1.
Cardiovascular disease remains the leading cause of morbidity/mortality for U.S. women, with one of four U.S. women dying from cardiovascular disease. Importantly, two of three U.S. women have at least one major traditional coronary risk factor, and this percentage increases with older age.
Appropriately, most recommendations from the 2019 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Primary Prevention of Cardiovascular Disease1 are not gendered, reflecting the scientific databases from which they were derived, although admittedly women were underrepresented in most studies.
The basis for individual patient preventive recommendations is use of the Pooled Cohort Equations; the resultant Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score is calculated separately for women and men (Figure 1 ). New to this guideline is consideration of risk‐enhancing factors, a concept that may particularly advantage women. Advocated in this listing is the consideration of features unique to or predominant in women. These include pregnancy‐associated conditions such as a history of preeclampsia,2 preterm delivery,3 small for gestational age infants, chronic inflammatory diseases, such as rheumatoid arthritis,4 lupus,5 or HIV/AIDS infection6 and if measured persistently elevated inflammatory markers, A history of premature menopause is also relevant.7 The ASCVD Risk Score, for example, fails to capture that individuals of South Asian ancestry constitute a high‐risk population.8 Metabolic syndrome, a not infrequent presentation for women, encompasses the risk of increased waist circumference, elevated triglycerides, elevated blood pressure, elevated glucose and low HDL‐cholesterol. For women at intermediate risk (a sizeable population since only 1 in 5 U.S. women has no traditional cardiovascular risk factors), addressing risk‐enhancing factors for women assumes particular importance in the clinician/patient risk discussion.
Figure 1.
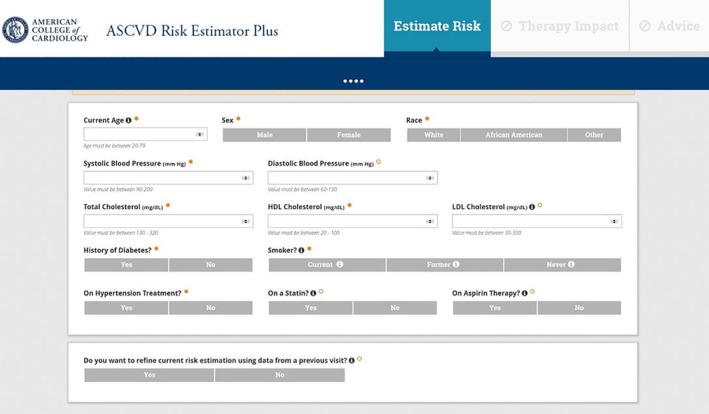
ASCVD risk estimator plus
A detailed pregnancy history is an integral component of risk assessment for women, in that complications of pregnancy, specifically preeclampsia, gestational diabetes, pregnancy‐induced hypertension, preterm delivery, and small for gestational age infants, are early indicators of an increased cardiovascular risk. More specifically, preeclampsia and gestational diabetes impart a 3‐ to 6‐fold increased risk for subsequent hypertension, a 2‐fold increased risk of ischemic heart disease and stroke. And although many manifestations of preeclampsia subside with the delivery of the placenta, there remains residual endothelial dysfunction, and this is associated with an increase in coronary artery calcium.9
Systemic autoimmune disorders are highly prevalent in women and increase the risk of coronary heart disease and cerebrovascular accident. Indeed, coronary disease is the leading cause of morbidity and mortality in women with systemic lupus erythematosus. There is a 2‐ to 3‐fold increase in myocardial infarction and cardiovascular mortality in women with rheumatoid arthritis, and an increased risk of cardiovascular events with psoriatic arthritis, warranting screening for traditional cardiovascular risk factors in such women.10, 11
For adults 40 to 75 years, the Guideline recommends that clinicians routinely assess cardiovascular risk factors and calculate the 10‐year ASCVD risk score. At age 20 to 39 years, it is reasonable to assess traditional risk factors at least every 4 to 6 years. In this younger population, however, the pregnancy‐associated risk factors may uniquely identify the younger woman at increased risk. In adults at borderline risk (5% to <7.5%) 10‐year ASCVD risk, or intermediate risk (≥ 7.5% to <20%) 10‐year ASCVD risk, it is reasonable to use additional risk enhancing factors to guide decisions about preventive interventions (eg, statin therapy). For adults at borderline risk and with uncertain evidence‐based indications for preventive interventions, it is reasonable to measure a coronary artery calcium score to guide clinician/patient risk discussions. This may be particularly relevant for women in that in the MESA database, women in the highest quintile of coronary calcium had a low risk Framingham risk score.12
To insure a female‐friendly focus, the clinician/patient discussion should further highlight that traditional risk factors often impart a selectively high risk for women, as well as the non‐traditional risk factors identified above, and that some interventions offer greater benefit for women.
Nutrition/diet
Diet should emphasize the intake of vegetables, fruits, legumes, nuts, and fish.
Dietary issues are particularly relevant as regards obesity (see below) and for women with type 2 diabetes mellitus.
Exercise and physical activity
Recommendations are that adults engage in at least 150 minutes weekly of moderate‐intensity or 75 minutes of vigorous‐intensity aerobic physical activity.
In the INTERHEART Study, the protective effects of exercise were greater for women than for men,13 yet physical inactivity is the most prevalent risk factor for U.S. women. One‐fourth of U.S. women report no regular physical activity and ¾ describe less than the recommended amount of activity. This is despite female‐specific data from the Nurses Health Study showing the lesser development of diabetes in women who exercised regularly and a decreased risk of cardiovascular events in diabetic women who exercised..14, 15
Overweight and obesity
In individuals with overweight and obesity, weight loss is recommended to improve the ASCVD risk profile. Obesity is identified as a body mass index (BMI) ≥ 30 kg/m2 and overweight as a BMI = 25 to 29 kg/m2.
Two of three U.S women are obese or overweight (2010 data); and obesity is associated with hypertension, dyslipidemia, physical inactivity, and insulin resistance. Obesity increases coronary risk by 64% in women, compared with 46% in men.
-
Type 2 diabetes mellitus
Diabetes confers greater cardiovascular risk for women than for men, 19.1% vs 10.1%. It is associated with a 40% increased risk of incident coronary heart disease and a 25% increased risk of stroke. Importantly, in most studies diabetic women compared with diabetic men have lesser treatment and control of conventional cardiovascular risk factors.16
A tailored nutrition plan focusing on a healthy dietary pattern is recommended to improve glycemic control and achieve weight loss if needed, and physical activity guidelines are noted above. It is reasonable to initiate metformin as first line therapy at the diagnosis of diabetes. With additional ASCVD risk factors a sodium‐glucose cotransporter‐2 (SGLC‐2) inhibitor or a glucagon‐like peptide‐1 receptor (GLP‐1R) agonist is prudent to improve glycemic control and reduce CVD risk. Diabetic women have a greater burden of traditional ASCVD risk factors, and risk factor control is often suboptimal in diabetic women.17, 18, 19, 20
-
High blood cholesterol
Hypercholesterolemia imposes the highest population‐adjusted cardiovascular risk for women, 47%, with similar statin benefit evident for women and men.13, 21
For adults at intermediate risk, a decision should be made for moderate‐intensity statin therapy; in high‐risk patients, cholesterol level should be reduced by 50% or more. In adults with diabetes, moderate‐intensity statin therapy is indicated. Lifestyle modifications include weight loss, a heart healthy dietary pattern, sodium reduction, dietary potassium supplementation, increased physical activity and limited alcohol intake.
High blood pressure or hypertension
Use of blood pressure lowering medications is recommended for primary prevention with a systolic blood pressure of 130 mm Hg or higher and a diastolic pressure of 80 mm Hg or higher.
Although more men than women have hypertension up to age 45, after age 65 the occurrence of hypertension increases sharply in U.S. women with 80% of women aged 75 and older having hypertension. Important for preventive interventions, there is an impressive correlation of increased BMI with increased systolic blood pressure in women.22
Tobacco use
Tobacco use status should be assessed at every healthcare visit, with a goal of tobacco abstinence.
Women cigarette smokers have a 25% increased cardiovascular risk compared with similarly aged men who smoke, and cigarette smoking triples the risk for MI for women.23
Psychosocial issues, particularly depression, preferentially disadvantage women. In the INTERHEART study,13 psychosocial factors were associated with greater cardiovascular mortality in women than men, 45.2% vs 28.8%. The increased cardiovascular mortality with depression appears independent of the severity of depression. It is uncertain whether the increased mortality is due to high‐risk behaviors, non‐adherence to therapies, or other features.
Aspirin use
Low‐dose aspirin may be considered for the primary prevention of ASCVD among selected adults at higher ASCVD risk, but not at increased bleeding risk. It should not be routinely used for primary prevention among adults older than age 70.
Consideration of cardiovascular risk factors unique to or predominant in women as risk‐enhancing features in clinician/patient preventive shared decision‐making discussions will likely result in an improved spectrum of care for women.
Wenger NK. Female‐friendly focus: 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Clin Cardiol. 2019;42:706–709. 10.1002/clc.23218
REFERENCES
- 1. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. J Am Coll Cardiol. 2019. 10.1016/j.jacc.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu P, Haththotuwa R, Kwok CS, et al. Preeclampsia and future cardiovascular health: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. [DOI] [PubMed] [Google Scholar]
- 3. Tanz LJ, Stuart JJ, Williams PL, et al. Preterm delivery and maternal cardiovascular disease in young and middle‐aged adult women. Circulation. 2017;135:578‐589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. del Rincon ID, Williams K, Stern MP, et al. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001;44:2737‐2745. [DOI] [PubMed] [Google Scholar]
- 5. Manzi S, Mellahn EN, Rairie JE, et al. Age‐specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol. 1997;145:408‐415. [DOI] [PubMed] [Google Scholar]
- 6. Triant VA, Perez J, Regan S, et al. Cardiovascular risk prediction functions underestimate risk in HIV infection. Circulation. 2018;137:2203‐2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wellons M, Ouyang P, Schreiner PJ, Herrington DM, Vaidya D. Early menopause predicts future coronary heart disease and stroke: the multi‐ethnic study of atherosclerosis. Menopause. 2012;19:1081‐1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in south Asians in the United States: epidemiology, risk factors, and treatments: a Scientific Statement from the American Heart Association. Circulation. 2018;138:e1‐e34. [DOI] [PubMed] [Google Scholar]
- 9. Wenger NK. Recognizing pregnancy‐associated cardiovascular risk factors. Am J Cardiol. 2014;113:406‐409. [DOI] [PubMed] [Google Scholar]
- 10. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness‐based guidelines for the prevention of cardiovascular disease in women – 2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243‐1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang J, Chen L, Delzell E, et al. The association between inflammatory markers, serum lipids and the risk of cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis. 2014;73:1301‐1308. [DOI] [PubMed] [Google Scholar]
- 12. Lakoski SG, Greenland P, Wong ND, et al. Coronary artery calcium scores and risk for cardiovascular events in women classified as “low‐risk” based on Framingham risk score. The Multi‐Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2007;167:2437‐2442. [DOI] [PubMed] [Google Scholar]
- 13. Yusuf S, Hawken S, Ounpuu S, et al. On behalf of the INTERHEART study investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:937‐952. [DOI] [PubMed] [Google Scholar]
- 14. Manson JE, Rimm EB, Stampfer MJ, et al. Physical activity and incidence of non‐insulin‐dependent diabetes mellitus in women. Lancet. 1991;338:774‐778. [DOI] [PubMed] [Google Scholar]
- 15. Hu FB, Stampfer MJ, Solomon C, et al. Physical activity and risk for cardiovascular events in diabetic women. Ann Intern Med. 2002;134:96‐105. [DOI] [PubMed] [Google Scholar]
- 16. Kalyani RR, Lazo M, Ouyang P, et al. Sex differences in diabetes and risk of incident coronary artery disease in healthy young and middle‐aged adults. Diabetes Care. 2014;37:830‐838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non‐diabetes than men? The British Regional Heart Study and the British Women's Heart Health Study. Diabetologia. 2012;55:80‐87. [DOI] [PubMed] [Google Scholar]
- 18. Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta‐analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542‐1551. [DOI] [PubMed] [Google Scholar]
- 19. Wexler DJ, Nathan DM, Grant RW, et al. Sex disparities in treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28:514‐520. [DOI] [PubMed] [Google Scholar]
- 20. Regensteiner JG, Golden S, Huebschmann AG, et al., on behalf of the Council on Lifestyle and Cardiometabolic Health, Council on Epidemiology and Prevention, Council on Functional Genomics and Translational Biology, and Council on Hypertension. Sex differences in the cardiovascular consequences of diabetes mellitus. A Scientific Statement from the American Heart Association. Circulation. 2015;132:2424‐2447. [DOI] [PubMed] [Google Scholar]
- 21. Kostis WJ, Cheng JQ, Dobrzynski JM, Cabrera J, Kostis JB. Meta‐analysis of statin effects in women versus men. J Am Coll Cardiol. 2012;59:572‐581. [DOI] [PubMed] [Google Scholar]
- 22. Wenger NK, Arnold A, Baiey Merz CN, et al. Hypertension across a woman's life cycle. J Am Coll Cardiol. 2018;71:1797‐1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta‐analysis of prospective cohort studies. Lancet. 2011;378:1297‐1305. [DOI] [PubMed] [Google Scholar]


