Abstract
Background:
Osteochondral lesions of the talus are frequent pathologies of the ankle joint. Especially through arthroscopy, the treatment is kept as minimally invasive as possible. However, there are some drawbacks as to the reachability because of the high congruency of the ankle joint. Here, either noninvasive distraction or maximal dorsiflexion may be an option for better access to the lesion. The purpose of this study was to evaluate maximal dorsiflexion compared to neutral position or noninvasive distraction of the ankle joint in the arthroscopic reachability of the talar dome. The hypothesis of this study was that maximal dorsiflexion would allow for greater accessibility of the talar dome compared to neutral position or noninvasive distraction of the joint.
Methods:
Twenty matched pairs (n=40) of anatomical ankle specimens were used. The effects of neutral position, maximal dorsiflexion, and noninvasive distraction of the ankle joint on arthroscopic accessibility of the ankle joint were tested. After disarticulation of the talus, reach was measured and compared between the 3 positions.
Results:
In neutral position, 13.7±1.2 mm of the talar dome was reached laterally and 14.0±1.0 mm medially. In maximal dorsiflexion, the distance was 19.0±1.1mm laterally and 19.8±1.4 mm medially, and in noninvasive distraction it was 16.1±1.5 mm laterally and 15.7±1.0 mm medially. The statistical comparison showed a significantly better reach in dorsiflexion laterally (P = .003) and medially (P = .026).
Conclusion:
Accessibility of the talar dome in maximal dorsiflexion was superior to that in neutral position or noninvasive distraction.
Clinical Relevance:
Results of this study may allow for better planning in arthroscopic treatment of osteochondral lesions of the talus.
Keywords: osteochondral defect, OCD, ankle arthroscopy, talus, talar dome, dorsiflexion, noninvasive distraction
Introduction
With an incidence of 27 per 100 000, osteochondral lesions (OCD) of the talus are frequent pathologies of the ankle joint. They occur in 61% to 70% of rotational ankle sprains, leading to the conclusion that trauma is most often the reason for those OCDs.23,36,51,56 Most frequently, their location is described as the middle third of the medial or lateral talar dome, but also the anterior or posterior third may be affected.5,8,28,56,62 As talar OCDs have a strong influence on the quality of life of patients,5 successful treatment is important. Meanwhile, ankle arthroscopy has been defined as the gold standard for visualization, and treatment of talar OCDs is performed most frequently with debridement of the lesion and bone marrow stimulation by microfracture.13,16,36,48,54,62
In arthroscopy, joint space visibility and accessibility of structures play a major role in the success of the operative procedure. Because arthroscopy of the ankle joint can be challenging because of the high congruency of the talar dome and the distal tibial articular surface,47,49,50,52,54 the surgeon has to be aware of the limitations of the planned procedure. To minimize anatomical hindrances during ankle arthroscopy, several work-arounds have been described, namely, different portal placement,15,27,33,42,46 invasive or noninvasive distraction,6,29,44,55,58 and maximal joint flexion or extension.24,47
Ankle arthroscopy is performed primarily via anterior portals, though in cases in which the anterior approach is not sufficient, lesions may be addressed through posterior portals.10,15,31,41,53 However, these posterior portals are associated with complications,4,33,61 because important anatomical structures, that is, the posterior tibial vessels and the tibial nerve, are in proximity to the medial portal.1,22,26,27,33,41,42,46 Additionally, there seems to be no clear consensus on when to approach defects through an anterior or through a posterior approach.15,16,35,50 Apart from joint distraction to maximize space in the joint cavity, moving the talar dome from underneath the tibial plafond is a recently emphasized method to improve accessibility of the cartilage in talar OCD. This has already been shown for anterior arthroscopy in combination with maximal plantarflexion24,54 and suggested for posterior arthroscopy in combination with maximal dorsiflexion.26 The purpose of this study was to show the advantage of maximal dorsiflexion of the ankle joint with respect to the accessibility of the talar dome compared to neutral position or noninvasive distraction of the ankle joint. The hypothesis of this study was that maximal dorsiflexion would allow for greater accessibility of the talar dome compared to neutral position or noninvasive distraction of the joint.
Methods
Twenty matched pairs (n=40) of fresh-frozen anatomic ankle specimens were used for this study. The specimens originated from voluntary body donations to the Department of Anatomy. Approval from the institutional ethical review board of the Medical University of Vienna was obtained (No. 2266/2017).
Available specimens were included in this study if they were of sufficient soft tissue quality, free of evidence of previous surgery or trauma as well as signs of vascular or neural problems in the ankle region and showed minimal to no osteoarthritis of the joint. The specimens were stored at −20°C and thawed at 4°C for 48 hours.
The specimens were divided randomly into 2 groups (group 1: neutral position and maximal dorsiflexion; group 2: noninvasive distraction). This grouping was important to minimize measuring bias due to slackening of stabilizing structures during the joint manipulations. Prior to the arthroscopic procedure, passive range of motion was evaluated and documented. Manual tests (anterior drawer stress and lateral tilt) were performed to investigate the ligamentous status of each specimen.
Arthroscopic Procedure
The specimens were mounted in a customized vice for arthroscopic procedures, which was similar to devices used in recent literature.9,24,59 The serrated jaws of the vice prevented unintended movement of the specimens during manipulation and distraction. Posterior arthroscopy of the ankle was performed through a modification of the standard posteromedial (instrumentation) and posterolateral (arthroscope) portals53 using a 4-mm 30-degree scope. The posterolateral portal was located 5 mm proximal to the tip of the lateral malleolus and just lateral to the calcaneal tendon. The posteromedial portal was located just medial to the calcaneal tendon at the same level of the posterolateral portal. Placement of the portals was standardized throughout all specimens. All arthroscopic procedures were performed by the same experienced orthopedic surgeon who completed a foot and ankle fellowship.
Accessibility of the talar dome was tested using a standard concave pick with a 90-degree tip. Neutral position and maximal dorsiflexion were performed by an operative assistant, and distraction was performed using a noninvasive arthroscopic Ankle Distraction Strap (Arthrex, Naples, FL). The average force applied was approximately 115 N as documented by van Dijk et al55 (Figure 1). As a first step, a diagnostic inspection for pathology (ligamentous integrity, absence of severe osteoarthritic changes) of the ankle joint was performed. Only after confirmation of the absence of any intra-articular exclusion criteria, accessibility of the talar dome was determined in each group by using the chondral pick. The most anterior position in neutral position, dorsiflexion, and noninvasive distraction was marked.
Figure 1.

Intraoperative setting during posterior ankle arthroscopy, the specimen simulating a patient’s prone position during surgery using (A) maximal dorsiflexion performed by an operative assistant and (B) noninvasive distraction with an Ankle Distraction Strap.
Specimens
The paired specimens (n=40) originated from 24 male and 16 female donors. Their age distribution showed a mean of 79.7 ± 10.5 years (60-98 years). They were distributed equally among the 2 groups. Ligamentous stability was ascertained in all specimens. Anterior drawer stress and lateral tilt were negative in each joint. Passive range of motion was 7.6±7.2 (0-20) dorsiflexion and 37.1±8.5 (15-50) plantarflexion. During the diagnostic arthroscopy, no pathologies were detected in 9 specimens. In the remaining specimens some degenerative changes were present; however, they did not influence the intended procedure: synovitis (n=21), slight degenerative changes (n=2), small dorsal osteophyte (n=3), os trigonum (n=4).
Evaluation
Dissection of the ankle joint was performed after completion of the arthroscopic procedure. First, the posterior capsule of the joint was opened and the position of the posterior rim of the tibia in neutral position was marked with a lateral- and a medial-positioned guide wire. Afterwards, the talus was extracted.
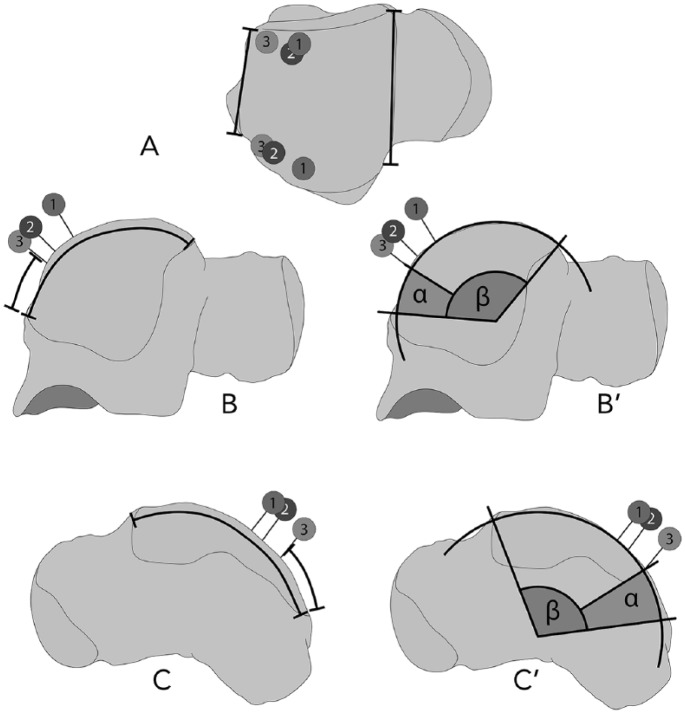
The following parameters were measured similar to the evaluation of Hirtler and Schuh24 (Figure 2):
Figure 2.
Measurements performed on the talus with exemplary markers of all ankle positions (example showing a right talus, 1: maximal dorsiflexion; 2: noninvasive distraction; 3: neutral position). (A) Anterior and posterior talar width, (B) medial circumference of the talar dome and distance to the marker of neutral position, and (B′) the respective α-angle (α) and β-angle (β), (C) lateral circumference of the talar dome and distance to the marker of neutral position and (C′) the respective α-angle (α) and β-angle (β).
Morphology of the talar dome: anterior width, posterior width, lateral circumference, and medial circumference
Distal tibial morphology: width and length of the distal tibial articular surface
Position of the posterior tibial rim: lateral and medial distance from the posterior rim of the talar dome to the posterior tibial rim in neutral position
Position of the inserted markers: distance from the posterior rim, distance from the lateral and the medial border of the talar dome
All measurements were documented for each specimen and standardized photographs from the superior, medial, and lateral positions were taken.
In the lateral and medial photos, measurements similar to those described by Magerkurth et al30 and van Bergen et al50 were performed. These measurements have the advantage to be applicable to preoperative planning of the operative procedure:
A circle was fitted to the contour of the talar dome, its center providing an imaginary center of rotation of the ankle joint. The α-angle was defined as the angle subtended by the arc between the posterior extent of the talar articular surface and the respective marker (maximal reach in neutral position, dorsiflexion, or noninvasive distraction). The β-angle was defined as the angle subtended by the arc between the anterior extent of the talus articular surface and the posterior extent of the talar articular surface. The accessible area (%) of the talar dome was calculated by dividing α (indicating the posterior area) by β (indicating the complete talar dome) (Figure 2).
Statistics
The statistical analysis was performed with IBM SPSS Statistics 24.0 for Mac OS. Mean, standard deviation, and range were calculated for every metric variable. Using the Kolmogorov-Smirnov test and visual evaluation by Gaussian distribution curve over the histogram of the respective data, normal distribution was tested. Through a nonsignificant Levene test, homogeneity of variances was ensured. By Pearson correlation coefficient, the correlations for metric data were tested. In data without normal distribution, the Spearman rank correlation coefficient was used instead. A Student t test was used for normally distributed metric variables. In data without normal distribution, the Mann-Whitney U test was used instead. For categorical variables, the chi-square test was used. In comparison between the 3 groups, an analysis of variances (ANOVA) was performed with a post hoc test (Tukey if variance homogeneity was proven, Games-Howell if not). A P value <.05 was considered as statistically significant, and it was corrected by Bonferroni correction in multiple testing.
Results
Descriptive results of the measurements can be found in Tables 1 (direct measurements) and 2 (image evaluation in accordance with Magerkurth et al30 and van Bergen et al50). Comparing the results showed significant differences between the 3 groups on the medial and on the lateral talar dome looking at the distance from the posterior border of the talar dome to the anteriormost chondral pick (medial P = .026, lateral P = .003), at the α-angle (medial P = .027, lateral P = .001), and at the accessible area (medial P = .022, lateral P = .001) (Figures 3 and 4). On the medial side, the difference was limited to a significantly better result of both maximal dorsiflexion and noninvasive distraction (1) compared to neutral position for the distance to the marker (P = .020), the α-angle (P = .020), and the accessibility (P = .016). On the lateral side, the difference was significant comparing maximal dorsiflexion to neutral position as well as to noninvasive distraction for the distance to the marker (P = .002 and .046), the α-angle (P = .001 and .007), and the accessibility (P = .001 and .007) (Fig. 3 and 4). Dorsal range of motion as well as age showed no correlation with the accessibility of the talar dome (P > .05).
Table 1.
Evaluation of all Directly Measured Variables.
| Dorsiflexion | Neutral Position | Distraction | |
|---|---|---|---|
| Talar dome | |||
| Anterior width (mm) | 31.0±0.7 (26.0-35.0) | 31.6±0.8 (22.2-37.8) | |
| Posterior width (mm) | 28.5±1.0 (24.1-39.7) | 28.1±0.6 (23.9-34.1) | |
| Lateral circumference (mm) | 40.3±1.4 (32.0-48.0) | 38.9±1.3 (32.0-53.0) | |
| Medial circumference (mm) | 38.2±1.8 (28.0-50.0) | 36.3±1.3 (28.0-50.0) | |
| Inferior tibial articular surface | |||
| Width (mm) | 36.4±1.0 (28.6-42.1) | 35.4±1.0 (27.4-42.9) | |
| AP length (mm) | 31.8±0.9 (25.2-37.7) | 31.5±0.9 (25.0-39.3) | |
| Distance from posterior border of talar dome to anterior tibial rim in neutral position | |||
| Lateral (mm) | 6.5±1.0 (0.0-12.0) | 6.9±0.7 (0.0-12.2) | |
| Medial (mm) | 8.0±1.2 (0.0-20.0) | 9.0±0.8 (0.0-16.0) | |
| Distance from posterior border of talar dome to marked indentation by chondral pick | |||
| Lateral (mm) a | 19.0±1.1 (11.0-26.0) | 13.7±1.2 (5.0-30.0) | 16.1±1.5 (4.1-30.3) |
| Medial (mm) b | 19.8±1.4 (9.0-28.0) | 14.0±1.0 (6.4-26.0) | 15.7±1.0 (6.3-24.0) |
Abbreviation: AP, anteroposterior.
Significant difference between maximal dorsiflexion and neutral position (P = .002) as well as maximal dorsiflexion and noninvasive distraction (P = .046).
Significant difference between maximal dorsiflexion and noninvasive distraction compared to neutral position (P = .020).
Table 2.
| Dorsiflexion | Neutral Position | Distraction | |
|---|---|---|---|
| α-angle lateral (degrees)a | 56.7±3.8 (37.3-93.8) | 37.3±3.2 (8.3-72.5) | 40.8±3.2 (20.2-68.2) |
| β-angle lateral (degrees) | 133.5±3.5 (111.6-156.3) | 132.6±3.2 (106.6-167.7) | |
| Accessible area lateral (%)b | 42.6±2.6 (24.9-64.7) | 28.4±2.4 (6.6-51.6) | 30.9±2.3 (14.4-48.2) |
| α-angle medial (degrees)c | 53.3±3.4 (33.8-76.1) | 39.6±3.0 (17.0-72.5) | 45.5±3.7 (13.3-81.3) |
| β-angle medial (degrees) | 129.0±3.2 (110.2-150.2) | 132.8±3.1 (104.0-162.7) | |
| Accessible area medial (%)d | 41.2±2.1 (27.8-57.5) | 30.4±2.3 (13.6-55.0) | 34.9±3.1 (8.2-60.4) |
| Tibial coverage of the talus lateral (%) | 85.3±3.6 (63.0-108.7) | 88.5±3.4 (54.7-116.7) | |
| Tibial coverage of the talus medial (%) | 80.1±3.0 (53.6-102.1) | 82.7±3.4 (51.2-110.0) | |
Significant difference between maximal dorsiflexion and neutral position (P = .001) as well as maximal dorsiflexion and noninvasive distraction (P = .007).
Significant difference between maximal dorsiflexion and neutral position (P = .001) as well as maximal dorsiflexion and noninvasive distraction (P = .007).
Significant difference between maximal dorsiflexion and noninvasive distraction compared to neutral position (P = .020).
Significant difference between maximal dorsiflexion and noninvasive distraction compared to neutral position (P = .16).
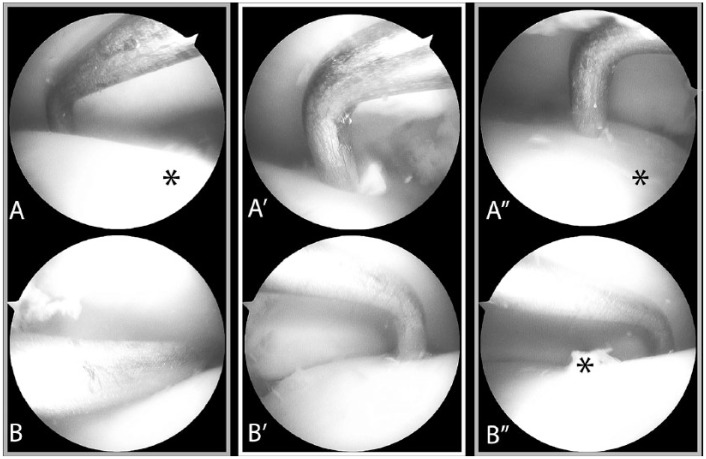
Figure 3.
Arthroscopic comparison between (A resp. B) dorsiflexion, (A′ resp. B′) neutral position and (A″ resp. B″) noninvasive distraction in a left ankle joint. Starting with the ankle in (*) neutral position, the pick was positioned at the tibial rim and the ankle joint either dorsiflexed or distracted. The difference in accessibility between (A) lateral and (B) medial talar dome was compared.
Figure 4.
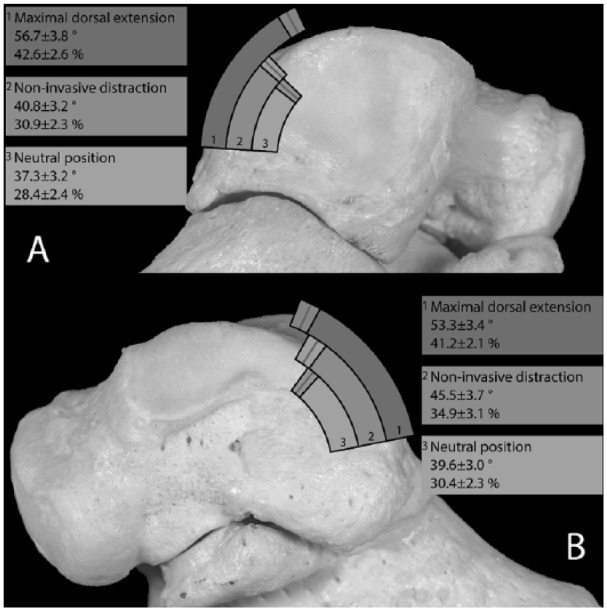
Comparison of the reachable area in (1) dorsiflexion, (2) noninvasive distraction, and (3) neutral position on the (A) medial and (B) lateral talar dome (example in a right talus).
Summarizing, maximal dorsiflexion (42.6%±2.6%) allowed a significantly larger accessible area compared to noninvasive distraction (30.9%±2.3%) on the lateral talar dome, whereas on the medial side there was no significant difference between maximal dorsiflexion (41.2%±2.1%) and noninvasive distraction (34.9%±3.1%). The accessibility of the talar dome in neutral position was always significantly less (lateral 28.4±2.4, medial 30.4±2.3) compared to maximal dorsiflexion (see Table 2).
Discussion
Our results show that noninvasive distraction in posterior ankle arthroscopy was not necessary to improve accessibility of the talar dome. Placing the ankle in maximal dorsiflexion was sufficient to reach approximately 40% of the talar cartilage for treatment of OCD through standard posteromedial (arthroscope) and posterolateral (instrumentation) portals in anatomical specimens. Specific literature concerning talar OCD addressed solely through posterior arthroscopic portals is scarce. Information may be found on the extent of the talar dome being visualized by a posterior approach, ranging between 52% and 54% (see Table 3).22,41 Recently, studies began to investigate the accessibility of the talar cartilage with the objective of reliable preoperative planning for talar OCD. Mainly, these studies evaluated operative reach through standard anterior portals (anteromedial and anterolateral) in ankle arthroscopy and compared different means of improving the procedure through maximal plantarflexion,24,47,49,50 moving the talar dome from under the distal tibial articular surface, and distraction of the joint,2,24 either wire-based, that is, invasive, or noninvasive. Here, van Bergen and van Dijk et al47,49,50 were able to show the advantage of preoperative planning of the procedure by performing computed tomography (CT) of the ankle joint in maximal plantarflexion in combination with a possible reach of 47.8%±5.6% laterally and 48.2%±6.7% medially in this joint position. Hirtler and Schuh24 reported access to 45%±11% of the lateral and to 49%±8% of the medial talar dome performing maximal plantarflexion and 37%±13% of the lateral and 44%±10% of the medial talar dome using noninvasive distraction.
Table 3.
Summary of Reported Results.
| Dorsiflexion | Neutral Position | Distraction | |
|---|---|---|---|
| Barg et al2 | Invasive: 56.4%±20.0% Noninvasive: 39.8%±14.9% |
||
| Phisitkul et al35 | Noninvasive: | ||
| 49.3% | 50.3% | 39.76%-48.54%a | |
| This study | Noninvasive: | ||
| Lateral: 42.6%±2.6% | Lateral: 28.4%±2.4% | Lateral: 30.9%±2.3% | |
| Medial: 41.2%±2.1% | Medial: 30.4%±2.3% | Medial: 34.9%±3.1% |
Different distraction levels evaluated. Specified accessibility is reached in 3- to 5-mm distraction.
The study of Magerkurth et al30 started the discussion of different ankle positions for better accessibility, as the amount of uncovered cartilage of the talar dome is around 15.8%30 and can rise to around 48% to 68% in maximal plantarflexion24,35,50 and to around 42% (in this study) to 49% in maximal dorsiflexion.35 The morphometric evaluation of the talus was similar to Magerkurth et al,30 comparing the width of the distal tibial articular surface (34±3.6mm) and the amount of talar coverage (88±6.7 degrees). However, one has to keep in mind that those measurements were performed in radiographs, leading to a slight variability in direct measurements of a specimen.
Recently, Barg and Phisitkul et al2,35 addressed the accessibility of the talar dome from both anterior and posterior approaches in noninvasive table-based distraction and invasive distraction as well as in different positions of the ankle joint. Barg et al2 were able to show an anterior accessibility of the talar cartilage with invasive distraction of 61.5%±15.2% and with noninvasive distraction of 57.8%±17.2%. Their posterior accessibility with invasive distraction was 56.4%±20.0% and with noninvasive distraction 39.8%±14.9%. Their noninvasive distraction technique was—contrary to the technique performed in this study—table based, and their invasive distraction involved a tensioned wire drilled transversely through the calcaneal tuberosity combined with longitudinal distraction. The results of the present study (30.9%±2.3% lateral and 34.9%±3.1% medial) using solely noninvasive distraction, posterior arthroscopy, focusing primarily at the access to the medial and lateral shoulders of the talar dome, are at least partially comparable to the results by Barg et al.2 Their reported posterior access to the talar dome is significantly larger than in the present study. This may be caused by the higher age of the donors in this study as our mean age was 79.7±10.5 years (60-98 years). Although no significant correlation between age and accessibility was shown in this study, this reflects a relative homogenous sample. Compared to the younger age of donors used by Barg et al2 (54.0 ±9.5 years, 38-63 years), this significant difference may nonetheless play a major role in interpreting the presented results.20 However, the number of specimens in the present study is more than twice as many, which would help minimize statistical bias, and additionally the results of these 2 studies may be difficult to compare because in their study, apart from one sagittal length of the talus and the total talar area, no information was given concerning the shape of the talar dome, its anterior or posterior width, or the coverage by the distal tibial articular surface.
Phisitkul et al35 reported the overall access to the talar dome through anterior portals in neutral position (44.8%), 30 degrees plantarflexion (63.0%), maximal plantarflexion (67.5%), and through posterior portals in neutral position (50.3%) and maximal dorsiflexion (49.3%). Overall, they showed a significantly lower overall accessibility in posterior arthroscopy (49.8%) than in anterior arthroscopy (58.5%). In the present study, access was shown in neutral position to be 28.4%±2.4% (6.6%-51.6%) laterally and 30.4%±2.3% (13.6%-55.0%) medially, and in maximal dorsiflexion 42.6%±2.6% (24.9%-64.7%) laterally and 41.2%±2.1% (27.8%-57.5%) medially, results again being significantly smaller in comparison. Additionally, Phisitkul et al35 showed an increase of accessibility of the talar dome using noninvasive distraction for both the anterior and the posterior approach. Here however, one has to take 2 points into consideration when comparing to the results presented in this paper: (1) Using a distraction strap, the ankle joint automatically moves into plantarflexion, rotating the talar dome away from view in posterior arthroscopy. (2) Distraction was performed after the evaluation of plantarflexion and dorsiflexion first in anterior arthroscopy and second in posterior arthroscopy. Looking at the mean amount of distraction during anterior (3.1±1.4mm) and posterior arthroscopy (5.4±0.8mm) the question arises,whether this noninvasive distraction may have influenced the soft tissues by the slackening during the procedures.
While the tensioning effect of maximal plantarflexion on the anterior joint capsule similar to distraction has been discussed,6 and a possible shift of portals placed in neutral position has been mentioned,35 this study was able to show the positive effect of maximal dorsiflexion of the ankle in maximizing the reach to the talar dome. Although noninvasive distraction may improve accessibility in posterior arthroscopy2,35 and even wire-based invasive distraction may have its place in specific cases,2,32,57,58,63 one should nonetheless take all possible means to minimize complication rate, which has been shown to be higher in procedures using invasive or noninvasive distraction.3,7,11,12,14,17,18,21,25,29,39,43,45,52,54,55,58
Though most talar OCDs may be addressed though anterior arthroscopy, there can arise situations in which the location of the specific OCD may warrant a posterior approach. As the majority of OCDs treated by arthroscopic approaches commonly do not exceed 1 cm2,19,38,60 the authors feel certain that the results shown in this study are clinically significant as the information presented may affect preoperative planning and the arthroscopic treatment of some talar lesions. Through a posterior approach, at least 40% of the posterior talar dome may be reached as shown in this study and by others.2,22,41 Here, age and range of motion do not play such a large role in assessing accessibility. This is contrary to the anterior approach, where the anatomical morphology of the talar dome leads to a larger accessible area, especially on the lateral side. Particularly in younger patients with a better range of motion, the accessibility using anterior portals may be sufficient to also reach defects located more posterior, as the reported mean accessibility ranges from 45% to 60%.24,35,50
Maximal dorsiflexion showed the best accessibility compared to neutral position of the ankle, in which most of the talar dome is covered by the distal tibial articular facet, and also to noninvasive distraction, especially as the distraction strap automatically leads to plantarflexion of the joint which additionally moves parts of the talar dome away from the view of the surgeon. Using noninvasive distraction in ankle arthroscopy therefore did not improve accessibility to the talar dome but could also be associated with a higher risk of neurovascular complications.7,17,18,21,29,45,55
Limitations
Some disadvantages in the use of anatomical specimens have to be mentioned, which may have an effect on the interpretation of the results of this study. The age of the donors is in general higher than the average age of OCD patients, and their joints may have been altered by degeneration. Therefore, strict exclusion criteria were defined to minimize this component and only joints with minimal damage were included. Additionally, studies have shown that specimen population age influences the amount of motion possible in a joint.20,40 A correlation of age and range of motion however was not shown in this study due to the homogenous age-distribution in the sample. The lack of physiological muscle tone and the decreasing tension of stabilizing ligaments and surrounding soft tissue, the type of specimens in addition to the freezing and thawing of the specimens may have led to higher results in talar dome accessibility than possible in vivo.34,37 Finally, as posterior portals in ankle arthroscopy are anatomically challenging per se and all procedures in this study were performed by a highly specialized orthopedic surgeon, the results may not be reproducible in the generalized orthopedic community.
Conclusion
Accessibility of the talar dome in maximal dorsiflexion was superior to neutral position or noninvasive distraction in cadaveric specimens with posterior ankle arthroscopy. Based on the results of this study, preoperative planning may be improved in patients with lesions of the talus.
Supplemental Material
Supplemental material, FAI847134-ICMJE for Accessibility to Talar Dome in Neutral Position, Dorsiflexion, or Noninvasive Distraction in Posterior Ankle Arthroscopy by Lena Hirtler, Katarina Schellander and Reinhard Schuh in Foot & Ankle International
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Lena Hirtler, MA, MD, PhD,  https://orcid.org/0000-0001-5194-9118
https://orcid.org/0000-0001-5194-9118
References
- 1. Balci HI, Polat G, Dikmen G, Atalar A, Kapicioglu M, Asik M. Safety of posterior ankle arthroscopy portals in different ankle positions: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2119-2123. [DOI] [PubMed] [Google Scholar]
- 2. Barg A, Saltzman CL, Beals TC, Bachus KN, Blankenhorn BD, Nickisch F. Arthroscopic talar dome access using a standard versus wire-based traction method for ankle joint distraction. Arthroscopy. 2016;32(7):1367-1374. [DOI] [PubMed] [Google Scholar]
- 3. Bonnin M, Bouysset M. Arthroscopy of the ankle: analysis of results and indications on a series of 75 cases. Foot Ankle Int. 1999;20(11):744-751. [DOI] [PubMed] [Google Scholar]
- 4. Carlson MJ, Ferkel RD. Complications in ankle and foot arthroscopy. Sports Med Arthrosc Rev. 2013;21(2):135-139. [DOI] [PubMed] [Google Scholar]
- 5. D’Ambrosi R, Maccario C, Serra N, Ursino C, Usuelli FG. Relationship between symptomatic osteochondral lesions of the talus and quality of life, body mass index, age, size and anatomic location. Foot Ankle Surg. 2018;24(4):365-372. [DOI] [PubMed] [Google Scholar]
- 6. de Leeuw PA, Golano P, Clavero JA, van Dijk CN. Anterior ankle arthroscopy, distraction or dorsiflexion? Knee Surg Sports Traumatol Arthrosc. 2010;18(5):594-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dowdy PA, Watson BV, Amendola A, Brown JD. Noninvasive ankle distraction: relationship between force, magnitude of distraction, and nerve conduction abnormalities. Arthroscopy. 1996;12(1):64-69. [DOI] [PubMed] [Google Scholar]
- 8. Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28(2):154-161. [DOI] [PubMed] [Google Scholar]
- 9. Feller R, Borenstein T, Fantry AJ, et al. Arthroscopic quantification of syndesmotic instability in a cadaveric model. Arthroscopy. 2017;33(2):436-444. [DOI] [PubMed] [Google Scholar]
- 10. Ferkel RD, Fischer SP. Progress in ankle arthroscopy. Clin Orthop Relat Res. 1989;240:210-220. [PubMed] [Google Scholar]
- 11. Ferkel RD, Heath DD, Guhl JF. Neurological complications of ankle arthroscopy. Arthroscopy. 1996;12(2):200-208. [DOI] [PubMed] [Google Scholar]
- 12. Ferkel RD, Small HN, Gittins JE. Complications in foot and ankle arthroscopy. Clin Orthop Relat Res. 2001;391:89-104. [DOI] [PubMed] [Google Scholar]
- 13. Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750-1762. [DOI] [PubMed] [Google Scholar]
- 14. Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint: does sinus tarsi syndrome exist? Foot Ankle Int. 1999;20(3):185-191. [DOI] [PubMed] [Google Scholar]
- 15. Gasparetto F, Collo G, Pisanu G, et al. Posterior ankle and subtalar arthroscopy: indications, technique, and results. Curr Rev Musculoskelet Med. 2012;5(2):164-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478-1490. [DOI] [PubMed] [Google Scholar]
- 17. Golano P, Vega J, Perez-Carro L, Gotzens V. Ankle anatomy for the arthroscopist. Part I: the portals. Foot Ankle Clin. 2006;11(2):253-273, v. [DOI] [PubMed] [Google Scholar]
- 18. Golano P, Vega J, Perez-Carro L, Gotzens V. Ankle anatomy for the arthroscopist. Part II: role of the ankle ligaments in soft tissue impingement. Foot Ankle Clin. 2006;11(2):275-296, v-vi. [DOI] [PubMed] [Google Scholar]
- 19. Grambart ST. Arthroscopic management of osteochondral lesions of the talus. Clin Podiatr Med Surg. 2016;33(4):521-530. [DOI] [PubMed] [Google Scholar]
- 20. Grimston SK, Nigg BM, Hanley DA, Engsberg JR. Differences in ankle joint complex range of motion as a function of age. Foot Ankle. 1993;14(4):215-222. [DOI] [PubMed] [Google Scholar]
- 21. Guhl JF. New concepts (distraction) in ankle arthroscopy. Arthroscopy. 1988;4(3):160-167. [DOI] [PubMed] [Google Scholar]
- 22. Heck J, Mendicino RW, Stasko P, Shadrick D, Catanzariti AR. An anatomic safe zone for posterior ankle arthroscopy: a cadaver study. J Foot Ankle Surg. 2012;51(6):753-756. [DOI] [PubMed] [Google Scholar]
- 23. Hintermann B, Regazzoni P, Lampert C, Stutz G, Gachter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. 2000;82(3):345-351. [DOI] [PubMed] [Google Scholar]
- 24. Hirtler L, Schuh R. Accessibility of the talar dome-anatomic comparison of plantarflexion versus noninvasive distraction in arthroscopy. Arthroscopy. 2018;34(2):573-580. [DOI] [PubMed] [Google Scholar]
- 25. Jerosch J, Schneider T, Strauss JM, Schurmann N. Arthroscopy of the upper ankle joint. List of indications from the literature—realistic expectations–complications [in German]. Unfallchirurg. 1993;96(2):82-87. [PubMed] [Google Scholar]
- 26. Kim HN, Kim GL, Park JY, Woo KJ, Park YW. Fixation of a posteromedial osteochondral lesion of the talus using a three-portal posterior arthroscopic technique. J Foot Ankle Surg. 2013;52(3):402-405. [DOI] [PubMed] [Google Scholar]
- 27. Lee KB, Saltzman CL, Suh JS, Wasserman L, Amendola A. A posterior 3-portal arthroscopic approach for isolated subtalar arthrodesis. Arthroscopy. 2008;24(11):1306-1310. [DOI] [PubMed] [Google Scholar]
- 28. Lee RKL, Griffith JF, Law EKC, Ng AWH, Yeung DKW. Ankle traction during MRI of talar dome osteochondral lesions. AJR Am J Roentgenol. 2017;209(4):874-882. [DOI] [PubMed] [Google Scholar]
- 29. Lozano-Calderon SA, Samocha Y, McWilliam J. Comparative performance of ankle arthroscopy with and without traction. Foot Ankle Int. 2012;33(9):740-745. [DOI] [PubMed] [Google Scholar]
- 30. Magerkurth O, Knupp M, Ledermann H, Hintermann B. Evaluation of hindfoot dimensions: a radiological study. Foot Ankle Int. 2006;27(8):612-616. [DOI] [PubMed] [Google Scholar]
- 31. Muir D, Saltzman CL, Tochigi Y, Amendola N. Talar dome access for osteochondral lesions. Am J Sports Med. 2006;34(9):1457-1463. [DOI] [PubMed] [Google Scholar]
- 32. Nakasa T, Adachi N, Kato T, Ochi M. Distraction arthroplasty with arthroscopic microfracture in a patient with rheumatoid arthritis of the ankle joint. J Foot Ankle Surg. 2015;54(2):280-284. [DOI] [PubMed] [Google Scholar]
- 33. Nickisch F, Barg A, Saltzman CL, et al. Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg Am. 2012;94(5):439-446. [DOI] [PubMed] [Google Scholar]
- 34. Orishimo KF, Burstein G, Mullaney MJ, et al. Effect of knee flexion angle on Achilles tendon force and ankle joint plantarflexion moment during passive dorsiflexion. J Foot Ankle Surg. 2008;47(1):34-39. [DOI] [PubMed] [Google Scholar]
- 35. Phisitkul P, Akoh CC, Rungprai C, et al. Optimizing arthroscopy for osteochondral lesions of the talus: the effect of ankle positions and distraction during anterior and posterior arthroscopy in a cadaveric model. Arthroscopy. 2017;33(12):2238-2245. [DOI] [PubMed] [Google Scholar]
- 36. Polat G, Ersen A, Erdil ME, Kizilkurt T, Kilicoglu O, Asik M. Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1299-1303. [DOI] [PubMed] [Google Scholar]
- 37. Ralis ZA. Freezing of orthopaedic specimens before mechanical testing. J Bone Joint Surg Br. 1989;71(1):55-57. [DOI] [PubMed] [Google Scholar]
- 38. Ramponi L, Yasui Y, Murawski CD, et al. Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med. 2017;45(7):1698-1705. [DOI] [PubMed] [Google Scholar]
- 39. Salvi AE. Has plantarflexion any positive impact on the clinical risk of vascular injury during ankle arthroscopy? J Foot Ankle Surg. 2007;46(6):515-516; author reply 516. [DOI] [PubMed] [Google Scholar]
- 40. Schwarz NA, Kovaleski JE, Heitman RJ, Gurchiek LR, Gubler-Hanna C. Arthrometric measurement of ankle-complex motion: normative values. J Athl Train. 2011;46(2):126-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sitler DF, Amendola A, Bailey CS, Thain LM, Spouge A. Posterior ankle arthroscopy: an anatomic study. J Bone Joint Surg Am. 2002;84(5):763-769. [PubMed] [Google Scholar]
- 42. Smyth NA, Zwiers R, Wiegerinck JI, et al. Posterior hindfoot arthroscopy: a review. Am J Sports Med. 2014;42(1):225-234. [DOI] [PubMed] [Google Scholar]
- 43. Sun YQ, Slesarenko YA. Joint distraction may be unnecessary in ankle arthroscopy. Orthopedics. 2006;29(2):118-120. [DOI] [PubMed] [Google Scholar]
- 44. Takao M, Ochi M, Shu N, et al. Bandage distraction technique for ankle arthroscopy. Foot Ankle Int. 1999;20(6):389-391. [DOI] [PubMed] [Google Scholar]
- 45. Unangst A, Martin KD. Simple 1-step ankle arthroscopy distraction. Arthrosc Tech. 2015;4(6):e873-e876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Urguden M, Cevikol C, Dabak TK, Karaali K, Aydin AT, Apaydin A. Effect of joint motion on safety of portals in posterior ankle arthroscopy. Arthroscopy. 2009;25(12):1442-1446. [DOI] [PubMed] [Google Scholar]
- 47. van Bergen CJ, Gerards RM, Opdam KT, Terra MP, Kerkhoffs GM. Diagnosing, planning and evaluating osteochondral ankle defects with imaging modalities. World J Orthop. 2015;6(11):944-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 2013;95(6):519-525. [DOI] [PubMed] [Google Scholar]
- 49. van Bergen CJ, Tuijthof GJ, Blankevoort L, Maas M, Kerkhoffs GM, van Dijk CN. Computed tomography of the ankle in full plantar flexion: a reliable method for preoperative planning of arthroscopic access to osteochondral defects of the talus. Arthroscopy. 2012;28(7):985-992. [DOI] [PubMed] [Google Scholar]
- 50. van Bergen CJ, Tuijthof GJ, Maas M, Sierevelt IN, van Dijk CN. Arthroscopic accessibility of the talus quantified by computed tomography simulation. Am J Sports Med. 2012;40(10):2318-2324. [DOI] [PubMed] [Google Scholar]
- 51. van Dijk CN, Reilingh ML, Zengerink M, van Bergen CJ. Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc. 2010;18(5):570-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. van Dijk CN, Scholte D. Arthroscopy of the ankle joint. Arthroscopy. 1997;13(1):90-96. [DOI] [PubMed] [Google Scholar]
- 53. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16(8):871-876. [DOI] [PubMed] [Google Scholar]
- 54. van Dijk CN, van Bergen CJ. Advancements in ankle arthroscopy. J Am Acad Orthop Surg. 2008;16(11):635-646. [DOI] [PubMed] [Google Scholar]
- 55. van Dijk CN, Verhagen RA, Tol HJ. Technical note: resterilizable noninvasive ankle distraction device. Arthroscopy. 2001;17(3):E12. [DOI] [PubMed] [Google Scholar]
- 56. Verhagen RA, Struijs PA, Bossuyt PM, van Dijk CN. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003;8(2):233-242, viii-ix. [DOI] [PubMed] [Google Scholar]
- 57. Vopat BG, Lareau CR, Sangal RB, Fantry AJ, Blankenhorn BD. Use of a pneumatic limb positioner for invasive skeletal traction in posterior hindfoot arthroscopy. Arthrosc Tech. 2015;4(5):e417-e422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Waseem M, Barrie JL. A new distraction method in difficult ankle arthroscopy. J Foot Ankle Surg. 2002;41(6):412-413. [DOI] [PubMed] [Google Scholar]
- 59. Watson BC, Lucas DE, Simpson GA, Berlet GC, Hyer CF. Arthroscopic evaluation of syndesmotic instability in a cadaveric model. Foot Ankle Int. 2015;36(11):1362-1368. [DOI] [PubMed] [Google Scholar]
- 60. Yoshimura I, Kanazawa K, Hagio T, Minokawa S, Asano K, Naito M. The relationship between the lesion-to-ankle articular length ratio and clinical outcomes after bone marrow stimulation for small osteochondral lesions of the talus. J Orthop Sci. 2015;20(3):507-512. [DOI] [PubMed] [Google Scholar]
- 61. Young BH, Flanigan RM, DiGiovanni BF. Complications of ankle arthroscopy utilizing a contemporary noninvasive distraction technique. J Bone Joint Surg Am. 2011;93(10):963-968. [DOI] [PubMed] [Google Scholar]
- 62. Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):238-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Zhang K, Jiang Y, Du J, et al. Comparison of distraction arthroplasty alone versus combined with arthroscopic microfracture in treatment of post-traumatic ankle arthritis. J Orthop Surg Res. 2017;12(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, FAI847134-ICMJE for Accessibility to Talar Dome in Neutral Position, Dorsiflexion, or Noninvasive Distraction in Posterior Ankle Arthroscopy by Lena Hirtler, Katarina Schellander and Reinhard Schuh in Foot & Ankle International