Abstract
Liver transplant programs in Canada require a period of 6 months of abstinence from alcohol before considering a patient with liver disease secondary to alcohol for transplantation. Although some studies have demonstrated good outcomes following a transplant in carefully selected patients before the 6‐month abstinence period has been met, there have been arguments against this, including the claim that the public has a general negative perception of those with alcohol dependence. We performed a multicenter cross‐sectional survey to determine the perception of people in British Columbia, Canada, toward liver transplantation in patients with liver disease due to alcohol who have not demonstrated the capacity to remain abstinent from alcohol for 6 months. A total of 304 patient questionnaires were completed, and 83.1% agreed with a period of abstinence of 6 months. In those patients who were unlikely to survive 6 months without a transplant, 34.1% of respondents agreed with, 44.1% did not agree with, and 21.4% were neutral about, early transplantation; 42.8% would have less trust in the process of transplantation if a period of abstinence was not maintained, but relaxing the requirement for an abstinence period would not have an impact on the majority's decision to donate organs. Only 30.5% would support abandoning the abstinence criteria. Conclusion: Among patients followed at general gastroenterology, medicine, or transplant clinics, there is a willingness to relax the criteria in selected patients unlikely to survive without a transplant, although a general consensus remains in support of the existing 6‐month alcohol abstinence rule. A larger scale survey of all provinces in Canada would be required to assess support for such a change in policy.
Abbreviations
- ACLF
acute‐on‐chronic liver failure
- AH
alcoholic hepatitis
- CI
confidence interval
- OR
odds ratio
Alcohol‐associated liver disease, whether by liver cirrhosis or alcoholic hepatitis (AH), is a frequent cause of death. Alcohol cessation is of paramount importance in the management of this condition. However, some patients will continue to progress to decompensated liver disease and liver failure despite abstinence from alcohol. It is accepted that liver transplantation is the only option for survival for these patients. The majority of transplant centers in North America require a 6‐month abstinence period before assessing a patient for liver transplantation.1, 2 The reasons for recommending this 6‐month period are that significant improvement of liver function in a good proportion of patients can be observed to levels where a liver transplant is no longer needed and it allows sufficient time for evaluation of a patient's risk of potential relapse in alcohol consumption.3, 4
However, patients presenting with severe AH unresponsive to prednisone treatment have a poor prognosis and may not survive the abstinence period of 6 months without transplant.4 In addition, the 6‐month abstinence period as a predictor of reduced risk of alcohol consumption relapse has not been consistently demonstrated.5, 6 It is increasingly recognized that certain patients may have a low risk of relapse following a liver transplant before achieving 6 months of abstinence.7 Evidence to support the use of the 6‐month abstinence period is weak because it comes from poorly controlled studies.8, 9, 10
Early transplantation in acute AH before the 6‐month period of abstinence has been effective in both European and American trials.4, 11 As a consequence of the outcomes of these studies, interest has been expressed by Canadian adult transplant programs in considering the possibility of providing transplants for patients with AH within the 6‐month abstinence period.3, 5 Liver transplantation for end‐stage liver disease due to alcohol misuse has always been controversial, in part due to a general negative perception of alcoholism among the public12 and the perception that these patients are less deserving due to the behavioral component of their disease.5 A survey in the United States of 503 participants that assessed the attitudes among the public about liver transplantation12 indicated that the majority (81.5%) were at least neutral toward early transplantation for these patients. There are no data in Canada on this subject. This study aims to explore this gap in understanding patient perspectives on early liver transplantation for alcoholic liver disease in British Columbia.
Participants and Methods
Study Design and Participants
This was a cross‐sectional study using a paper‐based self‐assessment questionnaire to evaluate public opinion on liver transplantation in alcohol‐associated liver disease. The participants were consecutive patients recruited at clinics in three cities in British Columbia and included a general gastroenterology clinic in Vancouver, a liver transplant clinic in Vancouver, a general internal medicine clinic in Nanaimo, and a general gastroenterology clinic in Prince George. Participants were invited to answer a questionnaire if they were older than 19 years of age, had some fluency in English, and were capable of providing informed consent. Participants were excluded if they were inpatients, diagnosed with AH within the last 6 months, and had previously participated in the survey. The study was approved by the University of British Columbia Clinical Research Ethics Board.
Questionnaire
The questionnaire Appendix 1 was a paper‐based self‐assessment that included questions on the theme of liver transplantation and alcohol‐related liver disease, using a Likert‐type scale (completely disagree, disagree, neutral, agree, completely agree). The questionnaire also included questions on desire to become an organ donor, impact of a change in policy on trust in the organ donation process, and opinion on length of abstinence required. Data were also collected on sex, ethnic background, level of education, income, alcohol consumption, presence and etiology of liver disease, transplantation status, and the three first letters of the postal code. Postal code information was collected in order to assess if attitudes differed among participants taken from urban as opposed to rural communities.
One unit of alcohol was defined as 350 mL (12 U.S. ounces) of beer, 150 mL (5 U.S. ounces) of wine, or 44 mL (1.5 U.S. ounces) of liquor. Participants were asked to estimate their frequency of alcohol consumption as well as the volume of alcohol consumed on average at each sitting. Participants who had stopped consuming alcohol were asked to provide an estimate of the same information during the time when they had been actively drinking. Alcohol consumption level was defined as “none,” “little–moderate,” and “heavy,” based on estimates participants provided, including prior consumption from participants who had abstained. Participants who never drank were classified as “none,” participants who drank less than 2 to 4 times a month or who drank more frequently but only 1 to 2 units at each time were defined as “little–moderate,” and everyone else was classified as “heavy” (Supporting Fig. S1). The definition used to define the “heavy” drinker group was based on a self‐reported estimated consumption above the recommended Canadian guidelines.13 The questionnaire was pretested for clarity among staff workers of the transplant and gastroenterology clinic at Vancouver General Hospital.
The primary outcome measures of the study were descriptive; each statement was an estimate of the proportion of participants in agreement or in disagreement and the strength of that opinion. The secondary outcome measures were demographic data, transplant status, and presence of liver disease or alcohol consumption in order to identify factors associated with the level of agreement.
Statistical Analysis
Continuous variables are presented as means, SDs, medians, and interquartile ranges as applicable. Categorical data are presented as proportions (%). Continuous data are compared using the Student t test and categorical data using the Pearson chi‐square test or the Fischer's exact test as applicable.
An ordinal logistic regression model was used to identify variables that were associated with more agreement for a particular statement. In ordinal regression, the odds that a variable is associated with a greater likelihood to be in a higher category is measured. Answers are ranked as “in complete disagreement” (lowest category), “disagreement,” “neutral,” “agreement,” and “in complete agreement” (highest category). The ordinal model predicts the odds of a result in a higher category. All baseline variables collected were included in the univariate analysis, but only variables that were statistically significant, had a 95% confidence interval (CI) within 5% of the null value, or were potential confounders were included in the multivariable model. All analyses were performed using Stata, version 15.1 (StataCorp, College Station, TX).
Results
Population Description
A total of 304 participants were recruited as follows: 105 from the transplant clinic in Vancouver, 114 from the general gastroenterology clinic in Vancouver, 51 from the internal medicine clinic in Nanaimo, and 34 from the general gastroenterology clinic in Prince George. The mean age of participants was 54.2 years (SD, 13.6), 55.3% were men, and 71.0% were white. The majority of participants had an underlying history of liver disease (57.3%); in order of frequency, the diagnoses were hepatitis C (20.4%) and autoimmune hepatitis (13.5%). The prevalence of alcohol‐associated liver disease was 8.9%. Of the participants, 17.1% had received a previous liver transplant, 20.4% were either in the assessment process or had been listed, and 62.2% did not need a liver transplant at that time. A summary of participant description, including other variables, is provided in Table 1.
Table 1.
Population Description
| Variable | Total Population N = 304 |
|---|---|
| Age, mean (SD) | 54.2 (13.6) |
| Sex | |
| Male | 55.3% |
| Female | 44.6% |
| Urban | 90.7% |
| Rural | 9.3% |
| Ethnicity | |
| White | 71.0% |
| African American | 1.6% |
| First Nations | 6.3% |
| Latin American | 0.7% |
| South Asian | 5.3% |
| South‐East Asian | 5.3% |
| Middle Eastern | 1.3% |
| Chinese/Japanese/Korean | 4.9% |
| Other/missing | 3.6% |
| Liver Disease | |
| Hepatitis C | 20.4% |
| Hepatitis B | 3.6% |
| Nonalcoholic steatohepatitis | 10.9% |
| Alcohol‐associated liver disease | 8.9% |
| Autoimmune hepatitis | 13.5% |
| Other | 4.0% |
| None | 23.4% |
| Unsure/missing | 15.5% |
| Liver transplant status | |
| Not assessed/not needed | 62.2% |
| Assessed/listed | 20.4% |
| Previous transplant | 17.1% |
| Missing | 0.33% |
| Highest level of education achieved | |
| Elementary school | 4.0% |
| High school | 47.7% |
| Undergraduate degree | 24.0% |
| Graduate degree | 17.4% |
| Prefer not to disclose/missing | 6.9% |
| Annual income | |
| Less than Can $25,000 | 16.8% |
| Can $25,000 to 49,999 | 19.7% |
| Can $50,000 to 74,999 | 15.5% |
| Can $75,000 to 99,999 | 10.5% |
| More than Can $100,000 | 17.1% |
| Prefer not to disclose/no answer | 20.4% |
| Alcohol consumption | |
| Still drink some alcohol | 33.9% |
| Quit drinking | 43.1% |
| Never drank alcohol | 13.8% |
| Missing | 9.2% |
Questionnaire
The first question assessed the agreement to a requirement for an abstinence period before liver transplantation in patients with liver disease due to alcohol. The majority of participants were in agreement (complete agreement, 52.0%, 95% CI, 46.3‐57.6; agreement, 34.4%, 95% CI, 29.3‐40.0) (Fig. 1A). After providing arguments usually given in favor of the 6‐month abstinence rule, including the possibility of spontaneous improvement and assessing the risk of alcohol consumption relapse, the majority of participants remained in agreement with the 6‐month abstinence rule, although fewer were in complete agreement (complete agreement, 36.4%, 95% CI, 31.2‐42.0; agreement, 46.7%, 95% CI, 41.1‐52.4) (Fig. 1B).
Figure 1.
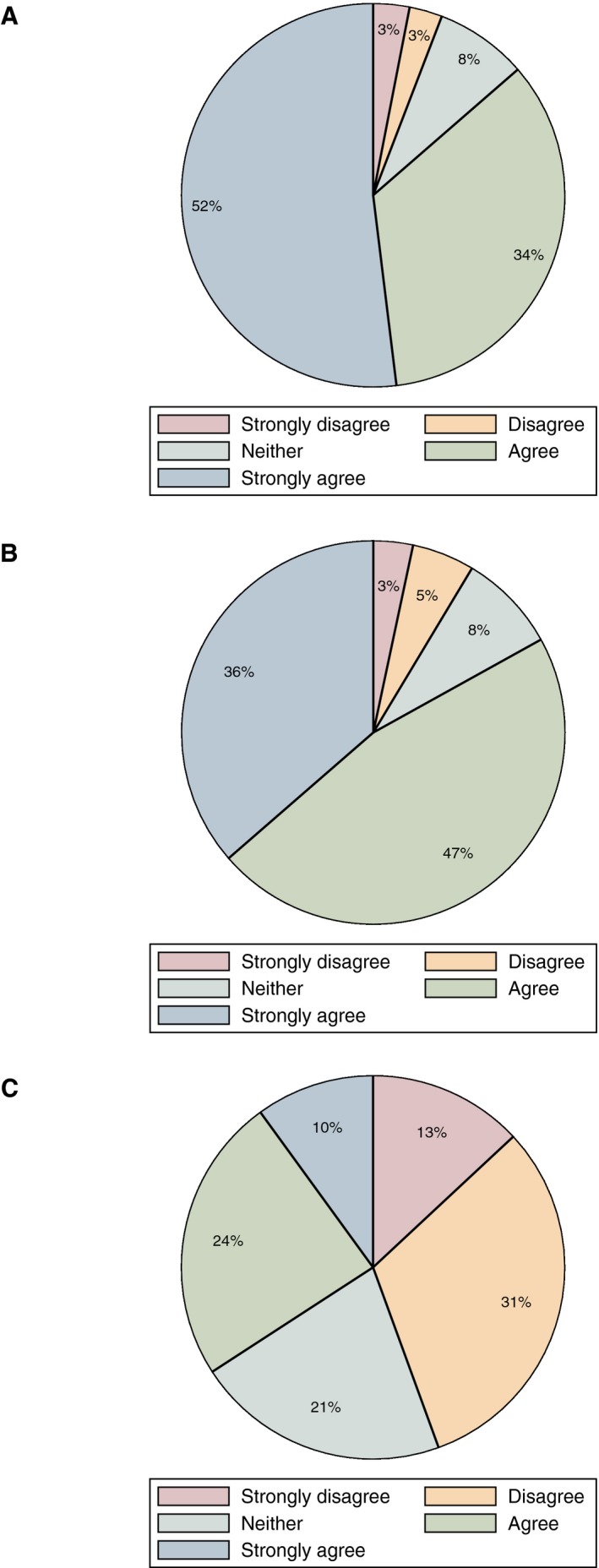
Pie graphs of summarizing distributions to questionnaire answers. Respondents' agreement (A) to a period of abstinence, (B) to a 6‐month period of abstinence, and (C) to drop the requirement for a period of abstinence in patients unlikely to survive 6 months.
In the case of a patient considered to be unlikely to survive the period of 6 months without a transplant, a significant number of participants were in agreement with relaxing the abstinence rule (complete agreement, 10.0%, 95% CI, 7.1‐14.1; agreement, 24.1%, 95% CI, 19.5‐29.3) and 21.4% were neutral to the idea (95% CI, 17.1‐26.4) (Fig. 1C). When the participant subgroups were analyzed according to the level of alcohol consumption (none, little–moderate, heavy), there was no difference in maintaining or relaxing the 6‐month abstinence rule in cases of severe AH unlikely to survive without a transplant (Fig. 2).
Figure 2.
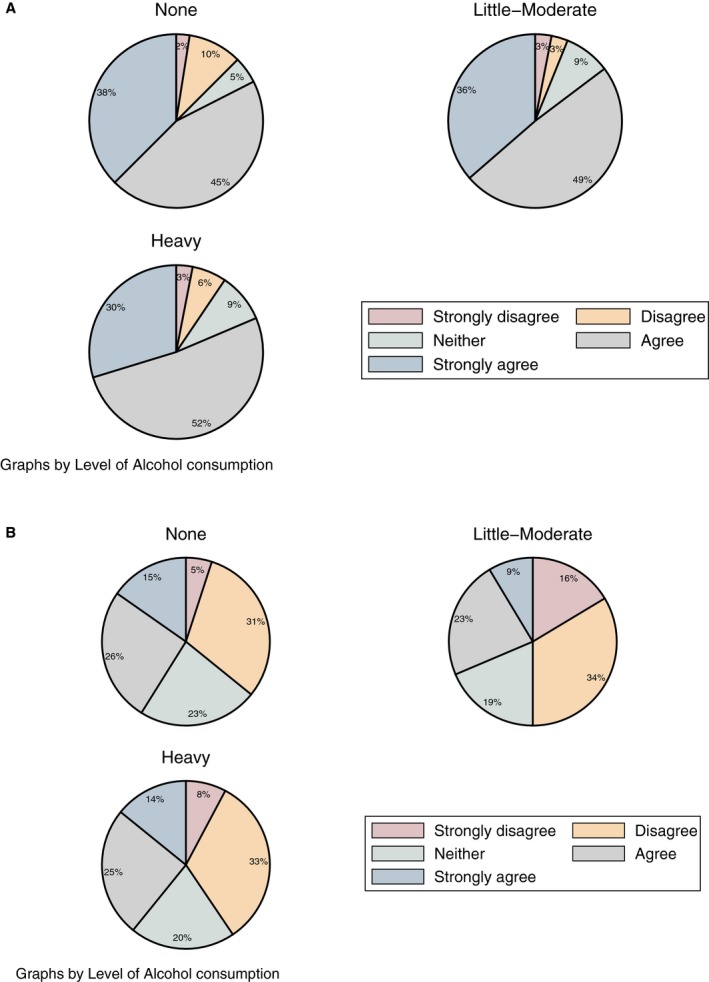
Respondents' agreement stratified by alcohol consumption history. (A) Response to a 6‐month period of abstinence and (B) response to drop the requirement for a period of abstinence in patients unlikely to survive 6 months.
The majority of participants (58.7%) considered the 6‐month period of time an appropriate length for abstinence, 28.2% were in favor of a longer period, and 13.0% were in favor of a shorter period. Of the participants, 42.8% considered that if liver transplantation were offered to patients with alcohol‐associated liver disease who were still actively drinking or not showing a period of abstinence, it would decrease their trust in the process of transplantation. Among participants who have considered being organ donors, 63.2% considered that it would not have an impact on their decision whereas 36% considered that it would make them less likely to become an organ donor. When participants were asked if they would support a change in the current criteria for liver transplantation to abandon the requirement for an abstinence period, 29.5% were in agreement, 38.6% were in disagreement, and 31.9% were undecided (Table 2).
Table 2.
Potential Impact of Change in Policy on Public Trust and Donation
| Would knowing that liver transplantation was offered to patients with alcoholic liver disease who are still actively drinking alcohol or have not shown a period of abstinence affect your trust in the process of transplantation? | ||
| Increase, 3.9% | Decrease, 42.8% | No impact, 53.3% |
| If liver transplantation were offered to patients with alcoholic liver disease who are still drinking alcohol, would you be more or less likely to become an organ donor? | ||
| All respondents | ||
| More likely, 1.8% | Less likely, 34.8% | No impact, 63.5% |
| Respondents who have considered becoming organ donors | ||
| More likely, 0.8% | Less likely, 36% | No impact, 63.2% |
| Would you support a change in the current criteria for liver transplantation to transplant patients with alcoholic liver disease who are still consuming alcohol or have not been abstinent for 6 months? | ||
| Yes, 30.5% | No, 39.3% | Undecided, 30.2% |
Factors Associated with Support for the Abstinence Rule
Participants were in agreement with a 6‐month abstinence rule. Univariate analysis identified a higher odds for being at a higher category of agreement among patients that had a previous liver transplant (odds ratio [OR], 2.07; 95% CI, 1.15‐3.71). Respondents with a previous history of alcohol‐related liver disease were also more likely to be in a higher category of agreement, but this was not statistically significant (OR, 2.20; 95% CI, 0.97‐5.01). Multivariate analysis indicated that liver transplant status remained statistically significant (OR, 2.24; 95% CI, 1.15‐4.36). A summary of the univariate and multivariate ordinal logistic regression is shown in Table 3.
Table 3.
Results of Univariate and Multivariate Ordinal Logistic Regression Assessing Respondents' Agreement to a 6‐Month Abstinence Period
| Variable | OR Univariate | 95% CI | OR Multivariate | 95% CI |
|---|---|---|---|---|
| Age (continuous) | 1.01 | 0.99‐1.02 | ||
| Age categories | ||||
| Less than 45 years | Ref. | |||
| 45‐60 years | 0.91 | 0.52‐1.60 | ||
| Older than 60 years | 1.29 | 0.73‐2.29 | ||
| Sex | ||||
| Male | Ref. | |||
| Female | 0.80 | 0.52‐1.23 | ||
| Rural | Ref. | |||
| Urban | 0.88 | 0.39‐1.98 | ||
| Liver Disease | ||||
| None/unknown | Ref. | Ref. | ||
| Nonalcohol related | 0.84 | 0.53‐1.35 | 0.67 | 0.39‐1.14 |
| Alcohol related | 2.20 | 0.97‐5.01 | 1.64 | 0.62‐4.38 |
| Transplant status | ||||
| Not needed | Ref. | Ref. | ||
| Assessed/listed | 1.19 | 0.68‐2.09 | 1.15 | 0.63‐2.17 |
| Received transplant | 2.07 | 1.15‐3.71 | 2.24 | 1.15‐4.36 |
| Schooling | ||||
| Elementary school | Ref. | |||
| High school | 1.65 | 0.52‐5.28 | ||
| Undergraduate | 1.25 | 0.38‐4.17 | ||
| Graduate | 1.49 | 0.44‐5.10 | ||
| Alcohol status | ||||
| Still drinks alcohol | Ref. | |||
| Quit | 1.23 | 0.76‐2.00 | ||
| Never drank | 1.07 | 0.54‐2.13 | ||
| Alcohol consumption history | ||||
| None | Ref. | |||
| Light–moderate | 1.05 | 0.53‐2.07 | ||
| Heavy | 0.78 | 0.37‐1.66 | ||
| Income (Can $) | ||||
| <25,000 | Ref. | |||
| 25,000‐50,000 | 0.61 | 0.21‐1.72 | ||
| 50,000‐75,000 | 1.17 | 0.34‐4.00 | ||
| 75,000‐100,000 | 0.61 | 0.18‐2.04 | ||
| >100,000 | 0.75 | 0.25‐2.27 |
Abbreviation: Ref., reference.
Regarding participant response to the question as to whether liver transplant should be considered if the patient were unlikely to survive before the end of a 6‐month abstinence period, univariate analysis showed lower odds for agreement to relax the abstinence rule among the following variables: age 45‐60 years (OR, 0.51; 95% CI, 0.30‐0.88), age older than 60 years (OR, 0.54; 95% CI, 0.31‐0.93), and annual income greater than Can $100,000 (OR, 0.49; 95% CI, 0.24‐0.99). These variables remained significant following multivariate analysis. Those participants that were being assessed or listed for transplant were also less likely to be in agreement with relaxing the abstinence rule (OR, 0.48; 95% CI, 0.24‐0.98) (Table 4).
Table 4.
Results of Univariate and Multivariate Ordinal Logistic Regression Assessing Respondents' Agreement to Drop the Abstinence Period for Patients Unlikely to Survive 6 Months
| Variable | OR Univariate | 95% CI | OR Multivariate | 95% CI |
|---|---|---|---|---|
| Age (continuous) | 0.98 | 0.97‐1.00 | ||
| Age categories | ||||
| Less than 45 years | Ref. | |||
| 45‐60 years | 0.51 | 0.30‐0.88 | 0.38 | 0.2‐0.76 |
| Older than 60 years | 0.54 | 0.31‐0.93 | 0.46 | 0.23‐0.95 |
| Sex | ||||
| Male | Ref. | |||
| Female | 0.99 | 0.66‐1.49 | ||
| Rural | Ref. | |||
| Urban | 0.96 | 0.46‐2.03 | ||
| Liver disease | ||||
| None/unknown | Ref. | Ref. | ||
| Nonalcohol related | 0.65 | 0.41‐1.02 | 0.92 | 0.50‐1.68 |
| Alcohol related | 0.73 | 0.34‐1.58 | 0.67 | 0.23‐2.02 |
| Transplant status | ||||
| Not needed | Ref. | Ref. | ||
| Assessed/listed | 0.66 | 0.40‐1.10 | 0.48 | 0.24‐0.98 |
| Received transplant | 0.89 | 0.52‐1.56 | 0.84 | 0.40‐1.75 |
| Schooling | ||||
| Elementary school | Ref. | |||
| High school | 0.64 | 0.20‐2.03 | ||
| Undergraduate | 0.70 | 0.21‐2.29 | ||
| Graduate | 0.73 | 0.21‐2.45 | ||
| Alcohol status | ||||
| Still drinks alcohol | Ref. | |||
| Quit | 0.99 | 0.62‐1.58 | ||
| Never drank | 1.61 | 0.83‐3.11 | ||
| Alcohol consumption history | ||||
| None | Ref. | Ref. | Ref. | |
| Light–moderate | 0.55 | 0.29‐1.03 | 0.69 | 0.34‐1.42 |
| Heavy | 0.86 | 0.43‐1.74 | 1.60 | 0.68‐3.80 |
| Income (Can $) | ||||
| <25,000 | Ref. | Ref. | ||
| 25,000‐50,000 | 0.61 | 0.31‐1.22 | 0.70 | 0.30‐1.65 |
| 50,000‐75,000 | 0.66 | 0.32‐1.36 | 0.89 | 0.35‐2.26 |
| 75,000‐100,000 | 0.58 | 0.26‐1.28 | 0.53 | 0.21‐1.37 |
| >100,000 | 0.49 | 0.24‐0.99 | 0.39 | 0.16‐0.97 |
Abbreviation: Ref., reference.
There was no difference in support for the abstinence rule between patients that were followed at the liver transplant clinic and general medicine or gastroenterology clinics. Analyses restricted to the subgroup of patients that were not being followed by the transplant clinic did not show any predictors of acceptance of early liver transplant (Supporting Tables S2 and S3).
Discussion
In severe AH unresponsive to corticosteroids, the mortality at 6 months can be as high as 70%.4, 14 In severe AH, the only treatment option to improve survival is transplantation; however, the majority of transplant centers require a period of abstinence before considering a patient for liver transplant, and most centers have set the time period at 6 months.
Advocates of an abstinence period justify this recommendation on the basis that such a period allows time for recovery in liver function, making transplantation unnecessary. Arguments against this recommendation include that although recovery without transplant might be more consistently expected in patients presenting with decompensated cirrhosis, it is much less likely in acute‐on‐chronic liver failure (ACLF) or severe AH. Concerns have also been expressed about subsequent relapse in alcohol consumption and damage to the allograft in patients with alcohol‐associated liver disease who have received a transplant without the usual pretransplant abstinence period. Studies evaluating the risk of relapse in alcohol consumption in patients abstinent for less than 6 months found a considerably higher risk of relapse in alcohol consumption compared to patients who were abstinent for more than 6 months,15, 16, 17 and a meta‐analysis found risk of relapse was higher when there was less than 6 months of abstinence.18 Although setting a 6‐month abstinence period has been considered by some as arbitrary and good outcomes have been observed in patients receiving a transplant without an imposed abstinence period in strongly motivated individuals with good social support,4, 11 it has been shown that the duration of pretransplant abstinence is the only independent predictor of problem drinking following transplant, with a 5% reduced risk of relapse in alcohol consumption for each month of successful abstinence before transplant.19
A possible negative impact on public opinion and a loss of trust in the transplantation process have also been suggested as reasons for maintaining the current period of alcohol abstinence before transplantation. Alcohol‐associated liver disease is often considered by the general public as a self‐inflicted disease. In a survey of the general public in Hong Kong, 75% of participants considered that priority for liver transplantation should be for those whose liver disease developed from naturally occurring disease rather than personal behavior,20 and a study of the general public, family doctors, and gastroenterologists in the United Kingdom showed that alcoholic liver disease ranked lower than other causes of liver disease in the list of priorities for transplantation.21 A recent web‐based survey conducted in the United States, however, found that 81.5% were at least neutral to and 51.3% were in agreement with the idea of early liver transplantation for alcohol‐associated liver disease, but 85% of respondents were still concerned about the risk of relapse in alcohol consumption and graft damage.12
In this study, the majority of participants surveyed were in favor of a period of abstinence before considering transplantation in alcohol‐related liver disease. Of the participants, 86.4% agreed with a period of abstinence and 83.1% agreed with a 6‐month period of abstinence after providing arguments in favor of this time interval. Support for maintaining a 6‐month period of abstinence waned when considering a patient unlikely to survive this period of abstinence without a transplant: 34.1% were in agreement, 44.4% did not agree with relaxing the abstinence period, and 21.4% were neutral. Our interpretation of these results is that participants recognize the importance of meaningful behavioral changes to ensure that the process of allocation is fair; however, when urgency of the situation merits it, for example, when a patient may not survive the abstinence period without a transplant, some leniency from transplant programs may be expected for these patients.
When the possible negative impact of relaxation of the abstinence rule on the process of transplantation was assessed in this survey, a large proportion of participants (42.8%) considered that such a decision would decrease their trust in the transplant process, and in those considering organ donation, 33.7% would make them less likely to become donors. We believe that in this survey the participants are sending the following messages to transplant programs: they expect the programs to be gatekeepers and to offer transplantation selectively as a last resort; they are re‐emphasizing the view that there is still a negative perception of transplantation in alcohol‐associated liver disease; and any significant change in policy should be accompanied by an intensive education campaign to avoid significant decreases in the donor pool. These should include reinforcing the message of addiction as a disease rather than as a behavior, that minor slips should not be perceived as failures, and that there is no significant difference in outcomes compared to liver transplantation for other diseases.
Ordinal logistic regression was performed to identify participant‐related factors associated with a higher agreement about the abstinence rule. This analysis showed that participants diagnosed with alcohol‐associated liver disease and those with prior liver transplants were more likely to have a higher level of agreement to the abstinence rule in the univariate analysis, but in the multivariate analysis, only prior liver transplantation remained significant. The posttransplant groups are a population who have experienced both the hardship of advanced liver disease and the transplantation process and have a better understanding of the value of organ donation and graft survival. It is interesting that the patients with alcohol‐associated liver disease agreed with maintaining the abstinence period, suggesting that they recognize the nature of the disease and understand the importance of abstinence for graft survival. Analysis of subgroups about the possibility of early liver transplantation indicated that older participants and those with a higher level of personal income were less likely to agree.
We did not attempt to distinguish between transplantation for AH and alcohol‐associated liver disease presenting with ACLF or severe decompensation. We felt that it would have been difficult to explain the differences in the pathophysiology and prognosis between these distinct clinical entities. More broadly, we asked about liver transplantation for patients unlikely to survive the 6‐month abstinence period as dictated by the current protocol of our institution. Studies on early liver transplantation have considered “entry into disease” as an important inclusion criterion. We argue that patients with preexisting cirrhosis are at risk of an ACLF event within their road to abstinence, and the high short‐term mortality probability warrants considering them as well for liver transplantation. In the American Consortium of Early Liver Transplantation for Alcoholic Hepatitis (ACCELERATE‐AH), 41% of patients did not have a histologic definition of AH; the authors argued that patients with ACLF could have been included and that this subset of patients was equally unlikely to survive 6 months without liver transplantation.11
There are several limitations to this study. The method of sampling resulted in overrepresentation of certain groups (older individuals, urban dwellers), participants were confined almost exclusively to patients and not members of the general public, and most participants had liver disease and/or gastrointestinal disease. However, as far as the ethnic distribution is concerned, our sampled population reflected the Canadian diversity.22 There was no argument against the abstinence rule or the arbitrary nature of the 6‐month time period, which could bias results in favor of an abstinence period. There was no data capture of possible participant reasons for support for an abstinence period, and some variables were prone to misclassification and information bias. Although accepting these limitations, this study is the first evaluation of a subset of the Canadian population on this important issue.
In conclusion, this study of patient participants suggests that consensus remains in support of the existing 6‐month abstinence rule in alcohol‐associated liver disease, with a willingness to relax the criteria in those patients unlikely to survive the 6‐month period of abstinence without a liver transplant. A larger scale survey of all provinces in Canada would be required to assess support for a change in policy. The discussion on a change of policy should involve representatives of the general public as well as representatives of patients with liver disease waiting for transplant and previous organ recipients.
Supporting information
Potential conflict of interest: Dr. Wallach advises Merck, AbbVie, Intercept, and Gilead. Dr. Yoshida received grants from Gilead, Merck, Janssen, AbbVie, Intercept, Genfit, and Springbank; he received honoraria for Continuing Medical Education/Ad Board lectures from Gilead Canada, Merck Canada, AbbVie Canada, Celgene Canada, and Intercept Canada. The other authors have nothing to report.
See Editorial on Page 1019
References
- 1. Kollmann D, Rasoul‐Rockenschaub S, Steiner I, Freundorfer E, Gyori GP, Silberhumer G, et al. Good outcome after liver transplantation for ALD without a 6 months abstinence rule prior to transplantation including post‐transplant CDT monitoring for alcohol relapse assessment ‐ a retrospective study. Transpl Int 2016;29:559‐567. [DOI] [PubMed] [Google Scholar]
- 2. Lucey MR, Rice JP. Liver transplantation for severe alcoholic hepatitis crosses the Atlantic. Am J Transplant 2016;16:739‐740. [DOI] [PubMed] [Google Scholar]
- 3. Chandok N, Aljawad M, White A, Hernandez‐Alejandro R, Marotta P, Yoshida EM. Liver transplantation for alcoholic liver disease among Canadian transplant centres: a national study. Can J Gastroenterol 2013;27:643‐646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 2011;365:1790‐1800. [DOI] [PubMed] [Google Scholar]
- 5. Congly SE, Lee SS. Liver transplantation for alcoholic liver disease: a devilish dilemma. Can J Gastroenterol 2013;27:625‐626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Singhvi A, Welch AN, Levitsky J, Singhvi D, Gordon EJ. Ethical considerations of transplantation and living donation for patients with alcoholic liver diseases. AMA J Ethics 2016;18:163‐173. [DOI] [PubMed] [Google Scholar]
- 7. Im GY, Kim‐Schluger L, Shenoy A, Schubert E, Goel A, Friedman SL, et al. Early liver transplantation for severe alcoholic hepatitis in the United States–a single‐center experience. Am J Transplant 2016;16:841‐849. [DOI] [PubMed] [Google Scholar]
- 8. Berlakovich GA, Steininger R, Herbst F, Barlan M, Mittlbock M, Muhlbacher F. Efficacy of liver transplantation for alcoholic cirrhosis with respect to recidivism and compliance. Transplantation 1994;58:560‐565. [DOI] [PubMed] [Google Scholar]
- 9. Fabrega E, Crespo J, Casafont F, De las Heras G, de la Peña J, Pons‐Romero F. Alcoholic recidivism after liver transplantation for alcoholic cirrhosis. J Clin Gastroenterol 1998;26:204‐206. [DOI] [PubMed] [Google Scholar]
- 10. Wiesner RH, Lombardero M, Lake JR, Everhart J, Detre KM. Liver transplantation for end‐stage alcoholic liver disease: an assessment of outcomes. Liver Transpl Surg 1997;3:231‐239. [DOI] [PubMed] [Google Scholar]
- 11. Lee BP, Mehta N, Platt L, Gurakar A, Rice JP, Lucey MR, et al. Outcomes of early liver transplantation for patients with severe alcoholic hepatitis. Gastroenterology 2018;155:422‐430.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stroh G, Rosell T, Dong F, Forster J. Early liver transplantation for patients with acute alcoholic hepatitis: public views and the effects on organ donation. Am J Transplant 2015;15:1598‐1604. [DOI] [PubMed] [Google Scholar]
- 13. Stockwell T, Butt P, Beirness D, Gliksman L, Paradis C. The basis for Canada's new low‐risk drinking guidelines: a relative risk approach to estimating hazardous levels and patterns of alcohol use. Drug Alcohol Rev 2012;31:126‐134. [DOI] [PubMed] [Google Scholar]
- 14. Louvet A, Naveau S, Abdelnour M, Ramond MJ, Diaz E, Fartoux L, et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology 2007;45:1348‐1354. [DOI] [PubMed] [Google Scholar]
- 15. Dumortier J, Dharancy S, Cannesson A, Lassailly G, Rolland B, Pruvot FR, et al. Recurrent alcoholic cirrhosis in severe alcoholic relapse after liver transplantation: a frequent and serious complication. Am J Gastroenterol 2015;110:1160‐1166. [DOI] [PubMed] [Google Scholar]
- 16. De Gottardi A, Spahr L, Gelez P, Morard I, Mentha G, Guillaud O, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med 2007;167:1183‐1188. [DOI] [PubMed] [Google Scholar]
- 17. Fung JY. Liver transplantation for severe alcoholic hepatitis‐The CON view. Liver Int 2017;37:340‐342. [DOI] [PubMed] [Google Scholar]
- 18. Dew MA, DiMartini AF, Steel J, De Vito Dabbs A, Myaskovsky L, Unruh M, et al. Meta‐analysis of risk for relapse to substance use after transplantation of the liver or other solid organs. Liver Transpl 2008;14:159‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tandon P, Goodman KJ, Ma MM, Wong WW, Mason AL, Meeberg G, et al. A shorter duration of pre‐transplant abstinence predicts problem drinking after liver transplantation. Am J Gastroenterol 2009;104:1700‐1706. [DOI] [PubMed] [Google Scholar]
- 20. Chan HM, Cheung GM, Yip AK. Selection criteria for recipients of scarce donor livers: a public opinion survey in Hong Kong. Hong Kong Med J 2006;12:40‐46. [PubMed] [Google Scholar]
- 21. Neuberger J, Adams D, MacMaster P, Maidment A, Speed M. Assessing priorities for allocation of donor liver grafts: survey of public and clinicians. BMJ 1998;317:172‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Statistics Canada . Census Profile, 2016 Census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E. Updated May 30, 2018. Accessed April 3, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


