Abstract
Purpose/Background
There is little information to support the use of clinical tests to assess for microinstability of the hip joint. The purpose of this study was to use a string model to describe and compare length changes of the iliofemoral ligament in the test positions commonly used to assess hip ligament laxity.
Methods
Twelve hip joints from nine cadavers (4 male; 5 female) with lifespans of 57-84 years of age were studied. A string model representing the medial and lateral arms of the iliofemoral ligament was secured to the proximal and distal attachment points. The amount of length change of the string model was compared in four test positions: 1) external rotation, 2) hyperextension-external rotation 3) abduction-extension-external rotation, and 4) adduction-extension-external rotation.
Results
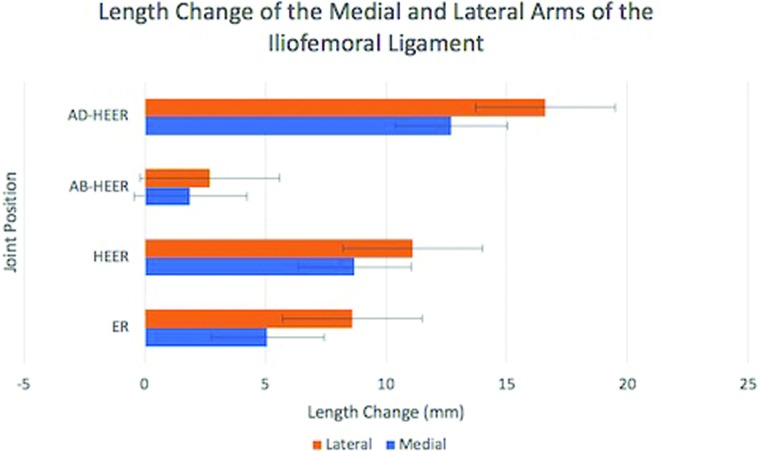
For the medial arm, the greatest change occurred in the adduction-extension-external rotation position (12.7mm). This was significantly greater than the external rotation (5.1mm; p=0.002) and abduction-extension-external rotation position (1.9mm; p<0.001). The lateral arm also had the greatest excursion in the adduction-extension-external rotation position (16.6mm). This length change was significantly greater than the external rotation position (8.6mm; p=0.002), the hyperextension-external rotation (11.1mm; p=0.047), and the abduction-extension-external rotation position (5.6mm; p<0.001).
Conclusions
Tests used for hip instability cause various levels of tension through the iliofemoral ligament. The combination of hip extension and external rotation increased the length change of string model and was maximized with hip adduction. The least amount of change occurred with the addition of hip abduction to extension and external rotation.
Clinical Relevance
Clinicians may use the information to help interpret tests for instability of the hip and may consider the combined position of hip extension, external rotation, and adduction to elucidate involvement of the iliofemoral femoral ligament.
Level of Evidence
2b; Exploratory cohort study with good reference standards
Keywords: hip, instability, ligament, special tests, validity
INTRODUCTION
Hip microinstability is defined as extra-physiologic motion between the femoral head and acetabulum that may cause pain originating from labral and cartilage damage, with or without symptoms of instability.1–4 The cause of microinstability can be multifactorial and often results from a contribution of boney abnormalities such as dysplasia,5 poor muscle function, and/or laxity of the ligaments and capsule.2,4,6–8 Laxity of the capsuloligamentous structures can be part of a genetic disorder such as Ehlers-Danlos Syndrome9 or may be acquired through repetitive motions of the hip joint. The most common mechanism of injury is forced external rotation with axial loading that causes atraumatic anterior focal rotational microinstability.10–12 Microinstability is a recognized source of hip pain and disability in athletes that participate in sports that require repetitive and forceful movements beyond their available range of motion.1–4 This injury pattern most commonly occurs in sports such as ballet, skating, gymnastics, baseball, and golf.10,12,13
The importance of a thorough clinical examination in the diagnostic process of those with non-arthritic hip pain, including microinstability has been emphasized.14–18 The diagnosis of hip microinstability is typically based on patient history, physical examination and radiographic evaluation.1,3,4,10 However, there is little information to support the use of clinical tests to assess for microinstability, specifically for patients with suspected anterior focal rotational microinstability from iliofemoral ligament laxity.1 Since forced repetitive external rotation is known to cause injury to the iliofemoral ligament,6,11 most tests for microinstability of the hip joint stress the hip in positions of end range external rotation. These include the following special tests to assess anterior hip ligamentous laxity: 1) log roll/dial test (external rotation in neutral),1,3 2) prone instability test (external rotation in neutral),3,19,20 3) anterior apprehension/hyperextension-external rotation (HEER) test,3,20 and 4) abduction-extension-external rotation (AB-HEER) test.3,20 Table 1 and Figures 1–4 describe these tests. Hoppe at el.20 found the prone instability, HEER, and AB-HEER to be valuable in diagnosing hip microinstability using arthroscopy as the gold standard. The authors noted that further studies are needed to validate these clinical tests.20 Because of the limited information available on the tests used to diagnose microinstability, there is a need to validate the best test position to assess for iliofemoral ligament laxity.
Table 1.
Test positions for anterior focal rotational microinstability.
| Test | Position; Procedure | Sign | Figure |
|---|---|---|---|
| Log Roll/Dial | Supine; Passive hip external rotation to end range with over pressure | Increase external rotation range of motion with decrease bounce back at end range of motion | 1 |
| Prone Instability | Prone; passive external rotation while the examiner applies an anteriorly directed force on the trochanter | Hip joint pain or sense of anterior instability | 2 |
| HEER/ Anterior Apprehension | Supine at the end of table with affected leg hanging off and unaffected knee toward chest; passive hip extension and external rotation | Hip joint pain or sense of anterior instability | 3 |
| AB-HEER | Side lying on unaffected hip; Passive hip abduction to 30 °, extension 10 ° and external rotation to end range while an anteriorly directed force applied to trochanter | Hip joint pain or sense of anterior instability | 4 |
| AD-HEER | Side lying on unaffected hip; Passive hip adduction to 20 °, extension 10 ° and external rotation to end range. | Hip joint pain or sense of anterior instability. ** Total amount of external rotation available should be less than the AB-HEER position if there is no anterior laxity** | 5 |
HEER = hyperextension external rotation; AB-HEER = abduction hyperextension external rotation; AD-HEER = adduction hyperextension external rotation
Figure 1.
Log Roll/Dial test. Supine; Passive hip external rotation to end range with over pressure.
Figure 4.
Abduction hyperextension external rotation (AB-HEER) test. Side lying on unaffected hip; Passive hip abduction to 30 °, extension 10 ° and external rotation to end range while an anteriorly directed force applied to trochanter.
Figure 2.
Prone Instability test. Prone; passive external rotation while the examiner applies an anteriorly directed force on the trochanter.
Figure 3.
Hyperextension external rotation (HEER)/Anterior Apprehension test. Supine at the end of table with affected leg hanging off and unaffected knee toward chest; passive hip extension and external rotation.
The iliofemoral ligament is shaped like an inverted Y and distally splits into medial and lateral arms. The medial arm passes downward in a near vertical direction to insert on the anterior femur at the level of the lesser trochanter. The lateral arm crosses the joint obliquely with a horizontal orientation and inserts on the crest of the greater trochanteric, just above the intertrochanteric line.10 The iliofemoral ligament is felt to limit external rotation in flexion and both internal and external rotation in extension.10 A study of intact ligaments found increased strain on the lateral arm with maximal external rotation in adduction and increased strain on the medial arm with external rotation in extension.21 The positions to assess for ligament laxity have included hip extension and external rotation with and without abduction.1,3,19,20 However, considering the orientation of the iliofemoral ligament fibers in relation to hip joint axis, a position with extension, external rotation and adduction may be the best position to asses for iliofemoral ligament laxity (Figure 5).
Figure 5.
Adduction hyperextension external rotation (AD-HEER) test. Side lying on unaffected hip;Passive hip adduction to 20 °, extension 10 ° and external rotation to end range.
The purpose of this study was to use a string model to describe and compare length changes of the iliofemoral ligament in the test positions commonly used to assess hip ligament laxity. It was hypothesized that the combined position of hip external rotation, extension, and adduction would produce the greatest length change of the medial and the lateral arms of the iliofemoral ligament when compared to the following hip positions: 1) external rotation, 2) external rotation and extension, and 3) external rotation, extension, and abduction.
METHODS
Cadaver Preparation
An ethics board for the study of human cadavers granted permission to perform the study. A total of 12 hip joints from nine embalmed cadavers (4 male; 5 female) with lifespans of 57-84 years of age were studied for the purpose of this study. Complete dissection of the cadavers was performed to remove all muscular and soft tissue attachments on the femur, leaving only the capsule and capsular ligaments intact. Fibers of the iliofemoral ligament were identified and dissected to isolate the proximal attachment point of the ligament, inferior to the anterior inferior iliac spine, and the distal attachments of the medial and lateral arms of the iliofemoral ligament along the intertrochanteric line. The mid-point of the proximal and distal attachments of the iliofemoral ligament the were marked with an 1/8 inch eyelet screw. Once the markings of the iliofemoral ligament were complete and the eyelet screws placed, the capsule was vented in a vertical direction for about 1 cm and spaced 1 cm apart along the periphery of the femoral neck.
String Model Set-up
A string model was then constructed that connected the medial and lateral distal attachment points to the eyelet screw at the proximal attachment point (Figure 6). The pelvis was then secured to a 2x10x24 inch board with two 6-inch lag screws so that the face of the board rested snuggly against the anterior superior iliac spines. This provided a reference from which the pelvis was securely affixed in a neutral position (neutral pelvic tilt, obliquity, and rotation). Additional eyelet screws were added to the end of the board so that the remaining length of the strings could freely move through the opening of the screws. To allow for consistent tension on the string when moving the hip joint, two 6-inch hemostats, weighing 11g each, were hung from the ends of the strings (Figure 7).
Figure 6.
Set-up of the string model following the arms of the iliofemoral ligament.
Figure 7.
The specimen is placed in a side lying position, secured to a wood plank that is attached to the table.
The specimen was then placed in a sidelying position with the side to be tested closest to the ceiling. The board that was affixed to the pelvis was then secured perpendicular to the edge of table edge with two large C-clamps as shown in Figure 7.
The hip joint was then positioned in neutral alignment in all the cardinal planes. This was confirmed using a bubble inclinometer and a standard goniometer. A long clamp that extended from the board was used to maintain the hip in neutral alignment of the sagittal plane during testing.
Test Positions
Four distinct test positions were analyzed for this study. The first position reproduced the position for the prone instability, dial, and log roll tests.1,3,19,20 The hip was held in neutral abduction/adduction and flexion/extension and then laterally rotated to 45 °. The second position recreated the hyperextension external rotation test (HEER test).3,20 The HEER test placed the hip joint in 10 ° of hip extension (confirmed with the goniometer), neutral abduction/adduction and lateral rotation to 45 ° (confirmed with bubble inclinometer). The third position recreated the abduction hyperextension external rotation (AB-HEER) test.3,20 This test position (Figure 8) combined 10 ° of extension, 45 ° external rotation and 30 ° of hip abduction (confirmed with bubble inclinometer). The final test position of hip extension, external rotation, and adduction was chosen to recreate a position previously reported to increase tension on the iliofemoral ligament.21 This position combined 10 ° extension, 45 ° external rotation, and 20 ° adduction.
Figure 8.
Positioning of the cadaver for the abduction hyperextension external rotation (AB-HEER) test.
Data Collection
The strings representing the iliofemoral ligament were marked while the cadaver was maintained in neutral alignment in all three cardinal planes. This served as the reference point from which a change in length could be determined. The hip was then moved into the first test position by one of the researchers. A second researcher confirmed the hip position with the standard goniometer for flexion/extension and the bubble inclinometer for rotation and adduction/abduction. A third investigator used an electronic caliper to measure the amount of distance the string moved of through the proximal eyelet screw. The distance from initial marking to the finished test position was recorded. Each test position was repeated a total of three times. Between each trial, the hip was returned to the neutral position for 20 seconds before returning to the test position. The average of the three trials was used to determine the change in length from neutral to each test position for each respective test.
Measures of boney morphology that included femoral version, acetabular version, and femoral inclination were recorded for each specimen. The version and inclination angles were measured using a standard 12-inch goniometer (Baseline® Goniometer, Fabrication Enterprises Inc., White Plains, NY) to describe the orientation of the acetabulum and proximal aspect of the femur. Acetabular version was determined by the angle formed by the sagittal plane and a line formed by connecting the midpoint of the anterior and the posterior acetabular rim. Femoral version was determined as the angle formed by a line bisecting the femoral head/neck and a line parallel to the posterior aspect of the femoral condyles. Femoral inclination was determined as the angle between a line bisecting the femoral neck relative to a line bisecting the femoral shaft.
Statistical Methods
All data were analyzed using SPSS 24 (IBM, Chicago). Descriptive statistics (mean, standard deviation, and range) of the age of the cadaver, femoral version, acetabular version, and femoral inclination were computed. An intraclass correlation coefficient (ICC) was performed to determine the retest reliability of the length change of the string model between trials. A one-way analysis of variance (ANOVA) with an a priori alpha set at 0.05 compared change of length of the string model in the four respective test positions for each arm of the iliofemoral ligament. Tukey's poc hoc analysis was performed to determine the individual differences between the test positions.
RESULTS
Descriptive statistics of the version and inclination angles of the femur and acetabulum are presented in Table 2. The ICC performed to assess test-retest reliability of the length change computed for each of the positions used in the current study was excellent, r=0.96; p<0.01.
Table 2.
Descriptive statistics of the version and inclination angles of the femur and acetabulum.
| N | Minimum | Maximum | Mean | Standard Deviation | |
|---|---|---|---|---|---|
| Acetabular version | 12 | 10 ° | 26 ° | 20 ° | 6 ° |
| Femoral version | 12 | 6 ° | 32 ° | 21 ° | 8 ° |
| Femoral Inclination | 12 | 109 ° | 140 ° | 124 ° | 8 ° |
The results of the one-way ANOVA demonstrated a significant effect for the test position on the change in length of the string model for the medial arm, F(3,47)=11.7, p<0.001, as well as the lateral arm, F(3,47)=15.7, p<0.001, as shown in Table 3. For the medial arm, the greatest change occurred in the AD-HEER position with an average of 12.7mm of length change in the string model (Figure 9). This was significantly greater than the ER position (5.1mm; p=0.002) and the AB-HEER position (1.9mm; p<0.001). The lateral arm also had the greatest excursion in the AD-HEER position with a length change of 16.6mm. This length change was significantly greater than the ER position (8.6mm;p=0.002), the HEER (11.1mm;p=0.047), and the AB-HEER position (5.6mm;p<0.001).
Table 3.
Descriptive statistics of the length change of the medial and lateral arms of the iliofemoral ligament in each test position.
| Arm | Position | N | Mean | Standard Deviation | 95% Confidence Interval | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| Medial | ER | 12 | 5.1 | 2.4 | 3.6-6.7 | 2.5 | 9.6 |
| HEER | 12 | 8.7 | 4.6 | 5.7-11.6 | 3.7 | 17.5 | |
| AB-HEER | 12 | 1.9 | 3.8 | -0.5-4.3 | 0.0 | 10.1 | |
| AD-HEER | 12 | 12.7 | 6.8 | 8.3-17.0 | 5.5 | 26.7 | |
| Lateral | ER | 12 | 8.6 | 3.5 | 6.3-10.8 | 4.0 | 16.4 |
| HEER | 12 | 11.1 | 5.2 | 7.8-14.4 | 5.1 | 21.8 | |
| AB-HEER | 12 | 2.7 | 4.4 | -0.1-5.5 | 0.0 | 11.4 | |
| AD-HEER | 12 | 16.6 | 6.6 | 12.4-20.9 | 8.1 | 29.1 |
ER = 45 ° of External Rotation; HEER=45 ° of External Rotation and 10 ° extension; AB-HEER=30 ° abduction, 45 ° of External Rotation and 10 ° extension; AD-HEER=20 ° adduction, 45 ° of External Rotation and 10 ° extension.
Figure 9.
Length Change of the Medial and Lateral Arms of the Iliofemoral Ligament
HEER = hyperextension external rotation; AB-HEER = abduction hyperextension external rotation;
AD-HEER = adduction hyperextension external rotation. Bars represent standard error.
DISCUSSION
The most important finding of this study was that a position of hip external rotation, extension, and adduction, as with the AD-HEER test, produced the greatest length change in both medial and lateral arms of the iliofemoral ligament when compared to the position of the hip joint when performing the prone instability, dial, log roll, HEER, or AB-HEER tests.1,3,19,20
The diagnostic accuracy to identify those with anterior focal rotational microinstability may be improved if a position that best stresses the iliofemoral ligament is used. The AD-HEER test position had nearly six times greater length change of the iliofemoral ligament than the AB-HEER test position. This is consistent with previous studies that showed the greatest strain of the iliofemoral ligament occurred when the hip was externally rotated from a position of adduction and extension.21,22 The addition of hip adduction with hip extension and external rotation caused the maximum length change of the string model of the iliofemoral ligament (Figure 5) and helps to validate this test position for stability testing of the hip joint.
The results of the current study compliment previous works on the function of the iliofemoral ligament.21,23,24 Martin et al.24 individually released the medial and lateral arms of the iliofemoral ligament and found an increase in external rotation range of motion when each arm was released. However, release of the lateral arm provided a greater increase in external rotation range of motion in flexion and in a neutral position compared to medial arm release. The lateral arm release also showed an increase of internal rotation range of motion when the hip was in an extended position.24 A study of intact ligaments found increased strain on the lateral arm with maximal external rotation in adduction and increased strain on the medial arm with external rotation in extension.21 Using magnetic resonance arthrography the medial arm tightened in extension and the lateral arm tightened with external rotation.23 Fuss and Bacher22 performed one of the most extensive evaluations of the hip joint ligaments. A total of 60 different combinations of multi-planar positions of the hip joint were examined to determine specific positions that maximized tension of the ligaments. Among the many combinations of joint positions that tensioned the iliofemoral ligament, both the medial and lateral arms were lengthened in positions that included extension, adduction, and external rotation.22 The results of the current study confer the findings from these previous studies that show that individual and combined movements of hip extension, adduction, and external rotation can result in increased tension of both arms of the iliofemoral ligament. In the current study, greater changes were seen in the lateral arm versus the medial arm of the iliofemoral ligament suggesting the proposed tests for microinstability may be more biased toward tensioning of the lateral arm of the iliofemoral ligament.
While the AD-HEER was shown to have the greatest change in length of the string model, the diagnostic accuracy of this test has not been reported on living subjects. The diagnostic accuracy of the prone instability, HEER, and AB-HEER tests, however, have been studied.20 Hoppe et al.20 found the AB-HEER test to be most accurate in predicting hip instability followed by the HEER and the prone instability tests. The AB-HEER test had a sensitivity of 80.6 and specificity of 89.4 and the HEER test had a sensitivity of 71.0 and specificity of 85.1.20 The prone instability test had a low value of sensitivity at 33.9 but a high specificity of 97.9.20 Despite showing the greatest combined sensitivity and specificity in detecting hip instability, the AB-HEER demonstrated the smallest length change in the string model used in this current study. The AB-HEER test increased the length of the medial arm by only 1.9mm and 2.7mm for the lateral arm. These results support findings by Hidaki et al.25 that demonstrated no increase of strain to the iliofemoral ligament when the hip was positioned in abduction. The work of Fuss and Bacher21,22 suggest that the AB-HEER test lengthens structures other than the iliofemoral ligament, specifically the pubofemoral ligament. Other studies have shown that the ligamentum teres tightens in combined positions of hip flexion and rotation.26–28 These findings illustrate the unique function of each structure and the importance of triplanar joint position in determining which ligament may be lengthened or stressed.22,24,29 Although it is beyond the scope of the current study, future research may investigate how specific test positions test can discriminate iliofemoral, ligamentum teres, and pubofemoral ligament dysfunction in symptomatic patients.
Limitations
While this study provides useful information on clinical tests for hip instability, there are a number of limitations that must be recognized. First, the use of cadaveric models limits the generalizability of the results to living subjects. The cadavers were embalmed and the surrounding soft tissue structures of the pelvis were removed. This may have changed the native mechanics of the hip joint and influenced the findings of the study.
Secondly, the morphologic characteristics of the specimens must be considered when interpreting the results of the study.2,4,6–8 Specimen measures of hip morphology showed that the average femoral anteversion (21o) and acetabular anteversion (20o) in the study population was greater than normal population averages of 10 °30 and 17 °,31 respectively. Conversely, the average femoral inclination of 124 ° in the current study was less than the normal population average of 129 °.30 To help mitigate the influence of boney morphology, the test positions were standardized with specific multiplanar positions for each specimen. However, it remains unclear how the morphologic characteristics of the specimens may have impacted the results of this study. A similar study with a larger sample size that categorizes specimens according to version angles may be of interest for future investigation.
Third, the string model does not account for the elasticity of the native ligamentous tissue but is a measure of a change in distance of a non-elastic string. While length change string may relate to the potential of strain across the ligament, it does not account for the elasticity of the tissue that may otherwise influence loading of the tissue. Future studies may be performed that test the tensile properties of the iliofemoral ligament in the common test positions used for evaluation of hip instability.
Another factor is that the age of the specimens that were used in the current study are much older than the population of patients generally diagnosed with microinstability of the hip. Therefore, the quality and integrity of the bony, cartilaginous, and capsular tissues may be different than patients generally treated for microinstability of the hip. Finally, the sample size for this project was limited by the number of available specimens. A larger and more diverse sample population may offer greater projection of the findings of the study to a general patient population.
CONCLUSIONS
The results of this study showed that common test positions used for evaluating hip instability may cause various levels of tension through the iliofemoral ligament based on the length changes observed in an anatomic string model of the iliofemoral ligament. The combination of hip extension and external rotation increased the length change of the string model and was maximized with the addition of hip adduction. The least amount of change occurred with the addition of hip abduction to extension and external rotation. Clinicians may find the information useful when interpreting tests for instability of the hip and may consider assessing the hip in the combined position of hip extension, external rotation, and adduction to elucidate potential involvement of the iliofemoral femoral ligament.
REFERENCES
- 1.Bolia I Chahla J Locks R Briggs K Philippon MJ. Microinstability of the hip: a previously unrecognized pathology. Muscles Ligaments Tendons J. 2016;6(3):354-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han S Alexander JW Thomas VS, et al. Does capsular laxity lead to microinstability of the native hip? Am J Sports Med. 2018;46(6):1315-1323. [DOI] [PubMed] [Google Scholar]
- 3.Kalisvaart MM Safran MR. Microinstability of the hip-it does exist: Etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2(2):123-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dangin A Tardy N Wettstein M May O Bonin N. Microinstability of the hip: A review. Orthop Traumatol Surg Res. 2016;102(8S):S301-S309. [DOI] [PubMed] [Google Scholar]
- 5.Dumont GD. Hip Instability: Current concepts and treatment options. Clin Sports Med. 2016;35(3):435-447. [DOI] [PubMed] [Google Scholar]
- 6.Philippon MJ Nepple JJ Campbell KJ, et al. The hip fluid seal--Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729. [DOI] [PubMed] [Google Scholar]
- 7.Reis AC Rabelo ND Pereira RP, et al. Radiological examination of the hip - clinical indications, methods, and interpretation: A clinical commentary. Int J Sports Phys Ther. 2014;9(2):256-267. [PMC free article] [PubMed] [Google Scholar]
- 8.Myers CA Register BC Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39 Suppl:85S-91S. [DOI] [PubMed] [Google Scholar]
- 9.Larson CM Stone RM Grossi EF Giveans MR Cornelsen GD. Ehlers-Danlos Syndrome: Arthroscopic management for extreme soft-tissue hip instability. Arthroscopy. 2015;31(12):2287-2294. [DOI] [PubMed] [Google Scholar]
- 10.Shu B Safran MR. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011; 30(2):349-367. [DOI] [PubMed] [Google Scholar]
- 11.Philippon MJ. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20(4):817-829. [DOI] [PubMed] [Google Scholar]
- 12.Klingenstein GG Martin R Kivlan B Kelly BT. Hip injuries in the overhead athlete. Clin Orthop Relat Res. 2012;470(6):1579-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shindle MK Ranawat AS Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25(2):309-326, ix-x. [DOI] [PubMed] [Google Scholar]
- 14.Martin HD Shears SA Palmer IJ. Evaluation of the hip. Sports Med Arthrosc. 2010;18(2):63-75. [DOI] [PubMed] [Google Scholar]
- 15.Braly BA Beall DP Martin HD. Clinical examination of the athletic hip. Clin Sports Med. 2006;25(2):199-210, vii. [DOI] [PubMed] [Google Scholar]
- 16.Martin HD. Clinical examination of the hip. Oper Techn Orthop. 2005;15(3):117-190. [Google Scholar]
- 17.Schenker ML Martin RL Weiland DE Philippon MJ. Current trends in hip arthroscopy: A review of injury diagnosis, techniques and outcome scoring. Curr Opin Orthop. 2005;16:89-94. [Google Scholar]
- 18.Martin RL Enseki KR Draovitch P Trapuzzano T Philippon MJ. Acetabular labral tears of the hip: Examination and diagnostic challenges. J Orthop Sports Phys Ther. 2006;36:503-515. [DOI] [PubMed] [Google Scholar]
- 19.Domb BG Stake CE Lindner D El-Bitar Y Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: Two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41(11):2591-2598. [DOI] [PubMed] [Google Scholar]
- 20.Hoppe DJ Truntzer JN Shapiro LM Abrams GD Safran MR. Diagnostic accuracy of 3 physical examination tests in the assessment of hip microinstability. Orthop J Sports Med. 2017;5(11):2325967117740121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hidaka E Aoki M Muraki T Izumi T Fujii M Miyamoto S. Evaluation of stretching position by measurement of strain on the ilio-femoral ligaments: An in vitro simulation using trans-lumbar cadaver specimens. Man Ther. 2009;14(4):427-432. [DOI] [PubMed] [Google Scholar]
- 22.Fuss FK Bacher A. New aspects of the morphology and function of the human hip joint ligaments. Am J Anat. 1991;192(1):1-13. [DOI] [PubMed] [Google Scholar]
- 23.Wagner FV Negrao JR Campos J, et al. Capsular ligaments of the hip: Anatomic, histologic, and positional study in cadaveric specimens with MR arthrography. Radiology. 2012;263(1):189-198. [DOI] [PubMed] [Google Scholar]
- 24.Martin HD Savage A Braly BA Palmer IJ Beall DP Kelly B. The function of the hip capsular ligaments: A quantitative report. Arthroscopy. 2008;24(2):188-195. [DOI] [PubMed] [Google Scholar]
- 25.Hidaka E Aoki M Izumi T Suzuki D Fujimiya M. Ligament strain on the iliofemoral, pubofemoral, and ischiofemoral ligaments in cadaver specimens: Biomechanical measurement and anatomical observation. Clin Anat. 2014;27(7):1068-1075. [DOI] [PubMed] [Google Scholar]
- 26.O’Donnell J Economopoulos K Singh P Bates D Pritchard M. The ligamentum teres test: A novel and effective test in diagnosing tears of the ligamentum teres. Am J Sports Med. 2014;42(1):138-143. [DOI] [PubMed] [Google Scholar]
- 27.Martin HD Hatem MA Kivlan BR Martin RL. Function of the ligamentum teres in limiting hip rotation: A cadaveric study. Arthroscopy. 2014;30(9):1085-1091. [DOI] [PubMed] [Google Scholar]
- 28.Kivlan BR Richard Clemente F Martin RL Martin HD. Function of the ligamentum teres during multi-planar movement of the hip joint. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1664-1668. [DOI] [PubMed] [Google Scholar]
- 29.Gray H Standring S Ellis H Berkovitz BKB. Gray's anatomy : The anatomical basis of clinical practice. 39th ed. Edinburgh ; New York: Elsevier Churchill Livingstone; 2005. [Google Scholar]
- 30.Toogood PA Skalak A Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Rel Res. 2009;467(4):876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reikeråls O Bjerkreim I Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54(1):18-23. [DOI] [PubMed] [Google Scholar]