Abstract
Background:
In the S-TRAC trial, adjuvant sunitinib prolonged disease-free survival (DFS) versus placebo in patients with loco-regional renal cell carcinoma at high risk of recurrence after nephrectomy. An exploratory analysis evaluated associations between single nucleotide polymorphisms (SNPs) in several angiogenesis- or hypoxia-related genes and clinical outcomes in S-TRAC.
Methods:
Blood samples were genotyped for 10 SNPs and one insertion/deletion mutation using TaqMan assays. DFS was compared using log-rank tests for each genotype in sunitinib versus placebo groups and between genotypes within each of three (sunitinib, placebo, and combined sunitinib plus placebo) treatment groups. P-values were unadjusted.
Results:
In all, 286 patients (sunitinib, n=142; placebo, n=144) were genotyped. Longer DFS (HR [95% confidence interval]) was observed with sunitinib versus placebo for VEGFR1 rs9554320 C/C (0.44 [0.21–0.91]; P=0.023), VEGFR2 rs2071559 T/T (0.46 [0.23–0.90]; P=0.020), and eNOS rs2070744 T/T (0.53 [0.30–0.94]; P=0.028). Shorter DFS was observed for VEGFR1 rs9582036 C/A versus C/C with sunitinib, placebo, and combined therapies (P≤0.05), and A/A vs C/C with sunitinib (P=0.022). VEGFR1 rs9554320 A/C versus A/A was associated with shorter DFS in the placebo (P=0.038) and combined (P=0.006) groups.
Conclusions:
Correlations between VEGFR1 and VEGFR2 SNPs and longer DFS with sunitinib suggest germline SNPs are predictive of improved outcomes with adjuvant sunitinib in patients with renal cell carcinoma. Independent validation studies are needed to confirm these findings.
Keywords: adjuvant, disease-free survival, pharmacogenomics, renal cell carcinoma, sunitinib
Translational Relevance
In patients with loco-regional renal cell carcinoma (RCC) at high risk of recurrence after nephrectomy, correlations between single nucleotide polymorphisms (SNPs) in VEGFR1, VEGFR2, and eNOS genes and improved disease-free survival (DFS) in the sunitinib group compared with the placebo group support the hypothesis that germline SNPs could have potential predictive value to identify patients who might derive more benefit from adjuvant sunitinib. Additionally, SNPs in VEGFR1, VEGFR2, and CCDC26 demonstrated a potential trend toward prognostic value for either DFS or overall survival across treatment groups. Therefore, these data could be used in the development of a pharmacogenomic biomarker assay that could potentially improve risk assessment and help to select patients who are most likely to benefit from adjuvant treatment in the RCC setting.
INTRODUCTION
Due to the increased use of radiologic and ultrasound imaging techniques, incidental detection of renal cell carcinoma (RCC) occurs more frequently today, contributing to an increase in the number of patients diagnosed with stage I–III (localized or loco-regional) disease. Thus, optimizing the management of early stage RCC is a key priority in clinical practice (1, 2). For patients with TNM [tumor, lymph nodes, metastasis] stage I and II RCC, surgery alone may be sufficient, with 5-year cancer-specific survival rates of 91% and 74% for stage I and II, respectively. However, a number of patients with stage III or IV non-metastatic RCC (+/– regional lymph node involvement) will eventually relapse and progress to stage IV metastatic RCC (3). To try and identify those patients with the highest risk of relapse, there are several scoring systems in use, based on clinical and pathologic features (4–8). Based on risk stratification using the University of California Los Angeles Integrated Staging System (UISS), up to 15% of patients with non-metastatic RCC who undergo nephrectomy are considered at high risk (UISS III–IV) of recurrence and approximately 40% of these will relapse within 5 years (6, 9, 10).
Sunitinib is a multi-targeted inhibitor of the VEGF signaling pathway and is approved for the treatment of metastatic RCC, and approved by the US Food and Drug Administration as adjuvant therapy in patients at high risk for recurrent RCC post nephrectomy (11). In the randomized phase III S-TRAC trial, adjuvant sunitinib prolonged disease-free survival (DFS) versus placebo in patients with loco-regional RCC (≥T3 and/or N+) at high risk of recurrence following nephrectomy (based on blinded independent central review): HR 0.76; 95% confidence interval (CI), 0.59–0.98 (P = 0.03), and median DFS 6.8 years versus 5.6 years (12, 13).
The addition of a pharmacogenomic biomarker assay based on the understanding of host versus disease biology could potentially improve risk assessment and help to select patients who are most likely to benefit from adjuvant treatment. The most common genetic DNA sequence variations are single nucleotide polymorphisms (SNPs) (14). A number of SNPs have been reported as potential predictors of efficacy and/or toxicity in patients with advanced RCC treated with anti-angiogenic tyrosine kinase inhibitors (15–23). The impact of these SNPs on the efficacy and safety of tyrosine kinase inhibitors range from modulating pharmacokinetics (e.g., through increased drug clearance) through to pharmacodynamics (e.g., increased expression of target proteins), and/or activation of downstream signaling pathways (15–29). With regards to SNPs in VEGF and VEGF receptors (VEGFR)-1, 2, or 3, various studies and analyses have reported that certain SNPs are associated with poorer response rate, overall survival (OS), and/or progression-free survival (PFS) in patients with metastatic RCC treated with sunitinib (19, 20, 24–29).
Therefore, the objectives of these exploratory, hypothesis-generating analyses were to evaluate potential associations between a subset of SNPs in genes known to be involved in angiogenesis and clinical outcomes by using data from a subset of patients enrolled in the S-TRAC trial.
METHODS
Study Design and Patients
S-TRAC was a randomized, double-blind, phase III trial (ClinicalTrials,gov, ) in patients with loco-regional RCC at high risk of tumor recurrence after nephrectomy (12, 13). Details on eligibility were previously reported (12, 13). Briefly, patients were ≥18 years old and had a histologic confirmation of clear-cell, loco-regional (≥T3 and/or N+) RCC. Other inclusion criteria were: Eastern Cooperative Oncology Group performance status 0–2 before nephrectomy; no prior systemic therapy for RCC; and lack of macroscopic residual or metastatic disease, determined by blinded independent central review.
Patients were randomly assigned (1:1) to receive sunitinib 50 mg/day or placebo on a 4-weeks-on/2-weeks-off schedule for 1 year or until disease recurrence, diagnosis of secondary malignancy, unacceptable side effect, or consent withdrawal (12, 13). The trial was approved by the independent review board or ethics committee at each center and was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonization Good Clinical Practice guidelines and applicable local regulatory requirements and laws. All patients provided written informed consent.
Molecular Biomarker Assays
Anonymized blood samples were prospectively collected from patients in the S-TRAC trial who consented to the molecular profiling substudy. Samples were genotyped for 10 SNPs and one insertion/deletion mutation, some of which have been previously hypothesized to predict response to sunitinib in treatment of metastatic RCC (Table 1) (19, 24–26).
Table 1.
Candidate SNPs associated with response to anti-angiogenic therapy
| Gene | Alternative Name | SNP Allele Change | mRNA Position Allele Change | Protein Position and Change |
|---|---|---|---|---|
| VEGFA | VPF, MVCD1, MGC70609 | rs699947 A>C | –2055 A>C NM_001025366.2 |
– |
| VEGFA | VPF, MVCD1, MGC70609 | rs833061 C>T | –958 C>T NM_001025366.2 |
– |
| VEGFR1 | FLT, FLT1 | rs9554320 A>C | 3387–692 T>G NM_002019.4 |
– |
| VEGFR1 | FLT, FLT1 | rs9582036 C>A | 3635+319 G>T NM_002019.4 |
– |
| VEGFR2 | KDR, FLK1, CD309 | rs2071559 T>C | –906 T>C NM_002253.2 |
– |
| VEGFR2 | KDR, FLK1, CD309 | rs1870377 T>A | 1416 A>T NM_002253.2 |
Gln472His |
| VEGFR3 | FLT4, PCL, FLT41, LMPH1A | rs6877011 C>G | 721 G>C NM_182925.4 |
― |
| LOXL2 | LOR2, WS9–14 | rs4872122 A>C | –84+12722 T>G NM_002318.2 |
― |
| eNOS | NOS3, ecNOS | rs2070744 T>C | –813 C>T NM_001160109.1 |
― |
| SH3GL2 | CNSA2, SH3P4, EEN-B1, SH3D2A | rs10963287 C>T | ― | ― |
| CCDC26 | RAM | rs60315789 −/TAT | ― | ― |
Following sample de-identification and DNA extraction, DNA amplification was carried out using PCR. Commercially available TaqMan® assays (Thermo Fisher Scientific, Waltham, MA) were used and analyzed on an Applied Biosystems QuantStudio™ 12K Flex Real-Time PCR System (Thermo Fisher Scientific; dba: Life Technologies), and was performed at Pfizer Clinical Pharmacogenomics Laboratory (Pfizer Inc, Groton, CT). The SNP SH3GL2 rs10963287 was determined using a laboratory developed TaqMan assay. The region immediately surrounding SNP rs10963287 contains a short interspersed nuclear elements [SINE] region; therefore, the assay to determine the genotype of rs10963287 involved amplifying a region encompassing the SNP. The PCR product from this initial reaction was used as the input template for TaqMan analysis. For coiled-coil domain-containing protein 26 (CCDC26), the three nucleotide in-Del rs60315789 was detected by amplifying a region around the insertion, sizing the fragment using an ABI3730xl DNA analyzer, and then analyzing the data using the GeneMapper® 5.0 software (Thermo Fisher Scientific).
Statistical Analyses
The pharmacogenomics population comprised all patients who received at least one dose of study medication (i.e., treatment assignments designated according to actual study treatment received) and who had at least one genotype result. The primary endpoint in S-TRAC was DFS, which was defined as time from randomization until recurrence or secondary malignancy, as assessed by blinded independent central review, or death. OS was assessed as a secondary endpoint.
Fisher’s exact test was used to compare baseline demographics and characteristics between treatment groups. Two-sided 95% CIs for allele frequency and genotype frequency were determined by exact method using the F distribution. All SNPs were examined for deviation from Hardy-Weinberg Equilibrium; P values were calculated using Pearson’s Chi-squared test based on 10,000 replicates. Linkage disequilibrium analysis was also performed for SNP pairs. D′, r2, and P values were calculated for each pair of SNPs within a given gene or on the same chromosome.
In exploratory analyses, DFS and OS between sunitinib and placebo groups were compared for each genotype with Kaplan–Meier estimates and an unstratified log-rank test. Estimated HR and its two-sided 95% CI were provided using Cox proportional hazards models. Genotype subgroups were also compared within each treatment group and for the combined sunitinib and placebo treatment groups (“combined group”) using the same statistical approach, where applicable. P values were unadjusted for multiplicity. The log-rank P value and HR statistic were produced only when there were ≥10 events in both comparison groups. The data cut-off date for these analyses was April 7, 2016 (per the primary S-TRAC analyses) (12).
RESULTS
Patient Population
Of 615 patients enrolled in S-TRAC, 610 received treatment (n=306 and n=304, sunitinib and placebo, respectively) (12). Of these patients, 286 (46.9%; n=142 and 144, sunitinib and placebo, respectively) consented to the pharmacogenomic analysis and provided a blood sample that was successfully genotyped. Due to ethnic or religious reasons, or regulations imposed by local health authorities, 324 patients did not consent or provide a blood sample that could be successfully genotyped. Demographics and baseline clinical characteristics of genotyped subgroups treated with sunitinib or placebo were generally comparable (Table 2). However, there were differences between 286 patients who were genotyped and the 324 who were not genotyped; a greater number of genotyped patients were older, white, and were categorized in the UISS high-risk group (Table 2).
Table 2.
Patient baseline characteristics
| Variable, n (%) | All Patients |
Genotyped |
||||
|---|---|---|---|---|---|---|
| Genotyped n=286 | Non-genotyped n=324 | P Valuea (Genotyped vs. Non-genotyped) | Sunitinib n=142 | Placebo n=144 | P Value (Sunitinib vs. Placebo) | |
| Age, years | ||||||
| <65 | 195 (68.2) | 258 (79.6) | 0.002 | 95 (66.9) | 100 (69.4) | 0.704 |
| ≥65 | 91 (31.8) | 66 (20.4) | 47 (33.1) | 44 (30.6) | ||
| Sex | ||||||
| Male | 206 (72.0) | 241 (74.4) | 0.522 | 97 (68.3) | 109 (75.7) | 0.188 |
| Female | 80 (28.0) | 83 (25.6) | 45 (31.7) | 35 (24.3) | ||
| Race | ||||||
| White | 258 (90.2) | 254 (78.4) | <0.001 | 127 (89.4) | 131 (91.0) | 0.097 |
| Asian | 17 (5.9) | 59 (18.2) | 11 (7.7) | 6 (4.2) | ||
| Other | 11 (3.8) | 11 (3.4) | 4 (2.8) | 7 (4.9) | ||
| ECOG PS | ||||||
| 0 | 208 (72.7) | 237 (73.1) | 0.730 | 101 (71.1) | 107 (74.3) | 0.818 |
| 1 | 75 (26.2) | 86 (26.5) | 39 (27.5) | 36 (25.0) | ||
| 2 | 1 (0.3) | 0 | 1 (0.7) | 1 (0.7) | ||
| UISS group | ||||||
| T3 lowb | 86 (30.1) | 139 (42.9) | 0.009 | 41 (28.9) | 45 (31.3) | 0.805 |
| T3 highc | 172 (60.1) | 158 (48.8) | 89 (62.7) | 83 (57.6) | ||
| T4, N0 or NX, M0d | 5 (1.7) | 3 (0.9) | 2 (1.4) | 3 (2.1) | ||
| Any T, N+, M0d | 23 (8.0) | 24 (7.4) | 10 (7.0) | 13 (9.0) | ||
P values calculated using Fisher’s exact test.
Genotyped vs. non-genotyped; unadjusted for multiplicity.
N0 or NX, M0, any Fuhrman grade and ECOG PS 0 or N0 or NX, M0, Fuhrman grade 1 and ECOG PS ≥1.
N0 or NX, M0, Fuhrman grade ≥2 and ECOG PS ≥1.
Any Fuhrman grade and any ECOG PS.
Abbreviations: ECOG PS, Eastern Cooperative Oncology Group performance status.
Genotyping
There were no unexpected findings in allele and genotype frequencies for SNPs (Supplementary Tables S1 and S2). For most SNPs, there were no deviations in genotype frequencies from the Hardy-Weinberg Equilibrium; however, two SNPs showed deviation from Hardy-Weinberg Equilibrium: VEGFR2 rs1870377 (P = 0.017) and VEGFR3 rs6877011 (P < 0.001). High linkage disequilibrium was detected between the following SNPs: VEGFR2 rs1870377 and rs2071559 on chromosome 4 (D′ = 0.250; r2 = 0.015; P = 0.036); VEGFA rs699947 and rs833061 on chromosome 6 (D′=1.000; r2 = 0.979; P < 0.001); and VEGFR1 rs9582036 and rs9554320 on chromosome 13 (D′ = 0.977; r2 = 0.584; P < 0.001).
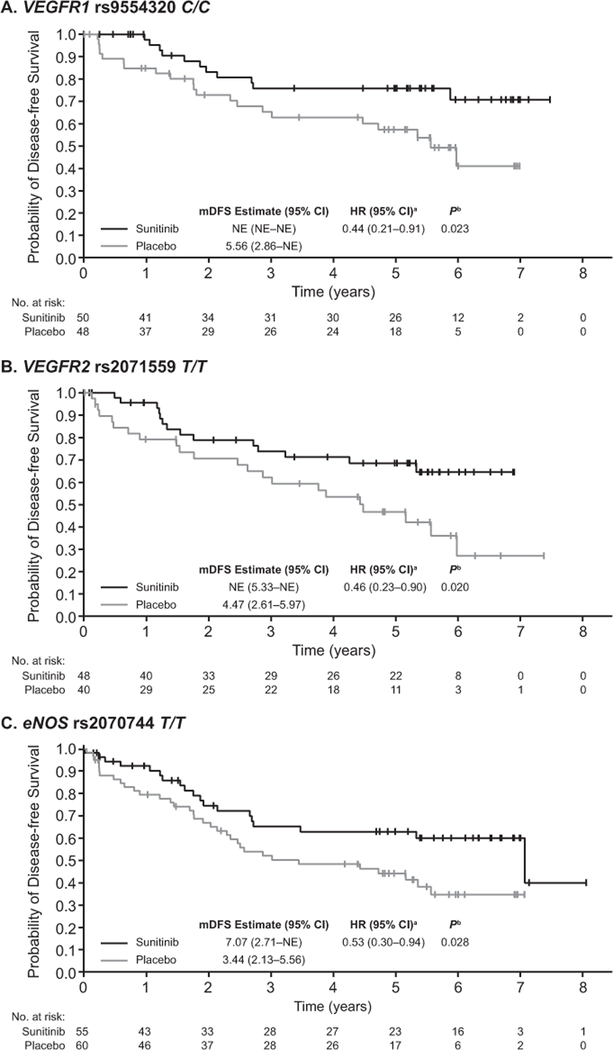
Association Between DFS and Each Genotype in Sunitinib Versus Placebo Group
The following genotypes were associated with a longer DFS in the sunitinib versus placebo group (Table 3): C/C genotype for VEGFR1 rs9554320 (HR 0.44; 95% CI, 0.21–0.91; P = 0.023) (Figure 1A); T/T genotype for VEGFR2 rs2071559 (HR 0.46; 95% CI, 0.23–0.90; P = 0.020) (Figure 1B); T/T genotype for eNOS rs2070744 (HR 0.53; 95% CI, 0.30–0.94; P = 0.028) (Figure 1C).
Table 3.
Comparison of DFS stratified by genotype and treatment group
| Gene/SNP | Sunitinib vs. Placebo: HR (95% CI); P Unadjusted | ||
|---|---|---|---|
| VEGFA rs699947 | A/A 0.78 (0.33–1.87); 0.579 |
A/C 0.65 (0.39–1.10); 0.107 |
C/C 0.81 (0.41–1.61); 0.547 |
| VEGFA rs833061 | C/C 0.78 (0.33–1.87); 0.579 |
C/T 0.65 (0.39, 1.08); 0.094 |
T/T 0.83 (0.41–1.68); 0.604 |
| VEGFR1 rs9554320 | A/A 1.32 (0.42–4.20); 0.636 |
A/C 0.85 (0.54–1.36); 0.507 |
C/C 0.44 (0.21–0.91); 0.023 |
| VEGFR1 rs9582036 | C/C 0.77 (0.08–7.49); 0.825 |
C/A 0.98 (0.61–1.59); 0.945 |
A/A 0.56 (0.30–1.02); 0.054 |
| VEGFR2 rs2071559 | T/T 0.46 (0.23–0.90); 0.020 |
T/C 1.03 (0.60–1.78); 0.914 |
C/C 0.72 (0.33–1.58); 0.417 |
| VEGFR2 rs1870377 | A/A Not donea |
A/T 0.74 (0.39–1.40); 0.357 |
T/T 0.70 (0.43–1.15); 0.161 |
| VEGFR3 rs6877011 | C/C 0.72 (0.48–1.06); 0.096 |
C/G 1.38 (0.48–4.01); 0.550 |
G/G Not donea |
| LOXL2 rs4872122 | A/A 0.81 (0.37–1.75); 0.589 |
A/C 0.72 (0.41–1.26); 0.245 |
C/C 0.75 (0.39–1.44); 0.388 |
| eNOS rs2070744 | T/T 0.53 (0.30–0.94); 0.028 |
T/C 0.96 (0.55–1.66); 0.879 |
C/C 0.85 (0.26–2.80); 0.794 |
| SH3GL2 rs10963287 | C/C 0.82 (0.50–1.32); 0.407 |
C/T 0.56 (0.28–1.10); 0.088 |
T/T 0.94 (0.29–3.10); 0.920 |
| CCDC26 rs60315789 | –/– 0.56 (0.24–1.28); 0.161 |
–/TAT 0.66 (0.38–1.12); 0.117 |
TAT/TAT 1.06 (0.53–2.10); 0.874 |
HR calculated using the unstratified Cox proportional hazards model. Two-sided P value from the unstratified log-rank test.
Due to events <10 in both comparison groups.
Figure 1.
Kaplan–Meier curve of DFS by genotype. aSunitinib vs. placebo. bUnstratified two-sided log-rank test. Abbreviation: NE, not estimable.
A trend for a longer DFS in the sunitinib versus placebo group was observed for VEGFR1 rs9582036 A/A (HR 0.56; 95% CI, 0.30–1.02; P = 0.054; Table 3). None of the genotypes for other tested SNPs showed differences in DFS between sunitinib and placebo (Table 3).
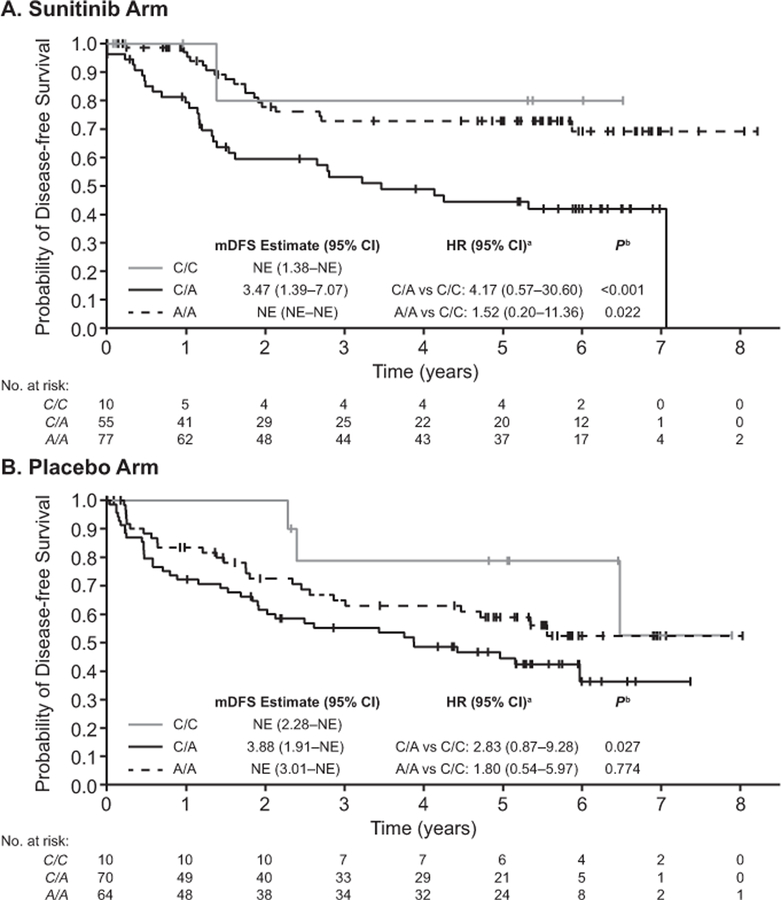
Association Between DFS and Genotype Subgroups Within Each Treatment Group and the Combined Group
The following genotype subgroups were associated with a shorter DFS (Supplementary Table S3). The heterozygous genotype C/A of VEGFR1 rs9582036 compared with the homozygous genotype C/C in the sunitinib (P < 0.001), placebo (P = 0.027), and combined (P < 0.001) groups; homozygous genotype A/A compared with genotype C/C only in the sunitinib group (P = 0.022) (Figure 2A–B); heterozygous genotype A/C of VEGFR1 rs9554320 compared with the homozygous genotype A/A in the placebo (P = 0.038) and combined (P = 0.006) groups, with a trend in the sunitinib group (P = 0.051); and A/A genotype of VEGFR2 rs1870377 compared with genotype T/T in the combined (P = 0.018) but not the placebo (P = 0.198) groups. No statistical test was performed in the sunitinib group because only seven patients had the A/A genotype.
Figure 2.
Kaplan–Meier Curve of DFS by genotype subgroups for VEGFR1 rs9582036. aSunitinib vs. placebo. bUnstratified two-sided log-rank test. Abbreviation: NE, not estimable.
None of the genotype subgroups for the other SNPs analyzed showed differences in DFS within each treatment group or when the treatments groups were combined.
Association Between OS and Genotypes
Correlation between the genotypes and OS was assessed by comparing sunitinib versus placebo within each SNP genotype subgroup. There were no other significant associations between SNP genotype and OS for sunitinib versus placebo; however, OS data were not mature at the time of data cut-off (Supplementary Table S4).
Correlations between OS and the SNP genotype subgroups were also carried out within each treatment group and by combining the two treatment groups. The genotype ‘−/−’ (i.e., no insertion) of CCDC26 rs60315789 showed a trend toward longer OS versus the heterozygous −/TAT genotype in the sunitinib (HR 3.01; 95% CI, 0.88–10.31; P = 0.089) and placebo (HR 2.01; 95% CI, 0.74–5.44; P = 0.122) groups. A significant association was observed when the treatment groups were combined (HR 2.39; 95% CI, 1.11–5.16; P = 0.022). No other associations were reported for OS and genotypes within each treatment group or in the combined group.
DISCUSSION
In these exploratory analyses, correlations between 11 SNPs (including specific SNPs in VEGFA, VEGFR1, and VEGFR3) and DFS and OS were assessed in patients with locoregional RCC. Three of the 11 SNPs demonstrated improved DFS with sunitinib treatment over placebo with HRs between 0.44 and 0.56, compared to 0.76 for the overall population. This improvement in HR supports a predictive value for this biomarker-defined subset of patients receiving sunitinib treatment. In particular, the genotypes C/C for VEGFR1 rs9554320, T/T for VEGFR2 rs2071559, and T/T for eNOS rs2070744 were associated with a longer DFS with sunitinib versus placebo treatment. In addition, some SNPs demonstrated a potential trend toward prognostic value across treatment groups. The genotypes homozygous C/C of VEGFR1 rs9582036 and A/A of VEGFR1 rs9554320 showed trends toward longer DFS versus the heterozygous and other homozygous genotypes in the sunitinib, placebo, and combined treatment groups. For the VEGFR2 rs1870377 SNP, the only significant association was observed when both treatment groups were combined; the A/A genotype showed an association with shorter DFS versus the T/T genotype only. Despite differences in baseline demographics, the effect of sunitinib treatment on DFS in the pharmacogenomic analysis cohort was similar to that overall S-TRAC population (HR 0.74; 95% CI, 0.51–1.07; P = 0.107), with median DFS of 7.07 years and 5.56 years for sunitinib and placebo, respectively. With a limited number of OS events, there were no significant associations between SNP genotype and OS for sunitinib versus placebo. Still, for OS and genotypes within each treatment group and in the combined group, the genotype ‘−/−’ (i.e. , no insertion) of CCDC26 rs60315789 showed a trend towards longer OS versus the heterozygous −/TAT genotype in the sunitinib and placebo groups. A significant association was observed when the treatment groups were combined.
In the Renal EFFECT study, patients with metastatic RCC demonstrated marginally significant interactions between two sunitinib treatment arms and VEGFR3 rs448012 for time-to-tumor progression, PFS, and OS; however, the study could not identify which treatment group had a significant association between genotype and the clinical outcome (28). The current analyses of patients in the adjuvant setting did not demonstrate any associations between efficacy and VEGFR3 with sunitinib versus placebo, although longer DFS was seen for sunitinib versus placebo treatment in patients with C/C for VEGFR1 rs9554320, T/T for VEGFR2 rs2071559, and T/T for eNOS rs2070744. Genetic polymorphism in eNOS rs2070744 has been previously identified as independently predicting a rise in blood pressure and/or development of severe hypertension, but not as a predictor of clinical outcome in sunitinib-treated patients with metastatic RCC (19, 30). A recent study has highlighted that endothelial nitric oxide synthase (eNOS) SNPs may have a role as predictive biomarkers for bevacizumab efficacy and toxicity in patients with metastatic colorectal carcinoma (31). Therefore, it will be necessary to explore the impact of eNOS, VEGFR1, VEGFR2, and VEGFR3 SNPs on clinical outcomes in different treatment arms in patients with RCC or other tumor types.
In the current analyses, some SNPs in VEGFR1, VEGFR2, and CCDC26 demonstrated potential for prognostic value in DFS or OS outcomes across treatment groups in the adjuvant setting. To date, certain VEGFR1 SNPs have been proposed as candidate prognostic biomarkers in patients with metastatic RCC (24, 25). In patients treated with first-line sunitinib, poorer response rate, PFS, and OS were observed in those with VEGFR1 rs9554320 A/A and rs9582036 C/C genotypes compared with more favorable genotypes (19, 24, 25). Dornbusch et al. also reported that poorer OS was observed in those with VEGFR1 rs9582036 C/C genotypes versus A/A and A/C genotypes in patients with metastatic RCC treated with first-line sunitinib (26). However, they did not report any associations between VEGFR1 rs9582036 and PFS or VEGFR1 rs9554320 and PFS or OS (26).
Furthermore, SNPs in the VEGFA (rs833061, rs699947, rs2010963, and rs3025039), VEGFR2 (rs2305948), and VEGFR3 (rs6877011, rs307826, and rs307821) genes have been associated with varying clinical outcomes in patients with metastatic RCC treated with sunitinib (19, 20, 27, 29). For example, significantly longer PFS and OS were observed in patients with the C/C or C/T genotype of VEGFA rs833061 compared with the T/T genotype; similar results were observed in patients with the A/A or A/C versus the C/C genotype of VEGFA rs699947 (29). In patients with metastatic RCC treated with axitinib, certain SNPs in the VEGFA gene were associated with improved OS (19, 32). In contrast, in the Renal EFFECT study, Motzer et al. could not identify associations of certain SNPs (VEGFA rs699947, VEGFA rs1570360, VEGFR3 rs448012, VEGFR3 rs307821, and VEGFR3 rs307826) with efficacy (PFS, OS, objective response, or time-to-tumor progression) (19, 33). The contrasting observations for the impact of VEGF and VEGFR SNPs on sunitinib efficacy in RCC highlight the need to confirm exploratory studies and the differences reported. Additionally, some of the observations in the adjuvant setting appear to be divergent from the observations reported in the metastatic setting. These analyses were exploratory and were limited by small sample sizes in some subgroup analyses; therefore, further validation in independent adjuvant studies are needed to confirm if these SNPs can predict those patients who are most likely to derive benefit from adjuvant sunitinib treatment. Investigation into the association of SNPs and OS in the adjuvant setting would be of value; however, conservative estimates suggest that a suitably powered trial would require approximately 1650 patients with a follow-up of 18.5 years to demonstrate a substantial impact on OS (13). Patients in the S-TRAC trial were followed-up for an additional year to further assess OS; however, only 16 additional events in the intent-to-treat population occurred between the data cut-off date and the final OS follow-up and data remained immature. Further analyses would therefore not be expected to provide additional insight. In lieu of mature OS data and given the clinical need, DFS can be considered a suitable endpoint, especially where survival may be prolonged. The importance of DFS as an endpoint is recognized by the FDA and formed the primary basis for the approval of other adjuvant therapies including colon cancer and hormonal and cytotoxic breast cancer therapies (34). Finally, additional analyses in the adjuvant setting should also address whether the frequency and outcomes associated with the identified SNPs are consistent across a more diverse range of ethnic groups.
CONCLUSIONS
Correlations between SNPs in VEGFR1, VEGFR2, and eNOS genes and improved DFS in the sunitinib compared with placebo groups support the hypothesis that germline SNPs could have potential predictive value to identify patients who might derive more benefit from adjuvant sunitinib. Additionally, SNPs in VEGFR1, VEGFR2, and CCDC26 demonstrated a potential trend toward prognostic value for either DFS or OS across treatment groups. Further independent validation studies are necessary to confirm the potential predictive and prognostic value of these SNPs in the adjuvant setting.
Supplementary Material
ACKNOWLEDGEMENTS
This study was sponsored by Pfizer. Patients treated at Memorial Sloan Kettering Cancer Center were supported in part by Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748). The authors thank Patients in the S-TRAC trial who provided blood samples for analytical purposes. They acknowledge the following investigators who were also involved in the study: Yen-Hwa Chang, Jan Breza, Jean-Jacques Patard, and Giacomo Carteni. They also acknowledge the contribution of the following individuals at Pfizer: Linda Wood, Jean-Claude Marshall for their assistance with laboratory study execution and review of the article, and Cheyenne Bolanos and Lea Harty for biospecimens reconciliation and informed consent review. Medical writing support was provided by Anne Marie McGonigal, PhD, of Engage Scientific Solutions and was funded by Pfizer Inc.
Financial support
This study was sponsored by Pfizer. Patients treated at Memorial Sloan Kettering Cancer Center were supported in part by Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748).
• Dr George receives honoraria & consulting: Sanofi, Exelixis, Bayer; consulting: Merck, Sanofi; grants: Genentech/Roche, Novartis, Astellas, Celldex, Acerta; grants & consulting: Exelixis, Janssen, Pfizer, Innocrin Pharma, Bristol-Myers Squibb.
• Dr Staehler receives grant support and fees for serving on advisory boards for Pfizer, GlaxoSmithKline, Novartis, Bayer, Exelixis, and Roche; and consulting fees, honoraria, and travel support from Pfizer, GlaxoSmithKline, Novartis, Bayer, and Roche.
• Dr Motzer receives consulting fees from Pfizer, Eisai, Novartis, Acceleron, and Exelixis; and clinical trial support to his institution from Pfizer, Eisai, Novartis, Bristol-Myers Squibb, Genentech/Roche, GlaxoSmithKline, and Exelixis.
• Dr Magheli receives fees for serving on an advisory board for Ipsen Pharma; and lecture fees from Pfizer, Astellas, Janssen, and Ipsen Pharma.
• Dr Donskov receives grant support from Novartis, Pfizer, and Ipsen.
• Dr Escudier receives fees for serving on advisory boards from Pfizer, Novartis, Bristol-Myers Squibb, Exelixis, and Roche; and lecture fees from Pfizer and Novartis.
• Dr Laguerre receives honoraria from Pfizer.
• Dr Pantuck receives fees for consulting from Pfizer.
• Dr Pandha receives fees for serving on advisory boards for Ipsen and Eisai.
• Dr Patel receives fees for consulting and serving on a steering committee from Pfizer.
• Dr Ravaud receives fees for serving on advisory boards from Pfizer, Novartis, GlaxoSmithKline, Bristol-Myers Squibb, and Roche; lecture fees from Pfizer, Novartis, and GlaxoSmithKline; travel support from Pfizer, Novartis, GlaxoSmithKline, Bristol-Myers Squibb, and Merck Sharp & Dohme; and grant support from Pfizer and Novartis.
• Drs Martini, Li, Casey, Valota, and Lechuga are employees of Pfizer.
Abbreviations:
- CCDC26
coiled-coil domain-containing protein 26
- CI
confidence interval
- DFS
disease-free survival
- eNOS
endothelial nitric oxide synthase
- HR
Hazard ratio
- OS
overall survival
- PFS
progression-free survival
- RCC
renal cell carcinoma
- SINE
short interspersed nuclear elements
- SNPs
single nucleotide polymorphisms
- TNM
tumor, lymph nodes, metastasis
- UISS
University of California Los Angeles Integrated Staging System
- VEGF
vascular endothelial growth factor
- VEGFR
VEGF receptors
Footnotes
DATA SHARING STATEMENT
Upon request, and subject to certain criteria, conditions and exceptions (see https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information), Pfizer will provide access to individual de-identified participant data from Pfizer-sponsored global interventional clinical studies conducted for medicines, vaccines and medical devices (1) for indications that have been approved in the US and/or EU or (2) in programs that have been terminated (i.e., development for all indications has been discontinued). Pfizer will also consider requests for the protocol, data dictionary, and statistical analysis plan. Data may be requested from Pfizer trials 24 months after study completion. The de-identified participant data will be made available to researchers whose proposals meet the research criteria and other conditions, and for which an exception does not apply, via a secure portal. To gain access, data requestors must enter into a data access agreement with Pfizer.
REFERENCES
- 1.National Cancer Institute, Surveillance Epidemiology and End Results (SEER) Program. Cancer stat facts: kidney and renal pelvis cancer (2016) National Cancer Institute; Available from: https://seer.cancer.gov/statfacts/html/kidrp.html. [Google Scholar]
- 2.Smittenaar CR, Petersen KA, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer 2016;115:1147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsui KH, Shvarts O, Smith RB, Figlin RA, deKernion JB, Belldegrun A. Prognostic indicators for renal cell carcinoma: a multivariate analysis of 643 patients using the revised 1997 TNM staging criteria. J Urol 2000;163:1090–5; quiz 295. [DOI] [PubMed] [Google Scholar]
- 4.George DJ, Martini JF, Staehler M, Motzer RJ, Magheli A, Escudier B, et al. Immune biomarkers predictive for disease-free survival with adjuvant sunitinib in high-risk locoregional renal cell carcinoma: from randomized phase III S-TRAC study. Clin Cancer Res 2018. doi: 10.1158/1078-0432.CCR-17-2822. [DOI] [PubMed] [Google Scholar]
- 5.Rini B, Escudier B, Martini JF, Magheli A, Svedman C, Lopatin M, et al. Validation of the 16-Gene Recurrence Score in patients with locoregional, high-risk renal cell carcinoma from a phase 3 trial of adjuvant sunitinib. Clin Cancer Res 2018;In press. [DOI] [PubMed] [Google Scholar]
- 6.Zisman A, Pantuck AJ, Dorey F, Said JW, Shvarts O, Quintana D, et al. Improved prognostication of renal cell carcinoma using an integrated staging system. J Clin Oncol 2001;19:1649–57. [DOI] [PubMed] [Google Scholar]
- 7.Leibovich BC, Blute ML, Cheville JC, Lohse CM, Frank I, Kwon ED, et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer 2003;97:1663–71. [DOI] [PubMed] [Google Scholar]
- 8.Sorbellini M, Kattan MW, Snyder ME, Reuter V, Motzer R, Goetzl M, et al. A postoperative prognostic nomogram predicting recurrence for patients with conventional clear cell renal cell carcinoma. J Urol 2005;173:48–51. [DOI] [PubMed] [Google Scholar]
- 9.Lam JS, Shvarts O, Leppert JT, Pantuck AJ, Figlin RA, Belldegrun AS. Postoperative surveillance protocol for patients with localized and locally advanced renal cell carcinoma based on a validated prognostic nomogram and risk group stratification system. J Urol 2005;174:466–72; discussion 72; quiz 801. [DOI] [PubMed] [Google Scholar]
- 10.Patard JJ, Kim HL, Lam JS, Dorey FJ, Pantuck AJ, Zisman A, et al. Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: an international multicenter study. J Clin Oncol 2004;22:3316–22. [DOI] [PubMed] [Google Scholar]
- 11.Pfizer Inc. Highlights of prescribing information: Sutent (2017) US Food and Drug Administration; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021938s033lbl.pdf. [Google Scholar]
- 12.Ravaud A, Motzer RJ, Pandha HS, George DJ, Pantuck AJ, Patel A, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med 2016;375:2246–54. [DOI] [PubMed] [Google Scholar]
- 13.Motzer RJ, Ravaud A, Patard JJ, Pandha HS, George DJ, Patel A, et al. Adjuvant sunitinib for high-risk renal cell carcinoma after nephrectomy: subgroup analyses and updated overall survival results. Eur Urol 2018;73:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erichsen HC, Chanock SJ. SNPs in cancer research and treatment. Br J Cancer 2004;90:747–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Apellaniz-Ruiz M, Diekstra MH, Roldan JM, Boven E, Castellano D, Gelderblom H, et al. Evaluation of KDR rs34231037 as a predictor of sunitinib efficacy in patients with metastatic renal cell carcinoma. Pharmacogenet Genomics 2017;27:227–31. [DOI] [PubMed] [Google Scholar]
- 16.Diekstra MH, Fritsch A, Kanefendt F, Swen JJ, Moes D, Sorgel F, et al. Population modeling integrating pharmacokinetics, pharmacodynamics, pharmacogenetics, and clinical outcome in patients with sunitinib-treated cancer. CPT Pharmacometrics Syst Pharmacol 2017;6:604–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diekstra MH, Liu X, Swen JJ, Boven E, Castellano D, Gelderblom H, et al. Association of single nucleotide polymorphisms in IL8 and IL13 with sunitinib-induced toxicity in patients with metastatic renal cell carcinoma. Eur J Clin Pharmacol 2015;71:1477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diekstra MH, Swen JJ, Boven E, Castellano D, Gelderblom H, Mathijssen RH, et al. CYP3A5 and ABCB1 polymorphisms as predictors for sunitinib outcome in metastatic renal cell carcinoma. Eur Urol 2015;68:621–9. [DOI] [PubMed] [Google Scholar]
- 19.Diekstra MH, Swen JJ, Gelderblom H, Guchelaar HJ. A decade of pharmacogenomics research on tyrosine kinase inhibitors in metastatic renal cell cancer: a systematic review. Expert Rev Mol Diagn 2016;16:605–18. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Donas J, Esteban E, Leandro-Garcia LJ, Castellano DE, del Alba AG, Climent MA, et al. Single nucleotide polymorphism associations with response and toxic effects in patients with advanced renal-cell carcinoma treated with first-line sunitinib: a multicentre, observational, prospective study. Lancet Oncol 2011;12:1143–50. [DOI] [PubMed] [Google Scholar]
- 21.van der Veldt AA, Eechoute K, Gelderblom H, Gietema J, Guchelaar HJ, van Erp NP, et al. Genetic polymorphisms associated with a prolonged progression-free survival in patients with metastatic renal cell cancer treated with sunitinib. Clin Cancer Res 2011;17:620–9. [DOI] [PubMed] [Google Scholar]
- 22.van der Zanden LFM, Vermeulen SH, Oskarsdottir A, Maurits JSF, Diekstra MHM, Ambert V, et al. Description of the EuroTARGET cohort: A European collaborative project on TArgeted therapy in renal cell cancer-GEnetic- and tumor-related biomarkers for response and toxicity. Urol Oncol 2017;35:529 e9–e16. [DOI] [PubMed] [Google Scholar]
- 23.Xu CF, Bing NX, Ball HA, Rajagopalan D, Sternberg CN, Hutson TE, et al. Pazopanib efficacy in renal cell carcinoma: evidence for predictive genetic markers in angiogenesis-related and exposure-related genes. J Clin Oncol 2011;29:2557–64. [DOI] [PubMed] [Google Scholar]
- 24.Beuselinck B, Jean-Baptiste J, Schoffski P, Couchy G, Meiller C, Rolland F, et al. Validation of VEGFR1 rs9582036 as predictive biomarker in metastatic clear-cell renal cell carcinoma patients treated with sunitinib. BJU Int 2016;118:890–901. [DOI] [PubMed] [Google Scholar]
- 25.Beuselinck B, Karadimou A, Lambrechts D, Claes B, Wolter P, Couchy G, et al. VEGFR1 single nucleotide polymorphisms associated with outcome in patients with metastatic renal cell carcinoma treated with sunitinib - a multicentric retrospective analysis. Acta Oncol 2014;53:103–12. [DOI] [PubMed] [Google Scholar]
- 26.Dornbusch J, Walter M, Gottschalk A, Obaje A, Junker K, Ohlmann CH, et al. Evaluation of polymorphisms in angiogenesis-related genes as predictive and prognostic markers for sunitinib-treated metastatic renal cell carcinoma patients. J Cancer Res Clin Oncol 2016;142:1171–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim HR, Park HS, Kwon WS, Lee JH, Tanigawara Y, Lim SM, et al. Pharmacogenetic determinants associated with sunitinib-induced toxicity and ethnic difference in Korean metastatic renal cell carcinoma patients. Cancer Chemother Pharmacol 2013;72:825–35. [DOI] [PubMed] [Google Scholar]
- 28.Motzer RJ, Hutson TE, Hudes GR, Figlin RA, Martini JF, English PA, et al. Investigation of novel circulating proteins, germ line single-nucleotide polymorphisms, and molecular tumor markers as potential efficacy biomarkers of first-line sunitinib therapy for advanced renal cell carcinoma. Cancer Chemother Pharmacol 2014;74:739–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scartozzi M, Bianconi M, Faloppi L, Loretelli C, Bittoni A, Del Prete M, et al. VEGF and VEGFR polymorphisms affect clinical outcome in advanced renal cell carcinoma patients receiving first-line sunitinib. Br J Cancer 2013;108:1126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eechoute K, van der Veldt AA, Oosting S, Kappers MH, Wessels JA, Gelderblom H, et al. Polymorphisms in endothelial nitric oxide synthase (eNOS) and vascular endothelial growth factor (VEGF) predict sunitinib-induced hypertension. Clin Pharmacol Ther 2012;92:503–10. [DOI] [PubMed] [Google Scholar]
- 31.Di Salvatore M, Pietrantonio F, Orlandi A, Del Re M, Berenato R, Rossi E, et al. IL-8 and eNOS polymorphisms predict bevacizumab-based first line treatment outcomes in RAS mutant metastatic colorectal cancer patients. Oncotarget 2017;8:16887–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Escudier B, Rini BI, Motzer RJ, Tarazi J, Kim S, Huang X, et al. Genotype correlations with blood pressure and efficacy from a randomized phase III trial of second-line axitinib versus sorafenib in metastatic renal cell carcinoma. Clin Genitourin Cancer 2015;13:328–37 e3. [DOI] [PubMed] [Google Scholar]
- 33.Motzer RJ, Figlin RA, Martini JF, Hariharan S, Agarwal N, Li CX, et al. Germline genetic biomarkers of sunitinib efficacy in advanced renal cell carcinoma: results from the RENAL EFFECT trial. Clin Genitourin Cancer 2017;15:526–33. [DOI] [PubMed] [Google Scholar]
- 34.US Food and Drug Administration. Clinical Trial Endpoints for the Approval of Cancer Drugs and Biologics (2007). Available from: https://www.fda.gov/downloads/drugsGuidanceComplianceRegulatoyInformation/Guidance/UCM071590.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.