Abstract
Introduction
Hypnosis is a therapeutic strategy for pain control. We aimed at investigating the use of this technique in a large population undergoing atrial fibrillation (AF) ablation.
Methods
70 consecutive AF patients referred for transcatheter ablation, underwent hypnotic communication for periprocedural analgesia (Group A), were compared with 70 patients undergoing conventional analgesia (Group B). Procedural data, anxiety, perceived pain, perceived procedural duration and the dosages of administered analgesic drugs were compared using validated score scales.
Results
Hypnotic communication (Group A) resulted in a significant procedural-related anxiety reduction (Pre procedural 4.7 ± 2.9 Vs Intra Procedural 0.8 ± 1.2, P < 0.001) and perceived procedural duration (Real length 108 ± 33 min Vs Perceived Length 77 ± 39 min, P < 0.001). Group A patients reported a painless procedure in 78% (Pain scale ≤2). Regarding analgesic drug, Group A used only Fentanyl and Paracetamol. The Fentanyl dosage was similar in Group A and B (mean 0.142 Vs 0.146 mg, P = 0.65) while higher Paracetamol dosage was reported in Group A (mean 853 Vs 337 mg, P < 0.001). Group B also used Midazolam (mean 1.8 mg), Propofol (mean 43.8 mg) and narcosis was required in 2 patients. Total radiofrequency (RF) delivered time did not differ between the two groups (mean 28.9 Vs 27.6 min, P = 0.623) as well as mean RF power (mean 35.3 Vs 35.5 W, P = 0.424). No complications occurred.
Conclusion
Hypnotic communication during AF ablation was related to a significant reduction of intra-procedural anxiety, perceived pain, procedural analgesic drugs dosage and perceived procedural duration without affecting total RF delivered time and procedural safety.
Keywords: Atrial fibrillation, Ablation, Hypnosis
1. Introduction
Atrial fibrillation (AF) is the most prevalent clinical supraventricular arrhythmia [1]. Catheter ablation of AF is a widely performed effective therapy for symptomatic patients since 20 years ago [2]. However, it generally requires long procedural times and furthermore, patients should be still on the table to avoid movements that may interfere with the ablation workflow. Therefore, pain control during the procedure is becoming crucial for safety and effectiveness. Pain control can be obtained using analgesic drugs and sedation or by the means of narcosis. The second approach, although it is much more effective, needs a more complex set up with the presence of an anesthesiologist and dedicated devices. In addition, there is not interaction between the physician and the patient.
In the recent years, hypnosis is emerging as an effective strategy for acute and chronic pain control. Hypnosis is defined as a modified state of consciousness characterized by reduced self-awareness associated with an enhanced capacity for response to suggestion [3]. Several reports are available about the use of hypnosis for managing chronic pain problems and pain during surgical procedures. Hypnosis and traditional analgesia techniques have a synergistic effect, allowing a reduction in the use of analgesics and sedative drugs [4,5].
Few data are available for the role of the use of hypnosis in cardiovascular patients: few reports have been published in case of percutaneous coronary intervention and during transesophageal echocardiography [6,7]. A recent case series experience [8], described that hypnotic communication allows to perform a discomfortless electrophysiological procedure. However, no data are available about the use of this technique in a large population undergoing AF catheter ablation. Most of the electrophysiology laboratories use the traditional technique, based on analgesic drugs and/or narcosis, requiring often the use of Propofol, Midazolam, Fentanyl, Remifentanil that may have adverse events (negative inotropic effect, respiratory depression). Conversely, hypnosis conducted by a trained therapist or health care professional is a safe practice, without severe adverse effects and its use may help carrying out the procedure reducing or even avoiding the need of the drugs [9].
Based on these previous considerations we decided to perform a study aiming to assess the potential role and results of the hypnosis technique as adjunctive strategy for pain control during paroxysmal/persistent AF catheter ablation. To accomplish this goal we compared prospectively a group of patients undergoing AF ablation with the addition of hypnosis with a second group undergone AF ablation with our standard pain control approach.
2. Methods
2.1. Study population
Between March 2018 and December 2018, we enrolled 140 consecutive AF patients referred to our center (Cardinal Massaia Hospital, Asti, Italy) for the first procedure of catheter ablation. The patients were prospectively assigned to Group A (n 70 patients) and Group B (n 70 patients). About patient's group assignment no pre-procedural tests were used to identify patients most suitable for hypnosis. Patients were allocated to Group A or B, respectively, in a sequential, prospective 1:1 ratio. Group A patients underwent ablation procedure with hypnotic communication as an adjuvant approach for periprocedural analgesia. Group B patients underwent ablation with conventional analgesic approach and were used as control group. AF was stratified as paroxysmal or persistent according to recent European Society of Cardiology guidelines [2]. All the two group patients underwent only pulmonary vein isolation.
The study was conducted in compliance with the good clinical practices protocol and Declaration of Helsinki principles. All patients signed informed consent before undergoing the procedure and to be clinically followed thereafter.
Each patient underwent trans-esophageal echocardiography (TEE) before ablation in order to rule out the presence of thrombi in the left atrium (LA) or in the left atrial appendage (LAA). A contrast-enhanced magnetic resonance imaging (MRI) of the LA was obtained and merged with the cardiac chamber reconstruction performed during the ablation procedure.
2.2. Ablation procedure
Traditional fluoroscopic view and navigation system CARTO3 EAM (Electro Anatomic Mapping) (Biosense Webster, Diamond Bar, CA) and Nav-X (St. Jude), providing real-time visualization of multiple catheters as in a standard fluoroscopic view, were used. The procedure was performed via both right and left femoral veins. A decapolar electrode catheter was positioned in the coronary sinus (Decanav, Biosense Webster, Diamond Bar, CA or Livewire 2-5-2, St. Jude) and the LA was accessed by the means of a septal puncture or through a patent foramen ovale (PFO), if present. The ablation catheter (Thermocool SF Smarttouch catheter, Biosense Webster Inc., CA, Tacticath Sensor Enabled St Jude) was inserted into the LA through the same septal. After LA access was gained, all the patients underwent an EAM reconstruction that was merged with the MRI. In every patient, total procedural time, ablation time and total fluoroscopy time were recorded. In Group A patients time required to reach the hypnotic status was recorded.
For each patient, procedural endpoint was PV isolation, demonstrated as disappearance of PV potentials on the circular mapping catheter and entrance/exit block when pacing from the LA/PV. Radiofrequency (RF) energy was delivered to create a circumferential lesion around the PV antrum using maximum power up to 45 W (range 30-45 W).
All patients on vitamin K antagonist (VKA) performed the ablation procedure with a target INR of 2-2.5 the day of the procedure. On the other side, if the patient was taking direct oral anticoagulants (DOACs), the decision whether to stop the medication only the morning of the procedure or earlier, was based on the type of anticoagulant taken, the renal function and the bleeding risk. After the ablation procedure a transthoracic echocardiography (TTE) was performed in all patients to assess for the presence of pericardial effusion.
2.3. Pain control protocol
-
1)
Local anesthesia with Lidocaine 2% 10 ml was administered in each groin to manage femoral access.
-
2)
If the patient did not experience anxiety or pain, no further drugs were administered until the left atrium mapping was completed
-
3)
Ad this point, before starting the RF delivery, Fentanyl 0.05 mg bolus was given as a standard protocol in both groups.
-
4)
Further doses of analgesic/sedative drugs were administered in both groups during the procedure depending on the patients' tolerance.
-
5)
In case of patient's intolerance to the procedure despite the drug's use, narcosis was applied.
2.4. Hypnotic approach
All the health professionals, either physician or nurse, were trained in hypnotic communication attending a specific in-hospital course held by Tutors belonging to the “Istituto Franco Granone - Centro Italiano Ipnosi Clinico Sperimentale of Turin” achieving complete autonomy in the hypnotic communication. Group A: once the patient was in the electrophysiological (EP) laboratory the health professional trained in hypnotic communication had a preparatory conversation with the patient to prove the absence of contraindications for hypnosis and to test the patient's compliance. Cognitive impairment and/or psychiatric disorders were considered as exclusion criteria for enrollment. At this point, the trained health professional (either physician or nurse) started the hypnotic communication. He/she was required to stay in the EP laboratory for the entire length of the procedure to manage hypnosis. In our center there are 8 professionals (4 physicians and 4 nurses) trained in this technique and all of them were involved in a rotating shift fashion regardless to be first operator or not.
The hypnotic workflow may be divided into the following steps:
-
A.
Checking confirmation of the indication; explanation of the medical care, lowering of inappropriate anxiety and definition of aim (trading)
-
B.
Focusing patient's attention in order to be dissociated from the surrounding
-
C.
Suggestions
-
D.
Validation of hypnotic status
-
E.
Reinforcement and consolidation
-
F.
Posthypnotic suggestions (self-hypnosis)
-
G.
Discussion (physician-patient comparison)
Once the patient entered the EP laboratory was monitored and all the EAM systems patches were applied. Before applying the sterile drape on the patient on the surgical bed, the hypnotic status was induced. The operator used, at his discretion, the internal focusing technique (focusing the patient's attention to an inner perception such as breathing) or the external focusing technique (concentrating the patient's attention toward a visible, external point of interest) as described by step B of the hypnotic workflow. Step C consisted in giving suggestions to the patient aiming to lower his critical thinking, leading him to a modified state of mind (para-physiologic) with muscle relaxation and regular breath, guiding his mind toward a pleasant place or situation. At this point a focused analgesia was induced by means of metaphoric suggestions and hypnotic status was validated by means of a sharp needle puncture in different sites of the body (Workflow step D).
The patient rest in this status characterized by a change in the external stimuli consciousness and space-time orientation. From the outside the patient seems to be asleep but from the inside his mind is alert and awake and in control. During the procedure the operator reinforced and consolidated this status interacting verbally with the patient (Workflow step E). Approaching the end of the procedure, before to re-orientate the patient, the operator gave post-hypnotic suggestions in order to deal the post-procedural pain and/or further ability in self-hypnosis (Workflow step F).
At the end of the procedure, with the patient still on the operator bed, the same hypnosis operator guides the exit the hypnotic status, returning in contact with the present moment (re-orientation).
The re-orientation step allows the patient to recover a complete contact with the reality in few seconds and this is verified by confirming the spatial and temporal orientation of the patient by the operator. After being, for a while, in the recovery room, the patient than answered questionnaires to collect procedural data. In order to avoid possible bias, the questionnaires reporting feeling about the ablation procedure were administered by a different health care professional. Measured parameters related to hypnotic status were: anxiety score, perceived pain, procedural time perception, type and amount of drugs administered during the procedure. In the entire Group A patients, pain perception, were quantified using Numeric Rating Scale (NRS) score from 0 to 10 [10]. A Anxiety Score Scale from 0 to 10 was also used for perceived anxiety evaluation. For further details, see Supplementary Figs. 1 and 2 in the Appendix, web only. Finally, also the perceived procedural time was asked to the patient and compared to the real one.
Considering that in Group B patients intra-procedural anxiety and pain were suppressed by using sedative drugs or narcosis, we decided not to apply the questionnaires because, by definition, all these patients reached by means of sedation/narcosis this goal.
2.5. Endpoints
Primary endpoint was to evaluate hypnosis as adjunctive technique to perform a painless procedure (NRS ≤ 2) without patient's movements which may affect the electroanatomical reconstruction.
Secondary endpoints were: evaluation of the impact of hypnosis on the intra-procedural anxiety and perceived procedural length, sedative drugs sparing, procedural data, needing for non-invasive ventilatory support (oxygen support using nasal cannula or mask) and fluoroscopy time of the catheter ablation between two different study cohorts.
2.6. Statistical analysis
Continuous variables are expressed as mean and standard deviations or median and interquartile ranges, while categorical variables are reported as absolute values and frequencies. Comparison between hypnotic group and standard control group was made with T-Student test for continuous variables and Chi-Square test for categorical variables.
All statistical analyses were performed with SPSS 21 (SPSS Inc., Chicago, IL, USA) and statistically significant P-values were considered with a threshold <0.05.
The study was performed in accordance with the latest Declaration of Helsinki and patients provided written informed consent to participate in the study.
2.7. Patients characteristics
A total of 140 consecutive patients were prospectively enrolled in 1:1 ratio, 70 cases assigned to the hypnotic group (Group A) and 70 patients allocated at the traditional approach group (Group B). Baseline and clinical characteristics of the study population are shown in Supplementary Table 1. The demographic parameters do not differ between the two groups, with an average age of 58.1 for group A and 60.2 for group B, while women represent <1/3 of both groups. Cardiovascular risk factors and comorbidity are equally distributed between the two study groups, in particular, all analyzed patients have a low rate of diabetes and dyslipidemia. In each group, no patients referred a previous non-fatal stroke or TIA; and only 1 patient, in the group A, suffered from HF. Paroxysmal AF is the main catheter ablation indication in both groups (64% in group A and 72% in group B).
There were not differences regarding the management of anticoagulant therapy and anti-arrhythmic drugs between two groups (For further details see Supplementary Table 1). Echocardiographic data are shown in Supplementary Table 1. The mean LA volume resulted of 79.9 ml in the group A and 81.1 ml in the group B, without a statistically significant difference. At the TEE, the LAA dimensional and functional features did not differ between the two groups, in particular the LAA maximum velocity was high in both study population. The left ejection fractions in the two studies population were similar, estimated respectively 60.6 and 59.8.
3. Results
PVI was obtained in 100% of all patients.
No periprocedural complication occurred in both groups.
Hypnosis induction was successful in 97% of cases (68 out of 70 Group A patients).
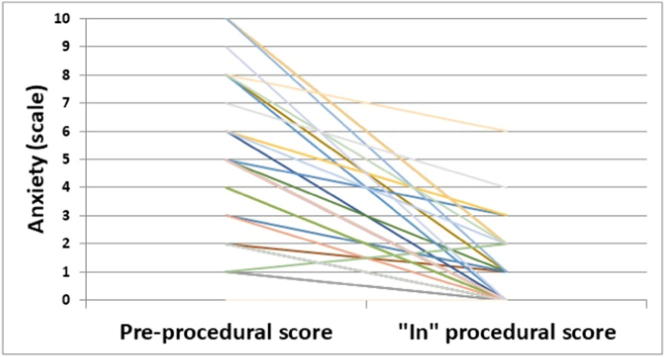
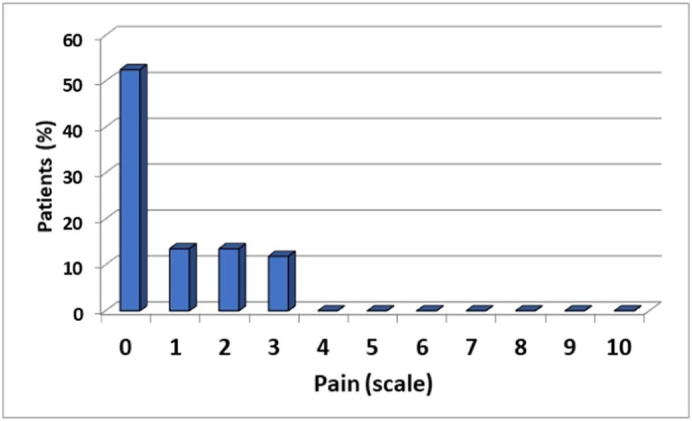
Group A patients reached the primary outcome of painless procedure in 77.9% of cases (53 out of 68 pts) while all the patients remained still on the bed for the whole procedure. Moreover, there was a significant reduction in anxiety (Pre-procedural 4.7 ± 2.9 vs Intra-procedural 0.8 ± 1.2; P < 0.001) and perceived procedural time compared to real one (Real length 108.7 ± 33.3 min Vs Perceived Length 77.1 ± 39.3 min, P < 0.001). The mean time to reach hypnotic status was 4.2 ± 1.2 min. For more details see Table 1 and Fig. 1, Fig. 2 and Supplementary Fig. 3.
Table 1.
Outcomes of the hypnotic communication.
| Hypnotic communication 70 patients (Group A) | |
|---|---|
| Successful hypnotic induction (%) | 68 (97%) |
| Painless procedure (NRS score ≤ 2) (%) | 53 (77.9%) |
| Mean pain scale during procedure (NRS score) ± SD | 1.3 ± 1.6 |
| Median pain scale during procedure (NRS score) ± minimum-maximum | 1 (0–2) |
| Mean pre-procedural anxiety score (ASS) ± SD | 4.7 ± 2.9 |
| Mean Intra-procedural anxiety score (ASS) ± SD | 0.8 ± 1.2 |
| Median pre-procedural anxiety score (ASS) ± minimum-maximum | 5 (2–7) |
| Median Intra-procedural anxiety score (ASS) ± minimum-maximum | 0 (0–1) |
| Mean perceived procedural time (minutes) ± SD | 77.1 ± 39.3 |
NRS: Numeric Rating Scale; SD: Standard Deviation; ASS: Anxiety Score Scale.
Fig. 1.
Procedural Pain perception in Group A patients according to the numeric pain scale.
Fig. 2.
Anxiety reduction in Group A patients following hypnotic communication.
There were no differences in terms of effective procedural time, radiofrequency time and radiation dose, between the two groups. In Group B two patients underwent orotracheal intubation because of difficulties in pain control and 56% of sedated patients required oxygen support during the procedure. In Group A no patient needed invasive or non-invasive ventilatory support or anesthesiologic invasive assistance with major sedative (midazolam or propofol). As regards analgesic drugs, the same dose of Fentanyl (0.142 mg vs 0.146 mg; P 0.650) was used in both cohorts, whereas a higher dose of paracetamol (853 mg vs 337 mg; P < 0.001) was required in group A (for more details see Table 2).
Table 2.
Procedural characteristics.
| Hypnotic group (n = 70) | Conventional group (n = 70) | P value | |
|---|---|---|---|
| First ablation procedure (%) | 70 (100) | 70 (100) | 1.000 |
| PFO (%) | 13 (18) | 18 (26) | 0.416 |
| PVI (%) | 70 (100) | 70 (100) | 1.000 |
| Mean total RF time ± SD (minutes) | 28.9 ± 14.12 | 27.6 ± 12.18 | 0.623 |
| Mean power ± SD (W) | 35.3 ± 1.42 | 35.5 ± 1.53 | 0.424 |
| Mean fluoroscopy time ± SD (sec) | 273.1 ± 214.81 | 331.6 ± 419.11 | 0.383 |
| Mean radiaton dose ±SD (Gray) | 6.7 ± 9.27 | 12.3 ± 21.45 | 0.114 |
| ECV (%) | 14 (20) | 27 (38) | 0.025 |
| Mean effective procedural time ± SD (minutes) | 108.7 ± 33.27 | 109.9 ± 27.95 | 0.999 |
| Non-invasive ventilatory support (%) | 0 (0) | 39 (56) | < 0.001 |
| OTI (%) | 0 (0) | 2 (1) | 0.5 |
| Navigation system | |||
| CARTO3 (%) | 63 (90) | 70 (100) | 0.013 |
| Nav-X (%) | 7 (10) | 0 (0) | |
| Mean Paracetamol ±SD (mg) | 853 ± 342 | 337 ± 425 | < 0.001 |
| Mean Fentanyl ±SD (mg) | 0.142 ± 0.49 | 0.146 ± 0.55 | 0.650 |
| Mean Midazolam ±SD (mg) | 0 ± 0 | 1.8 ± 1.9 | < 0.001 |
| Mean Propofol ±SD (mg) | 0 ± 0 | 43.8 ± 57.2 | < 0.001 |
CT-AFL: common typical atrial flutter; A-AFL: atypical atrial flutter; PFO: patent foramen ovale; PVI: Pulmonary Vein Isolation; CTI-A: Cavotricuspid isthmus ablation; RF: radiofrequency; OTI: orotracheal intubation; ECV: electrical cardioversion.
4. Discussions
To the best of our knowledge this is the largest observational study aiming to evaluate the role of the hypnotic communication as periprocedural analgesia in patients undergoing AF catheter ablation.
The main findings are:
-
1)
In patients in Group A, hypnosis as adjunctive technique/strategy to standard pain protocol reduced intra-procedural and pain perception without increasing the actual procedural time.
-
2)
The use of hypnosis reduced intra-procedural anxiety and perceived procedural length.
-
3)
Hypnosis compared with conventional analog-sedation protocol allowed to reduce the use of sedative drugs without the need of ventilatory support during ablation.
No differences in safety, success rate, total radiofrequency and fluoroscopy time were observed between the two groups. As far as concerned the procedural endpoint, PVI was reached in the 100% of the cases without the occurrence of adverse events either in Group A and B patients. However, in Group B patients a higher rate of oxygen support was necessary and endo-tracheal intubation was needed in two cases.
In the study the patients who underwent ablation with hypnotic communication showed an advantage in terms of intra-procedural anxiety reduction and a good tolerance of the procedure (pain-less ablation in 77.9% of patients). This result confirms what has been described in a recent paper regarding ophthalmological surgery. In fact patients who experienced perceptible pain during previous interventions benefited the most from hypnosis [11]. This advantage can be very useful for a better compliance in patients undergoing AF ablation because in about 30% of the cases the patients undergo redo procedures [12].
Furthermore, considering that AF ablation is offered to a growing number of old patients who may have comorbidities that may contraindicate the use of specific drugs or deep sedation, hypnosis may represent an appealing alternative. Moreover, these patients could also benefit on patient satisfaction and possible reduction of hospitalization time. The last one has been demonstrated in a series of patients undergoing cardiac surgery where the use of hypnosis in the pre and post-operative period was able to reduce hospitalization time [[13], [14], [15]].
In addition, hypnotic mediated analgesia is not related to opioid system, unlike other non-pharmacological techniques (acupuncture), indicating a possible synergistic effect [16]. In fact it has been demonstrated by Casiglia [17] that hypnotic analgesia is based on the “Gate Control” phenomenon. Because our study aimed to assess the potential role and results of the hypnosis technique as adjunctive strategy during paroxysmal/persistent AF catheter ablation, local anesthesia and Fentanyl were administered as a standard protocol to achieve the above-mentioned synergistic effect.
It should be noted that the patient under hypnotic state experienced also a reduction of the perceived procedural length. This effect together with the intra-procedural anxiety and pain relief made the procedure more tolerable despite the lower dosage of administered analgesic medications.
These effects may result in a possible reduction of the procedural costs considering the fewer amounts of analgesic drugs and the un-necessary anaesthesiological support.
In our study, we did not use the hypnotic induction profile test to select the patient, in fact in two patients we failed to induce the hypnotic status. This failure may be attributed to the particular personality of the patients having a self-structured hyper-controlled behavior making difficult the relaxation. There are many tests that can be used to evaluated subject's hypnotisability: Spiegel's Hypnotic Induction Profile [18], Stanford Scale of Hypnotic Susceptibility [19] and Harvard Group Scale of Hypnotic Susceptibility [20], but the first one is the only available test suitable for clinical use. Therefore, a key factor to further improve the hypnosis effect, may be the good patient selection, identifying the most sensitive psychological profile. Moreover, it should be taken into account that the level of suggestibility would have a biphasic pattern, higher in childhood and in the elderly.
Interestingly, the implementation of hypnotic communication in the workflow of the procedure, did not affect the procedural time and the required time to reach the hypnotic status was short (about 4 min). It can be speculated that the absence of statistical difference in the total procedural time in the two groups may be due to the fact that the time spent for hypnotic communication may be balanced by the better management of pain control during the procedure.
In the recent times AF ablation has been performed with the use of electroanatomical mapping systems to reduce the fluoroscopy time and to better evaluate anatomic details. The electroanatomical mapping requires the immobility of the patient as an absolute need to maintain the stability of the body reference and the map reliability. It should be noted that patient stability was reached in both Groups. However, the Group B patients needed a higher amount of sedative drugs and in two cases narcosis was necessary to achieve this goal.
Finally, it should be noted that in our experience all the EP lab personnel was trained in hypnotic communication over a period of around 4 months. The acquisition of hypnotic skills made possible that the hypnotic communication was routinely applied by different professional figures in our daily practice. Therefore, we can assume that this workflow could be reproduced and shared in other Laboratories.
5. Limitations
The present paper shares some limitations. First of all, this is a single-center not randomized controlled trial. Considering that patients' allocation was not randomized, the results may be affected by this bias. Secondly, the procedural outcomes (anxiety, pain perception, perceived procedural length) represent subjective values. Thirdly, questionnaires to assess the outcome were offered only to Group A patients because Group B patients it was assumed that Group B patients were sedated with drugs, obtaining a painless procedure. A further limitation, may be the use of Fentanyl, which may also has an anxiolytic effect. Lastly being an observational study, these results can only be interpreted as descriptive and hypothesis-generating for subsequent scientific studies (clinical trials or meta-analyses).
6. Conclusions
Hypnotic communication as an adjunctive analgesic strategy during AF catheter ablation resulted in a painless procedure in three quarters of the patients with reduction of intra-procedural anxiety and perceived duration of the procedure. Comparing hypnosis group versus conventional analgo-sedation group, the use of sedative drugs was significantly reduced. Moreover, the procedural safety, success rate and total radiofrequency time were not affected by hypnotic communication.
Funding
The authors declare that there is no funding.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Acknowledgement
Special thanks to Caterina Franco, Anna Morittu, Gabriella Amerio, Giuseppe Liccardi, Gerardo Di Filippo, Marinella Sicurella, Mariangela Musso, Silvia Ferraris.
Footnotes
All the authors have no grant support to disclose.
All the authors have no conflict of interest nor funding to disclose.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2019.100405.
Appendix A. Supplementary data
Supplementary material
References
- 1.Chugh S.S., Havmoeller R., Narayanan K., Singh D., Rienstra M., Benjamin E.J., Gillum R.F., Kim Y.H., McAnulty J.H., Jr., Zheng Z.J., Forouzanfar M.H., Naghavi M., Mensah G.A., Ezzati M., Murray C.J. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 2014;129:837–847. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016 07; 37 (38): 2893–962. [DOI] [PubMed]
- 3.Elkins G.R., Barabasz A.F., Council J.R., Spiegel D. Advancing research and practice: the revised APA division 30 definition of hypnosis. Int. J. Clin. Exp. Hypn. 2015;63:1–9. doi: 10.1080/00207144.2014.961870. [DOI] [PubMed] [Google Scholar]
- 4.Adachi T., Fujino H., Nakae A., Mashimo T., Sasaki J. A meta-analysis of hypnosis for chronic pain problems: a comparison between hypnosis, standard care, and other psychological interventions. Int. J. Clin. Exp. Hypn. 2014;62(1):1–28. doi: 10.1080/00207144.2013.841471. [DOI] [PubMed] [Google Scholar]
- 5.Wobst A.H.K. Hypnosis and surgery: past, present, and future. Anesth. Analg. 2007;104(5):1199–1208. doi: 10.1213/01.ane.0000260616.49050.6d. May. [DOI] [PubMed] [Google Scholar]
- 6.Baglini R., Sesana M., Capuano C., Gnecchi-Ruscone T., Ugo L., Danzi G.B. Effect of hypnotic sedation during percutaneous transluminal coronary angioplasty on myocardial ischemia and cardiac sympathetic drive. Am. J. Cardiol. 2004;93(8):1035–1038. doi: 10.1016/j.amjcard.2003.12.058. Apr 15. [DOI] [PubMed] [Google Scholar]
- 7.Amedro P., Gavotto A., Gelibert D., Fraysse V., De La Villeon G., Vandenberghe D. Feasibility of clinical hypnosis for transesophageal echocardiography in children and adolescents. Eur. J. Cardiovasc. Nurs. 2018 Sep 19;1474515118803513 doi: 10.1177/1474515118803513. [DOI] [PubMed] [Google Scholar]
- 8.Barbero U., Ferraris F., Muro M., Budano C., Anselmino M., Gaita F. Hypnosis as an effective and inexpensive option to control pain in transcatheter ablation of cardiac arrhythmias. J. Cardiovasc. Med. (Hagerstown) 2018;19(1):18–21. doi: 10.2459/JCM.0000000000000605. Jan. [DOI] [PubMed] [Google Scholar]
- 9.Ebert T.J. Sympathetic and hemodynamic effects of moderate and deep sedation with propofol in humans. Anesthesiology. 2005;103(1):20–24. doi: 10.1097/00000542-200507000-00007. Jul. [DOI] [PubMed] [Google Scholar]
- 10.Ware L.J., Epps C.D., Herr K., Packard A. Evaluation of the revised faces pain scale, verbal descriptor scale, numeric rating scale, and Iowa pain thermometer in older minority adults. Pain Manag Nurs. 2006;7:117–125. doi: 10.1016/j.pmn.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Chen X., Yuan R., Chen X., Sun M., Lin S., Ye J. Hypnosis intervention for the management of pain perception during cataract surgery. J. Pain Res. 2018;11:1921–1926. doi: 10.2147/JPR.S174490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cappato R., Calkins H., Chen S.A., Davies W., Iesaka Y., Kalman J., Kim Y.H., Klein G., Natale A., Packer D., Skanes A., Ambrogi F., Biganzoli E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ. Arrhythm. Electrophysiol. 2010;3(1):32–38. doi: 10.1161/CIRCEP.109.859116. Feb. [DOI] [PubMed] [Google Scholar]
- 13.Ashton R.C., Jr., Whitworth G.C., Seldomridge J.A. The effects of selfhypnosis on quality of life following coronary artery bypass surgery: preliminary results of a prospective, randomized trial. J. Altern. Complement. Med. 1995;1:285–290. doi: 10.1089/acm.1995.1.285. [DOI] [PubMed] [Google Scholar]
- 14.Akgul A., Guner B., C¸ ırak M., C¸ elik D., Hergünsel O., Bedirhan S. The beneficial effect of hypnosis in elective cardiac surgery: a preliminary study. Thorac. Cardiovasc. Surg. 2016;64:581–588. doi: 10.1055/s-0036-1580623. [DOI] [PubMed] [Google Scholar]
- 15.Münkler P., Attanasio P., Parwani A.S., Huemer M., Boldt L.H., Haverkamp W., Wutzler A. High patient satisfaction with deep sedation for catheter ablation of cardiac arrhythmia. Pacing Clin. Electrophysiol. 2017;40(5):585–590. doi: 10.1111/pace.13063. May. [DOI] [PubMed] [Google Scholar]
- 16.Facco E. Hypnosis and anesthesia: back to the future. Minerva Anestesiol. 2016;82(12):1343–1356. [PubMed] [Google Scholar]
- 17.Casiglia E., Tikhonoff V., Giordano N., Andreatta E., Regaldo G., Tosello M.T. Measured outcomes with hypnosis as an experimental tool in a cardiovascular physiology laboratory. Int. J. Clin. Exp. Hypn. 2012;60(2):241–261. doi: 10.1080/00207144.2012.648078. [DOI] [PubMed] [Google Scholar]
- 18.Spiegel H., Aronson M., Fleiss J.L., Haber J. Psychometric analysis of the hypnotic induction profile. Int. J. Clin. Exp. Hypn. 1976;24:300–315. doi: 10.1080/00207147608416210. [DOI] [PubMed] [Google Scholar]
- 19.Weitzenhoffer A.M., Hilgard E.R. Consulting Psychologists Press; Palo Alto, CA: 1965. Stanford Hypnotic Susceptibility Scale, Form C. [Google Scholar]
- 20.Shor R., Orne E.C. Consulting Psychologists; Palo Alto, CA: 1962. Harvard Group Scale of Hypnotic Susceptibility, Form A. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material