Abstract
Background
Femoroacetabular Impingement (FAI) is becoming increasingly more common with noted impairments in physical function, increased pain, and decreased quality of life. Typically, a conservative approach is used through physical therapy or intra-articular injections before an invasive surgical approach is utilized. Identifying the proper course of conservative care by the clinician will aid in improving outcomes.
Purpose
The purpose of this systematic review and meta-analysis was to investigate short-term effects of conservative physical therapy and intra-articular injections on pain and physical function measures in patients with FAI.
Study Design
Systematic Review & Meta-Analysis.
Methods
A systematic review and meta-analysis were completed using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and registered with the International Prospective Registry of Systematic Reviews. A literature review was performed in May 2018 using Pubmed, CINAHL, Proquest, and Scopus. Inclusion criteria included humans classified as having femoroacetabular impingement, conservative rehabilitation, and utilization of outcome measures in the domains of pain or function. Exclusion criteria included absence of skilled interaction and study protocols that were not completed.
Results
Seven studies were included that summarized physical therapy or intra-articular injection outcomes for femoroacetabular impingement management. Results showed that conservative interventions for short-term periods are effective in reducing pain and improving function for femoroacetabular impingement. Overall, physical therapy revealed moderate to large effect sizes and statistically significant differences in both pain (SMD, 0.91, CI: 0.07, 1.76, p=0.030) and function (SMD, 0.80, CI: 0.34, 1.28, p=0.001) for femoroacetabular impingement. Intra-articular injection demonstrated small effect sizes for pain outcomes (SMD, 0.29, CI: -1.25, 1.83, p = 0.710) and small to moderate effect size for improvement in function (SMD, 0.49, CI: 0.03, 0.96, p = 0.040).
Conclusions
Physical therapy demonstrated positive results to self-reported pain and function and may hold more promise than intra-articular injection alone. Common treatments that were associated with improved outcomes were patient education, activity modification, manual therapy, and strengthening. There are a limited number of high-quality articles on this topic, which should be addressed in future research.
Level of Evidence
1a.
Keywords: conservative management, femoroacetabular impingement, pain, physical function, physical therapy
INTRODUCTION
Femoroacetabular Impingement (FAI) has been gaining more recognition over the last several years, especially in the younger athletic population. Femoroacetabular Impingement is a pathology caused by a bony adaptation or malformation of either the acetabulum, femoral head or both and is predominately seen in an athletic population with a higher prevalence in younger individuals, Caucasians, and females.1-3 When symptoms do become problematic, pain and decreased physical function are commonly noted. Common complaints of FAI are groin pain, pain with hip motions (especially hip flexion and internal rotation), activity limitations, and restricted range of motion.1,2
FAI can occur as a result of bony overgrowth of the femoral neck or the acetabulum resulting in structural abnormalities which cause friction between the joint structures and microtrauma to the labrum and cartilage.1,2 If left untreated, this pathology can lead to: labral avulsion, pain, chondral damage, and secondary osteoarthritis.2 The etiology for FAI is unclear; however, there are several theories including the presence of pediatric conditions, prior trauma to the femoral neck, genetic predisposition, and high intensity activities in adolescent years.1,2
This condition can cause a financial burden due to the costly imaging and interventions needed for diagnosis. Since the most effective medical management option for FAI is still under investigation, an individual often endures a myriad of interventions before relief of symptoms is experienced. Treatment options range from less invasive options, such as medications and physical therapy, to more invasive procedures including intra-articular injections and even surgical intervention. The utilization of multiple conservative treatment interventions may consume resources such as time, energy, and money potentially negatively impacting their quality of life. A study4 reported that the average amount spent on health care for a patient with FAI was $2,456.97; which includes visits with a primary care physician, medication, diagnosis of labral impairments, and conservative management; while a different study5 estimated the cost of hip arthroscopy surgery in patients with FAI to be $21,700.
Initially, the impairments associated with FAI are often addressed with conservative measures, including physical therapy and intra-articular injections. Current physical therapy practice for FAI has shifted away from stretching and passive range of motion (ROM), in favor of strengthening the hip flexors, gluteal muscles, and abdominals.6,7 Patient education on activity modification to avoid extreme ROM's that provoke patient's symptoms is another component of physical therapy practice.6,7
Intra-articular injections are more invasive forms of conservative management. Corticosteroids or hyaluronic acid injections are administered into the hip joint space to aid in pain relief.8 Khan et al.8 concluded that intra-articular hip injections could play a role in the diagnosis, treatment, and prognosis of FAI. However, the therapeutic benefits of intra-articular injections related to the short and long-term outcomes continue to be investigated.
FAI can lead to chronic and debilitating symptoms if left untreated.1,2,3 Identifying the most effective course of treatment early can not only improve the patient's quality of life, but could possibly prevent further financial burden. Therefore, the purpose of this systematic review and meta-analysis is to investigate short-term effects of conservative physical therapy and intra-articular injections on pain and physical function measures in patients with FAI.
METHODS
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines. PRISMA is a prospective 27-item checklist and 4-phase flow diagram utilized to aid author reporting in systematic reviews and meta-analyses.9 This manuscript was registered with the International Prospective Registry of Systematic Reviews (PROSPERO). PROSPERO is a database that prospectively evaluates systematic reviews in relation to the health outcomes for proper writing procedures and to prevent duplicity of published literature (#CRD42018084845).
Search Strategies
Search strategies for PubMed, CINAHL, ProQuest, and Scopus electronic databases were developed in May 2018. All databases were searched using a comprehensive strategy that included search terms related to conservative interventions for individuals with FAI. There were limits applied to: (1) Publication date of articles limited from 1999 to present based on FAI inception and prevalence of the term, (2) humans (3) English language, and (4) level of evidence higher than case studies to improve the quality of data synthesis. A hand search of completed Systematic Reviews on FAI was performed for inclusion of relevant articles. Grey literature searches were utilized through Clinical Trial sites and Google Scholar for thoroughness of article inclusion. The full Pubmed search strategy can be found in Appendix I.
Eligibility Requirement
Studies were considered for inclusion in this systematic review and meta-analysis based on the following characteristics: (1) humans classified as having FAI, (2) conservative rehabilitation management in the form of physical therapy and/or injections (3) utilization of an outcome measure in the domains of pain or function. Exclusion criteria consisted of: (1) no rehabilitation protocol, (2) cadaveric studies, (3) level of evidence lower than cohort study, (4) interventions that lacked skilled interaction by a licensed professional, (5) study protocols that were not completed.
Study Selection
Article titles and abstracts as well as full texts were each screened independently by two authors to look for relevant publications that satisfied inclusion and exclusion criteria. In cases of disagreement, the two authors discussed their differences and came to a final agreement about inclusion. At the end of both screens, an unweighted kappa score was calculated to determine the strength of agreement between the two reviewers.10 Kappa scores are interpreted as follows: κ < 0.00 is poor agreement, 0.00-0.20 slight, 0.21-0.40 fair, 0.41-0.60 moderate, 0.61-0.80 substantial, and 0.81-1.00 almost perfect agreement.11
Risk of Bias
The McGill Mixed Methods Appraisal Tool (MMAT) was used to assess the quality of the included articles. This tool includes two screening questions and five categories of mixed methods study component questions that are analyzed and given a response of “Yes”, “No”, or “Can't tell”. The appropriate category of questions is chosen based on study design to better inform the assessment of quality of included studies. Study design questions include qualitative, quantitative randomized controlled trials, quantitative non-randomized, quantitative descriptive, and mixed methods. Four questions are assessed, per appropriate section chosen, and are weighted equally at 25% intervals per ‘yes’ responses. The fifth section of the MMAT contains three questions for which every ‘no’ response yields an additional 25% to the total score. Scores can range from 0% to 100%. This tool is both a reliable and valid measure to interpret the quality of the included articles.12 Two authors independently assessed for risk of bias in the included articles. Where differences were present, both authors deliberated and came to a mutual conclusion on the methodological quality. An unweighted kappa with 95% confidence interval was calculated to assess strength of agreement and inter-rater reliability during the quality checklist assessment.10
Data Extraction and Analysis
Two individuals participated in data extraction. One individual selected the data while the other individual verified the selection for accuracy. The characteristics extracted from the included articles are as follows: (1) title, (2) author, (3) publication date, (4) study level of evidence, (5) population demographics (including age and gender), (6) study duration, (7) surgery, (8) rehabilitation intervention and frequency, (9) outcome measures utilized in each study and length of time between baseline and follow-up, (10) results of the outcome measures at base-line and follow-up including means and standard deviations, (11) quality assessment score, (12) effect size, (13) adherence rate.
Outcome/Summary Measures
Outcome measures included in this study were classified into either a pain or physical function domain. The outcomes are compared across studies and extracted to observe improvements of physical function and pain. Short-term outcomes are defined as changes in a patient's symptoms while receiving the intervention; consequently, this review defines short-term as measurements taken within the first six months of intervention.13
The pain outcome measures are the Visual Analogue Scale (VAS) and the Numerical Rating Scale (NRS). The VAS and NRS are unidimensional measures of pain intensity that are both reliable and valid.14,15 In both assessments, a higher score indicates greater pain intensity whereas a lower score indicates lower pain.14 The VAS scale is represented in varying forms such as an 11-point scale, 100-point scale, or a 10 cm visual reference, all of which are accepted forms of the VAS scale. Comparatively, the NRS is a self-report measure of pain intensity on a 11-point scale 0-10.14 In this study there were three outcome measures that had a similar study design to the NRS. The outcome tools were the Oral Numeric Scale (ORS), Numeric Pain Scale (NPS), and Numeric Pain Rating Scale (NPRS). Due to similarities in the measurements and design, the description of the NRS encompasses these tools.
Physical function outcome measures are the Hip Outcome Score (HOS), Harris Hip Score (HHS), and Hip Disability and Osteoarthritis Outcome Score (HOOS). The HOS is an instrument to assess self-reported functional status in the domains of activities of daily living (ADL) and sports related activities. The HOS scoring rates 100 being the patient's prior level of function and 0 being unable to perform the task. The HOS has shown to be reliable and valid in the research for acetabular labral tears.16 The HHS is both reliable and valid to assess pain, function, and range of motion following hip surgery.17 The score has a maximum of one hundred points, with a higher score representing an improved status. There are five subsections of this outcome measure: pain (one item, 0–44 points), function (seven items, 0–47 points), absence of deformity (one item, 4 points), and range of motion (two items, 5 points).17 The HOOS is an instrument to assess the patients’ opinion about their hip and associated disabilities for use in adults with and without osteoarthritis. This scale ranges from 0-100 with 0 indicating maximal disability and 100 indicating no symptoms. The HOOS has shown to be reliable and valid in the research for postoperative hip interventions.17
Meta-analyses were completed for self-reported pain and physical function using Comprehensive Meta-Analysis (Biostat; Englewood, NJ), Version 3. One study23 was not included in the meta-analyses due to a lack of reported statistical data. Both meta-analyses were completed using the standardized mean difference (SMD) as the summary measure of effect. SMD with 95% confidence intervals (CI) were used. I2 statistics were calculated in order to determine the level of heterogeneity between included studies. The I2 statistic is more useful than the Q test, which only indicates the presence versus absence of heterogeneity.18 Percentages used by Higgins and Thompson19 were utilized to quantify the magnitude of heterogeneity: 25% = low, 50% = medium, 75% = high heterogeneity. Utilizing the scale, if I2 was < 50%, a fixed effects model was used, and if the I2 was > 50%, a random effects model was used. Interpretation of effect size will be defined by the following scale: 0.2 as small, 0.5 as moderate, and 0.8 as large effect sizes.20
Risk of bias was assessed via funnel plot construction. A symmetrical funnel plot indicates low risk of publication bias, whereas an asymmetrical funnel plot indicates a higher risk of publication bias.21
RESULTS
Study selection
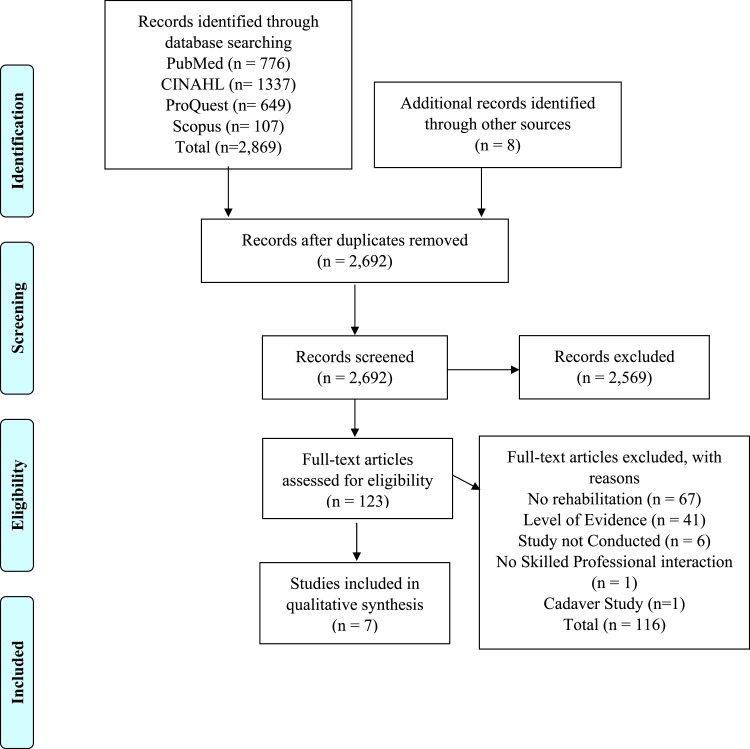
This study identified 2,877 titles, with eight located through hand searches and 2,869 through databases. Overall the search provided 2,692 studies after the removal of duplicates. After the title and abstract screen, 123 full text studies were assessed, and 116 studies were excluded because they did not meet the inclusion criteria. The remaining seven studies22-28 were included in the systematic review and meta-analysis. Screening of titles and abstracts as well as full texts resulted in substantial agreement between the reviewers with κ = 0.72, (95% CI, 0.65-0.78) and κ = 0.79 (95% CI, 0.62-0.95) respectively. Refer to Figure 1 for the study selection process.
Figure 1.
PRISMA Flow Diagram.
Risk of Bias within Individual Studies
The seven studies22-28 were evaluated using the Mixed Methods Appraisal Tool with κ = 0.55 (95% CI, 0.18-0.90) demonstrating moderate agreement between reviewers.11 Scores ranged from lower quality (25%) to higher quality (100%). Five studies22-24,26,27 were determined to have moderate to high risk of bias due to unclear descriptions of overall outcomes, considerations on how the findings relate to context and researchers’ influence, or consideration on limitations of the studies. Quality assessment scoring is summarized in Table 1.
Table 1.
Methodological Quality of Included Studies – Mixed Methods Appraisal Tool.
| Author | 1.1 | 1.2 | 1.3 | 1.4 | 2.1 | 2.2 | 2.3 | 2.4 | 4.1 | 4.2 | 4.3 | 4.4 | Overall |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abate et al.26 2013 | Y | N | Y | C | 50% | ||||||||
| Emara et al.27 2011 | Y | Y | N | N | 50% | ||||||||
| Kemp et al.28 2018 | Y | Y | Y | Y | 100% | ||||||||
| Krych et al.22 2014 | Y | Y | Y | N | 75% | ||||||||
| Lee et al.23 2016 | Y | Y | N | N | 50% | ||||||||
| Smeatham et al.24 2016 | Y | Y | N | N | 50% | ||||||||
| Wright et al.25 2016 | Y | Y | Y | Y | 100% |
Y=Yes. N=No. C=Can't Tell.
1.1- Are the sources of qualitative data (archives, documents, informants, observations) relevant to address the research question (objective)? 1.2- Is the process for analyzing qualitative data relevant to address the research question (objective)? 1.3. Is appropriate consideration given to how findings relate to the context, e.g., the setting, in which the data were collected? 1.4. Is appropriate consideration given to how findings relate to researchers’ influence, e.g., through their interactions with participants? 2.1. Is there a clear description of the randomization (or an appropriate sequence generation)? 2.2. Is there a clear description of the allocation concealment (or blinding when applicable)? 2.3. Are there complete outcome data (80% or above)? 2.4. Is there low withdrawal/drop-out (below 20%)? 4.1. Is the sampling strategy relevant to address the quantitative research question (quantitative aspect of the mixed methods question)? 4.2. Is the sample representative of the population understudy? 4.3. Are measurements appropriate (clear origin, or validity known, or standard instrument)? 4.4. Is there an acceptable response rate (60% or above)? (Section 3.1-3.4 and 5.1-5.3 were not utilized of the MMAT).
Study Characteristics
Seven studies were included in this meta-analysis, four24,25,27,28 on physical therapy management and three22,23,26 investigating intra-articular injections for FAI. All study details including sample size, patient age, intervention type, outcome measure, timepoint assessed, results, and details of the physical therapy intervention are found in Table 2. The studies involving physical therapy included a variety of interventions such as stretching, hip and core strengthening, manual therapy, functional training, and patient education on activity modification. Further detail regarding the studies specific intervention techniques and dosage can be found in Table 3.
Table 2.
.Characteristics of Studies.
| Author | Timepoint Assessment | Level of evidence | Age mean ± SD (yrs) | Gender | Type of Intervention | Rehabilitation | Frequency and Duration of Int. | Outcome Measure |
|---|---|---|---|---|---|---|---|---|
| Krych et al.22 2014 | baseline, post-injection, 2 wks | Case series | N = 54 mean age 32.1 ± 11.9 |
19 m 35 f |
IA Injection |
IA corticosteroid injections 1) methyl- prednisolone acetate 2) triamcinolone 3) betamethasone, plus local anesthetic Pts were instructed to return to full activity as tolerated after the injection |
Injection at baseline | NRS |
| Lee et al.23 2016 | baseline and 12 wks | Prospective, randomized, double-blind, cross over study | N = 30 mean age 37 range (24-51) |
11 m 19 f |
IA Injection |
IA injection Two types of injections: 1) steroid TA 2) HA |
Injection at baseline and two wks later | NRS, HOOS |
| Abate et al.26 2013 | baseline, 6 mo, 12 mo | Open prospective trial | N=20 mean age 45 ± 16.9 |
13 m 7 f |
IA Injection | IA Injection high molecular weight HA | Injection at baseline & 40 days after. Dosage was repeated 6 mo after. | VAS, HHS |
| Smeatham et al.24 2016 | baseline and 3 mo | Parallel group, pilot RCT |
Routine Care: N = 15 mean age 32.6 range (18.5-50.3) Intervention: N = 15 mean age 35.9 range (18.6-48.8) |
30 m | PT |
PT Intervention group: Education, core stability, hip strength, ex (functional, proprioception, spinal) stretching, MT |
PT session mean 6.5 (range 1-13) over a 3 mo period |
VAS, HOS (ADL) |
| Wright et al.25 2016 | baseline and 7 wks | Prospective, randomized controlled clinical trial pilot study | N=18 mean age 33.7 ± 9.5 range (18-55) |
4 m 11 f |
PT |
MTEX group: PT and HEP, each session had 1 MT & a minimum of 15 min of ex focused on hip & core strengthening |
Both groups had HEP MTEX group 12 sessions for 1 hr, 2x/ week for 6 weeks |
NPRS, HOS (ADL) |
| Emara et al.27 2011 | baseline, 6 mo, 12 mo, 18 mo, 24 mo | Cohort study | N=37 mean age 33 ± 5 |
27 m 10 f |
PT |
4 stages of PT: 1) education on activity avoidance & NSAIDs (2) physiotherapy 2-3 weeks: stretching 20-30 min daily (3) assess normal ROM of hip IR & flexion, ADL ROM modifications (4) modify ADL predisposing FAI (avoid FADIR) |
Stage 1 2 x day/ 2-4 wks Stage 2 20-30 min sessions daily for 2-3 wks Stage 3 2-3 wks Stage 4 2-3 wks |
VAS, HHS |
| Kemp et al.28 2018 | baseline and 12 weeks | Pilot RCT | N=24 Mean age 37 ± 8 | 7 m 17 f |
PT |
FAIS-specific PT group: personalized progressive strengthening and functional retraining Both Groups: received manual therapy, progressive physical activity, and education |
8 PT sessions over a 12 week period, and 12 weekly supervised gym visits. Participants were also asked to complete 2 additional unsupervised sessions at their convenience. |
HOOS-P, HOOS-Q |
FAI(S) = Femoroacetabular Impingement (Syndrome), Tx = treatment, yrs = years, Int. = intervention, IA injection = intra-articular injection, PT = physical therapy, post-op = post-operative, pre-op = pre-operative, SD = Standard Deviation,TA = triamcinolone acetoimide, HA = hyaluronic acid, wk = week, mo = month, m = males, f = females, ex = exercise, WB = weight bearing, TTWB = Toe Touch Weight Bearing, FWBAT = full weight bearing as tolerated, WBAT = Weight Bearing as Tolerated; MRA/I = magnetic resonance arthrography/ imaging, CT = Commuted Tomography, US = Ultrasound, VAS = visual analog scale; mHHS = modified Harris Hip Score; HOOS = Hip Disability and Osteoarthritis Outcome Score; HOS = Hip Outcome Score; NRS = Numeric Rating Scale; HHS = Harris Hip Score; NPRS = Numeric Pain Rating Scale, ORS = Oral Numeric Scale NPS = Numeric Pain Scale, MTEX = manual therapy and supervised exercise group, Ad+HEP = advice plus home exercise group, pt = Patient, HEP = Home Exercise Plan, MT = Manual Therapy, HS=Hamstrings, BL=Bilateral
Table 3.
Available Study Interventions.
| Author | Physical Therapy Interventions |
|---|---|
| Smeatham et al.24 2016 |
Control group: routine care, analgesia, and self-management advise/exercise previously provided Intervention group: control group interventions, MT, patient education, exercise (core stability, hip strengthening, spinal, and functional activity), stretching, corrective shoe insoles, gym class, and video gait analysis |
| Wright et al.25 2016 |
Control group: education on activity modification and HEP to complete 2-3x a week consisting of stretching with 30 sec. holds (HS, hip flexor, glutes, piriformis) and strengthening 3 sets x 15 with 3 second holds (clamshells, bridges, and standing hip abduction) Intervention group: HEP and treatment algorithm to classify patient after exam into the following groups: (1) pain – pain control interventions, low grade mobilizations, ROM activities, stretching; (2) stiffness – ROM activities, high grade mobilizations; (3) weakness – strength and stability exercises, strength training, balance activities, and functional WB exercises Strength training: 3 sets of 10 or until fatigue; areas addressed: hip abduction, hip extension, hip ER, knee flexion and extension, TA and multifidus training Neuromuscular control: balance activities of varied surfaces and progress to sports movements MT: manual stretching (quadricep, hip flexors, HS, adductors, gluteus, external rotators, internal rotators, FABER) 2 reps x 60 secs or 4 reps x30 secs; long axis distraction with thrust, caudal glide or distraction mobilization with hip flexion, hip glides (posterior, anterior, and lateral), IR in prone, quadrant (flexion, adduction, and rotation) |
| Emara et al.27 2011 |
4 stages of Therapy: Stage 1: physical activity modification and NSAIDs (2-4 weeks) Stage 2: PT for hip ER and abduction in extension and flexion stretching (20-30 min. daily), activity modification (2-3 weeks) Stage 3: activity modification adjusted for new pain-free ranges between maximum hip IR and ER Stage 4: modifying activity that pre-disposed FAI |
| Kemp et al.28 2018 |
Control: hip joint manual therapy, progressive cardiovascular fitness with dosage varying between 15 minutes to 1 hour, muscle stretching (hip, lower leg, and trunk) and health education FAIS -Specific physical therapy group: joint MT, specific trunk and hip (adductor, abductor, extensor, and ER) strengthening exercises with dosage varying from 1-2 sets for 15-50 reps, progressive cardiovascular fitness with the same as the control group, functional movement retraining, education; therapy tailored to clinical presentation and comorbidities |
NSAIDs = Nonsteroidal Anti-Inflammatory Drug, FAI = Femoroacetabular impingement, FAIS = Femoroacetabular impingement syndrome, PT = Physical therapy, ER = External rotation, IR = Internal rotation, MT = Manual therapy, HEP = Home exercise plan, HS = Hamstring, ROM = Range of motion, tx = Treatment, WB = Weight bearing, TA = Transverse abdominus, FABER = Flexion Abduction External Rotation, reps = Repetitions, secs = Seconds
Results of Individual Studies
Seven studies assessed self-reported pain following the use of conservative interventions in FAI and utilized the following scales: VAS,24,26,27 some variation of the NRS,22,23,25 and the HOOS-P.28 Six studies measured self-reported physical function outcomes following the use of conservative interventions in FAI and utilized the following tools: HHS or modified HHS (mHHS),26,27 HOS ADL,24,25 and HOOS.23,28 Outcome measures for pain and function in both treatment groups were assessed at two different timepoints: pre and post treatment. The meta-analysis was conducted on six of the seven studies.22,24-28 The authors of one study23 were contacted for additional data, but did not respond.
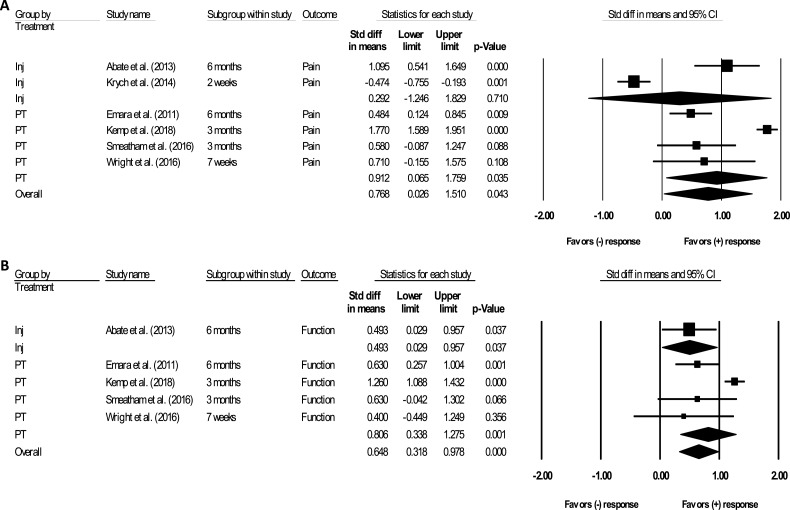
Pain
Two of the six studies22,26 assessed self-reported pain after the use of an intra-articular injection. These studies did not demonstrate statistically significant differences in self-reported pain and had a small effect size (SMD, 0.29, CI: -1.25, 1.83, p = 0.710). Four of the six studies24,25,27,28 assessed self-reported pain after the use of physical therapy interventions. Results demonstrated a significant reduction in pain and a large effect size (SMD, 0.91, CI: 0.07, 1.76, p=0.030). When analyzing the pooled impact of both conservative interventions for FAI, a significant reduction in pain and a moderate effect size was demonstrated (SMD, 0.77, CI: 0.03, 1.51, p=0.040). See Figure 2 and Table 4 for meta-analysis results.
Figure 2.
Standard difference in means in individual studies comparing injection, physical therapy, and overall combined conservative treatment for short-term (A) pain and (B) function. Squares represent study-specific findings and diamond represents summary estimates of random effects meta-analysis. CI = Confidence Interval, Inj = Injection, PT = physical therapy..
Table 4.
Meta-analysis for short-term impact.
| Outcome Category | Treatment | Participants, n | Studies, n | Overall I2 | p value | SMD | 95% CI |
|---|---|---|---|---|---|---|---|
| Pain | INJ | 74 | 2 | 0.710 | 0.29 | -1.25 – 1.83 | |
| PT | 81 | 4 | 0.035 | 0.91 | 0.07 – 1.76 | ||
| Combined | 155 | 6 | 97.291 | 0.043 | 0.77 | 0.03 – 1.51 | |
| Function | INJ | 20 | 1 | 0.037 | 0.49 | 0.03 – 0.96 | |
| PT | 81 | 4 | 0.001 | 0.80 | 0.34 – 1.28 | ||
| Combined | 101 | 5 | 79.821 | <0.001 | 0.65 | 0.32 – 0.98 |
INJ = Injection; PT = Physical Therapy; SMD = Standardized Mean Difference
Physical Function
One of the six studies26 assessed self-reported function after the use of intra-articular injection. This study did not demonstrate statistically significant differences in self-reported function and had a small effect size (SMD, 0.49, CI: 0.03, 0.96, p = 0.040). Four of the six studies24,25,27,28 assessed function after the use of physical therapy interventions. Results of the four studies demonstrated a significant improvement in function and a large effect size (SMD, 0.80, CI: 0.34, 1.28, p=0.001). When analyzing the pooled impact of both conservative interventions for FAI, a significant improvement in function and a moderate effect size was demonstrated (SMD, 0.65, CI: 0.32, 0.98, p≤0.001). See Figure 2 and Table 4 for meta-analysis results.
DISCUSSION
The purpose of this systematic review and meta-analysis was to analyze the results of two conservative interventions, intra-articular injections and physical therapy, within the domains of self-reported pain and physical function. Results demonstrated that physical therapy had significant positive changes in self-reported pain and function whereas intra-articular injections results were inconsistent. Overall, the literature demonstrated that conservative treatment (both injection and physical therapy) for this condition presented with moderate to large effect sizes and significantly impacted self-reported pain and function in individuals with FAI.
FAI is a condition that results in impairments that can be addressed by physical therapy interventions. All four studies that evaluated physical therapy interventions,24,25,27,28 utilized patient education and activity modification techniques in patients with FAI, and were effective in producing significant changes in self-reported pain and function. Education on the condition and activity modification techniques aimed at avoiding painful ranges of motion, including flexion and internal rotation during ADLs, can potentially limit the progression of symptoms.29 However, it is unclear the short-term impact of patient education and activity modification in isolation because they occurred simultaneously with other interventions in these studies.
Strength training is a common intervention used in a physical therapy plan of care. Previous literature has also demonstrated that patients with FAI have weaker hip musculature than a healthy population.30 Three of the four studies24,25,28 included hip strengthening in their plan of care for patients with FAI. Strengthening exercises can be utilized to address muscular imbalances and dynamic control deficits in the hip, potentially improving the patient's tolerance for his or her desired activities. This may ultimately lead to improved function and quality of life. Although strength outcomes were not analyzed in this meta-analysis, the duration of the strengthening programs appeared to be of an appropriate length to possibly induce changes in strength, size, or activation patterns of the muscles of the hip joint. However, frequency of training was not consistent within these studies and ranged from twice a week to several visits per month. Adherence to the individual strengthening program completed outside of supervised exercise was also not clearly reported. Both frequency of treatment and adherence to the exercise program established by the physical therapists could have had an impact on these results.
Joint mobilization and manipulation techniques are used for a variety of reasons including pain relief and improving range of motion.31 Three of the four studies24,25,28 in this meta-analysis included some form of manual therapy, including soft tissue mobilization, manual stretching, and joint mobilizations and manipulations. For FAI, an improvement in range of motion resulting from manual therapy techniques could improve the patient's ability to perform functional activities with lower levels of pain. However, it's unclear as to which manual techniques are effective as these were not clearly defined in two of the three studies. In the study by Wright et al.,25 the treatment protocol and included manual therapy techniques were clearly explained and those authors were able to produce small to moderate effect sizes related to pain and function.
Pain and limited function are two common results of FAI and a sequelae of FAI, osteoarthritis (OA). Intra-articular injections are commonly used for these two conditions with mixed results.22,26,32 The results of this meta-analysis support the variability of the effectiveness of injections on self-reported pain and function in FAI. As with physical therapy interventions, the frequency of the treatment can have an impact on its effectiveness. Previous literature32 in the area of hip OA reported the greatest improvement in function and pain to be within one week of a steroid injection with a gradual decline in effects thereafter. The results of this meta-analysis for mitigation of pain are contradictory to this suggestion. It appears multiple injections over six months26 is more effective in reducing pain in FAI. However, there were only two studies utilizing injections that were included for pain and one study included for function in this meta-analysis. Furthermore, one study was excluded from the meta-analysis due to limited reporting of data. Therefore, it may be difficult to completely determine the effectiveness of injections for the treatment of FAI based upon this analysis.
FAI is a structural deformity that requires surgery in the form of arthroscopy or open hip dislocation to correct the abnormality. Surgical intervention is accompanied by many risks, adverse effects, and increased costs.4,5 Previous literature supports the use of physical therapy either in place of or prior to surgery to improve outcomes related to FAI.7,29,33 Prior to resorting to surgery, conservative interventions could be utilized to improve self-reported pain and function and ultimately decide if surgery is necessary, thereby reducing the risk and financial burden of this condition.
This systematic review and meta-analysis had several limitations. The exclusion of non-English studies may have resulted in applicable studies being omitted. Quality assessment revealed the included studies had varying amounts of potential bias which may have influenced the results. Another limiting factor of this study is the limited number of studies, particularly in the area of intra-articular injections. This limits the total number of participants included in the aggregate calculations and comparisons. Furthermore, one study23 did not report enough statistical data to be included in the meta-analysis, despite demonstrating favorable results. Finally, limitations in intervention reporting could limit the applicability to current clinical practice.
Due to the limited amount of high-quality literature on this topic, it is evident that further research is needed to improve medical management for patients with FAI. A study comparing the effectiveness of intra-articular injection to physical therapy as well as combining the two interventions would provide further insight into effectiveness of the various conservative interventions. This information could assist clinicians in determining the proper course of medical management for FAI. Another study could also compare the outcomes of conservative intervention to surgical procedures to further assist the clinician in patient management. Finally, research investigating the impact of conservative care on functional performance and pain with daily and sport related activities in patients with FAI is indicated.
CONCLUSIONS
Current literature includes various studies investigating the outcomes concerning FAI and what may be the proper course of treatment. The results of this systematic review and meta-analysis indicate that conservative intervention results in beneficial outcomes related to reduction of pain and improvement of function in patients with FAI. Physical therapy demonstrated positive results related to self-reported pain and function as well as in comparison to intra-articular injection alone. The results of this study could be implemented into clinical practice along with clinician expertise to improve the care and medical management for individuals with FAI.
Appendix 1.
PubMed Search Strategy:
MeSH terms: hip injuries; hip joint; femoroacetabular impingement; physical therapy modalities; conservative treatment; injections, intra-articular; postperative period; pain; quality of life; return to sport; treatment outcome
Text Words: hip joint; femoroacetabular impingement; FAI; intra-articular hip injuries; “hip labr*”; physical therapy modalities; conservative treatment; injections, intra-articular; postoperative period; pain; quality of life; return to sport; treatment outcome
REFERENCES
- 1.Bredella M Ulbrich E Stoller D, et al. Femoroacetabular impingement. Magn Reson Imaging Clin N Am. 2013;21(1):45-64. [DOI] [PubMed] [Google Scholar]
- 2.Kuhns BD Weber AE Levy DM, et al. The natural history of femoroacetabular impingement. Front Surg. 2015;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clohisy J Baca G Beaulé P, et al. Descriptive epidemiology of femoroacetabular impingement. Am J Sports Med. 2013;41(6):1348-1356. [DOI] [PubMed] [Google Scholar]
- 4.Kahlenberg CA Han B Patel RM, et al. Time and cost of diagnosis for symptomatic femoroacetabular impingement. Orthop J Sports Med. 2014;2(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shearer DW Kramer J Bozic KJ, et al. Is hip arthroscopy cost-effective for femoroacetabular impingement? Clin Orthop. 2011;470(4):1079-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris JD Erickson BJ Bush-Joseph CA, et al. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskel Med. 2013;6(3):207-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wall PD Fernandez M Griffin DR, et al. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PMR. 2013;5(5):418-426. [DOI] [PubMed] [Google Scholar]
- 8.Khan W Khan M Alradwan H, et al. Utility of intra-articular hip injections for femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2015;3(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liberati A Altman D Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4). [DOI] [PubMed] [Google Scholar]
- 10.Kappa as a measure of concordance in categorical sorting. Vassarstats. http://vassarstats.net/kappa.html. Published 2001. Accessed February 4, 2018.
- 11.Cook C. Clinimetrics Corner: Use of effect sizes in describing data. J Man Manip Ther. 2008;16(3):54-57. [Google Scholar]
- 12.Pace R Pluye P Bartlett G, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47-53. [DOI] [PubMed] [Google Scholar]
- 13.What is the difference between short-term, intermediate, and long-term outcomes? eXtension http://articles.extension.org/page/44517/what-is-the-difference-between-short-term-intermediate-and-long-term-outcomes. Published May 2013. Accessed February 26, 2018.
- 14.Chuang LL Lin KC Hsu AL, et al. Reliability and validity of a vertical numerical rating scale supplemented with a faces rating scale in measuring fatigue after stroke. Health Qual Life Outcomes. 2015;13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferreira-Valente MA Pais-Ribeiro JL Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399-2404. [DOI] [PubMed] [Google Scholar]
- 16.Martin R Kelly B Philippon M. Evidence of validity for the Hip Outcome Score. Arthroscopy. 2006;22(12):1304-1311. [DOI] [PubMed] [Google Scholar]
- 17.Nilsdotter A Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons. Arthritis Care Res. 2011;63(S11):S200-S207. [DOI] [PubMed] [Google Scholar]
- 18.Huedo-Medina T Sanchez-Meca J Martin-Martinez F. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? The center for Health, Intervention, and Prevention (CHIP): Digital Commons; 2006. [DOI] [PubMed]
- 19.Higgins J Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21(11):1539-58. [DOI] [PubMed] [Google Scholar]
- 20.Landis J Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [PubMed] [Google Scholar]
- 21.Liberati A Altman DG Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krych AJ Griffith TB Hudgens JL, et al. Limited therapeutic benefits of intra-articular cortisone injection for patients with femoro-acetabular impingement and labral tear. Knee Surg Sports Traum Arthros. 2014;22(4):750-755. [DOI] [PubMed] [Google Scholar]
- 23.Lee YK Lee GY Lee JW, et al. Intra-Articular injections in patients with femoroacetabular impingement: a prospective, randomized, double-blind, cross-over study. J Korean Med Sci. 2016;31(11):1822-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smeatham A Powell R Moore S, et al. Does treatment by a specialist physiotherapist change pain and function in young adults with symptoms from femoroacetabular impingement? A pilot project for a randomised controlled trial. Physiother. 2017;103(2):201-207. [DOI] [PubMed] [Google Scholar]
- 25.Wright AA Hegedus EJ Taylor JB, et al. Non-operative management of femoroacetabular impingement: A prospective, randomized controlled clinical trial pilot study. J Sci Med Sport. 2016;19(9):716-721. [DOI] [PubMed] [Google Scholar]
- 26.Abate M Scuccimarra T Vanni D, et al. Femoroacetabular impingement: is hyaluronic acid effective? Knee Surg Sports Traumatol Arthrosc. 2013;22(4):889-892. [DOI] [PubMed] [Google Scholar]
- 27.Emara K Samir W Motasem EH, et al. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg. 2011;19(1):41-45. [DOI] [PubMed] [Google Scholar]
- 28.Kemp J Coburn S Jones D, et al. The Physiotherapy for Femoroacetabular Impingement Rehabilitation STudy (physioFIRST): A pilot randomized controlled trial. J Orthop Sports Phys Ther. April 2018;48(4):307-315. [DOI] [PubMed] [Google Scholar]
- 29.Enseki K Harris-Hayes M White D, et al. Nonarthritic hip joint pain. J Orthop Sports Phys Ther. 2014;44(6):A1-A32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freke M Kemp J Svege I, et al. Physical impairments in symptomatic femoroacetabular impingement: a systematic review of the evidence. Br J Sports Med. 2016;50(19):1180. [DOI] [PubMed] [Google Scholar]
- 31.Dutton M. Manual Techniques. In: Dutton M, ed. Dutton Orthopaedic examination, evaluation, and intervention. 4th ed. New York, NY: McGraw-Hill Medical; 2017:428-434. [Google Scholar]
- 32.McCabe P Maricar N Parkes M, et al. The efficacy of intra-articular steroids in hip osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2016;24(9):1509-1517. [DOI] [PubMed] [Google Scholar]
- 33.Guenther J Cochrane C Hunt M, et al. A pre-operative exercise intervention can be safely delivered to people with femoroacetabular impingement and improve clinical and biomechanical outcomes. Physiother Can. 2017;69(3):204-211. [DOI] [PMC free article] [PubMed] [Google Scholar]