps are even likely underestimating future USUV transmission rates.
Given the similarities in the ecology of WNV and USUV (Table 1), and the relatively recent emergence of USUV in Europe, it is possible that USUV has the potential to reach levels of viral circulation similar to those of WNV. For now, USUV has seemingly not reached the United States, but a study established that North American colonies of Culex pipiens and Culex quinquefasciatus are competent vectors for USUV [45]. As stated earlier, USUV also infects multiple bird species very closely related to the ones that were involved in dissemination of WNV in the United States. Therefore, USUV emergence outside of Europe should be considered a real possibility, prompting research and surveillance efforts.
Table 1.
Comparison of WNV and USUV main characteristics. Some important features of West Nile Virus (WNV) and Usutu Virus (USUV) are listed here, with the corresponding bibliographical references.
| WNV | USUV | |
|---|---|---|
| Geographical Distribution | Africa, Europe, Middle East, North America and West Asia | Africa, Europe |
| Main Vector | Culex spp. | Culex spp. |
| Putative Seconday Vector | A. vexans [98], A. japonicus [99], A. albopictus [100] | A. albopictus [45,50] |
| Amplifying Host | Migratory birds | Migratory birds |
| Main Route of Transmission | Mosquito bite | Mosquito bite |
| Alternate Route of Transmission | Rare cases of contamination through organ transplant and transfusion [101] and of mother-to-child transmission [102] | Not described |
| Sensitivity to IFN | Strong [88] | Very strong [88] |
| Antagonism of IFN Response | Through NS4B [103] | Not described |
On the other hand, it is possible that WNV and USUV are competing with each other, and that the co-existence of both viruses at high levels in the same geographical areas and ecological niches is impossible. Such competition between two related flaviviruses has been observed before, for instance in the case of WNV and Saint Louis encephalitis virus (SLEV). Indeed, prior to WNV emergence in the US, SLEV was endemic in southern California, but circulation drastically dropped after WNV invasion in 2003 [104]. This led to the hypothesis that SLEV, while still capable of sporadically re-emerging [105], has been outcompeted by WNV, which infects similar bird and vector species with greater success.
7. Concluding Remarks
While USUV has caused significant outbreaks in birds since 2001, its limited circulation and overall low pathogenicity in humans explain why researchers and public health authorities are not yet too concerned about this pathogen. In the context of unprecedented viral circulation in 2018, and since USUV has now clearly been shown to be associated with neurological disorders, increased surveillance and research efforts are in order. In particular, larger cohort studies of populations of interest, such as wildlife workers and patients suffering from encephalitis, will help more accurately estimate USUV prevalence. Identifying molecular determinants associated with virulence, host tropism, and adaptation to new vectors may help anticipate key events leading to the possible emergence of USUV. Finally, developing antiviral approaches, or other preemptive or control measures in humans or at the reservoir-vector interface, will help control USUV circulation and reduce the economic and sanitary burden it may pose in the future.
Supplementary Materials
The following are available online at https://www.mdpi.com/1999-4915/11/7/640/s1, Table S1: List of USUV strains used to build the phylogenetic tree.
Funding
This work was funded by the DARPA PREEMPT program managed by Jim Gimlett, radley Ringeisen and Amy Jenkins and administered though DARPA Cooperative Agreement #HR001118S0017-PREEMPT-FP001 (the content of the information does not necessarily reflect the position or the policy of the U.S. government, and no official endorsement should be inferred).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Williams M.C., Simpson D.I., Haddow A.J., Knight E.M. THE ISOLATION OF WEST NILE VIRUS FROM MAN AND OF USUTU VIRUS FROM THE BIRD-BITING MOSQUITO MANSONIA AURITES (THEOBALD) IN THE ENTEBBE AREA OF UGANDA. Ann. Trop. Med. Parasitol. 1964;58:367–374. doi: 10.1080/00034983.1964.11686258. [DOI] [PubMed] [Google Scholar]
- 2.Nikolay B., Diallo M., Boye C.S., Sall A.A. Usutu virus in Africa. Vector Borne Zoonotic. Dis. 2011;11:1417–1423. doi: 10.1089/vbz.2011.0631. [DOI] [PubMed] [Google Scholar]
- 3.Weissenbock H., Kolodziejek J., Url A., Lussy H., Rebel-Bauder B., Nowotny N. Emergence of Usutu virus, an African mosquito-borne flavivirus of the Japanese encephalitis virus group, central Europe. Emerg. Infect. Dis. 2002;8:652–656. doi: 10.3201/eid0807.020094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weissenbock H., Bakonyi T., Rossi G., Mani P., Nowotny N. Usutu virus, Italy, 1996. Emerg. Infect. Dis. 2013;19:274–277. doi: 10.3201/eid1902.121191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kemenesi G., Buzas D., Zana B., Kurucz K., Krtinic B., Kepner A., Foldes F., Jakab F. First genetic characterization of Usutu virus from Culex pipiens mosquitoes Serbia, 2014. Transbound Emerg. Dis. 2018;63:58–61. doi: 10.1016/j.meegid.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Bakonyi T., Jungbauer C., Aberle S.W., Kolodziejek J., Dimmel K., Stiasny K., Allerberger F., Nowotny N. Usutu virus infections among blood donors, Austria, July and August 2017-Raising awareness for diagnostic challenges. Euro Surveill. 2017;22:17-00644. doi: 10.2807/1560-7917.ES.2017.22.41.17-00644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engel D., Jost H., Wink M., Borstler J., Bosch S., Garigliany M.M., Jost A., Czajka C., Luhken R., Ziegler U., et al. Reconstruction of the Evolutionary History and Dispersal of Usutu Virus, a Neglected Emerging Arbovirus in Europe and Africa. MBio. 2016;7:e01938-15. doi: 10.1128/mBio.01938-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cadar D., Luhken R., van der Jeugd H., Garigliany M., Ziegler U., Keller M., Lahoreau J., Lachmann L., Becker N., Kik M., et al. Widespread activity of multiple lineages of Usutu virus, western Europe, 2016. Euro Surveill. 2017;22:30452. doi: 10.2807/1560-7917.ES.2017.22.4.30452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calzolari M., Chiapponi C., Bonilauri P., Lelli D., Baioni L., Barbieri I., Lavazza A., Pongolini S., Dottori M., Moreno A. Co-circulation of two Usutu virus strains in Northern Italy between 2009 and 2014. Infect. Genet. Evol. 2017;51:255–262. doi: 10.1016/j.meegid.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Ben Hassine T., De Massis F., Calistri P., Savini G., BelHaj Mohamed B., Ranen A., Di Gennaro A., Sghaier S., Hammami S. First detection of co-circulation of West Nile and Usutu viruses in equids in the south-west of Tunisia. Transbound Emerg. Dis. 2014;61:385–389. doi: 10.1111/tbed.12259. [DOI] [PubMed] [Google Scholar]
- 11.Durand B., Haskouri H., Lowenski S., Vachiery N., Beck C., Lecollinet S. Seroprevalence of West Nile and Usutu viruses in military working horses and dogs, Morocco, 2012: Dog as an alternative WNV sentinel species? Epidemiol. Infect. 2016;144:1857–1864. doi: 10.1017/S095026881600011X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mannasse B., Mendelson E., Orshan L., Mor O., Shalom U., Yeger T., Lustig Y. Usutu Virus RNA in Mosquitoes, Israel, 2014–2015. Emerg. Infect. Dis. 2017;23:1699–1702. doi: 10.3201/eid2310.171017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaintoutis S.C., Dovas C.I., Papanastassopoulou M., Gewehr S., Danis K., Beck C., Lecollinet S., Antalis V., Kalaitzopoulou S., Panagiotopoulos T., et al. Evaluation of a West Nile virus surveillance and early warning system in Greece, based on domestic pigeons. Immunol. Microbiol. Infect. Dis. 2014;37:131–141. doi: 10.1016/j.cimid.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Eiden M., Gil P., Ziegler U., Rakotoarivony I., Marie A., Frances B., L’Ambert G., Simonin Y., Foulongne V., Groschup M.H., et al. Emergence of two Usutu virus lineages in Culex pipiens mosquitoes in the Camargue, France, 2015. Infect. Genet. Evol. 2018;61:151–154. doi: 10.1016/j.meegid.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Bakonyi T., Busquets N., Nowotny N. Comparison of complete genome sequences of Usutu virus strains detected in Spain, Central Europe, and Africa. Vector Borne Zoonotic Dis. 2014;14:324–329. doi: 10.1089/vbz.2013.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bazanow B., Jansen van Vuren P. A Survey on West Nile and Usutu Viruses in Horses and Birds in Poland. Viruses. 2018;10:87. doi: 10.3390/v10020087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bakonyi T., Erdelyi K., Ursu K., Ferenczi E., Csorgo T., Lussy H., Chvala S., Bukovsky C., Meister T., Weissenbock H., et al. Emergence of Usutu virus in Hungary. J. Clin. Microbiol. 2007;45:3870–3874. doi: 10.1128/JCM.01390-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rudolf I., Bakonyi T., Sebesta O., Mendel J., Pesko J., Betasova L., Blazejova H., Venclikova K., Strakova P., Nowotny N., et al. Co-circulation of Usutu virus and West Nile virus in a reed bed ecosystem. Parasit Vectors. 2015;8:520. doi: 10.1186/s13071-015-1139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buckley A., Dawson A., Moss S.R., Hinsley S.A., Bellamy P.E., Gould E.A. Serological evidence of West Nile virus, Usutu virus and Sindbis virus infection of birds in the UK. J. Gen. Virol. 2003;84:2807–2817. doi: 10.1099/vir.0.19341-0. [DOI] [PubMed] [Google Scholar]
- 20.Barbic L., Vilibic-Cavlek T., Listes E., Stevanovic V., Gjenero-Margan I., Ljubin-Sternak S., Pem-Novosel I., Listes I., Mlinaric-Galinovic G., Di Gennaro A., et al. Demonstration of Usutu virus antibodies in horses, Croatia. Vector Borne Zoonotic Dis. 2013;13:772–774. doi: 10.1089/vbz.2012.1236. [DOI] [PubMed] [Google Scholar]
- 21.Rijks J.M., Kik M.L., Slaterus R., Foppen R., Stroo A., Jzer J.I., Stahl J., Grone A., Koopmans M., van der Jeugd H.P., et al. Widespread Usutu virus outbreak in birds in the Netherlands, 2016. Euro Surveill. 2016;21:30391. doi: 10.2807/1560-7917.ES.2016.21.45.30391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steinmetz H.W., Bakonyi T., Weissenbock H., Hatt J.M., Eulenberger U., Robert N., Hoop R., Nowotny N. Emergence and establishment of Usutu virus infection in wild and captive avian species in and around Zurich, Switzerland--genomic and pathologic comparison to other central European outbreaks. Vet. Microbiol. 2011;148:207–212. doi: 10.1016/j.vetmic.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Manarolla G., Bakonyi T., Gallazzi D., Crosta L., Weissenbock H., Dorrestein G.M., Nowotny N. Usutu virus in wild birds in northern Italy. Vet. Microbiol. 2010;141:159–163. doi: 10.1016/j.vetmic.2009.07.036. [DOI] [PubMed] [Google Scholar]
- 24.Jost H., Bialonski A., Maus D., Sambri V., Eiden M., Groschup M.H., Gunther S., Becker N., Schmidt-Chanasit J. Isolation of usutu virus in Germany. Am. J. Trop. Med. Hyg. 2011;85:551–553. doi: 10.4269/ajtmh.2011.11-0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sieg M., Schmidt V., Ziegler U., Keller M., Hoper D., Heenemann K., Ruckner A., Nieper H., Muluneh A., Groschup M.H., et al. Outbreak and Cocirculation of Three Different Usutu Virus Strains in Eastern Germany. PLoS Negl. Trop. Dis. 2017;17:662–664. doi: 10.1089/vbz.2016.2096. [DOI] [PubMed] [Google Scholar]
- 26.Ziegler U., Fast C., Eiden M., Bock S., Schulze C., Hoeper D., Ochs A., Schlieben P., Keller M., Zielke D.E., et al. Evidence for an independent third Usutu virus introduction into Germany. BMC Vet. Res. 2016;192:60–66. doi: 10.1016/j.vetmic.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Gaibani P., Cavrini F., Gould E.A., Rossini G., Pierro A., Landini M.P., Sambri V. Comparative genomic and phylogenetic analysis of the first Usutu virus isolate from a human patient presenting with neurological symptoms. PLoS ONE. 2013;8:e64761. doi: 10.1371/journal.pone.0064761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cavrini F., Gaibani P., Longo G., Pierro A.M., Rossini G., Bonilauri P., Gerunda G.E., Di Benedetto F., Pasetto A., Girardis M., et al. Usutu virus infection in a patient who underwent orthotropic liver transplantation, Italy, August-September 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.50.19448-en. [DOI] [PubMed] [Google Scholar]
- 29.Nikolay B. A review of West Nile and Usutu virus co-circulation in Europe: How much do transmission cycles overlap? Trans. R. Soc. Trop. Med. Hyg. 2015;109:609–618. doi: 10.1093/trstmh/trv066. [DOI] [PubMed] [Google Scholar]
- 30.Tamba M., Bonilauri P., Bellini R., Calzolari M., Albieri A., Sambri V., Dottori M., Angelini P. Detection of Usutu virus within a West Nile virus surveillance program in Northern Italy. Vector Borne Zoonotic Dis. 2011;11:551–557. doi: 10.1089/vbz.2010.0055. [DOI] [PubMed] [Google Scholar]
- 31.Vilibic-Cavlek T., Kaic B., Barbic L., Pem-Novosel I., Slavic-Vrzic V., Lesnikar V., Kurecic-Filipovic S., Babic-Erceg A., Listes E., Stevanovic V., et al. First evidence of simultaneous occurrence of West Nile virus and Usutu virus neuroinvasive disease in humans in Croatia during the 2013 outbreak. Infection. 2014;42:689–695. doi: 10.1007/s15010-014-0625-1. [DOI] [PubMed] [Google Scholar]
- 32.Aberle S.W., Kolodziejek J., Jungbauer C., Stiasny K., Aberle J.H., Zoufaly A., Hourfar M.K., Weidner L., Nowotny N. Increase in human West Nile and Usutu virus infections, Austria, 2018. Euro Surveill. 2018;23 doi: 10.2807/1560-7917.ES.2018.23.43.1800545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nikolay B., Fall G., Boye C.S., Sall A.A., Skern T. Validation of a structural comparison of the antigenic characteristics of Usutu virus and West Nile virus envelope proteins. Virus Res. 2014;189:87–91. doi: 10.1016/j.virusres.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 34.Chen Z., Ye F., Lin S., Yang F., Cheng Y., Cao Y., Chen Z., Lu G. Crystal structure of Usutu virus envelope protein in the pre-fusion state. Virol. J. 2018;15:183. doi: 10.1186/s12985-018-1092-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beck C., Jimenez-Clavero M.A., Leblond A., Durand B., Nowotny N., Leparc-Goffart I., Zientara S., Jourdain E., Lecollinet S. Flaviviruses in Europe: Complex circulation patterns and their consequences for the diagnosis and control of West Nile disease. Int. J. Environ. Res. Public Health. 2013;10:6049–6083. doi: 10.3390/ijerph10116049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Llorente F., Garcia-Irazabal A., Perez-Ramirez E., Cano-Gomez C., Sarasa M., Vazquez A., Jimenez-Clavero M.A. Influence of flavivirus co-circulation in serological diagnostics and surveillance: A model of study using West Nile, Usutu and Bagaza viruses. Transbound Emerg. Dis. 2019 doi: 10.1111/tbed.13262. [DOI] [PubMed] [Google Scholar]
- 37.Cleton N.B., van Maanen K., Bergervoet S.A., Bon N., Beck C., Godeke G.J., Lecollinet S., Bowen R., Lelli D., Nowotny N., et al. A Serological Protein Microarray for Detection of Multiple Cross-Reactive Flavivirus Infections in Horses for Veterinary and Public Health Surveillance. Transbound Emerg. Dis. 2017;64:1801–1812. doi: 10.1111/tbed.12569. [DOI] [PubMed] [Google Scholar]
- 38.Del Amo J., Sotelo E., Fernandez-Pinero J., Gallardo C., Llorente F., Aguero M., Jimenez-Clavero M.A. A novel quantitative multiplex real-time RT-PCR for the simultaneous detection and differentiation of West Nile virus lineages 1 and 2, and of Usutu virus. J. Virol. Methods. 2013;189:321–327. doi: 10.1016/j.jviromet.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 39.Merino-Ramos T., Blazquez A.B., Escribano-Romero E., Canas-Arranz R., Sobrino F., Saiz J.C., Martin-Acebes M.A. Protection of a single dose west nile virus recombinant subviral particle vaccine against lineage 1 or 2 strains and analysis of the cross-reactivity with Usutu virus. PLoS ONE. 2014;9:e108056. doi: 10.1371/journal.pone.0108056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blazquez A.B., Escribano-Romero E., Martin-Acebes M.A., Petrovic T., Saiz J.C. Limited susceptibility of mice to Usutu virus (USUV) infection and induction of flavivirus cross-protective immunity. Virology. 2015;482:67–71. doi: 10.1016/j.virol.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 41.Mancini G., Montarsi F., Calzolari M., Capelli G., Dottori M., Ravagnan S., Lelli D., Chiari M., Santilli A., Quaglia M., et al. Mosquito species involved in the circulation of West Nile and Usutu viruses in Italy. Vet. Ital. 2017;53:97–110. doi: 10.12834/VetIt.114.933.4764.2. [DOI] [PubMed] [Google Scholar]
- 42.Lebl K., Zittra C., Silbermayr K., Obwaller A., Berer D., Brugger K., Walter M., Pinior B., Fuehrer H.P., Rubel F. Mosquitoes (Diptera: Culicidae) and their relevance as disease vectors in the city of Vienna, Austria. Parasitol. Res. 2015;114:707–713. doi: 10.1007/s00436-014-4237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fros J.J., Miesen P., Vogels C.B., Gaibani P., Sambri V., Martina B.E., Koenraadt C.J., van Rij R.P., Vlak J.M., Takken W., et al. Comparative Usutu and West Nile virus transmission potential by local Culex pipiens mosquitoes in north-western Europe. One Health. 2015;1:31–36. doi: 10.1016/j.onehlt.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hernandez-Triana L.M., de Marco M.F., Mansfield K.L., Thorne L., Lumley S., Marston D., Fooks A.A., Johnson N. Assessment of vector competence of UK mosquitoes for Usutu virus of African origin. PLoS Negl. Trop. Dis. 2018;11:381. doi: 10.1186/s13071-018-2959-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cook C.L., Huang Y.S., Lyons A.C., Alto B.W., Unlu I., Higgs S., Vanlandingham D.L. North American Culex pipiens and Culex quinquefasciatus are competent vectors for Usutu virus. PLoS Negl. Trop. Dis. 2018;12:e0006732. doi: 10.1371/journal.pntd.0006732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Camp J.V., Kolodziejek J., Nowotny N. Targeted surveillance reveals native and invasive mosquito species infected with Usutu virus. Parasit Vectors. 2019;12:46. doi: 10.1186/s13071-019-3316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nikolay B., Diallo M., Faye O., Boye C.S., Sall A.A. Vector competence of Culex neavei (Diptera: Culicidae) for Usutu virus. Am. J. Trop. Med. Hyg. 2012;86:993–996. doi: 10.4269/ajtmh.2012.11-0509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Calzolari M., Bonilauri P., Bellini R., Albieri A., Defilippo F., Maioli G., Galletti G., Gelati A., Barbieri I., Tamba M., et al. Evidence of simultaneous circulation of West Nile and Usutu viruses in mosquitoes sampled in Emilia-Romagna region (Italy) in 2009. PLoS ONE. 2010;5:e14324. doi: 10.1371/journal.pone.0014324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Calzolari M., Gaibani P., Bellini R., Defilippo F., Pierro A., Albieri A., Maioli G., Luppi A., Rossini G., Balzani A., et al. Mosquito, bird and human surveillance of West Nile and Usutu viruses in Emilia-Romagna Region (Italy) in 2010. PLoS ONE. 2012;7:e38058. doi: 10.1371/journal.pone.0038058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Puggioli A., Bonilauri P., Calzolari M., Lelli D., Carrieri M., Urbanelli S., Pudar D., Bellini R. Does Aedes albopictus (Diptera: Culicidae) play any role in Usutu virus transmission in Northern Italy? Experimental oral infection and field evidences. Acta. Trop. 2017;172:192–196. doi: 10.1016/j.actatropica.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 51.Llopis I.V., Tomassone L., Grego E., Silvano F., Rossi L. Investigation into Usutu and West Nile viruses in ticks from wild birds in Northwestern Italy, 2012-2014. New Microbiol. 2017;40:56–57. [PubMed] [Google Scholar]
- 52.Mancini F., Toma L., Ciervo A., Di Luca M., Faggioni G., Lista F., Rezza G. Virus investigation in ticks from migratory birds in Italy. New Microbiol. 2013;36:433–434. [PubMed] [Google Scholar]
- 53.Schuffenecker I., Iteman I., Michault A., Murri S., Frangeul L., Vaney M.C., Lavenir R., Pardigon N., Reynes J.M., Pettinelli F., et al. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 2006;3:e263. doi: 10.1371/journal.pmed.0030263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Benzarti E., Linden A., Desmecht D., Garigliany M. Mosquito-borne epornitic flaviviruses: An update and review. J. Gen. Virol. 2019;100:119–132. doi: 10.1099/jgv.0.001203. [DOI] [PubMed] [Google Scholar]
- 55.Weissenbock H., Kolodziejek J., Fragner K., Kuhn R., Pfeffer M., Nowotny N. Usutu virus activity in Austria, 2001–2002. Microbes. Infect. 2003;5:1132–1136. doi: 10.1016/S1286-4579(03)00204-1. [DOI] [PubMed] [Google Scholar]
- 56.Becker N., Jost H., Ziegler U., Eiden M., Hoper D., Emmerich P., Fichet-Calvet E., Ehichioya D.U., Czajka C., Gabriel M., et al. Epizootic emergence of Usutu virus in wild and captive birds in Germany. PLoS ONE. 2012;7:e32604. doi: 10.1371/annotation/6841c4e1-58e6-4412-9b71-bd6bc8bbe549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chvala S., Kolodziejek J., Nowotny N., Weissenbock H. Pathology and viral distribution in fatal Usutu virus infections of birds from the 2001 and 2002 outbreaks in Austria. J. Comp. Pathol. 2004;131:176–185. doi: 10.1016/j.jcpa.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 58.Bergsman L.D., Hyman J.M., Manore C.A. A mathematical model for the spread of west nile virus in migratory and resident birds. Math. Biosci. Eng. 2016;13:401–424. doi: 10.3934/mbe.2015009. [DOI] [PubMed] [Google Scholar]
- 59.Lecollinet S., Blanchard Y., Manson C., Lowenski S., Laloy E., Quenault H., Touzain F., Lucas P., Eraud C., Bahuon C., et al. Dual Emergence of Usutu Virus in Common Blackbirds, Eastern France, 2015. Emerg. Infect. Dis. 2016;22:2225. doi: 10.3201/eid2212.161272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meister T., Lussy H., Bakonyi T., Sikutova S., Rudolf I., Vogl W., Winkler H., Frey H., Hubalek Z., Nowotny N., et al. Serological evidence of continuing high Usutu virus (Flaviviridae) activity and establishment of herd immunity in wild birds in Austria. Vet. Microbiol. 2008;127:237–248. doi: 10.1016/j.vetmic.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 61.Chvala S., Bakonyi T., Hackl R., Hess M., Nowotny N., Weissenbock H. Limited pathogenicity of Usutu virus for the domestic chicken (Gallus domesticus) Avian Pathol. 2005;34:392–395. doi: 10.1080/03079450500268500. [DOI] [PubMed] [Google Scholar]
- 62.Chvala S., Bakonyi T., Hackl R., Hess M., Nowotny N., Weissenbock H. Limited pathogenicity of usutu virus for the domestic goose (Anser anser f. domestica) following experimental inoculation. J. Vet. Med. B Infect. Dis. Vet. Public Health. 2006;53:171–175. doi: 10.1111/j.1439-0450.2006.00942.x. [DOI] [PubMed] [Google Scholar]
- 63.Rouffaer L.O., Steensels M., Verlinden M., Vervaeke M., Boonyarittichaikij R., Martel A., Lambrecht B. Usutu Virus Epizootic and Plasmodium Coinfection in Eurasian Blackbirds (Turdus merula) in Flanders, Belgium. J. Wildl. Dis. 2018;54:859–862. doi: 10.7589/2017-07-163. [DOI] [PubMed] [Google Scholar]
- 64.Vanhomwegen J., Beck C., Despres P., Figuerola A., Garcia R., Lecollinet S., Lopez-Roig M., Manuguerra J.C., Serra-Cobo J. Circulation of Zoonotic Arboviruses in Equine Populations of Mallorca Island (Spain) Vector Borne Zoonotic Dis. 2017;17:340–346. doi: 10.1089/vbz.2016.2042. [DOI] [PubMed] [Google Scholar]
- 65.Lupulovic D., Martin-Acebes M.A., Lazic S., Alonso-Padilla J., Blazquez A.B., Escribano-Romero E., Petrovic T., Saiz J.C. First serological evidence of West Nile virus activity in horses in Serbia. Vector Borne Zoonotic Dis. 2011;11:1303–1305. doi: 10.1089/vbz.2010.0249. [DOI] [PubMed] [Google Scholar]
- 66.Montagnaro S., Piantedosi D., Ciarcia R., Loponte R., Veneziano V., Fusco G., Amoroso M.G., Ferrara G., Damiano S., Iovane G., et al. Serological Evidence of Mosquito-Borne Flaviviruses Circulation in Hunting Dogs in Campania Region, Italy. Vector Borne Zoonotic Dis. 2019;19:142–147. doi: 10.1089/vbz.2018.2337. [DOI] [PubMed] [Google Scholar]
- 67.Busani L., Capelli G., Cecchinato M., Lorenzetto M., Savini G., Terregino C., Vio P., Bonfanti L., Pozza M.D., Marangon S. West Nile virus circulation in Veneto region in 2008-2009. Epidemiol. Infect. 2011;139:818–825. doi: 10.1017/S0950268810001871. [DOI] [PubMed] [Google Scholar]
- 68.Garcia-Bocanegra I., Paniagua J., Gutierrez-Guzman A.V., Lecollinet S., Boadella M., Arenas-Montes A., Cano-Terriza D., Lowenski S., Gortazar C., Hofle U. Spatio-temporal trends and risk factors affecting West Nile virus and related flavivirus exposure in Spanish wild ruminants. BMC Vet. Res. 2016;12:249. doi: 10.1186/s12917-016-0876-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Escribano-Romero E., Lupulovic D., Merino-Ramos T., Blazquez A.B., Lazic G., Lazic S., Saiz J.C., Petrovic T. West Nile virus serosurveillance in pigs, wild boars, and roe deer in Serbia. Vet. Microbiol. 2015;176:365–369. doi: 10.1016/j.vetmic.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 70.Cadar D., Becker N., Campos Rde M., Borstler J., Jost H., Schmidt-Chanasit J. Usutu virus in bats, Germany, 2013. Emerg. Infect. Dis. 2014;20:1771–1773. doi: 10.3201/eid2010.140909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Romeo C., Lecollinet S. Are tree squirrels involved in the circulation of flaviviruses in Italy? Transbound Emerg. Dis. 2018;65:1372–1376. doi: 10.1111/tbed.12874. [DOI] [PubMed] [Google Scholar]
- 72.Diagne M.M., Ndione M.H.D., Di Paola N., Fall G., Bedekelabou A.P. Usutu Virus Isolated from Rodents in Senegal. Viruses. 2019;11:181. doi: 10.3390/v11020181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cle M., Salinas S., Lecollinet S., Beck C., Gutierrez S., Baldet T., Vande Perre P., Foulongne V., Simonin Y. Usutu virus: The phantom menace. Med. Sci. (Paris) 2018;34:709–716. doi: 10.1051/medsci/20183408018. [DOI] [PubMed] [Google Scholar]
- 74.Pecorari M., Longo G., Gennari W., Grottola A., Sabbatini A., Tagliazucchi S., Savini G., Monaco F., Simone M., Lelli R., et al. First human case of Usutu virus neuroinvasive infection, Italy, August-September 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.50.19446-en. [DOI] [PubMed] [Google Scholar]
- 75.Simonin Y., Sillam O., Carles M.J., Gutierrez S., Gil P., Constant O., Martin M.F., Girard G., Van de Perre P., Salinas S., et al. Human Usutu Virus Infection with Atypical Neurologic Presentation, Montpellier, France, 2016. Emerg. Infect. Dis. 2018;24:875–878. doi: 10.3201/eid2405.171122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Allering L., Jost H., Emmerich P., Gunther S., Lattwein E., Schmidt M., Seifried E., Sambri V., Hourfar K., Schmidt-Chanasit J. Detection of Usutu virus infection in a healthy blood donor from south-west Germany, 2012. Euro Surveill. 2012;17 doi: 10.2807/ese.17.50.20341-en. [DOI] [PubMed] [Google Scholar]
- 77.Pierro A., Gaibani P., Spadafora C., Ruggeri D., Randi V., Parenti S., Finarelli A.C., Rossini G., Landini M.P., Sambri V. Detection of specific antibodies against West Nile and Usutu viruses in healthy blood donors in northern Italy, 2010–2011. Clin. Microbiol. Infect. 2013;19:E451–E453. doi: 10.1111/1469-0691.12241. [DOI] [PubMed] [Google Scholar]
- 78.Cvjetković I.H., Petrović T., Petrić D., Cvjetković D., Kovačević G., Radovanov J., Galović A.J., Patić A., Nikolić N., Mikić S.S. Seroprevalence of mosquito-born and tick-born microorganisms in human population of South Backa District. Arhiv. Veterinarske Med. 2016;9:23–30. [Google Scholar]
- 79.Percivalle E., Sassera D., Rovida F., Isernia P., Fabbi M., Baldanti F., Marone P. Usutu Virus Antibodies in Blood Donors and Healthy Forestry Workers in the Lombardy Region, Northern Italy. Vector Borne Zoonotic Dis. 2017;17:658–661. doi: 10.1089/vbz.2017.2126. [DOI] [PubMed] [Google Scholar]
- 80.Grottola A., Marcacci M., Tagliazucchi S., Gennari W., Di A.G., Orsini M., Monaco F., Marchegiano P., Marini V., Meacci M., et al. Usutu virus infections in humans: A retrospective analysis in the municipality of Modena, Italy. Clin. Microbiol. Infect. 2017;23:33–37. doi: 10.1016/j.cmi.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 81.Maggi F., Mazzetti P., Focosi D., Macera L., Scagnolari C., Manzin A., Antonelli G., Nelli L.C. Lack of usutu virus RNA in cerebrospinal fluid of patients with encephalitis of unknown etiology, Tuscany, Italy. J. Med. Virol. 2015;87:913–916. doi: 10.1002/jmv.24149. [DOI] [PubMed] [Google Scholar]
- 82.Cordey S., Vieille G., Turin L., Kaiser L. Usutu virus in cerebrospinal fluid: A 2-year survey in a Tertiary Care Hospital, Geneva, Switzerland. J. Med. Virol. 2018;90:609–611. doi: 10.1002/jmv.24967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cavrini F., Della Pepa M.E., Gaibani P., Pierro A.M., Rossini G., Landini M.P., Sambri V. A rapid and specific real-time RT-PCR assay to identify Usutu virus in human plasma, serum, and cerebrospinal fluid. J. Clin. Virol. 2011;50:221–223. doi: 10.1016/j.jcv.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 84.Weissenbock H., Bakonyi T., Chvala S., Nowotny N. Experimental Usutu virus infection of suckling mice causes neuronal and glial cell apoptosis and demyelination. Acta. Neuropathol. 2004;108:453–460. doi: 10.1007/s00401-004-0916-1. [DOI] [PubMed] [Google Scholar]
- 85.Salinas S., Constant O., Desmetz C. Deleterious effect of Usutu virus on human neural cells. PLoS Negl. Trop. Dis. 2017;11:e0005913. doi: 10.1371/journal.pntd.0005913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vielle N.J., Garcia-Nicolas O., Oliveira Esteves B.I., Brugger M., Summerfield A., Alves M.P. The Human Upper Respiratory Tract Epithelium Is Susceptible to Flaviviruses. Front. Microbiol. 2019;10:811. doi: 10.3389/fmicb.2019.00811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sembene P.M., Faye O., Zanotto P.M.A., Sall A.A., Garcia-Nicolas O., Lewandowska M., Ricklin M.E., Summerfield A. Monocyte-Derived Dendritic Cells as Model to Evaluate Species Tropism of Mosquito-Borne Flaviviruses. Viruses. 2019;9:5. doi: 10.3389/fcimb.2019.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cacciotti G., Caputo B., Selvaggi C., la Sala A., Vitiello L., Diallo D., Ceianu C., Antonelli G., Nowotny N., Scagnolari C. Variation in interferon sensitivity and induction between Usutu and West Nile (lineages 1 and 2) viruses. Virology. 2015;485:189–198. doi: 10.1016/j.virol.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 89.Segura Guerrero N.A., Sharma S., Neyts J., Kaptein S.J.F. Favipiravir inhibits in vitro Usutu virus replication and delays disease progression in an infection model in mice. Antiviral Res. 2018;160:137–142. doi: 10.1016/j.antiviral.2018.10.026. [DOI] [PubMed] [Google Scholar]
- 90.Blazquez A.B., Escribano-Romero E., Merino-Ramos T., Saiz J.C., Martin-Acebes M.A. Infection with Usutu virus induces an autophagic response in mammalian cells. PLoS Negl. Trop. Dis. 2013;7:e2509. doi: 10.1371/journal.pntd.0002509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Echavarria-Consuegra L., Smit J.M., Reggiori F. Role of autophagy during the replication and pathogenesis of common mosquito-borne flavi- and alphaviruses. Open Biol. 2019;9:190009. doi: 10.1098/rsob.190009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Merino-Ramos T., Vazquez-Calvo A., Casas J., Sobrino F., Saiz J.C., Martin-Acebes M.A. Modification of the Host Cell Lipid Metabolism Induced by Hypolipidemic Drugs Targeting the Acetyl Coenzyme A Carboxylase Impairs West Nile Virus Replication. Antimicrob. Agents. Chemother. 2016;60:307–315. doi: 10.1128/AAC.01578-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Papa A. Emerging arboviruses of medical importance in the Mediterranean region. J. Clin. Virol. 2019;115:5–10. doi: 10.1016/j.jcv.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 94.Walter M., Brugger K., Rubel F. Usutu virus induced mass mortalities of songbirds in Central Europe: Are habitat models suitable to predict dead birds in unsampled regions? Prev. Vet. Med. 2018;159:162–170. doi: 10.1016/j.prevetmed.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 95.Rubel F., Brugger K., Hantel M., Chvala-Mannsberger S., Bakonyi T., Weissenbock H., Nowotny N. Explaining Usutu virus dynamics in Austria: Model development and calibration. Prev. Vet. Med. 2008;85:166–186. doi: 10.1016/j.prevetmed.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 96.Brugger K., Rubel F. Simulation of climate-change scenarios to explain Usutu-virus dynamics in Austria. Prev. Vet. Med. 2009;88:24–31. doi: 10.1016/j.prevetmed.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 97.Cheng Y., Tjaden N.B., Jaeschke A., Luhken R., Ziegler U., Thomas S.M., Beierkuhnlein C. Evaluating the risk for Usutu virus circulation in Europe: Comparison of environmental niche models and epidemiological models. Int. J. Health Geogr. 2018;17:35. doi: 10.1186/s12942-018-0155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tiawsirisup S., Kinley J.R., Tucker B.J., Evans R.B., Rowley W.A., Platt K.B. Vector competence of Aedes vexans (Diptera: Culicidae) for West Nile virus and potential as an enzootic vector. J. Med. Entomol. 2008;45:452–457. doi: 10.1603/0022-2585(2008)45[452:VCOAVD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 99.Veronesi E., Paslaru A., Silaghi C., Tobler K., Glavinic U., Torgerson P., Mathis A. Experimental evaluation of infection, dissemination, and transmission rates for two West Nile virus strains in European Aedes japonicus under a fluctuating temperature regime. Parasitol. Res. 2018;117:1925–1932. doi: 10.1007/s00436-018-5886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fortuna C., Remoli M.E., Severini F., Di Luca M., Toma L., Fois F., Bucci P., Boccolini D., Romi R., Ciufolini M.G. Evaluation of vector competence for West Nile virus in Italian Stegomyia albopicta (=Aedes albopictus) mosquitoes. Med. Vet. Entomol. 2015;29:430–433. doi: 10.1111/mve.12133. [DOI] [PubMed] [Google Scholar]
- 101.Kusne S., Smilack J. Transmission of West Nile virus by organ transplantation. Liver Transpl. 2005;11:239–241. doi: 10.1002/lt.20350. [DOI] [PubMed] [Google Scholar]
- 102.Hayes E.B., O’Leary D.R. West Nile virus infection: A pediatric perspective. Pediatrics. 2004;113:1375–1381. doi: 10.1542/peds.113.5.1375. [DOI] [PubMed] [Google Scholar]
- 103.Zmurko J., Neyts J., Dallmeier K. Flaviviral NS4b, chameleon and jack-in-the-box roles in viral replication and pathogenesis, and a molecular target for antiviral intervention. Rev. Med. Virol. 2015;25:205–223. doi: 10.1002/rmv.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Reisen W.K., Lothrop H.D., Wheeler S.S., Kennsington M., Gutierrez A., Fang Y., Garcia S., Lothrop B. Persistent West Nile virus transmission and the apparent displacement St. Louis encephalitis virus in southeastern California, 2003–2006. J. Med. Entomol. 2008;45:494–508. doi: 10.1603/0022-2585(2008)45[494:pwnvta]2.0.co;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Diaz A., Coffey L.L., Burkett-Cadena N., Day J.F. Reemergence of St. Louis Encephalitis Virus in the Americas. Emerg. Infect. Dis. 2018;24:2150. doi: 10.3201/eid2412.180372. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.