Abstract
Background:
Operative time is a risk factor for short-term complications after orthopaedic procedures; however, it has yet to be investigated as an independent risk factor for postoperative complications after arthroscopic rotator cuff repair.
Purpose:
To determine whether operative time is an independent risk factor for complications, readmissions, and extended hospital stays within 30 days after arthroscopic rotator cuff repair.
Study Design:
Descriptive epidemiology study.
Methods:
The American College of Surgeons National Surgical Quality Improvement Program was queried for all hospital-based inpatient and outpatient arthroscopic rotator cuff repairs (Current Procedural Terminology code 29827) from 2005 to 2016. Concomitant procedures such as subacromial decompression, biceps tenodesis, superior labrum anterior and posterior (SLAP) repair, labral repair, and distal clavicle excision were also included, whereas patients undergoing arthroplasty were excluded from the study. Operative time was correlated with patient demographics, comorbidities, and concomitant procedures. All adverse events were correlated with operative time, while controlling for the above preoperative variables, using multivariate Poisson regression with a robust error variance.
Results:
A total of 27,524 procedures met inclusion and exclusion criteria. The mean age of patients was 58.4 ± 10.9 years, the mean operative time was 86.9 ± 37.4 minutes, and the mean body mass index was 30.4 ± 7.0 kg/m2. Concomitant biceps tenodesis, glenohumeral debridement, SLAP repair, labral repair, and distal clavicle excision significantly increased operative time (P < .001) but not the risk of adverse events (P > .05). The overall rate of adverse events was 0.88%. After adjusting for demographic and procedural characteristics, a 15-minute increase in operative duration was associated with an increased risk of anemia requiring transfusion (relative risk [RR], 1.27 [95% CI, 1.14-1.42]; P < .001), venous thromboembolism (RR, 1.17 [95% CI, 1.02-1.35]; P = .029), surgical site infection (RR, 1.13 [95% CI, 1.03-1.24]; P = .011), and extended length of hospital stay (RR, 1.07 [95% CI, 1.00-1.14]; P = .036).
Conclusion:
Although the rate of short-term complications after arthroscopic rotator cuff repair is low, incremental increases in operative time are associated with an increased risk of adverse events such as surgical site infection, pulmonary embolism, transfusion, and extended length of hospital stay. Efforts should be made to maximize surgical efficiency in the operating room through optimal coordination of the staff or increased preoperative planning.
Keywords: arthroscopic rotator cuff repair, operative time, complications, surgical site infection, venous thromboembolism
Rotator cuff tears are common musculoskeletal abnormalities that affect nearly 25% of patients in their sixties.43 Although the majority of rotator cuff tears are treated nonoperatively, arthroscopic rotator cuff repair has shown a 600% increase in utilization from 1996 to 2006.22,25 Future changes to bundled payment models after rotator cuff repair may result in physicians in the United States being awarded less reimbursement in cases where patients are readmitted within 90 days of initial discharge.27 Therefore, it is imperative to identify risk factors that may contribute to short-term adverse events postoperatively.10,16,24
Increased operative time has previously been shown to increase the risk of complications after orthopaedic and nonorthopaedic procedures.7,8,12,15,32,33,40 However, the relationship between operative time and the rate of complications is poorly understood, as operative time may be a confounding variable of more complicated procedures. Previous investigations established that extended operative time in arthroscopic rotator cuff repair was associated with an increased risk of complications.7,15,19,32 However, these investigations treated operative time as a binary variable (>45/<45 or >90/<90 minutes) to ascertain the relationship between operative time and postoperative complications. While a relationship between operative time and adverse events was identified, quantifying the impact of surgical duration on adverse events has not been identified in arthroscopic rotator cuff repair. A linear relationship between operative time and the risk of adverse events after total joint arthroplasty, anterior cruciate ligament reconstruction, anterior cervical diskectomy, and ankle open reduction internal fixation has previously been established.1,8,17,31 Therefore, identifying incremental increases in operative time as an independent risk factor for complications after arthroscopic rotator cuff repair would emphasize the need for operative efficiency and the significance for surgical planning in this patient population.
The purpose of this investigation was to determine whether operative time is an independent risk factor for short-term (30-day) complications, readmissions, and extended hospital stays after arthroscopic rotator cuff repair. We hypothesized that there is a positive linear correlation between operative time and the risk of developing complications, such as venous thromboembolic events or surgical site infections, within 30 days after arthroscopic rotator cuff repair.
Methods
This investigation analyzed the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. This registry contains demographics, comorbidities, laboratory values, and concomitant procedures with corresponding readmission and complication rates within 30 days of the indexed procedure. Patients are identified through Current Procedural Terminology (CPT) and International Classification of Diseases–Ninth Revision and –Tenth Revision (ICD-9 and ICD-10, respectively) codes.23 This database is composed of a network of hospitals that employ clinical reviewers with a background in health care to collect over 270 variables from surgical procedures. The ACS-NSQIP database has several quality assurance programs in place to ensure the accuracy and quality of collected data.14,39 Patients treated in inpatient and outpatient hospital facilities were included in this study; those treated at ambulatory surgical centers were not included.
The ACS-NSQIP database was queried for all arthroscopic rotator cuff repairs (CPT 29827) between 2005 and 2016. Secondary CPT codes for subacromial decompression (29826, 29826-51, 29826-59), glenohumeral debridement (29822, 29823), biceps tenodesis (29828, 23430), superior labrum anterior and posterior (SLAP) repair (29807), and labral repair (29806) were included in the investigation. Patients undergoing total shoulder arthroplasty (CPT 23472) or hemiarthroplasty (CPT 23470) were excluded from this analysis. Superior capsular reconstruction is commonly coded with CPT codes for arthroscopic rotator cuff repair. Thus, patients with CPT codes for allograft tissue in their record (n < 10) at the time of surgery were excluded from this investigation, as they likely represented cases of superior capsular reconstruction. It was not detectable whether the procedure was primary or revision repair.
Patient demographics, including age, smoking status, comorbidities, sex, and American Society of Anesthesiologists (ASA) physical status classification, were collected. An ASA score greater than 3 corresponded to severe systemic disease (new classification of physical status). A history of diabetes was reported as either insulin dependent, oral medication only, or no diabetes. Procedures were excluded if any of the following variables were missing: ASA class, sex, body mass index, operative time, and type of anesthetic. Cases were excluded if operative time was longer than 225 minutes (>3 SDs from the mean).
Complications were reported within 30 days of the indexed procedure, as the ACS-NSQIP database only tracks patients and records adverse events within this time period. These complications included anemia requiring transfusion, cardiac arrest requiring cardiopulmonary resuscitation, death, cerebrovascular accident, wound dehiscence, venous thromboembolism (deep vein thrombosis and pulmonary embolism), pneumonia, myocardial infarction, renal insufficiency, surgical site infection, sepsis, urinary tract infection, unplanned intubation, hospital readmission, and extended length of stay in the hospital (≥2 days).1,8 Extended length of stay was defined as such to exclude patients who were kept on a 23-hour observation period from being considered as a complication. Operative time was collected as a continuous variable and was defined as the duration, in minutes, from skin incision to wound closure. During analysis, operative time was segmented into 15-minute intervals to determine marginal increases in the complication risk after a 15-minute interval in operative duration.
Statistical Analysis
Stata 13.1 (StataCorp) was used to perform statistical analysis in this investigation. Demographic and comorbidity variables were correlated with operative duration by bivariate linear regression. Multivariate Poisson regression with a robust error variance was subsequently performed to determine which of these variables were correlated with operative time. A robust error variance prevents the overestimation of errors with Poisson regression. Poisson regression with a robust error variance was implemented into the analysis, as it has been previously shown to be efficacious in epidemiological investigations to calculate the relative risk (RR).46 Bivariate analysis was then performed on operative duration and the risk of developing short-term complications. Multivariate Poisson regression with a robust error variance was again utilized to determine the RR of developing each complication while accounting for correlated demographic variables. Fifteen-minute increments were used in this investigation to allow for clinical interpretation of the impact of marginal increases in operative time on postoperative complications. All statistical comparisons were considered significant at P < .05.
Results
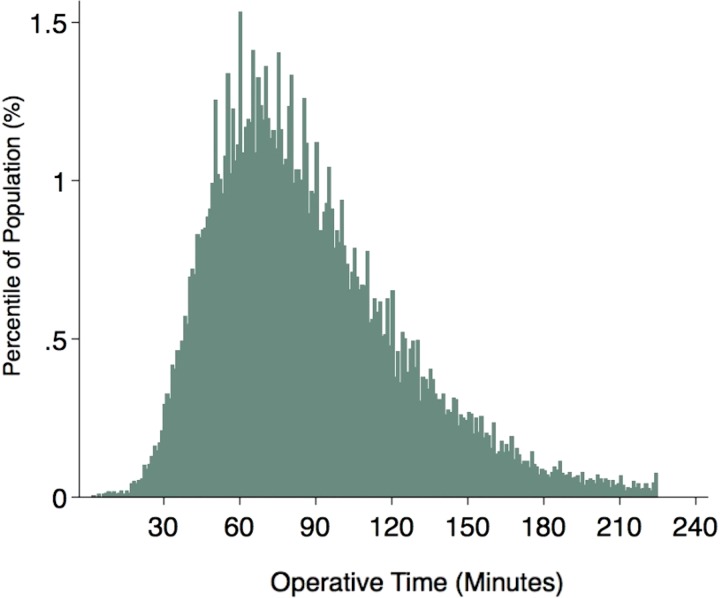
After exclusions, there were 27,524 rotator cuff repairs from 2005 to 2016 included in the analysis (Table 1). The mean age of the patients was 58.4 ± 10.9 years, and the mean body mass index was 30.4 ± 7.0 kg/m2. The mean operative time was 86.9 ± 37.4 minutes (Figure 1). Operative times based on patient demographics and comorbidities are provided in Tables 1 and 2, respectively. Concomitant glenohumeral debridement, arthroscopic biceps tenodesis, open biceps tenodesis, SLAP repair, labral repair, or distal clavicle excision resulted in increased operative times in comparison with those rotator cuff repairs without concomitant procedures (P < .001). However, concomitant subacromial decompression and synovectomy decreased the overall operative time (P < .001 and P = .012, respectively) when compared with cases that lacked these procedures. It should be noted that open biceps tenodesis resulted in the largest increase in operative time (111.9 ± 39.0 minutes; RR, 28.3; P < .001).
TABLE 1.
Operative Time by Demographic and Procedural Characteristicsa
| n | Operative Time, Mean ± SD, min |
Bivariate | Multivariateb | |||
|---|---|---|---|---|---|---|
| P Value | Coefficient | 95% CI | P Value | |||
| Overall | 27,524 | 86.9 ± 37.4 | ||||
| Age, y | .017 | .983 | ||||
| 18-40 | 1291 | 88.6 ± 40.6 | –0.1 | –2.3 to 2.1 | ||
| 41-60 | 13,214 | 87.4 ± 38.0 | 0.0 | –1.0 to 0.9 | ||
| 61-80 | 12,518 | 86.3 ± 36.4 | Reference | — | ||
| >80 | 501 | 85.1 ± 37.9 | 0.6 | –2.6 to 3.9 | ||
| Sex | <.001 | <.001 | ||||
| Female | 11,603 | 81.8 ± 35.6 | Reference | — | ||
| Male | 15,921 | 90.6 ± 38.3 | 7.3 | 6.4 to 8.2 | ||
| Body mass index, kg/m2 | <.001 | .074 | ||||
| <25 | 4872 | 84.8 ± 36.9 | –1.1 | –2.7 to 0.6 | ||
| 25-30 | 9921 | 87.1 ± 37.0 | –1.1 | –2.5 to 0.4 | ||
| 31-35 | 7243 | 88.3 ± 38.4 | 0.3 | –1.2 to 1.8 | ||
| 36-40 | 3332 | 87.1 ± 37.7 | Reference | — | ||
| >40 | 2156 | 85.7 ± 36.5 | 0.5 | –1.5 to 2.4 | ||
| ASA class | .059 | .284 | ||||
| 1 | 2674 | 87.7 ± 37.7 | 0.4 | –1.4 to 2.3 | ||
| 2 | 16,148 | 87.1 ± 37.6 | 0.4 | –0.6 to 1.5 | ||
| 3 | 8448 | 86.4 ± 36.9 | Reference | — | ||
| 4 | 254 | 82.0 ± 36.9 | –3.9 | –8.5 to 0.6 | ||
| Anesthesia | <.001 | <.001 | ||||
| Regional only | 2051 | 78.4 ± 34.9 | Reference | — | ||
| General | 25,473 | 87.6 ± 37.5 | 8.3 | 6.7 to 9.9 | ||
| Concomitant procedurec | ||||||
| Subacromial decompression | 17,674 | 85.5 ± 36.4 | <.001 | –5.6 | –6.5 to –4.7 | <.001 |
| Debridement | 6203 | 88.0 ± 37.7 | .008 | 2.3 | 1.2 to 3.3 | <.001 |
| Arthroscopic biceps tenodesis | 3543 | 99.5 ± 38.4 | <.001 | 16.2 | 14.9 to 17.5 | <.001 |
| Open biceps tenodesis | 1796 | 111.9 ± 39.0 | <.001 | 28.3 | 26.5 to 30.0 | <.001 |
| SLAP repair | 1204 | 94.0 ± 39.4 | <.001 | 6.2 | 4.1 to 8.3 | <.001 |
| Labral repair | 268 | 106.9 ± 42.9 | <.001 | 18.1 | 13.8 to 22.5 | <.001 |
| Distal clavicle excision | 5745 | 87.9 ± 36.6 | .021 | 2.5 | 1.4 to 3.6 | <.001 |
| Synovectomy | 796 | 82.5 ± 35.5 | <.001 | –3.3 | –5.8 to –0.7 | .012 |
aBold values are statistically significant (P < .05). ASA, American Society of Anesthesiologists; SLAP, superior labrum anterior and posterior.
bAdjusted for all baseline demographic and procedural characteristics listed in this table.
cConcomitant procedures were referenced to those rotator cuff repairs without each procedure (ie, subacromial decompression vs no subacromial decompression). Patients may have gone underwent more than 1 concomitant procedure at the time of index procedure.
Figure 1.
Distribution and incidence of operative duration of arthroscopic rotator cuff repair.
TABLE 2.
Operative Time by Comorbidity
| n | Operative Time, Mean ± SD, min | Bivariate | Multivariatea | |||
|---|---|---|---|---|---|---|
| P Value | Coefficient | 95% CI | P Value | |||
| Current smoker | .370 | .358 | ||||
| No | 23,299 | 82.7 ± 31.8 | Reference | — | ||
| Yes | 4225 | 82.2 ± 31.7 | –0.6 | –1.8 to 0.6 | ||
| Diabetes mellitus | .494 | .435 | ||||
| None | 23,356 | 86.8 ± 37.3 | –0.7 | –2.1 to 0.7 | ||
| Non–insulin dependent | 2984 | 87.7 ± 38.3 | Reference | — | ||
| Insulin dependent | 1184 | 86.8 ± 37.4 | –0.9 | –3.3 to 1.5 | ||
| Dyspnea | .003 | .178 | ||||
| No | 26,624 | 87.0 ± 37.5 | Reference | — | ||
| Yes | 900 | 83.3 ± 35.0 | –1.7 | –4.2 to 0.8 | ||
| Chronic obstructive pulmonary disease | <.001 | .023 | ||||
| No | 26,693 | 87.0 ± 37.5 | Reference | — | ||
| Yes | 831 | 82.3 ± 35.6 | –3.0 | –5.6 to –0.4 | ||
| Hypertension | .037 | .002 | ||||
| No | 14,876 | 86.5 ± 37.3 | Reference | — | ||
| Yes | 12,648 | 87.4 ± 37.5 | 1.5 | 0.6 to 2.5 | ||
| Functional dependence | .431 | .098 | ||||
| No | 27,385 | 86.9 ± 37.4 | Reference | — | ||
| Yes | 139 | 89.4 ± 42.8 | 5.1 | –0.9 to 11.1 | ||
aAdjusted for all baseline demographic and procedural characteristics listed in this table. Bold values are statistically significant (P < .05).
The overall rate of all adverse events was 0.88% among all arthroscopic rotator cuff repairs. The most common complication was pulmonary embolism, which occurred in 0.19% of procedures. The incidence of readmissions within 30 days and that of an extended length of stay (≥2 days) were 1.07% and 0.53%, respectively. After performing multivariate regression analysis and accounting for confounding demographics, comorbidities, and concomitant procedures, we found a 15-minute increase in operative duration to be associated with an increased risk of anemia requiring transfusion (RR, 1.27 [95% CI, 1.14-1.42]; P < .001), venous thromboembolism (RR, 1.17 [95% CI, 1.02-1.35]; P = .029), surgical site infection (RR, 1.13 [95% CI, 1.03-1.24]; P = .011), and extended length of hospital stay (RR, 1.07 [95% CI, 1.00-1.14]; P = .036) (Table 3).
TABLE 3.
Association of a 15-Minute Increase in Operative Time With the Rate of Each Adverse Event or Hospital Metrica
| Rate, % | Unadjusted (Bivariate) | Adjusted (Multivariate)b | |||||
|---|---|---|---|---|---|---|---|
| RR | 95% CI | P Value | RR | 95% CI | P Value | ||
| Adverse event | 0.88 | 1.06 | 1.01-1.11 | .018 | 1.06 | 1.01-1.11 | .01 |
| Anemia requiring transfusion | 0.02 | 1.29 | 0.98-1.71 | .070 | 1.27 | 1.14-1.42 | <.001 |
| Cerebrovascular accident | 0.03 | 1.13 | 0.89-1.44 | .320 | 1.16 | 0.99-1.36 | .071 |
| Dehiscence | 0.01 | 1.27 | 1.14-1.43 | <.001 | 1.33 | 0.96-1.85 | .086 |
| Myocardial infarction | 0.07 | 1.05 | 0.92-1.20 | .439 | 1.02 | 0.87-1.20 | .817 |
| Pneumonia | 0.13 | 1.00 | 0.89-1.12 | .958 | 1.02 | 0.90-1.15 | .774 |
| Renal insufficiency | 0.01 | 1.17 | 0.88-1.56 | .287 | 1.20 | 0.89-1.62 | .225 |
| Sepsis | 0.05 | 0.99 | 0.80-1.21 | .891 | 1.00 | 0.80-1.24 | .968 |
| Surgical site infection | 0.16 | 1.13 | 1.03-1.24 | .007 | 1.13 | 1.03-1.24 | .011 |
| Venous thromboembolism | 0.28 | 1.24 | 1.06-1.45 | .007 | 1.17 | 1.02-1.35 | .029 |
| Unplanned intubation | 0.07 | 1.02 | 0.83-1.24 | .865 | 1.05 | 0.86-1.29 | .635 |
| Urinary tract infection | 0.18 | 0.97 | 0.87-1.08 | .535 | 1.00 | 0.89-1.12 | .988 |
| Adverse hospital metric | |||||||
| Hospital readmission | 1.07 | 1.03 | 0.98-1.08 | .276 | 1.04 | 0.99-1.09 | .161 |
| Extended length of stay | 0.53 | 1.06 | 1.00-1.13 | .067 | 1.07 | 1.00-1.14 | .036 |
aBold values are statistically significant (P < .05). RR, relative risk.
bAdjusted for all demographic, comorbidity, and procedural characteristics listed in Table 1.
Multivariate analysis of factors associated with an increased incidence of any adverse event demonstrated that operative time (RR, 1.06; P = .010), chronic obstructive pulmonary disease (RR, 2.36; P < .001), ASA classes 3 and 4 (RR, 2.32 [P = .033] and RR, 4.79 [P = .002], respectively), and functional dependence (RR, 3.14; P = .003) were independent risk factors for complications within 30 days of arthroscopic rotator cuff repair (Table 4). Nonsignificant factors that may have been associated with adverse events after arthroscopic rotator cuff repair are provided in the Appendix.
TABLE 4.
Multivariate Analysis of Significant Factors Associated With an Increased Incidence of Any Adverse Event After Arthroscopic Rotator Cuff Repaira
| Variableb | RR | 95% CI | P |
|---|---|---|---|
| Operative time | 1.06 | 1.01-1.11 | .010 |
| Chronic obstructive pulmonary disease | 2.36 | 1.52-3.64 | <.001 |
| ASA class | |||
| 1 | Reference | — | — |
| 2 | 1.76 | 0.84-3.68 | .132 |
| 3 | 2.32 | 1.07-5.02 | .033 |
| 4 | 4.79 | 1.78-12.98 | .002 |
| Functional dependence | 3.14 | 1.46-6.73 | .003 |
aBold values are statistically significant (P < .05). ASA, American Society of Anesthesiologists; RR, relative risk.
bMultivariate analysis adjusted for all baseline demographic and procedural characteristics listed in this table.
Discussion
This investigation established that a 15-minute incremental increase in operative duration is an independent risk factor for postoperative transfusion, pulmonary embolism, surgical site infection, and extended length of stay after arthroscopic rotator cuff repair. Concomitant biceps tenodesis, glenohumeral debridement, SLAP repair, labral repair, and distal clavicle excision significantly increased operative time; however, these concomitant procedures did not increase the risk of short-term adverse events. Physicians should be conscious of reducing potential causes of longer operative time, as this may be a contributing factor to postoperative adverse events.
Operative time has been shown to be an independent risk factor for postoperative complications after shoulder arthroscopic surgery and lower extremity joint arthroplasty.4,5,7,8 Boddapati et al7 demonstrated that operative time greater than 45 minutes was associated with an increased risk of surgical site infection and overnight hospital stays. However, their investigation treated operative time as a binary variable to determine the relationship between operative time and postoperative complications. Although an association between operative time and postoperative complications was identified, the investigation was unable to quantify the impact of increased operative time on short-term adverse events. In the present investigation, operative time was treated as a continuous variable, which allowed for subsequent analysis of the effect of incremental increases in operative time on postoperative complications. In an investigation examining the risk of operative time on complications after total hip arthroplasty and total knee arthroplasty, Bohl et al8 identified that 15-minute increases in operative time resulted in 13% and 9% increases in surgical site infection and wound dehiscence, respectively. Furthermore, concomitant procedures increased operative time but did not increase the risk of complications. Concomitant procedures may not directly cause adverse events; however, the associated increase in operative time may contribute to the risk of complications. The findings in the present investigation demonstrate that 15-minute increases in surgical duration can increase the incidence of adverse events after arthroscopic rotator cuff repair.
The overall rate of surgical site infection after arthroscopic rotator cuff repair was 0.16%, which is lower than what has been previously reported.15,22,32,41,44 The rate of surgical site infection may be lower because of the time period that was queried in this investigation (within 30 days), as previous investigations assessed the rate of infection within 3 to 6 months postoperatively.22,41 Age older than 65 years,15 open repair,15,20,41 and male sex32,41 have previously been identified as risk factors for a postoperative surgical site infection. Additionally, the incidence of venous thromboembolsim in this investigation (0.28%) is higher than what has been previously reported.35 Previous investigations have suggested that a history of cancer, tobacco use, thrombophilia, lateral positioning, and operative time are risk factors for developing venous thromboembolism after shoulder arthroscopic surgery.9,11,18,34 The present study establishes that prolonged operative time results in an increased risk of venous thromboembolism in patients undergoing arthroscopic rotator cuff repair. Blood may pool in the lower extremities because of positioning in the beach-chair or lateral position, despite the use of mechanical prophylaxis.
Currently, there are no guidelines provided by the American Academy of Orthopaedic Surgeons regarding the use of deep vein thrombosis prophylaxis specific to shoulder arthroscopic surgery; however, physicians commonly prescribe aspirin to patients in the perioperative period. Alyea et al2 demonstrated that the use of pneumatic compression devices and early mobilization provides equivalent prophylaxis to aspirin in this low-risk population. Because of the low incidence of deep vein thrombosis and lack of standard prophylactic protocol, physicians may continue to implement venous thromboembolic prophylaxis that best fits the individual needs of each patient.
This investigation further establishes chronic obstructive pulmonary disease, ASA class 3 or 4, and functional dependence as independent risk factors for adverse events. This finding corroborates previous investigations that establish that pulmonary or cardiac comorbidities influence adverse events after shoulder surgery.38,42 Patients with multiple comorbidities or systemic illnesses are at an increased risk of developing adverse events. Despite the low incidence of readmission after elective shoulder arthroscopic surgery, Hill et al19 demonstrated that operative time longer than 1.5 hours, age older than 40 years, ASA classes 3 and 4, chronic obstructive pulmonary disease, and chronic steroid use were independent risk factors for readmission. Patients who are functionally dependent on others may not have the assistance or resources to receive adequate postoperative care. This may predispose these patients to complications and readmissions. This finding highlights the importance of interdisciplinary collaboration with social workers and other members of the health care team to ensure that patients who are functionally dependent have adequate postoperative care. Smoking, diabetes, and obesity were not found to be significant risk factors for 30-day adverse events. This finding may suggest that these comorbidities may be less relevant in minimally invasive procedures or that the complication rate is too low to detect a difference, despite the use of a database.
The United States health care system emphasizes the importance of reducing short-term readmissions after surgery.10,16,24 Arthroscopic procedures are increasingly performed at outpatient surgical centers that may be owned by practicing physicians.21,30 This places larger accountability on physicians for patient outcomes, complications, consequential penalties, or reduced reimbursement.30 The findings of this investigation demonstrate that operative time should be optimized to maximize efficiency and patient safety. To minimize complications, it is imperative that physicians and the surgical team work efficiently to minimize operative duration. Working with the same operative staff has been shown to reduce operative time.28 Understanding patient-specific risk factors for prolonged operative time is imperative for physicians and operating staff to consider during preoperative planning. Physicians with a higher surgical volume, which may be driven by more experience, are a major factor in maximizing operative efficiency, and these physicians may experience a lower complication profile than lower volume physicians. Nonetheless, proper preoperative assessment and planning on behalf of the operative team may improve efficiency in the operating room, thus reducing the number of complications.
The ACS-NSQIP database provides high-quality data on a multitude of surgical variables and is sufficiently powered to address risk factors and trends of infrequent complications. Despite the power of this investigation and the quality of collected data, there are inherent limitations due to the use of a database. The results of this investigation are dependent on accurate coding by physicians and clinical reviewers. Any miscoding or noncoding by providers is a potential source of errors in these data. Although disagreement among clinical reviewers is less than 2%,14,39 differences in the definition of comorbidities and complications may cause variations in the results of this investigation.45 Furthermore, because of the size of the database, it is debatable at which point the P value to detect statistical significance becomes meaningless.45 Therefore, readers should evaluate the significance of the findings in this investigation. In addition, we were unable to discern whether the complications or extended length of stay recorded in this investigation were caused by a pre-existing condition or were a direct result of the procedure.
The external validity of this investigation may be limited, as the ACS-NSQIP database is only reflective of hospital-based patients and does not include patients who are treated at ambulatory surgical centers. This may contribute to selection bias, as hospital patients generally have more comorbidities compared with ambulatory patients. Furthermore, surgeon experience may vary between those who predominantly operate in inpatient facilities versus those who primarily operate in ambulatory surgery centers. Also various preoperative and intraoperative variables, such as patient positioning, antibiotic or deep vein thrombosis prophylaxis, and operative technique, are unknown and may contribute to variations in complication rates. Although operative technique, such as double-row or single-row repair as well as transosseous or transosseous-equivalent techniques, has been shown not to increase operative time,6,36 a variation of these techniques may affect operative time on a national scale. Risk factors for poorer outcomes, such as Goutallier grading, preoperative tendon length, initial tear size, and bone mineral density, were unable to be collected.13,26,29 The involvement of residents or fellows and their contribution to operative time and complications was not assessed in this investigation; however, resident involvement has been shown to not increase operative time or complications in shoulder arthroscopic surgery.3
It was unclear whether patients had undergone primary repair or revision repair. Revision cases may be technically difficult and can prolong operative times. Despite no difference in short-term outcomes, patients undergoing revision rotator cuff repair have a higher incidence of tendon retears, increased pain, impaired overhead function, weaker strength, and lower satisfaction in comparison with patients undergoing primary repair.37 Revision rotator cuff repair may not increase the incidence of short-term complications; however, complications may be higher in these patients because rehabilitation is a slower process. Future investigations may be needed to elucidate a relationship between short-term adverse events and revision rotator cuff repair. Last, the outcomes of this study are limited to complications within the immediate postoperative period, and long-term outcomes such as retears, reoperations, and other procedure-specific outcomes were not captured. The results of this investigation assess complication rates in the acute postoperative period and do not consider the impact of operative time on clinical outcomes or other complications such as stiffness or tendon retears. Future investigations may be beneficial to assess the impact of operative time on clinical outcomes and other complications.
Conclusion
While the rate of short-term complications after arthroscopic rotator cuff repair is low, incremental increases in operative time are associated with an increased risk of adverse events such as surgical site infections, transfusion, pulmonary embolism, and extended hospital stays. Efforts should be made to maximize surgical efficiency in the operating room through optimal coordination of the staff or increased preoperative planning or simulation training in the instance of resident or fellow physicians.
APPENDIX
TABLE A1.
Results of Nonsignificant Factors Associated With Any Adverse Event After Arthroscopic Rotator Cuff Repaira
| Variableb | RR | 95% CI | P Value |
|---|---|---|---|
| Age, y | |||
| 18-40 | Reference | — | — |
| 41-60 | 3.62 | 0.90-14.60 | .070 |
| 61-80 | 3.98 | 0.98-16.15 | .054 |
| >80 | 5.61 | 1.21-26.14 | .028 |
| Sex | |||
| Female | Reference | — | — |
| Male | 1.01 | 0.78-1.31 | .915 |
| Body mass index, kg/m2 | |||
| <25 | Reference | — | — |
| 25-30 | 0.92 | 0.62-1.39 | .706 |
| 31-35 | 1.23 | 0.81-1.84 | .329 |
| 36-40 | 1.14 | 0.71-1.85 | .587 |
| >40 | 0.98 | 0.57-1.69 | .932 |
| Diabetes mellitus | |||
| None | Reference | — | — |
| Non--insulin dependent | 0.96 | 0.66-1.41 | .838 |
| Insulin dependent | 1.27 | 0.80-2.04 | .312 |
| Dyspnea | 1.35 | 0.82-2.21 | .234 |
| Hypertension | 1.32 | 0.99-1.78 | .061 |
| Smoking | 0.93 | 0.65-1.33 | .674 |
| General anesthesia | 1.30 | 0.74-2.27 | .359 |
| Concomitant procedurec | |||
| Subacromial decompression | 0.91 | 0.69-1.20 | .483 |
| Debridement | 0.97 | 0.72-1.31 | .844 |
| Arthroscopic biceps tenodesis | 0.99 | 0.68-1.44 | .954 |
| Open biceps tenodesis | 1.23 | 0.75-2.02 | .421 |
| SLAP repair | 0.83 | 0.41-1.67 | .593 |
| Labral repair | 1.01 | 0.25-4.10 | .986 |
| Distal clavicle excision | 1.07 | 0.79-1.45 | .678 |
| Synovectomy | 1.30 | 0.67-2.52 | .431 |
aRR, relative risk; SLAP, superior labrum anterior and posterior.
bMultivariate analysis adjusted for all baseline demographic and procedural characteristics listed in this table.
cConcomitant procedures were referenced to those rotator cuff repairs without each procedure (ie, subacromial decompression vs no subacromial decompression).
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: D.D.B. has received educational support from Medwest Associates. N.H.A. has received research support from Arthrex, Pacira, Smith & Nephew, Stryker, Trice Medical, and Zimmer; speaking fees from DePuy, Pacira, and Smith & Nephew; consulting fees from Biom’up, Medical Device Business Services, Pacira, Smith & Nephew, and Trice Medical; and hospitality payments from Novadaq Technologies. N.N.V. has received research support from Arthrex, Arthrosurface, Athletico, Conmed Linvatec, DJO, MioMed, Mitek, and Ossur; has received consulting fees from Arthrex, Medacta, Minivasive, OrthoSpace, and Smith & Nephew; has received educational support from Medwest Associates; has stock options from CyMedica, Minivasive, and Omeros; and receives royalties from Smith & Nephew and Vindico Medical Education–Orthopedics Hyperguide. B.F. has received research support from Arthrex and Stryker, has received fellowship support from Ossur and Smith & Nephew, has received consulting fees from Sonoma Orthopedics and Stryker, has received honoraria from Arthrosurface, has stock/stock options from Jace Medical, and receives royalties from Elsevier. J.N.L. has received educational support from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Agarwalla A, Gowd AK, Liu JN. et al. Effect of operative time on short-term adverse events after isolated anterior cruciate ligament reconstruction. Orthop J Sports Med. 2019;7(2):2325967118825453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alyea E, Gaston T, Austin LS. et al. The effectiveness of aspirin for venous thromboembolism prophylaxis for patients undergoing arthroscopic rotator cuff repair. Orthopedics. 2019;42(2):e187–e192. [DOI] [PubMed] [Google Scholar]
- 3. Basques BA, Saltzman BM, Mayer EN. et al. Resident involvement in shoulder arthroscopy is not associated with short-term risk to patients. Orthop J Sports Med. 2018;6(12):2325967118816293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Belmont PJ, Jr, Goodman GP, Hamilton W, Waterman BR, Bader JO, Schoenfeld AJ. Morbidity and mortality in the thirty-day period following total hip arthroplasty: risk factors and incidence. J Arthroplasty. 2014;29(10):2025–2030. [DOI] [PubMed] [Google Scholar]
- 5. Belmont PJ, Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20–26. [DOI] [PubMed] [Google Scholar]
- 6. Black EM, Austin LS, Narzikul A, Seidl AJ, Martens K, Lazarus MD. Comparison of implant cost and surgical time in arthroscopic transosseous and transosseous equivalent rotator cuff repair. J Shoulder Elbow Surg. 2016;25(9):1449–1456. [DOI] [PubMed] [Google Scholar]
- 7. Boddapati V, Fu MC, Schairer WW. et al. Increased shoulder arthroscopy time is associated with overnight hospital stay and surgical site infection. Arthroscopy. 2018;34(2):363–368. [DOI] [PubMed] [Google Scholar]
- 8. Bohl DD, Ondeck NT, Darrith B, Hannon CP, Fillingham YA, Della Valle CJ. Impact of operative time on adverse events following primary total joint arthroplasty. J Arthroplasty. 2018;33(7):2256–2262. [DOI] [PubMed] [Google Scholar]
- 9. Bongiovanni SL, Ranalletta M, Guala A, Maignon GD. Case reports: heritable thrombophilia associated with deep venous thrombosis after shoulder arthroscopy. Clin Orthop Relat Res. 2009;467(8):2196–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173(8):695–698. [DOI] [PubMed] [Google Scholar]
- 11. Burkhart SS. Deep venous thrombosis after shoulder arthroscopy. Arthroscopy. 1990;6(1):61–63. [DOI] [PubMed] [Google Scholar]
- 12. Catanzarite T, Saha S, Pilecki MA, Kim JY, Milad MP. Longer operative time during benign laparoscopic and robotic hysterectomy is associated with increased 30-day perioperative complications. J Minim Invasive Gynecol. 2015;22(6):1049–1058. [DOI] [PubMed] [Google Scholar]
- 13. Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39(10):2099–2107. [DOI] [PubMed] [Google Scholar]
- 14. Davis CL, Pierce JR, Henderson W. et al. Assessment of the reliability of data collected for the Department of Veterans Affairs National Surgical Quality Improvement Program. J Am Coll Surg. 2007;204(4):550–560. [DOI] [PubMed] [Google Scholar]
- 15. Day M, Westermann R, Duchman K. et al. Comparison of short-term complications after rotator cuff repair: open versus arthroscopic. Arthroscopy. 2018;34(4):1130–1136. [DOI] [PubMed] [Google Scholar]
- 16. Epstein AM. Revisiting readmissions: changing the incentives for shared accountability. N Engl J Med. 2009;360(14):1457–1459. [DOI] [PubMed] [Google Scholar]
- 17. Gowd AK, Bohl DD, Hamid KS, Lee S, Holmes GB, Lin J. Longer operative time is independently associated with surgical site infection and wound dehiscence following open reduction and internal fixation of the ankle [published online March 27, 2019]. Foot Ankle Spec. doi:10.1177/1938640019835299 [DOI] [PubMed] [Google Scholar]
- 18. Hariri A, Nourissat G, Dumontier C, Doursounian L. Pulmonary embolism following thrombosis of the brachial vein after shoulder arthroscopy: a case report. Orthop Traumatol Surg Res. 2009;95(5):377–379. [DOI] [PubMed] [Google Scholar]
- 19. Hill JR, McKnight B, Pannell WC. et al. Risk factors for 30-day readmission following shoulder arthroscopy. Arthroscopy. 2017;33(1):55–61. [DOI] [PubMed] [Google Scholar]
- 20. Igde M, Kabasakal H, Ozturk O, Karatekin G, Aygun C. Palivizumab prophylaxis, respiratory syncytial virus and subsequent development of asthma. Minerva Pediatr. 2018;70(3):252–259. [DOI] [PubMed] [Google Scholar]
- 21. Iyengar JJ, Samagh SP, Schairer W, Singh G, Valone FH, 3rd, Feeley BT. Current trends in rotator cuff repair: surgical technique, setting, and cost. Arthroscopy. 2014;30(3):284–288. [DOI] [PubMed] [Google Scholar]
- 22. Jensen AR, Cha PS, Devana SK. et al. Evaluation of the trends, concomitant procedures, and complications with open and arthroscopic rotator cuff repairs in the Medicare population. Orthop J Sports Med. 2017;5(10):2325967117731310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Khuri SF. The NSQIP: a new frontier in surgery. Surgery. 2005;138(5):837–843. [DOI] [PubMed] [Google Scholar]
- 24. Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–1795. [DOI] [PubMed] [Google Scholar]
- 25. Kuhn JE. Nonoperative treatment of rotator cuff tears. Am J Orthop (Belle Mead NJ). 2016;45(2):66–67. [PubMed] [Google Scholar]
- 26. Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. [DOI] [PubMed] [Google Scholar]
- 27. Luzzi AJ, Fleischman AN, Matthews CN, Crizer MP, Wilsman J, Parvizi J. The “bundle busters”: incidence and costs of postacute complications following total joint arthroplasty. J Arthroplasty. 2018;33(9):2734–2739. [DOI] [PubMed] [Google Scholar]
- 28. Maruthappu M, Duclos A, Zhou CD. et al. The impact of team familiarity and surgical experience on operative efficiency: a retrospective analysis. J R Soc Med. 2016;109(4):147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Meyer DC, Wieser K, Farshad M, Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med. 2012;40(10):2242–2247. [DOI] [PubMed] [Google Scholar]
- 30. Mitchell JM. Effect of physician ownership of specialty hospitals and ambulatory surgery centers on frequency of use of outpatient orthopedic surgery. Arch Surg. 2010;145(8):732–738. [DOI] [PubMed] [Google Scholar]
- 31. Ondeck NT, Bohl DD, McLynn RP. et al. Longer operative time is associated with increased adverse events after anterior cervical diskectomy and fusion: 15-minute intervals matter. Orthopedics. 2018;41(4):e483–e488. [DOI] [PubMed] [Google Scholar]
- 32. Pauzenberger L, Grieb A, Hexel M, Laky B, Anderl W, Heuberer P. Infections following arthroscopic rotator cuff repair: incidence, risk factors, and prophylaxis. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):595–601. [DOI] [PubMed] [Google Scholar]
- 33. Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J. 2006;2(1):70–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Polzhofer GK, Petersen W, Hassenpflug J. Thromboembolic complication after arthroscopic shoulder surgery. Arthroscopy. 2003;19(9):e129–e132. [DOI] [PubMed] [Google Scholar]
- 35. Schick CW, Westermann RW, Gao Y, Group A. Wolf BR. Thromboembolism following shoulder arthroscopy: a retrospective review. Orthop J Sports Med. 2014;2(11):2325967114559506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Seidl AJ, Lombardi NJ, Lazarus MD. et al. Arthroscopic transosseous and transosseous-equivalent rotator cuff repair: an analysis of cost, operative time, and clinical outcomes. Am J Orthop (Belle Mead NJ). 2016;45(7):e415–e420. [PubMed] [Google Scholar]
- 37. Shamsudin A, Lam PH, Peters K, Rubenis I, Hackett L, Murrell GA. Revision versus primary arthroscopic rotator cuff repair: a 2-year analysis of outcomes in 360 patients. Am J Sports Med. 2015;43(3):557–564. [DOI] [PubMed] [Google Scholar]
- 38. Shields E, Iannuzzi JC, Thorsness R, Noyes K, Voloshin I. Postoperative morbidity by procedure and patient factors influencing major complications within 30 days following shoulder surgery. Orthop J Sports Med. 2014;2(10):2325967114553164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Trickey AW, Wright JM, Donovan J. et al. Interrater reliability of hospital readmission evaluations for surgical patients. Am J Med Qual. 2017;32(2):201–207. [DOI] [PubMed] [Google Scholar]
- 40. Vandendriessche D, Giraudet G, Lucot JP, Behal H, Cosson M. Impact of laparoscopic sacrocolpopexy learning curve on operative time, perioperative complications and short term results. Eur J Obstet Gynecol Reprod Biol. 2015;191:84–89. [DOI] [PubMed] [Google Scholar]
- 41. Vopat BG, Lee BJ, DeStefano S. et al. Risk factors for infection after rotator cuff repair. Arthroscopy. 2016;32(3):428–434. [DOI] [PubMed] [Google Scholar]
- 42. Westermann RW, Anthony CA, Duchman KR, Pugely AJ, Gao Y, Hettrich CM. Incidence, causes and predictors of 30-day readmission after shoulder arthroplasty. Iowa Orthop J. 2016;36:70–74. [PMC free article] [PubMed] [Google Scholar]
- 43. Yamamoto A, Takagishi K, Osawa T. et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. [DOI] [PubMed] [Google Scholar]
- 44. Yeranosian MG, Arshi A, Terrell RD, Wang JC, McAllister DR, Petrigliano FA. Incidence of acute postoperative infections requiring reoperation after arthroscopic shoulder surgery. Am J Sports Med. 2014;42(2):437–441. [DOI] [PubMed] [Google Scholar]
- 45. Yoshihara H, Yoneoka D. Understanding the statistics and limitations of large database analyses. Spine (Phila Pa 1976). 2014;39(16):1311–1312. [DOI] [PubMed] [Google Scholar]
- 46. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]