Abstract
A severely comminuted and contaminated open tibial pilon fracture is one of the most challenging fractures we face. Although nowadays conducting multiple operations over various stages is a common treatment option taking into account the possibility of soft tissue damage, a gold standard protocol for severe pilon fractures has not yet been established. This case concerns a 56-year-old gentleman who suffered a severely comminuted and contaminated Gustilo 3b open tibial pilon fracture (AO 43C3.3) that was successfully treated using a circular frame external fixator without flap. Two years six months after the injury, there were no indications of any skin conditions at the site of the open wound, the range of ankle motion had been maintained and independent walking was possible. The score under the JSSF (Japanese Society of Surgery of the foot) ankle/hind foot scale was 81. This indicates that use of a circular frame external fixator is a useful treatment method in the event of a severe open pilon fracture where there is a large osteochondral bone defect.
Keywords: Pilon fracture, Plafond fracture, Ankle reconstruction, Ilizarov, Circular frame external fixator, Teramoto distal tibial oblique osteotomy
Case report
A 56-year-old gentleman cleaning a rooftop accidentally fell from a height of 5 m. He first landed on his right lower leg in the sand which resulted in multiple fractures. The initial X-rays showed a tibial plafond comminuted fracture as well as several segmental fibula fractures (Fig. 1). In addition, a 4 cm open wound was present over the distal medial aspect of the tibia. (Photograph 1). Although fortunately while there was no neurovascular injury, severe sand contamination was observed. Emergency irrigation, debridement and temporary external fixation were performed at that time. The fracture site was severely sand contaminated. The contaminated free bone fragments were debrided and the talus dome could be seen through the open wound (Photograph 2). Negative-pressure wound therapy (NPWT) for that open wound was performed. The postoperative X-rays indicated an approximately 5 cm long bone defect (Fig. 2). 14 days later, as there were no signs of infection, we reconstructed the ankle joint using the remaining medial, lateral and posterior malleoli with an Ilizarov external fixator with foot ring (Fig. 3). One month after the injury, we performed an osteotomy of the proximal tibia. Subsequently, we commenced bone transport at the rate of 1.0 mm per day and also removed the foot ring (Fig. 4). We then performed proximal bone fragment docking into the distal side accompanied by an iliac bone graft. This docking resulted in the healing of the open wound as the bone lengthening also resulted in skin elongation (Photograph 3). At the time of completing bone lengthening, the remaining deformities were four degrees valgus, five degrees anterior convex, and 10 degrees external rotation. Accordingly, for deformity correction, a temporary hexapod system was installed in the short term (Fig. 5). 15 months after the injury we removed the external fixator. Two years six months after the injury the patient's legs were in good alignment and there was no leg length discrepancy, enabling independent pain free walking and preserving the range of motion (Photograph 4 and Fig. 6). Under the verified rating scale established by the Japanese Society for Surgery of the Foot (JSSF), the ankle/hind foot rating was 81 and we note that the patient was able to resume a normal lifestyle.
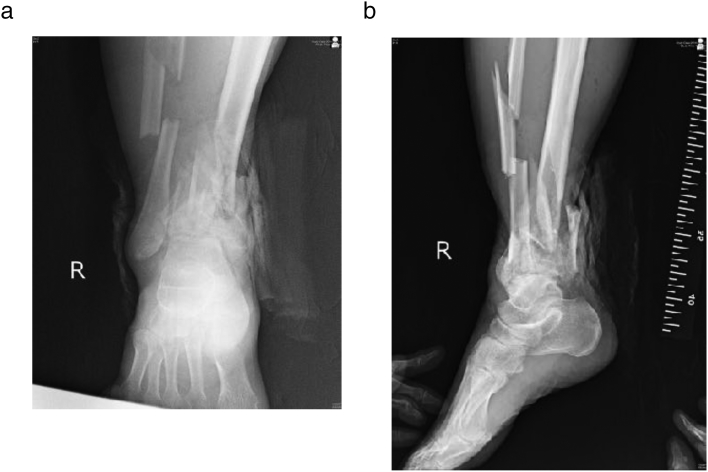
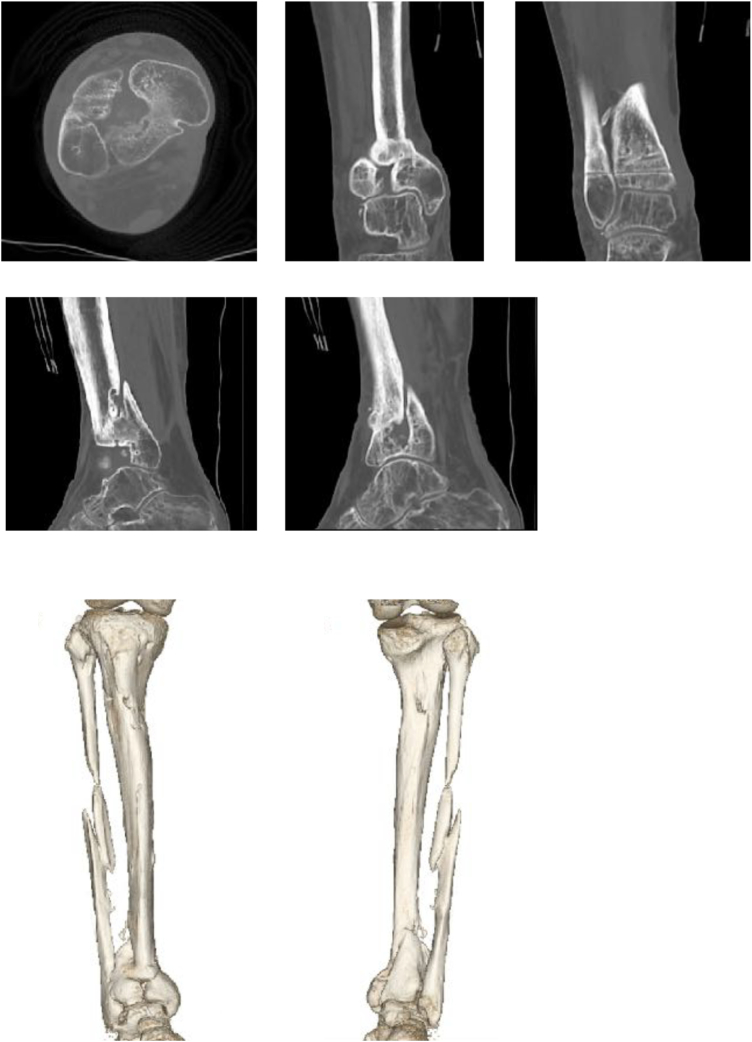
Fig. 1.
a) AP b) lateral.
Initial X-ray shows severe comminuted fractures in the tibia plafond and segmental fibula.
Photograph 1.
A 4 cm open wound was present over the distal medial aspect of the tibia. There was sand contamination in the open wound.
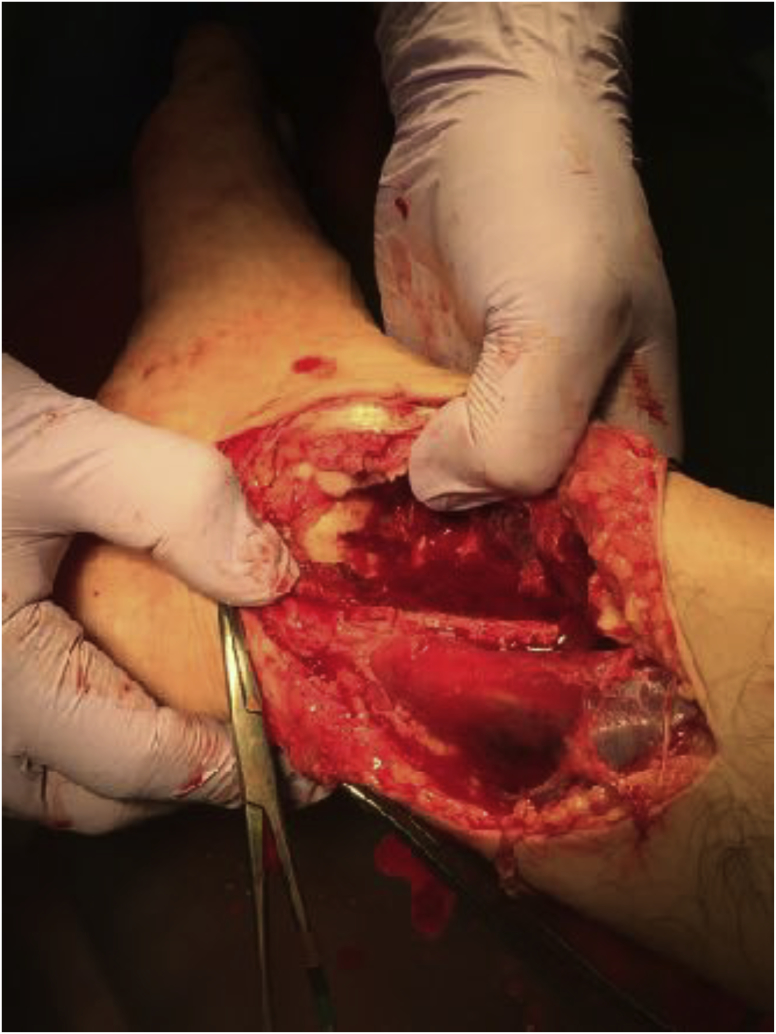
Photograph 2.
During the first debridement, the talus dome could be seen at the site of the open wound.
Fig. 2.
a) AP b) lateral.
A bone defect of approximately 5 cm was present from the tibial plafond to the distal tibial diaphysis.
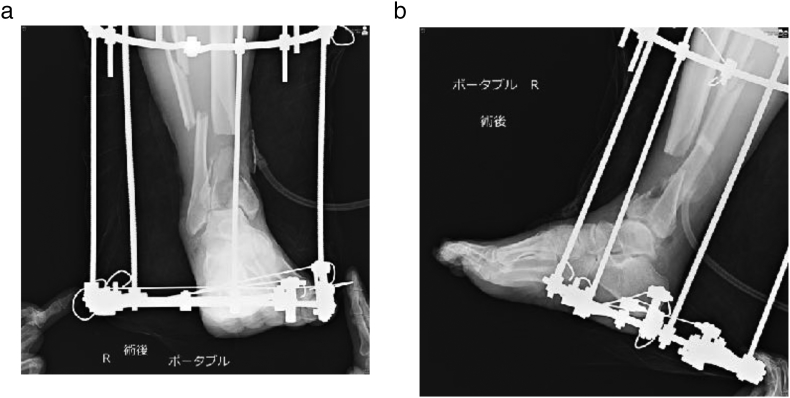
Fig. 3.
a) AP b) lateral.
The X-ray post ankle joint reconstruction shows remaining medial, lateral and posterior malleoli.
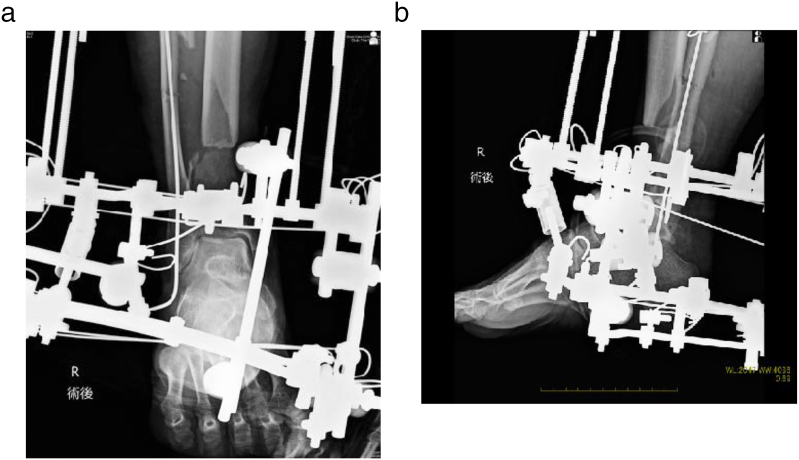
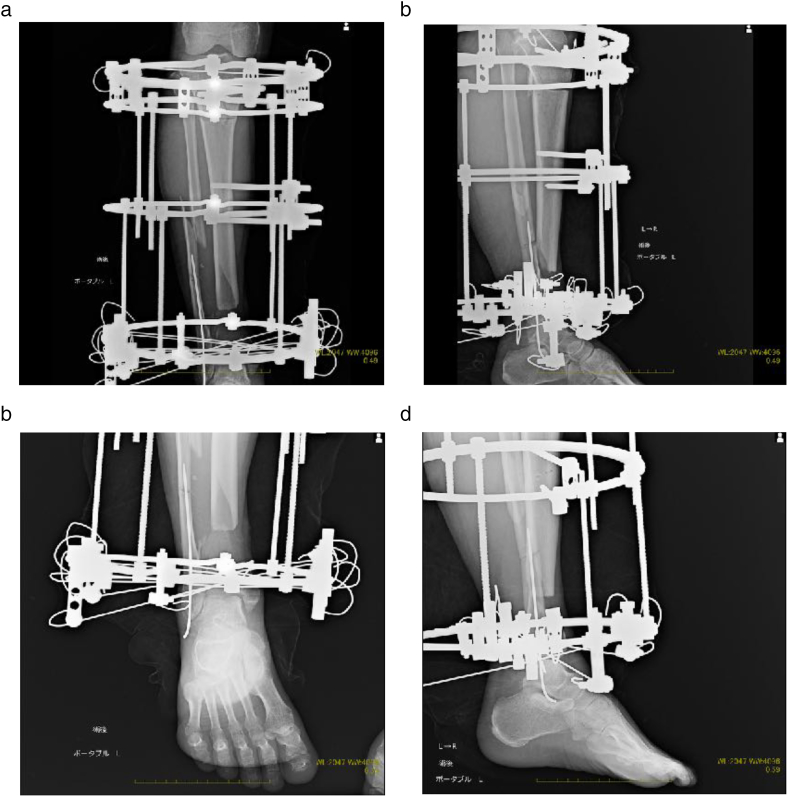
Fig. 4.
a) AP b) lateral c) AP d) lateral.
The X-ray after proximal tibia osteotomy and removal of the foot ring. Bone transport was performed one week after the osteotomy.
Photograph 3.
Open wound macroscopic picture process. The wound was allowed to heal prior to completing the bone transport. No skin flap or graft was required.
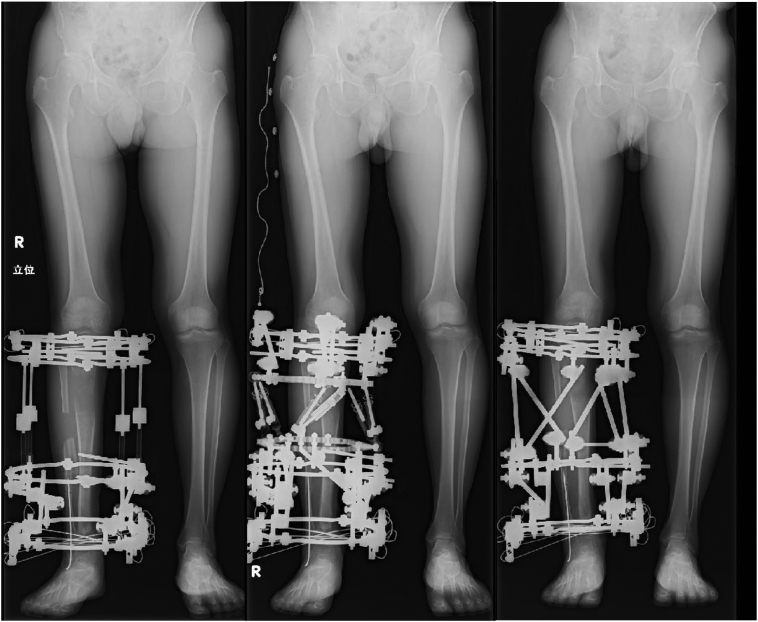
Fig. 5.
Deformity correction by temporary installation of hexapod system.
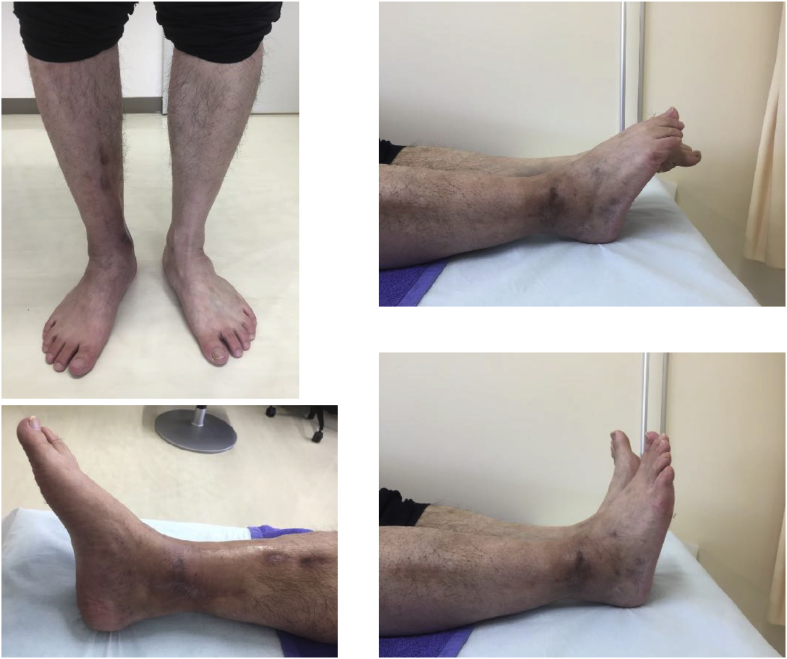
Photograph 4.
Macroscopic pictures two years six months post injury.
The open wound has healed well and is in good condition. Although the range of ankle motion is slightly restricted, the patient is able to walk independently.
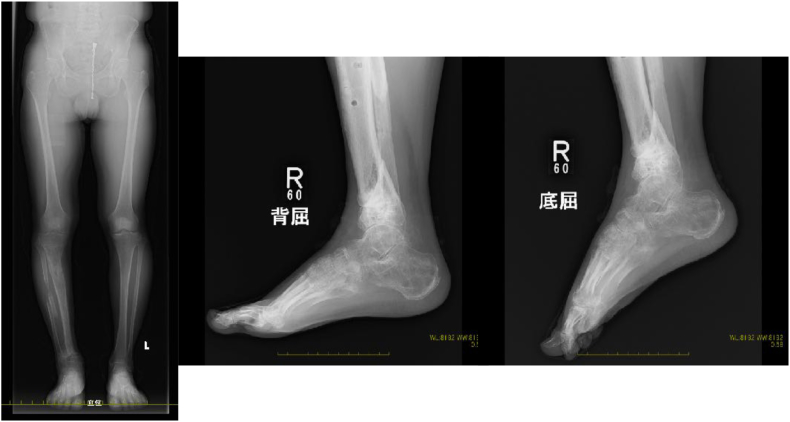
Fig. 6.
Final standing X-rays & lateral view of dorsiflex and plantarflex.
Lower extremity alignment is good and the talocrural joint has been preserved.
Discussion
Severe open pilon fractures are one of the most challenging fractures that we face given that is significantly difficult to recover ankle joint function [[1], [2], [3], [4]]. While operations over several stages are nowadays a popular treatment method taking into consideration soft tissue injuries [1,2], recently some articles have recommend early soft tissue cover of the open wound using a vascularized muscle flap [5,6]. In general, in the event of an open tibial fracture it is often the case that damage to the soft tissues poses a larger risk than bone damage. In this case there was a severely comminuted high-energy open pilon fracture that was further complicated by sand contamination. Accordingly, this is a rare case in which the possibility of bone defect outweighs the soft tissue injury that might result from radical debridement. In this case, preserving ankle joint function was challenging given the large bone defect and the absence of almost half of the cartilage on the joint surface. Some recent studies have reported that primary arthrodesis has resulted in good functional outcomes [[7], [8], [9], [10]]. The patient was made aware of this fact and that primary arthrodesis was one treatment option that would allow for his early reintegration into society. However the patient refused arthrodesis and therefore in order to preserve his ankle joint we urged him to take advantage of a circular frame external fixator. Ling et al. reported that “ankle arthrodesis does increase the risk of adjacent joint arthritis, particularly involving the subtalar joint and mid foot [11].” Further, Mr. Bear concluded in his report “primary arthrodesis should be considered on a case-by-case basis and used only in patients in which reconstruction of the articular surface is not a viable option [12].” We fully agree with these opinions, and especially for the younger generation, that arthrodesis should only be considered a treatment of last resort.
Ankle reconstruction was performed under fluoroscopic control using examples as reported in “Teramoto Distal Tibial Oblique Osteotomy [13]”. In this case study what is of importance is that the medial, lateral and posterior malleoli remained. So even though almost half of the tibia plafond was lost, we were able to preserve a functional ankle joint. As shown in the final follow-up CT scan (Fig. 7) a partial union of the medial, lateral and posterior sides of the distal tibia was indicated. Regardless of a bone defect in almost half of the tibia plafond, the patient is now able to walk without crutches. The X-rays taken shortly after removing the external fixator (Fig. 8) indicated the presence of early osteoarthritis (OA) of the ankle. The radiological assessment of the A-P mortise angle was 91 degrees, the empirical axis 80 degrees, the medial malleolar angle 15 degrees, the tibial angle 74 degrees, the fibular angle 66 degrees, the lateral mortise angle 81 degrees, the α-angle 108 degrees, and the β-angle 106 degrees. At the final follow-up (one year seven months post removal of the implant) X-rays (Fig. 9), no worsening of OA was indicated as of that date. In addition radiological assessments remained approximately the same as stated above, being (A-P mortise angle 88 degrees, Empirical axis 80 degrees, Medial malleolar angle 16 degrees, Tibial angle 76 degrees, Fibular angle 63 degree, Lateral mortise angle 79 degrees, α-angle 110 degrees, and β-angle 111 degrees). In the authors' experience few open tibial pilon fracture have achieved such success in terms of the satisfactory recovery of ankle function, which makes this case study of value. Although recognizing that there has only been a short-term follow up, it is our intent to conduct long-term follow ups to detect other future failures such as chronic ankle pain, so that we are best positioned to suggest future treatments: i.e. osteotomy or arthrodesis or total ankle arthroplasty.
Fig. 7.
CT scan imaging nine months after implant removal. The bone defect at the center of tibia plafond indicated a partial union of the medial, lateral and posterior sides of the distal tibia.
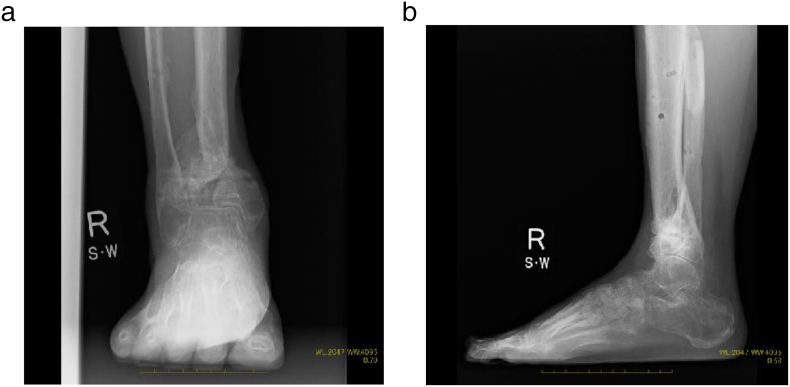
Fig. 8.
a) AP b) lateral.
Weight bearing X-rays shortly after removal of the external fixator. While these indicated the presence of early osteoarthritis, the congruency of the talocrural joint was good.
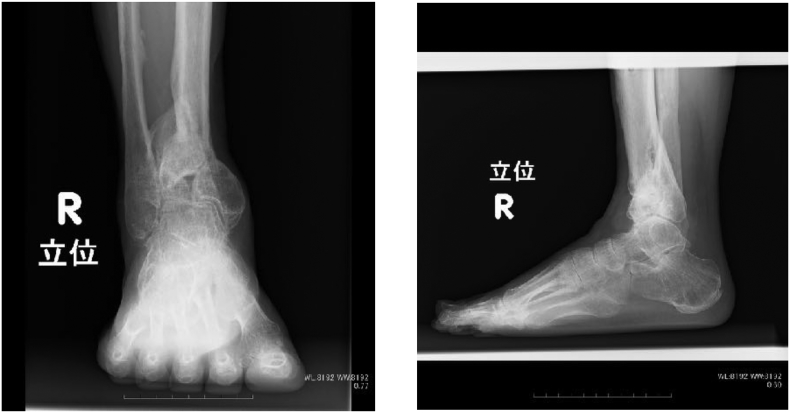
Fig. 9.
a) AP b) lateral.
Weight bearing X-rays at the final follow-up (one year seven months post implant removal). No exacerbation of early osteoarthritis was observed.
Conclusion
The treatment implemented in the herein case can be considered in similar severe open pilon fracture cases.
Declaration of Competing Interest
No conflicts of interest shall result from publication of this article.
Acknowledgements
The authors would like to acknowledge Prof. Peter V Giannoudis for supporting the publication of this article.
References
- 1.Tarkin I.S., Clare M.P., Marcantonio A. An update on the management of high-energy pilon fractures. Injury. Int. J. Care. 2008;39:142–154. doi: 10.1016/j.injury.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 2.Calori G.M., Tagliabue L., Mazza E. Tibial pilon fractures: which method of treatment? Injury. Int. J. Care Injured. 2010;41:1183–1190. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 3.Mauffrey C., Vasario G., Battiston B. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop. Belg. 2011;77:432–440. [PubMed] [Google Scholar]
- 4.Jacob N., Amin A., Giotakis N. Management of high-energy tibial pilon fractures. Strat Traum Limb Recon. 2015;10:137–147. doi: 10.1007/s11751-015-0231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gopal S., Majumder S., Batchelor A.G. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J. Bone Joint Surg. (Br.) 2000;82:959–966. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 6.Conroy J., Agarwal M., Giannoudis P.V. Early internal fixation and soft tissue cover of severe open tibial pilon fractures. Int. Orthop. 2003;27:343–347. doi: 10.1007/s00264-003-0486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho B., Ketz J. Primary arthrodesis for tibial pilon fractures. Foot Ankle Clin N Am. 2017;22:147–161. doi: 10.1016/j.fcl.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Ermias A., Dana J F., Boris Z. Primary posterior blade plate tibiotalar arthrodesis: a salvage procedure for complex nonreconstructable pilon fractures. J. Orthop. Trauma. 2017;31(Suppl. 3):S30–S33. doi: 10.1097/BOT.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 9.Beaman D.N., Gellman R. Fracture reduction and primary ankle arthrodesis: a reliable approach for a severely comminuted tibial pilon fracture. Clin. Orthop. Relat. Res. 2014;472:3823–3834. doi: 10.1007/s11999-014-3683-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zelle B., Gruen G., McMillen R. Primary arthrodesis of the tibiotalar joint in severely comminuted high-energy pilon fractures. J. Bone Joint Surg. Am. 2014;96(11):e91. doi: 10.2106/JBJS.M.00544. [DOI] [PubMed] [Google Scholar]
- 11.Ling J., Smyth N., Fraser E. Investigating the relationship between ankle arthrodesis and adjacent-joint arthritis in the hind foot: a systematic review. J. Bone Joint Surg. Am. 2015;97:513–520. doi: 10.2106/JBJS.N.00426. [DOI] [PubMed] [Google Scholar]
- 12.Bear J., Rollick N., Helfet D. Evolution in Management of Tibial Pilon Fractures. Curr Rev Musculoskelet Med. 2018;11:537–545. doi: 10.1007/s12178-018-9519-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teramoto T., Harada S., Takaki M. The Teramoto distal oblique osteotomy (DTOO): surgical technique and applicability for ankle osteoarthritis with varus deformity. Strat Traum Limb Recon. 2018;13:43–49. doi: 10.1007/s11751-018-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]