Abstract
Background:
Advances in the technology for percutaneous coronary angioplasty, such as coated stents, have reduced its complications, but restenosis remains an important clinical problem. The factors associated with an increased risk of restenosis include diabetes mellitus and multiple coronary artery disease. It is also possible that genetic factors play a role in restenosis although there are little data on this. We have investigated the association of three genetic markers of genes involved in inflammation leading to restenosis.
Materials and Methods:
In this case–control study, 306 unrelated Iranian patients who were thought to have restenosis on clinical grounds were investigated. Based on the results of angiography, 104 patients were found to have >50% stenosis within an implanted stent, and these were allocated to the in-stent restenosis (ISR) group; 202 patients with no in-stent stenosis or stenosis ≤50% were allocated to the non-ISR (NISR) group. Demographic data were collected from medical records. Biochemical parameters were measured using routine methods. Genotypes of the interleukin-10 (IL-10), annexin A5 (AnxA5), and tumor necrosis factor-alpha (TNFα) loci were determined using real-time polymerase chain reaction and a high-resolution melting assay.
Results:
Fasting blood glucose, serum triglycerides, and serum high-sensitivity C-reactive protein (hs-CRP) concentrations were higher in the ISR group than in the NISR group (P < 0.05), and a history of diabetes mellitus was significantly related to the presence of restenosis (P < 0.001). There were no significant differences in the frequency of the genetic polymorphisms of IL-10, AnxA5, and TNFα genes and the presence of ISR.
Conclusion:
After adjustment for clinical variables, the genetic polymorphisms at the IL-10, TNFα, and ANXA5 gene loci do not appear to be risk factors for >50% ISR in our population. However, our data suggested a significant association between diabetes mellitus, serum hs-CRP, stent type, and restenosis.
Keywords: Annexin A5, in-stent restenosis, interleukin-10, single-nucleotide polymorphism, tumor-necrotizing factor
INTRODUCTION
Coronary angioplasty has successfully reduced the numbers of patients requiring coronary artery bypass graft surgery.[1,2] However, recurrent disease or restenosis has been reported to occur in 15%–40% of cases after angioplasty.[3,4] Despite the placement of a stent following angioplasty, in-stent restenosis (ISR) remains an important clinical problem in interventional cardiology, with a prevalence of 15%–27%.[5,6]
Angiographic restenosis is defined by stenosis of >50% of the lumen of the artery, usually several months after percutaneous coronary intervention (PCI). Clinical stenosis is defined by the return of angina pectoris and the need for revascularization. Approximately, half of the patients who have angiographic restenosis do not have clinical symptoms.[7,8,9]
Approximately $1.6 billion per annum is spent for the treatment of restenosis in the US.[10] Because of the cost and complexity of repeated angioplasty, identifying those at risk of restenosis may be of clinical utility, by allowing the selection of the best management, for example, the use of drug-eluted stents exclusively or coronary artery bypass surgery.[10,11]
Most previous studies have investigated the use of biomarkers, clinical characteristics, and procedural aspects of angioplasty, but these have failed to identify high-risk individuals, apart from the presence of diabetes mellitus and multiple coronary artery disease. It is possible that genetic factors play an important role in restenosis.[12,13]
The insertion of stent in coronary artery induces an inflammation response. A systematic review analyzed the pathways of genes associated with restenosis (derived from genome-wide association studies [GWAS]) and revealed that 50% of these pathways were associated with inflammation, 25% related to proliferation, and 10% related to vascular function.[14]
Considering the likely importance of inflammation in restenosis, the goal of this current study was to investigate the frequency of polymorphisms of genes (interleukin 10 [IL-10], tumor necrosis factor-alpha [TNFα], annexin A5 [ANXA5]) that are involved in this process and were related to restenosis in GWAS or candidate gene studies.
Identification of risk factors associated with restenosis is useful in risk assessment of these patients and may also help to selection tailored therapy.
MATERIALS AND METHODS
Study design and population
In this case–control study, 306 unrelated Iranian patients who underwent elective PCI from Isfahan province were recruited between December 2014 and April 2017. The Scientific Ethics Committee of the Medical University of Mashhad, Iran, approved the study protocol (2015/930834), and all patients provided written informed consent.
The criteria used for selection of patients were as follows: patients were referred for re-angiography because of chest pain, equivalent symptoms such as dyspnea on exertion, and positive results of noninvasive cardiac tests after angioplasty. Based on the results of angiography, 104 patients who had >50% stenosis within an implanted stent between 1 month and 1 year after angioplasty (restenosis interval) were placed in the ISR group and 202 patients who had no in-stent stenosis or ≤50% stenosis in implanted stent were placed in the non-ISR (NISR) control group.
Demographic data including sex, age, smoking history, drug history, history of diabetes, hypertension, dyslipidemia, blood pressure, body weight, and height were collected from medical records. Patients with primary PCI, restenosis in the 1st month after angioplasty due to thrombosis, autoimmune disorder, active cancer, thrombophilia, or chronic kidney disease were excluded from the study.
Blood samples were taken before the procedure into ethylenediaminetetraacetic acid (EDTA) tubes for DNA extraction and into a tube with no anticoagulant for biochemistry markers.
Serum was separated by centrifuging the blood for 15 min at 1000 rpm speed (manufacturer's recommended speed). Serum was stored at −80°C and serum high-sensitivity C-reactive protein (hs-CRP) was measured using an enzyme immunoassay kit purchased from Diagnostics Biochem Canada Inc. Fasting blood glucose (FBG), triglycerides (TGs), total cholesterol (TC), and high-density lipoprotein were measured using Pars Azmoon kits on BT-3000 autoanalyzer. Low-density lipoprotein was calculated using the Friedewald formula.
Body mass index (kg/m2) was calculated by dividing the weight (kg) on square of the body height (m).
Genotyping
DNA was extracted from EDTA blood, using a genomic DNA isolation kit (Genet bio, Korea) based on the manufacturer's instructions. Purity and DNA quantification were recognized by ultraviolet spectrophotometry (Infinite 200 PRO NanoQuant, Tecan).
We genotyped single-nucleotide polymorphisms (SNPs) of three genes: IL-10, TNFα, and ANXA5 using real-time polymerase chain reaction (PCR) and high-resolution melting (HRM) assay (Light Cycler 96 System, Roche, Germany). We used “no template” controls to evaluate the contamination. The condition for real-time PCR and HRM was as follows: preincubation 1 Cycles: 95°C for 900 s; 3 Step amplification, 45 Cycles: 95°C for 15 s, 60°C for 20 s, 72°C for 20 s; HRM, 1 Cycles: 95°C for 60 s, 40°C for 60 s, 65°C for 1 s, 97°C for 1 s continuous; cooling, 1 Cycles: 40°C for 10 s.
We confirmed genotyping by sequencing of 10% of the templates. Data were analyzed using Light Cycler 96 System, Roche, Germany, Application Software.
Statistical analysis
Chi-square tests were used to assess agreement of genotypes with the Hardy–Weinberg equilibrium. The association between IL-10, TNFα, and ANXA5 polymorphisms and restenosis was calculated by the odds ratio (OR) with 95% confidence interval (CI).
Continuous variables were reported as mean ± standard deviation and categorical variables were expressed as percentage. Univariate and multivariate analysis was done with binary logistic regression and was expressed in OR (95% CI). All analyses were performed by the SPSS software (Chicago, IL, USA) version 20, and P < 0.05 was considered statistically significant.
Restenosis interval was defined as the time from stent insertion to angiographic diagnosis of ISR.
RESULTS
Baseline clinical findings and demographic and laboratory data are shown in Table 1.
Table 1.
Baseline findings in relation with nonin-stent restenosis and in-stent restenosis
| Variables | NISR (202) | ISR (104) | P |
|---|---|---|---|
| Age (years) | 62.2±9.2 | 60.8±8.4 | 0.196 |
| Sex, n (%) | |||
| Male | 138 (68.3) | 77 (74.8) | 0.101 |
| Female | 64 (31.7) | 26 (25.2) | |
| Hypertension, n (%) | 131 (70.4) | 55 (52.9) | 0.051 |
| Diabetes mellitus, n (%) | 70 (34.7) | 63 (60.6) | <0.001 |
| Positive smoking habit, n (%) | 33 (16.7) | 13 (13.0) | 0.271 |
| Statin consumption, n (%) | 185 (94.4) | 93 (95.9) | 0.235 |
| Aspirin consumption, n (%) | 187 (95.4) | 94 (95.9) | 0.305 |
| Clopidogrel consumption, n (%) | 171 (87.7) | 88 (90.7) | 0.234 |
| Stent type, n (%) | |||
| Bare | 51 (39.5) | 38 (60.3) | 0.005 |
| Drug eluting | 78 (60.5) | 25 (39.7) | |
| SBP (mean±SD) | 125.4±16.6 | 123.2±12.5 | 0.352 |
| DBP (mean±SD) | 77.4±8.8 | 78±7.9 | 0.377 |
| FBG (mg/l) | 109.9±57.0 | 126.5±66.9 | 0.038 |
| TG (mg/l) | 108 (79-146) | 127 (78.5-192.5) | 0.039 |
| TC (mg/l) | 148.9±39.8 | 153.7±41.2 | 0.347 |
| LDL (mg/l) | 89.3±32.0 | 88.3±30.3 | 0.807 |
| HDL (mg/l) | 35.7±10.7 | 35±8.4 | 0.581 |
| hs-CRP (mg/l) | 2.3 (1.3-4.2) | 3.46 (1.8-7.8) | 0.006 |
| BMI (kg/m2), n (%) | |||
| Normal | 72 (39.3) | 29 (31.5) | 0.333 |
| Overweight | 85 (46.4) | 45 (48.9) | |
| Obese | 26 (14.2) | 18 (19.6) | |
| Restenosis interval (months) | 36.00 (12.00-60.00) | 6.00 (4.00-8.00) | <0.001 |
SBP=Systolic blood pressure; DBP=Diastolic blood pressure; FBG=Fasting blood glucose; TG=Triglyceride; TC=Total cholesterol; HDL=High-density lipoprotein; LDL=Low-density lipoprotein; hs-CRP=High sensitivity C-reactive protein; BMI=Body mass index; NISR=Nonin-stent restenosis; ISR=In-stent restenosis; SD=Standard deviation
FBG, serum TG, and serum hs-CRP levels were higher in the ISR cases than in the NISR cases (P < 0.05), and a positive history of diabetes mellitus was significantly related to the presence of restenosis (P < 0.001).
The bioactive agents used in drug-eluting stents reduce inflammation and smooth muscle cell proliferation and migration and consequently reduce the risk of restenosis. Patients treated with a bare-metal stent had a greater risk of restenosis in interval time between 1 month and 1 year after stent insertion than those treated with a drug-eluting stent (P = 0.005).
HRM genotyping results were determined using a Light Cycler 96 System, Roche, Germany software [Figures 1 and 2].
Figure 1.
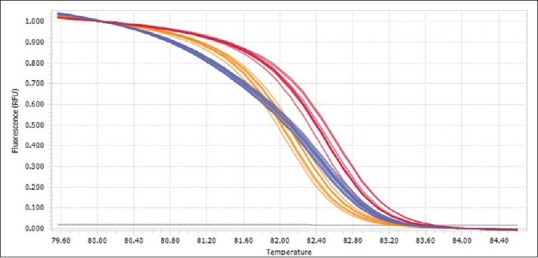
Normalized melting curves following analysis of HRM data for the IL10 SNP (A/C).  Homozygote C/C
Homozygote C/C  Heterozygote A/C
Heterozygote A/C  Homozygote A/A
Homozygote A/A
Figure 2.
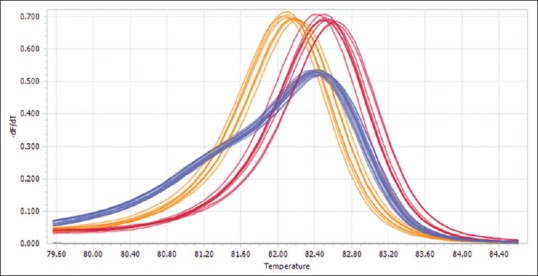
Normalized melting peaks following analysis of HRM data for the IL10 SNP (A/C).  Homozygote C/C
Homozygote C/C  Heterozygote A/C
Heterozygote A/C  Homozygote A/A
Homozygote A/A
A Chi-square test was used to assess the agreement of genotypes with the Hardy–Weinberg equilibrium, and there was no deviation from this for all three genotypes (P > 0.05).
Based on SPSS analysis, allele frequencies were 0.66/0.44, 0.92/0.08, and 0.40/0.60 for IL-10-592C/A, TNFα-238G/A, and ANXA5-1247T/C, respectively. In a genetic association study on SNP with two alleles, patients have three genotypes. For ANXA5 polymorphism, patients had CC, TC, and TT genotypes. T allele was more common in ISR group and may be susceptibility allele. We examined following genetic models: dominant model (TT + TC vs. CC), recessive model (TT vs. TC + CC), and additive model (TT vs. CC) and also for other two polymorphisms (IL-10 and TNFα). The most appropriate genetic models were dominant, recessive, and recessive for IL-10, TNFα, and ANXA5 SNPs, respectively [Table 2].
Table 2.
Distributions of interleukin-10, annexin A5, and tumor necrosis factor-alpha polymorphisms in association with in-stent restenosis using univariate logistic regression analysis
| Polymorphisms | Minor allele frequency | Genetic model | OR | 95% CI | P |
|---|---|---|---|---|---|
| IL-10-592C/A | 0.44 | Dominant | 1.591 | 0.627-3.785 | 0.32 |
| TNFα-238G/A | 0.08 | Recessive | 1.44 | 0.724-2.754 | 0.29 |
| ANXA5-1247T/C | 0.40 | Recessive | 1.723 | 1.039-2.883 | 0.03 |
IL-10=Interleukin-10; TNFα=Tumor necrosis factor-alpha; ANXA5=Annexin A5; OR=Odds ratio; CI=Confidence interval
Initially, associations between different genotypes and restenosis were assessed using univariate logistic regression analysis without adjusting for other variants. There was a significant association between the ANXA5 SNP and restenosis (OR: 1.72, 95% CI: 1.02–2.88, P = 0.03) but no other SNPs [Table 2]. In the final multiple logistic regression analysis with correction for covariates, there were no significant differences between the NISR and ISR groups for genotype distribution [Table 3].
Table 3.
Comparison of interleukin-10, annexin A5, and tumor necrosis factor-alpha polymorphism genotype between nonin-stent restenosis and in-stent restenosis groups using multiple logistic regression analysis
| Gene/polymorphisms | Allele | NISR (n=180) | ISR (n=93) | OR | 95% CI | P | |
|---|---|---|---|---|---|---|---|
| IL10/rs1800872 | CC | 79 | 40 | Reference=1 | |||
| AC | 79 | 46 | 0.933 | 0.511-1.594 | 0.864 | ||
| AA | 22 | 7 | 0.842 | 0.239-2.061 | 0.790 | ||
| TNFα/rs361525 | GG | 154 | 74 | Reference=1 | |||
| AG | 25 | 18 | 0.505 | 0.197-1.294 | 0.155 | ||
| AA | 1 | 1 | |||||
| AnxA5/rs6830321 | CC | 34 | 13 | Reference=1 | |||
| TC | 87 | 37 | 0.577 | 0.166-2.014 | 0.389 | ||
| TT | 59 | 43 | 0.476 | 0.134-1.686 | 0.250 | ||
OR=Odds ratio; CI=Confidence interval; IL-10=Interleukin-10; TNFα=Tumor necrosis factor-alpha; ANXA5=Annexin A5; NISR=Non in-stent restenosis; ISR=In-stent restenosiss
DISCUSSION
Angioplasty and stent implantation are associated with an inflammatory response because of the mechanical disruption of the coronary artery wall, and this stimulates smooth muscle cell migration and proliferation and finally neointimal hyperplasia.[15] Neointimal hyperplasia is the most common cause of ISR, and 50% of the pathways associated with restenosis are related to inflammatory genes.[14,16] hs-CRP is an inflammatory biomarker and the relationship between serum hs-CRP as an independent factor and coronary restenosis has been reported previously.[17,18,19]
Li et al. found in a meta-analysis study that high levels of serum CRP are accompanied by ISR, especially in patients with unstable angina.[20] In our study, after logistic regression model, serum hs-CRP level was associated with ISR as an independent predictor.
The most common clinical factor that is associated with risk of restenosis is diabetes mellitus, especially patients who are treated with insulin.[7] Endothelial dysfunction accompanies hyperglycemia, which is also a pro-inflammatory factor and increases production of cytokines and growth factors and consequently neointima formation.[21] We found that diabetes mellitus and high FBG is positively related to ISR.
Kundi et al. in a case–control study showed the relationship between high TG level and ISR.[22] In our study, TG level was associated with ISR.
Genetic factors play an important role in restenosis.[7,23] Polymorphisms in inflammatory-related genes have previously been reported to be associated with ISR.[24,25]
Some studies have shown that several polymorphisms in promoter region of the IL-10 and TNFα gene can regulate the transcription of genes and consequently affect restenosis. In a GWA study (the GENDER project), Monraats et al. showed an association between three polymorphisms including the rs1800872, rs1800871, and rs1800896 of the IL-10 gene and coronary restenosis and Martínez-Ríos et al. also reported a relationship between these polymorphisms and restenosis in the Mexican population.[26,27] In our study, we investigated the relationship between IL-10-592C/A (rs1800872) SNP and angiographic restenosis and there was no significant association.
Monraats et al. reported two polymorphisms −238G>A and −1031T>C in the TNF gene were associated with coronary restenosis.[27] However, Martínez-Ríos et al. and Koch et al. did not find an association between the −238G>A SNP and restenosis.[26,28] In our study, there was no significant association between TNFα −238G>A SNP and restenosis.
Ewing et al. found an association between rs4833229 and rs6830321 SNP in the ANXA5 gene and risk of restenosis.[29] Sampietro et al. also showed relationship between these polymorphisms and restenosis.[30] In our study, there was a significant association between the rs4833229 SNP in ANXA5 gene and restenosis in univariate logistic regression analysis, but there was no significant association in multiple logistic regression analysis.
CONCLUSION
After adjustment for clinical variables, the genetic polymorphisms at the IL-10, TNFα, and ANXA5 gene loci do not appear to be risk factors for ISR in our population. Our data suggest a significant association between diabetes mellitus, serum hs-CRP, and stent type with restenosis in logistic regression model and adjustment for other variables. Additional studies using a larger sample size are probably needed to evaluate the relationship of these polymorphisms and restenosis after coronary angioplasty.
Financial support and sponsorship
This study was supported by grants from Medical University of Isfahan (No: 1141292) and Medical University of Mashhad (No: 93570), Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr. Maracy, Ms. Sedghi, Ms. Gholamrezapour, Ms. Asadi and technicians of AL Zahra hospital's genetic laboratory and catheterization laboratory nurses of Sina Hospital, Iran.
REFERENCES
- 1.Bavry AA, Kumbhani DJ. Text book of complex coronary interventions. Indications and techniques of percutaneous procedures: Springer. 2012:17–23. [Google Scholar]
- 2.Sanei H NA, Bank H, Moshaveri F, Hosseini SM, Keshvari M, et al. Evaluation of Coronary Angioplasty Results in Patients Referring to Isfahan Cardiac Centers, Iran, and Comparing with Clinical Guidelines. J Isfahan Med Sch. 2017;35(443):1044–9. [Google Scholar]
- 3.Tsigkas GG, Karantalis V, Hahalis G, Alexopoulos D. Stent restenosis, pathophysiology and treatment options: A 2010 update. Hellenic J Cardiol. 2011;52:149–57. [PubMed] [Google Scholar]
- 4.Cassese S, Byrne RA, Tada T, Pinieck S, Joner M, Ibrahim T, et al. Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart. 2014;100:153–9. doi: 10.1136/heartjnl-2013-304933. [DOI] [PubMed] [Google Scholar]
- 5.Iqbal J, Gunn J, Serruys PW. Coronary stents: Historical development, current status and future directions. Br Med Bull. 2013;106:193–211. doi: 10.1093/bmb/ldt009. [DOI] [PubMed] [Google Scholar]
- 6.Valgimigli M, Campo G, Monti M, Vranckx P, Percoco G, Tumscitz C, et al. Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: A randomized multicenter trial. Circulation. 2012;125:2015–26. doi: 10.1161/CIRCULATIONAHA.111.071589. [DOI] [PubMed] [Google Scholar]
- 7.Jukema JW, Verschuren JJ, Ahmed TA, Quax PH. Restenosis after PCI. Part 1: Pathophysiology and risk factors. Nat Rev Cardiol. 2011;9:53–62. doi: 10.1038/nrcardio.2011.132. [DOI] [PubMed] [Google Scholar]
- 8.Scheller B, Clever YP, Kelsch B, Hehrlein C, Bocksch W, Rutsch W, et al. Long-term follow-up after treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. JACC Cardiovasc Interv. 2012;5:323–30. doi: 10.1016/j.jcin.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Hara H, Nakamura M, Palmaz JC, Schwartz RS. Role of stent design and coatings on restenosis and thrombosis. Adv Drug Deliv Rev. 2006;58:377–86. doi: 10.1016/j.addr.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 10.Weintraub WS. The pathophysiology and burden of restenosis. Am J Cardiol. 2007;100:3K–9K. doi: 10.1016/j.amjcard.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention. Circulation. 2011:CIR. 0b013e31823ba622. [Google Scholar]
- 12.Horibe H, Yamada Y, Ichihara S, Watarai M, Yanase M, Takemoto K, et al. Genetic risk for restenosis after coronary balloon angioplasty. Atherosclerosis. 2004;174:181–7. doi: 10.1016/j.atherosclerosis.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 13.Monraats PS, R P Agema W, Jukema JW. Genetic predictive factors in restenosis. Pathol Biol (Paris) 2004;52:186–95. doi: 10.1016/j.patbio.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Verschuren JJ, Trompet S, Sampietro ML, Heijmans BT, Koch W, Kastrati A, et al. Pathway analysis using genome-wide association study data for coronary restenosis – A potential role for the PARVB gene. PLoS One. 2013;8:e70676. doi: 10.1371/journal.pone.0070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simon DI. Inflammation and vascular injury: Basic discovery to drug development. Circ J. 2012;76:1811–8. doi: 10.1253/circj.cj-12-0801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Hoeven BL, Pires NM, Warda HM, Oemrawsingh PV, van Vlijmen BJ, Quax PH, et al. Drug-eluting stents: Results, promises and problems. Int J Cardiol. 2005;99:9–17. doi: 10.1016/j.ijcard.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Xu YL, Li JJ, Xu B, Zhu CG, Yang YJ, Chen JL, et al. Role of plasma C-reactive protein in predicting in-stent restenosis in patients with stable angina after coronary stenting. Chin Med J (Engl) 2011;124:845–50. [PubMed] [Google Scholar]
- 18.Niccoli G, Dato I, Imaeva AE, Antonazzo Panico R, Roberto M, Burzotta F, et al. Association between inflammatory biomarkers and in-stent restenosis tissue features: An optical coherence tomography study. Eur Heart J Cardiovasc Imaging. 2014;15:917–25. doi: 10.1093/ehjci/jeu035. [DOI] [PubMed] [Google Scholar]
- 19.Zurakowski A, Wojakowski W, Dzielski T, Milewski K, Gościńska-Bis K, Tendera M, et al. Plasma levels of C-reactive protein and interleukin-10 predict late coronary in-stent restenosis 6 months after elective stenting. Kardiol Pol. 2009;67:623–30. [PubMed] [Google Scholar]
- 20.Li JJ, Ren Y, Chen KJ, Yeung AC, Xu B, Ruan XM, et al. Impact of C-reactive protein on in-stent restenosis: A meta-analysis. Tex Heart Inst J. 2010;37:49–57. [PMC free article] [PubMed] [Google Scholar]
- 21.Aronson D, Edelman ER. Revascularization for coronary artery disease in diabetes mellitus: Angioplasty, stents and coronary artery bypass grafting. Rev Endocr Metab Disord. 2010;11:75–86. doi: 10.1007/s11154-010-9135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kundi H, Korkmaz A, Balun A, Cicekcioglu H, Kiziltunc E, Gursel K, et al. Is In-Stent Restenosis After a Successful Coronary Stent Implantation Due to Stable Angina Associated With TG/HDL-C Ratio Angiology. 2017;68(9):816–22. doi: 10.1177/0003319716689366. [DOI] [PubMed] [Google Scholar]
- 23.Monraats PS, Pires NM, Agema WR, Zwinderman AH, Schepers A, de Maat MP, et al. Genetic inflammatory factors predict restenosis after percutaneous coronary interventions. Circulation. 2005;112:2417–25. doi: 10.1161/CIRCULATIONAHA.105.536268. [DOI] [PubMed] [Google Scholar]
- 24.Osadnik T, Lekston A, Bujak K, Strzelczyk JK, Poloński L, Gąsior M, et al. The relationship between VEGFA and TGFB1 polymorphisms and target lesion revascularization after elective percutaneous coronary intervention. Dis Markers. 2017;2017:8165219. doi: 10.1155/2017/8165219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu W, Liu Y, Jiang H, Ding X, Zhu R, Li B, et al. Plasma levels of interleukin 18, interleukin 10, and matrix metalloproteinase-9 and -137G/C polymorphism of interleukin 18 are associated with incidence of in-stent restenosis after percutaneous coronary intervention. Inflammation. 2013;36:1129–35. doi: 10.1007/s10753-013-9647-6. [DOI] [PubMed] [Google Scholar]
- 26.Martínez-Ríos MA, Peña-Duque MA, Fragoso JM, Delgadillo-Rodríguez H, Rodríguez-Pérez JM, Miranda-Malpica E, et al. Tumor necrosis factor alpha and interleukin 10 promoter polymorphisms in mexican patients with restenosis after coronary stenting. Biochem Genet. 2009;47:707–16. doi: 10.1007/s10528-009-9268-9. [DOI] [PubMed] [Google Scholar]
- 27.Monraats PS, Pires NM, Schepers A, Agema WR, Boesten LS, de Vries MR, et al. Tumor necrosis factor-α plays an important role in restenosis development. FASEB J. 2005;19(14):1998–2004. doi: 10.1096/fj.05-4634com. [DOI] [PubMed] [Google Scholar]
- 28.Koch W, Tiroch K, von Beckerath N, Schömig A, Kastrati A. Tumor necrosis factor-alpha, lymphotoxin-alpha, and interleukin-10 gene polymorphisms and restenosis after coronary artery stenting. Cytokine. 2003;24:161–71. doi: 10.1016/j.cyto.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Ewing M, Verschuren J, Sampietro M, De Vries M, De Knijff P, Quax P, et al., editors. Eur Heart J. england: oxford univ press great clarendon st, oxford ox2 6dp; 2010. Annexin A5: genotypic risk marker for clinical restenosis after percutaneous coronary intervention. [Google Scholar]
- 30.Sampietro ML, Pons D, de Knijff P, Slagboom PE, Zwinderman A, Jukema JW, et al. A genome wide association analysis in the GENDER study. Neth Heart J. 2009;17:262–4. doi: 10.1007/BF03086261. [DOI] [PMC free article] [PubMed] [Google Scholar]


