Abstract
People with bipolar disorder frequently experience persistent residual symptoms, problems in psychosocial functioning, cognitive impairment, and poor quality of life. In the last decade, the treatment target in clinical and research settings has focused not only on clinical remission, but also on functional recovery and, more lately, in personal recovery, taking into account patients’ well-being and quality of life. Hence, the trend in psychiatry and psychology is to treat bipolar disorder in an integrative and holistic manner. This literature review offers an overview regarding psychosocial functioning in bipolar disorder. First, a brief summary is provided regarding the definition of psychosocial functioning and the tools to measure it. Then, the most reported variables influencing the functional outcome in patients with bipolar disorder are listed. Thereafter, we include a section discussing therapies with proven efficacy at enhancing functional outcomes. Other possible therapies that could be useful to prevent functional decline and improve functioning are presented in another section. Finally, in the last part of this review, different interventions directed to improve patients’ well-being, quality of life, and personal recovery are briefly described.
Keywords: bipolar disorder, psychotherapy, functional outcome, quality of life
Introduction
Bipolar disorder (BD) is a recurrent and chronic disorder characterized by fluctuations in mood state and energy that affects around 2.4% of the global population (Merikangas et al., 2011). As a lifelong and recurrent illness, BD is associated with functional decline, cognitive impairment, and a reduction in quality of life (QoL) (Martínez-Arán et al., 2004; Michalak et al., 2005; Bonnín et al., 2012). Given the complexity of this illness and its consequences, researchers and clinicians are not only focused on clinical remission but also functional recovery and, more lately, well-being too (Vieta and Torrent, 2016). This emergent paradigm includes not only symptom recovery but also return to normal functioning and attainment of a meaningful life. In fact, in 1988, Dion and colleagues already pointed out that factors other than symptoms were related to functioning of patients with BD and that treatment should target symptom amelioration as well as reduce a patient’s disability (Dion et al., 1988). It is known that even after the first manic episode, only 1 out of 3 patients regains psychosocial functioning at 1 year follow-up (Tohen et al., 2000), suggesting that functional outcomes in BD are undoubtedly impaired from the very beginning and should become a priority in therapeutic interventions.
In the last decade, many efforts have been made to improve functioning and well-being in BD; hence, this review aims at providing a brief overview of both issues. First, the definition and how to measure functioning is discussed. Then, a brief review of the variables influencing psychosocial functioning is performed. The following sections present some treatments that have proven to be effective at enhancing functional outcomes and other promising treatments that might also be useful at targeting functional impairment and prevent functional decline. Finally, a brief overview of therapies directed to improve well-being and QoL is also presented.
Definition of Psychosocial Functioning and How to Measure It
Despite the importance of psychosocial functioning in BD there is not a clear consensus regarding its definition. In the Task Force for the International Society for Bipolar Disorders conducted by Tohen and colleagues in 2009, different definitions of psychosocial functioning were examined but without reaching a consensus. The experts highlighted the definition provided by the International Classification of Functioning, Disability and Health (ICF) in which functioning comprises 3 different components: body structures and functions; activities and participation; and personal environmental factors. Moreover, the authors of these guidelines underlined that this construct was complex to measure and that besides the ICF, the Functioning Assessment Short Thest (FAST) scale (Rosa et al., 2007) might also constitute a good approach to measure functioning (Tohen et al., 2009). Before these guidelines, there were other attempts to define psychosocial functioning. For instance, in 2000, Zarate and colleagues suggested the assessment of psychosocial functioning should involve different behavioral domains such as the individuals’ ability to function socially or occupationally, to live independently, and to engage in a romantic life, with functional recovery typically being defined as the restoration of normal role functioning in the domains under scrutiny (Zarate et al., 2000). This definition represented a breakthrough in the field because in that moment, psychosocial functioning was measured by means of the Global Assessment Functioning Scale (GAF), endorsed by several consecutive editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM). The GAF provides 1 single score without differentiating between the behavioral domains pointed by Zarate and colleagues. Despite all, the GAF is still the most commonly used clinician rating scale to measure disability, at least in the United States (Von Korff et al., 2011). In 2007, Rosa and colleagues developed a tool to measure functioning, the already mentioned FAST scale. It was specifically created to measure the most common difficulties experienced by patients with BD. The rationale behind this scale is in line with the definition of functioning proposed by Zarate and colleagues in 2000, mostly focused on the assessment of different behavioral domains. More specifically, the FAST targets the following areas: autonomy, occupational functioning, cognitive functioning, financial issues, interpersonal functioning, and leisure time. In this regard, the FAST represented several advantages over the GAF, mainly that it assesses different behavioral domains, it does not rate the symptomatology, and it is specific for BD.
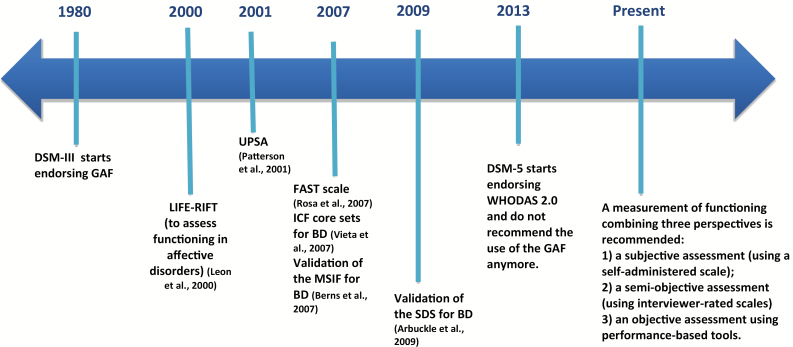
Currently, the DSM-5 no longer encourages the use of the GAF. Instead, the use of the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) (Üstün et al., 2010) is recommended. The WHODAS 2.0 allows the assessment of functioning and disability irrespective of diagnosis; that is, it can reflect difficulties due to any medical or psychiatric illness. In contrast, both the GAF and the FAST are limited to the impact of the psychiatric disease on functioning, excluding the medical or environmental limitations. The GAF, FAST, WHODAS 2.0, or ICF core sets specific for BD (Vieta et al., 2007; Ayuso-Mateos et al., 2013) are clinical tools, either rater administered (GAF, FAST, ICF core sets) or self-administered (WHODAS 2.0), but other approaches exist. For instance, the UCSD Performance-based skills Assessment (UPSA) (Patterson et al., 2001) is based on task performance and measures functional capacity, assessing the skills involved in community tasks such as comprehension and planning, finance, communication, mobility, and house management. Figure 1 represents an overview of some different scales available to measure functioning in BD during the last 40 years, starting in 1980, when the GAF was first endorsed by the DSM-III until the present.
Figure 1.
Timeline representing some scales to measure psychosocial functioning in bipolar disorder over the last 40 years. FAST, Functioning Assessment Short Test; GAF, Global Assessment of Functioning Scale; ICF, International Classification of Functioning, Disability, and Health; LIFE-RIFT, The Range of Impaired Functioning Tool; SDS, Sheehan Disability Scale; MSIF, Multidimensional Scale of Independent Functioning; UPSA, the UCSD Performance-based skills Assessment; WHODAS 2.0, World Health Organization Disability Assessment Schedule.
The scales presented in Figure 1 are just a little part of the big picture of the measurement of psychosocial functioning in BD. Nevertheless, it fairly represents the great variability that exists. It is likely that the way the researcher or clinician defines psychosocial functioning will determine the tool to measure it, but the reverse is true as well: the use of one tool or another implies how the concept of psychosocial functioning is understood. To overcome this bias, it would be ideal that psychosocial functioning could be measured taking into account 3 different perspectives: (1) a subjective view using a self-administered scale, such as the Sheehan Disability Scale for BD (SDS) (Arbuckle et al., 2009) or the WHODAS 2.0; (2) a semi-objective scale, using the FAST, GAF, or LIFE-RIFT (Leon et al., 1999), which are interviewer rated based on patients’ answers; and finally (3) an objective scale, like the UPSA, which is performance based and measures functional capacity. Combining these 3 different approaches might help to disentangle all the variables associated with functional impairment observed in BD.
Variables Influencing Functional Outcome in BD
Many variables have been associated with functional outcome in BD, including demographic, clinical, and neurocognitive factors. The brief summary presented below includes findings reported in some studies that use different scales, including the GAF, FAST, The Multidimensional Scale of Independent Functioning (Berns et al., 2007), and SDS among others. As mentioned above, there is a great variability not only in the assessment of functioning but also in the variables reported to influencing it. Despite this, the next paragraphs are useful to reveal the magnitude of the complex construct that researchers and clinicians are trying to predict.
Concerning the sociodemographic factors, it seems that male patients (Tohen et al., 1990; Sanchez-Moreno et al., 2018) as well as older patients (Sanchez-Moreno et al., 2018) show poorer functional outcomes. On the other hand, being married could represent a protective factor against functional impairment (Kupfer et al., 2002; Wingo et al., 2010). Higher socioeconomic status, based on education and employment, has also been associated with better functional outcomes (Keck et al., 1998; Wingo et al., 2010).
Regarding the clinical variables, the presence of subsyndromal depressive symptoms has been consistently reported as the strongest factor associated with functional impairment (Tohen et al., 1990; Bonnín et al., 2010, 2012; Gitlin et al., 2011; Gutiérrez-Rojas et al., 2011; Reinares et al., 2013; Samalin et al., 2016; Murru et al., 2018). Other clinical variables include history of psychosis, episode density, poor sleep quality, and longer illness duration (Huxley and Baldessarini, 2007; Sanchez-Moreno et al., 2009a, 2010; Reinares et al., 2013; Etain et al., 2017; Murru et al., 2018). Psychiatric comorbidity, particularly with substance use disorder (e.g., cannabis, alcohol) and personality disorders, can also negatively influence functional outcomes in patients with BD (Sánchez-Moreno et al., 2009b; Leen et al., 2013; Icick et al., 2017; Kizilkurt et al., 2018; Williams and Simms, 2018).
Finally, regarding neurocognitive variables, verbal memory has been found to be a good predictor of functional outcome in several studies (Martinez-Aran et al., 2007; Bonnín et al., 2010, 2014, Torres et al., 2011; Jiménez-López et al., 2018), However, variables related to other neurocognitive areas have also been reported, including executive functions, processing speed, and attention (Jaeger et al., 2007; Mur et al., 2009; Wingo et al., 2010). It might be hypothesized that the neurocognitive variables influencing functional outcome in BD may vary depending on illness progression. For instance, patients in early stages of the disease seem to present a more selective profile of cognitive impairment, with some domains capable of improving 1 year after the first manic episode, including improvements in processing speed and executive functions (Torres et al., 2014). In this line, at least 2 studies have found that first-episode patients who did not relapse during 1-year follow-up could improve their neurocognitive functioning (Kozicky et al., 2014; Demmo et al., 2018); hence, preserving neurocognition from the very beginning of the illness might guarantee better functional outcomes.
Restoring Psychosocial Functioning: Therapies That Have Improved Functional Outcome
Pharmacological Interventions
Research on pharmacological and nonpharmacological treatments to restore functioning in BD is still immature. As previously mentioned, the link between functional outcomes and neurocognition is well recognized, which is why in recent years many efforts have improved cognition, including both pharmacological and psychological treatments. In fact, new trends in pharmacological treatments include focusing on restoring cognitive functioning rather than psychosocial functioning. Among the most promising medical treatments to improve cognition in BD are mifepristone (Watson et al., 2012), lurasidone (Yatham et al., 2017), and erythropoietin (Miskowiak et al., 2014, 2015). Given the link between neurocognition and psychosocial functioning, it is likely that the efforts directed to improve neurocognition will also improve functional outcome; however, so far, no studies on pharmacological treatments have addressed both issues at the same time. It is worth mentioning that the methodological recommendations for cognition trials by the Cognition Task Force from the International Society for Bipolar Disorders encourage the inclusion of a functional measure as a key secondary outcome (Miskowiak et al., 2017). In this regard, a tool to measure functional improvement that allows the researchers and clinicians to classify patients into different categories of functional performance could be useful to assess the efficacy of these treatments (Bonnín et al., 2018a).
Psychological Therapies
In contrast to the area of pharmacological treatments, in the field of psychological interventions several efforts have been made lately to design therapies to restore psychosocial functioning in BD. The first attempt was an open trial using a program named Cognitive Rehabilitation (Deckersbach et al., 2010). The authors included a total of 18 patients with subsyndromal depressive symptoms and after 14 session of cognitive rehabilitation, patients improved cognitive performance and functional outcome. More interestingly, the findings showed that changes in executive function accounted, in part, for the improvements in occupational functioning. The first randomized controlled trial (RCT) implementing a similar therapy was conducted in 2013 by Torrent and colleagues (Torrent et al., 2013). The efficacy of functional remediation (FR) was proved in terms of improving functional outcomes in euthymic patients with moderate to severe functional impairment at baseline. Moreover, improvement in psychosocial functioning was maintained after 6 months’ follow-up (Bonnin et al., 2016). However, the impact of the intervention was low in terms of cognition. Contrary to others therapies labeled as “cognitive remediation,” FR is specially centered on functional recovery, focusing on the training of neurocognitive skills that are useful for daily functioning. Hence, this approach might be suitable especially for patients in late stages of the illness and who present moderate to severe functional impairment. Another preliminary study conducted in the Netherlands included 12 patients and replicated the positive results in functional outcome after receiving a shorter FR program (Zyto et al., 2016). However, not all the interventions targeting cognitive rehabilitation were found to improve functional outcome. For instance, another RCT conducted by Demant and colleagues (2015) found no improvement on either cognition or functional outcome after a 12-week intervention. It is worth mentioning that these negative results might be explained by some methodological limitations of the trial, including the length of the intervention (too short) or the fact that patients were subsyndromic at study enrolment. Another study leaded by Lewandowski and colleagues (2017) assessed the efficacy of an internet-based cognitive remediation program in patients with BD compared with an active control group both in neurocognition and community functioning. After treatment, patients who received the internet-based program improved cognitive performance in processing speed, visual learning and memory domains, and the composite score. These results were maintained over 6 months after finishing the intervention; however, the intervention was not associated with change in community functioning, although cognitive change was associated with functional change across the sample. There are other ongoing trials targeting cognition including action-based cognitive remediation programs in which computerized training is combined with practical in-session activities and cognitively challenging tasks between sessions. This novel approach may have greater effect at enhancing functional outcomes than traditional cognitive remediation programs (Bowie et al., 2017; Ott et al., 2018).
It is difficult to measure the power of these current approaches in changing functioning, since very few studies have used psychosocial functioning as a primary outcome. In this regard, meta-analyses providing these data are urgently needed.
How to Prevent Functional Decline: Promising Therapies
So far, there is no strong evidence regarding the prevention of functional decline in BD. The following section includes some targets and treatments that could address this issue and deserve to be further explored.
Addressing Subthreshold Depressive Symptoms
A considerable portion of the patients with BD (more than 50%) experience inter-episode residual depressive symptoms (De Dios et al., 2010; Gitlin et al., 1995), preventing them from living to the fullest. In this regard, subthreshold depressive symptoms together with neurocognitive impairment might be one of the strongest predictors of functional outcome (Bonnín et al., 2010, 2012, 2014; Reinares et al., 2013; Martinez-Aran and Vieta, 2015; Samalin et al., 2017). However, the relationship between functional outcome and subthreshold depressive symptoms might not be linear and unidirectional; instead, they seem to influence one another (Gitlin and Miklowitz, 2017; Weinstock and Miller, 2008). Besides the implications in functional outcome, residual depressive symptoms are also a major cause of relapse (Vieta and Garriga, 2016; Radua et al., 2017), consequently affecting psychosocial functioning and QoL (Bonnín et al., 2012; Xiang et al., 2014). The treatment of residual depressive symptoms during euthymia is an unmet need, but fortunately, clinical research has begun to investigate how to tackle them. One recent RCT proved that adjunctive extended-release quetiapine at a dose of 300 mg daily was significantly more effective than placebo in the treatment of subthreshold depressive symptoms (Garriga et al., 2017), but no significant improvement was detected in functional outcome. One possible explanation is that the sample size was not powered enough to detect significant changes in this secondary outcome.
Regarding psychological interventions, a limited number of therapies have addressed subthreshold depressive symptoms as a primary outcome. To the best of our knowledge, only one pilot RCT study assessed the effect of Eye Movement Desensitization and Reprocessing therapy on this type of symptomatology. Specifically, patients in the treatment group showed a statistically significant improvement in depressive and hypomanic symptoms when compared with treatment as usual at 12-month follow-up; however, psychosocial functioning was not assessed (Novo et al., 2014). Another multicenter study of Eye Movement Desensitization and Reprocessing with a bigger sample is underway with the objective to reduce symptoms and relapses and improve psychosocial functioning (Moreno-Alcázar et al., 2017). Regarding FR, secondary analyses showed that patients with subsyndromal symptoms could also improve psychosocial functioning after the therapy (Sanchez-Moreno et al., 2017).
Other therapies include an approach testing the long-term efficacy of an intervention that combined cognitive behavior therapy (CBT) and psychoeducation, which has also been described to be effective in terms of symptoms and social-occupational functioning improvement (González-Isasi et al., 2014). Positive results in social functioning were also found with CBT (Lam et al., 2003). Inder and colleagues (2015) randomized a group of patients with BD to Interpersonal and Social Rhythm Therapy or specialist supportive care, and both groups improved in depressive/manic symptoms and social functioning. Finally, an intensive psychotherapy (family-focused treatment [FFT], Interpersonal and Social Rhythm Therapy, or CBT) in patients with BD during an acute depressive episode also showed beneficial functional outcomes (Miklowitz et al., 2007a). Finally, positive results have also been reported on anxious and depressive symptoms using mindfulness-based cognitive therapy (Williams et al., 2008; Ives-Delipery et al., 2013; Perich et al., 2013).
Although more research is needed, it might be hypothesized that treating subthreshold depressive symptoms could be an indirect pathway to improve psychosocial functioning.
Enhancing Cognitive Reserve
Cognitive reserve (CR) is the capacity of the adult brain to endure neuropathology, minimizing clinical manifestations and allowing a successful accomplishment of cognitive tasks (Stern, 2009). Genetics determine, to some extent, CR; however, environmental factors such as an active lifestyle, education, and brain stimulation (mental activities) can also influence it. In BD the most common ways to measure CR include years of education, premorbid Intelligence Quotient, and leisure activities. So far, no interventions have tested whether improving CR enhances functioning, but some studies suggest that CR is a good predictor of both cognitive and psychosocial outcome in euthymic patients with BD (Anaya et al., 2012; Forcada et al., 2015). Further, it could also play an important role in patients with first psychotic episode since CR has shown to predict psychosocial functioning 2 years after the first episode (Amoretti et al., 2016). Hence, given the role of CR both in chronic patients and at early stages, this might constitute an area to explore and enhance to prevent functional decline (Vieta, 2015). In this regard, there is another ongoing trial by Torrent and colleagues (NCT03722082) that aims to enhance CR in child, adolescent, and young adult offspring of patients diagnosed with schizophrenia or BD; however, so far, no preliminary results are available.
Diet and Physical Exercise
Nutrition and physical exercise play a critical role in both the mental and physical health of patients with BD. Physical inactivity and poor diet habits can contribute to obesity, diabetes, hypertension, and dyslipidemia, which, in turn, increase the risk for cardiovascular disease (Soreca et al., 2008). At any rate, these risk factors should be targeted since it has been shown that obesity can also impact cognitive functioning (Mora et al., 2017), and in turn, cognitive impairment could be a predictor of weight gain (Bond et al., 2017). Hence, it seems that weight increase and cognitive impairment can influence one another. Moreover, another study has found that increased body mass index (BMI) was associated with a more chronic course of the disease, longer duration of illness, and lower psychosocial functioning (Calkin et al., 2009). In line with this, Bond and colleagues (2010) found that those patients who suffered a clinically significant weight gain (defined as gaining ≥7% of baseline weight over 12 months) had significantly poorer functional outcomes at 12-month follow-up, and, interestingly, functional impairment was independent from current mood symptoms.
Poor dietary habits and a sedentary lifestyle can increase physical and psychiatric morbidity, worsen psychosocial and cognitive functioning, and predict a poor pharmacological response. That is why clinicians treating individuals with BD face a dual challenge of treating not only patients’ brains but also their bodies. Interventions targeting healthy habits (including nutrition and exercise) are expected to benefit patients with BD. One RCT examined the effects of a 20-week CBT intervention (NEW tx) for BD consisting of 3 modules: nutrition, exercise, and wellness (Sylvia et al., 2013); patients who underwent the treatment showed improvements in nutritional habits, exercise, depressive symptoms, and overall functioning. Hence, this study provides preliminary evidence that improving nutrition and promoting an active lifestyle is associated with functional improvement and mood symptoms in patients with BD. Another previous study showed the efficacy of an intervention on healthy lifestyle, nutrition, and physical exercise on muscle mass index, particularly in women (Gillhoff et al., 2010). These lifestyle interventions are promising since they demonstrate that people with BD can engage and be successful in these types of therapies. Therapeutic mechanisms of action are still unknown but might include different pathways, for example, by reducing morbidity (i.e., depressive symptoms), which in turn would improve functional outcome (Ernst et al., 2006), or by enhancing treatment effects, including the synergistic effects of exercise in combination with other treatments. For instance, in schizophrenia there is some preliminary evidence suggesting that cognitive remediation efficacy can be enhanced by aerobic exercise-induced BDNF upregulation (Nuechterlein et al., 2016; Campos et al., 2017).
Multicomponent Programs
One advantage of this type of intervention is to tackle different areas to be improved at the same time, hence, allowing a holistic treatment of patients, taking into account not only education on the illness but also how to improve healthy lifestyles and functional outcomes. Following the premise that no single psychosocial intervention might be sufficient to address the morbidity, the functional impairment and the consequences associated with severe mental illnesses (Kern et al., 2009), multicomponent programs, and care packages are being developed for patients with BD.
An example of this kind of treatment that has proven to be effective in BD is the Integrated Risk Reduction Intervention developed by Frank and colleagues (2015). More specifically, this program consists of 17 sessions grouped in different modules, including psychoeducation, training to improve sleep/wake patterns and social rhythm regularity, nutrition, physical activity, and healthy habits (smoking cessation). Results from this study showed that patients who followed the intervention significantly reduce their BMI. Moreover, 3 variables (C-reactive protein, total cholesterol, and instability of total sleep time) contributed to a combined moderator of faster decrease in BMI with Integrated Risk Reduction Intervention treatment.
Recently, the Bipolar Disorder and Depression Unit in Barcelona has developed an integrative approach consisting of therapeutic components of broader programs that the Barcelona Bipolar Disorders Program had previously developed and whose effectiveness had been proven separately, such as psychoeducation for patients (Colom et al., 2003), psychoeducation for family members (Reinares et al., 2008), and FR (Torrent et al., 2013). In addition, an important emphasis is given to the promotion of a healthy lifestyle, and a module focused on mindfulness-based cognitive therapy has also been included. Therefore, some contents of psychoeducation for patients have been combined with a session for family members and complemented with aspects related to health promotion, mindfulness training, and strategies for cognitive and functional enhancement, always as adjunctive to pharmacological treatment. This integrative approach combines the main components of different treatments to cover broader therapeutic objectives, to improve the prognosis of the disease in both clinical and functional aspects, as well as the well-being and QoL of those who suffer from BD (Reinares, Martínez-Arán and Vieta, in press). Due to the characteristics of the intervention (12 sessions of 90 minutes each), in case it shows its efficacy, it could be easily implemented in routine clinical care.
Personal Recovery: Well-being and QoL
Subjective assessments and patient-reported outcomes are gaining ground in the field of BD (Morton et al., 2017; Bonnín et al., 2018b). As in psychosocial functioning, the problem with subjective measures is the variability in the definitions and in the instruments to assess the subjective experience of these patients (Morton et al., 2017). It is common that terms such as QoL, well-being or life satisfaction are used as synonyms and interchangeable terms (Morton et al., 2017). Moreover, the current lack of consensus between these construct definitions add uncertainty and complication to select an appropriate instrument to measure this dimension. Despite all, the subjective experience should always be taken into account since it can also impact on the course of the illness. Some studies indicate that the improvement in well-being provides a protective effect against recurrence (Keyes et al., 2010), and it has also been found that low levels in QoL are associated with an increase in oxidative stress (Nunes et al., 2018). For this reason, it is important to evaluate not only objective outcomes (symptoms and functioning) but also to assess patients’ subjective experience, since they can provide valuable information and might be an essential part to ensure better outcomes in BD.
Pharmacological Interventions
Rajagopalan et al. (2016) tested the effects of lurasidone as monotherapy or as adjunctive to lithium/valproate on health-related QoL (HRQoL). They found that patients in both conditions increased HRQoL. However, this improvement was not independent of changes in depression, indicating that the effect of lurasidone on improving patient HRQoL may act through a reduction in depressive symptoms associated with BD. Similarly, Gonda and colleagues (2016) found that patients enhanced both their work functional outcome and QoL after receiving prophylactic lamotrigine therapy at 6-months follow-up. In young patients (10–17 years old) with an acute episode of bipolar depression, it was found that those who received olanzapine/fluoxetine combination presented better QoL scores compared with those receiving placebo (Walker et al., 2017).
Psychological Interventions
Even though physical activity is not a psychological intervention itself, it is well-known for increasing well-being and QoL; however, the impact of this kind of interventions has been less studied in the field of BD. Vancampfort and colleagues (2017) proved the effect of 150 min/wk of physical activity on physical, psychological, social, and environmental QoL; those patients who did not meet the established minimum (150 minutes) showed lower QoL outcomes.
Involving the family, O’Donnell and colleagues (2017) tested the effect of 2 psychological interventions on QoL scores in a sample of adolescents with BD. They compared the efficacy of a FFTplus pharmacotherapy vs brief psychoeducation plus pharmacotherapy on self-related QoL over 2 years. They found the 2 groups did not differ in overall QoL scores at 24 months follow-up. However, adolescents who received the FFT had greater improvements in quality of family relationships and physical well-being compared with the brief psychoeducation program. Besides, internet-based approaches using smartphones are gaining traction (Lauder et al., 2015; Hidalgo-Mazzei et al., 2018), representing a useful and attractive tool especially for the young population with BD (Bauer et al., 2018). So far, some preliminary studies using a mobile application (SIMPLe) have reported an improvement of biological rhythms (Hidalgo-Mazzei et al., 2017) and increased QoL and well-being (Hidalgo-Mazzei et al., 2018).
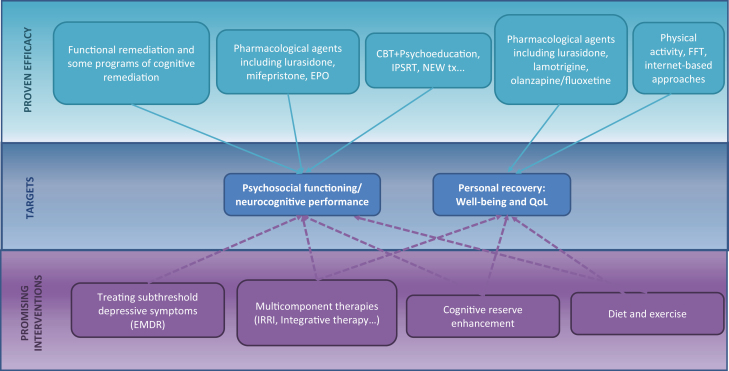
There is much room for improvement in the field of subjective well-being and QoL. These above-mentioned interventions may shed some light regarding the path to follow. Nevertheless, it is important to keep in mind that those patients who suffer from more depressive symptoms, irritability, and psychiatric comorbid conditions present lower QoL and functional outcomes (IsHak et al., 2012; Sylvia et al., 2017); hence, all the strategies directed to reduce medical and psychiatric burdens might also be useful to increase patients’ well-being and QoL. It is also worth mentioning that some authors defend that QoL depends not only on clinical remission but also relies on functional recovery (Vieta and Torrent, 2016). In this line, poor QoL is also associated with poor occupational outcome, reduced academic attainment (Marwaha et al., 2013), and difficulties in activities of daily life (Träger et al., 2017). Future studies should include subjective measures (such as QoL, well-being) to better understand the relationship with these clinical variables. Figure 2 represents a brief summary of the therapies and strategies that have been presented in this review.
Figure 2.
Overview of proven and promising therapies to treat bipolar disorder. CBT, cognitive behavioral therapy; EMDR, Eye Movement Desensitization and Reprocessing; EPO, erythropoietin; FFT, family-focused treatment; IPSRT, Interpersonal and Social Rhythm Therapy; IRRI, Integrated Risk Reduction Intervention; NEW tx, nutrition, exercise and wellness treatment; QoL, quality of life.
Conclusions
Because the construct of psychosocial functioning is complex and difficult to measure, it is therefore recommended to assess it based on the combination of 3 different approaches: (1) a subjective assessment that involves a self-administered measure (SDS, WHODAS 2.0, etc.), (2) a semi-objective measure including an interviewer-rated assessment (FAST, LIFE-RIFT, GAF, etc.), and (3) an objective assessment based on performance-based measurements (i.e., UPSA). Taking into account these different approaches might help to better disentangle the variables associated with the functional outcomes in BD, which are often heterogeneous and influenced by demographic, clinical, and neurocognitive factors.
Regardless of the great variability in the assessment of psychosocial functioning, many efforts have successfully improved functional outcomes in BD. But where are we now? At the present moment, the interventions that have proven to be effective at enhancing functioning and/or QoL include lurasidone, lamotrigine, FR, some programs of cognitive remediation, ISPRT, FFT, and NEW tx, among others. These therapies have set the stage for developing further interventions to prevent functional decline and ensure well-being, because this is where we go. Ideally, future therapies should focus not only on restoring functional outcomes but also preventing functional decline and enhancing QoL and well-being. In this regard, those programs that target cognitive enhancement and promote healthy lifestyles (including healthy nutrition patterns and physical activity) are urgently needed, since they constitute a preventive tool for cognitive and functional decline. Although more studies are still needed, multicomponent therapies might be also a good option since they include different approaches to cover several areas at a time (symptoms, functioning, cognition, well-being, etc.). Finally, it is likely that the future will also include personalized treatments focusing on tailored interventions that may differ from one patient to another (Salagre et al., 2018); in this sense, the type and duration of interventions might differ from patients recently diagnosed and patients with a complex course of the illness who might take advantage of restorative therapies such as cognitive and FR (Solé et al., 2017).
Statement of Interest
Dr Vieta has received grants and served as consultant, advisor, or CME speaker for the following identities: AB-Biotics, Abbott, Allergan, Angelini, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, Glaxo-Smith-Kline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, SAGE, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Generalitat de Catalunya (PERIS), the Spanish Ministry of Science and Innovation (CIBERSAM), EU Horizon 2020, and the Stanley Medical Research Institute. The other authors declare no conflicts of interest related to this manuscript.
Acknowledgments
The authors thank the Instituto de Salud Carlos III for the projects (PI12/01498, PI15/00330, PI17/00941) integrated into the Plan Nacional de I+D+I (co-funded by European Regional Development Fund/European Social Fund) “Investing in your future”); the CIBERSAM; and the Comissionat per a Universitats i Recerca del DIUE de la Generalitat de Catalunya to the Bipolar Disorders Group (2017 SGR 1365) and the CERCA Programme/Generalitat de Catalunya. This work has also been supported by the project SLT006/17/00357 in the “Pla estratègic de Recerca i Innovació en Salut 2016–2020.” Dr Bonnin would like to thank the Department de Salut de la Generalitat de Catalunya for the support through a PERIS grant (SLT002/16/00331)
References
- Amoretti S, Bernardo M, Bonnin CM, Bioque M, Cabrera B, Mezquida G, Solé B, Vieta E, Torrent C (2016) The impact of cognitive reserve in the outcome of first-episode psychoses: 2-year follow-up study. Eur Neuropsychopharmacol 26:1638–1648. [DOI] [PubMed] [Google Scholar]
- Anaya C, Martinez Aran A, Ayuso-Mateos JL, Wykes T, Vieta E, Scott J (2012) A systematic review of cognitive remediation for schizo-affective and affective disorders. J Affect Disord 142:13–21. [DOI] [PubMed] [Google Scholar]
- Arbuckle R, Frye MA, Brecher M, Paulsson B, Rajagopalan K, Palmer S, Degl’ Innocenti A (2009) The psychometric validation of the Sheehan Disability Scale (SDS) in patients with bipolar disorder. Psychiatry Res 165:163–174. [DOI] [PubMed] [Google Scholar]
- Ayuso-Mateos JL, Avila CC, Anaya C, Cieza A, Vieta E, Bipolar Disorders Core Sets Expert Group (2013) Development of the international classification of functioning, disability and health core sets for bipolar disorders: results of an international consensus process. Disabil Rehabil 35:2138–2146. [DOI] [PubMed] [Google Scholar]
- Bauer R, et al. (2018) Internet use by older adults with bipolar disorder: international survey results. Int J Bipolar Disord 6:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berns S, Uzelac S, Gonzalez C, Jaeger J (2007)Methodological considerations of measuring disability in bipolar disorder: validity of the Multidimensional Scale of Independent Functioning. Bipolar Disord 9:3–10. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Kunz M, Torres IJ, Lam RW, Yatham LN (2010) The association of weight gain with mood symptoms and functional outcomes following a first manic episode: prospective 12-month data from the Systematic Treatment Optimization Program for Early Mania (STOP-EM). Bipolar Disord 12:616–626. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Torres IJ, Lee SS, Kozicky JM, Silveira LE, Dhanoa T, Lam RW, Yatham LN (2017) Lower cognitive functioning as a predictor of weight gain in bipolar disorder: a 12-month study. Acta Psychiatr Scand 135:239–249. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Martínez-Arán A, Torrent C, Pacchiarotti I, Rosa AR, Franco C, Murru A, Sanchez-Moreno J, Vieta E (2010) Clinical and neurocognitive predictors of functional outcome in bipolar euthymic patients: a long-term, follow-up study. J Affect Disord 121:156–160. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Sánchez-Moreno J, Martínez-Arán A, Solé B, Reinares M, Rosa AR, Goikolea JM, Benabarre A, Ayuso-Mateos JL, Ferrer M, Vieta E, Torrent C (2012) Subthreshold symptoms in bipolar disorder: impact on neurocognition, quality of life and disability. J Affect Disord 136:650–659. [DOI] [PubMed] [Google Scholar]
- Bonnín Cdel M, González-Pinto A, Solé B, Reinares M, González-Ortega I, Alberich S, Crespo JM, Salamero M, Vieta E, Martínez-Arán A, Torrent C, CIBERSAM Functional Remediation Group (2014) Verbal memory as a mediator in the relationship between subthreshold depressive symptoms and functional outcome in bipolar disorder. J Affect Disord 160:50–54. [DOI] [PubMed] [Google Scholar]
- Bonnin CM, Torrent C, Arango C, Amann BL, Solé B, González-Pinto A, Crespo JM, Tabarés-Seisdedos R, Reinares M, Ayuso-Mateos JL, García-Portilla MP, Ibañez Á, Salamero M, Vieta E, Martinez-Aran A, CIBERSAM Functional Remediation Group (2016) Functional remediation in bipolar disorder: 1-year follow-up of neurocognitive and functional outcome. Br J Psychiatry 208:87–93. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Martínez-Arán A, Reinares M, Valentí M, Solé B, Jiménez E, Montejo L, Vieta E, Rosa AR (2018a) Thresholds for severity, remission and recovery using the functioning assessment short test (FAST) in bipolar disorder. J Affect Disord 240:57–62. [DOI] [PubMed] [Google Scholar]
- Bonnín CM, Yatham LN, Michalak EE, Martínez-Arán A, Dhanoa T, Torres I, Santos-Pascual C, Valls E, Carvalho AF, Sánchez-Moreno J, Valentí M, Grande I, Hidalgo-Mazzei D, Vieta E, Reinares M (2018b) Psychometric properties of the well-being index (WHO-5) Spanish version in a sample of euthymic patients with bipolar disorder. J Affect Disord 228:153–159. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Grossman M, Gupta M, Holshausen K, Best MW (2017) Action-based cognitive remediation for individuals with serious mental illnesses: effects of real-world simulations and goal setting on functional and vocational outcomes. Psychiatr Rehabil J 40:53–60. [DOI] [PubMed] [Google Scholar]
- Calkin C, van de Velde C, Růzicková M, Slaney C, Garnham J, Hajek T, O’Donovan C, Alda M (2009) Can body mass index help predict outcome in patients with bipolar disorder? Bipolar Disord 11:650–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos C, Rocha NBF, Lattari E, Nardi AE, Machado S (2017) Exercise induced neuroplasticity to enhance therapeutic outcomes of cognitive remediation in schizophrenia: analyzing the role of brain derived neurotrophic factor. CNS Neurol Disord Drug Targets 16:638–651. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Martinez-Aran A, Reinares M, Goikolea JM, Benabarre A, Torrent C, Comes M, Corbella B, Parramon G, Corominas J (2003) A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry 60:402–407. [DOI] [PubMed] [Google Scholar]
- Deckersbach T, Nierenberg AA, Kessler R, Lund HG, Ametrano RM, Sachs G, Rauch SL, Dougherty D (2010) RESEARCH: cognitive rehabilitation for bipolar disorder: an open trial for employed patients with residual depressive symptoms. CNS Neurosci Ther 16:298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Dios C, Ezquiaga E, Garcia A, Soler B, Vieta E (2010) Time spent with symptoms in a cohort of bipolar disorder outpatients in Spain: a prospective, 18-month follow-up study. J Affect Disord 125:74–81. [DOI] [PubMed] [Google Scholar]
- Demant KM, Vinberg M, Kessing LV, Miskowiak KW (2015) Effects of short-term cognitive remediation on cognitive dysfunction in partially or fully remitted individuals with bipolar disorder: results of a randomized controlled trial. PLoS One 10:e0127955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demmo C, Lagerberg TV, Kvitland LR, Aminoff SR, Hellvin T, Simonsen C, Haatveit B, Andreassen OA, Melle I, Ueland T (2018) Neurocognitive functioning, clinical course and functional outcome in first-treatment bipolar I disorder patients with and without clinical relapse: a 1-year follow-up study. Bipolar Disord 20:228–237. [DOI] [PubMed] [Google Scholar]
- Dion GL, Tohen M, Anthony WA, Waternaux CS (1988) Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hosp Community Psychiatry 39:652–657. [DOI] [PubMed] [Google Scholar]
- Etain B, Godin O, Boudebesse C, Aubin V, Azorin JM, Bellivier F, Bougerol T, Courtet P, Gard S, Kahn JP, Passerieux C, Leboyer M, Henry C, FACE-BD collaborators (2017) Sleep quality and emotional reactivity cluster in bipolar disorders and impact on functioning. Eur Psychiatry 45:190–197. [DOI] [PubMed] [Google Scholar]
- Ernst C, Olson AK, Pinel JP, Lam RW, Christie BR (2006) Antidepressant effects of exercise: evidence for an adult-neurogenesis hypothesis? J Psychiatry Neurosci 31:84–92. [PMC free article] [PubMed] [Google Scholar]
- Forcada I, Mur M, Mora E, Vieta E, Bartrés-Faz D, Portella MJ (2015) The influence of cognitive reserve on psychosocial and neuropsychological functioning in bipolar disorder. Eur Neuropsychopharmacol 25:214–222. [DOI] [PubMed] [Google Scholar]
- Frank E, Wallace ML, Hall M, Hasler B, Levenson JC, Janney CA, Soreca I, Fleming MC, Buttenfield J, Ritchey FC, Kupfer DJ (2015) An integrated risk reduction intervention can reduce body mass index in individuals being treated for bipolar I disorder: results from a randomized trial. Bipolar Disord 17:424–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriga M, Solé E, González-Pinto A, Selva-Vera G, Arranz B, Amann BL, Saiz-Ruiz J, Pérez-Blanco J, Vieta E (2017) Efficacy of quetiapine XR vs. Placebo as concomitant treatment to mood stabilizers in the control of subthreshold symptoms of bipolar disorder: results from a pilot, randomized controlled trial. Eur Neuropsychopharmacol 27:959–969. [DOI] [PubMed] [Google Scholar]
- Gillhoff K, Gaab J, Emini L, Maroni C, Tholuck J, Greil W (2010) Effects of a multimodal lifestyle intervention on body mass index in patients with bipolar disorder: a randomized controlled trial. Prim Care Companion J Clin Psychiatry 12 doi: 10.4088/PCC.09m00906yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin MJ, Miklowitz DJ (2017) The difficult lives of individuals with bipolar disorder: a review of functional outcomes and their implications for treatment. J Affect Disord 209:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin MJ, Mintz J, Sokolski K, Hammen C, Altshuler LL (2011) Subsyndromal depressive symptoms after symptomatic recovery from mania are associated with delayed functional recovery. J Clin Psychiatry 72:692–697. [DOI] [PubMed] [Google Scholar]
- Gitlin MJ, Swendsen J, Heller TL, Hammen C (1995) Relapse and impairment in bipolar disorder. Am J Psychiatry 152:1635–1640. [DOI] [PubMed] [Google Scholar]
- Gonda X, Kalman J, Dome P, Rihmer Z (2016) Changes in quality of life and work function during phase prophylactic lamotrigine treatment in bipolar patients: 6 month, prospective, observational study. Neuropsychopharmacol Hung 18:57–67. [PubMed] [Google Scholar]
- González Isasi A, Echeburúa E, Limiñana JM, González-Pinto A (2014) Psychoeducation and cognitive-behavioral therapy for patients with refractory bipolar disorder: a 5-year controlled clinical trial. Eur Psychiatry 29:134–141. [DOI] [PubMed] [Google Scholar]
- Gutiérrez-Rojas L, Jurado D, Gurpegui M (2011) Factors associated with work, social life and family life disability in bipolar disorder patients. Psychiatry Res 186:254–260. [DOI] [PubMed] [Google Scholar]
- Hidalgo-Mazzei D, Reinares M, Mateu A, Juruena MF, Young AH, Pérez-Sola V, Vieta E, Colom F (2017) Is a simple smartphone application capable of improving biological rhythms in bipolar disorder? J Affect Disord 223:10–16. [DOI] [PubMed] [Google Scholar]
- Hidalgo-Mazzei D, Reinares M, Mateu A, Nikolova VL, Bonnín CDM, Samalin L, García-Estela A, Pérez-Solá V, Young AH, Strejilevich S, Vieta E, Colom F (2018) OpenSIMPLe: a real-world implementation feasibility study of a smartphone-based psychoeducation programme for bipolar disorder. J Affect Disord 241:436–445. [DOI] [PubMed] [Google Scholar]
- Huxley N, Baldessarini RJ (2007) Disability and its treatment in bipolar disorder patients. Bipolar Disord 9:183–196. [DOI] [PubMed] [Google Scholar]
- Icick R, Gard S, Barde M, Carminati M, Desage A, Guillaume S, Scott J, Bellivier F, FondaMental Advanced Centers of Expertise in Bipolar Disorders (FACE-BD) Collaborators (2017) Physical and mental health burden in cases of bipolar disorder classified as current, former, or non-tobacco smokers. J Affect Disord 208:406–413. [DOI] [PubMed] [Google Scholar]
- Inder ML, Crowe MT, Luty SE, Carter JD, Moor S, Frampton CM, Joyce PR (2015) Randomized, controlled trial of Interpersonal and Social Rhythm Therapy for young people with bipolar disorder. Bipolar Disord 17:128–138. [DOI] [PubMed] [Google Scholar]
- IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R (2012) Health-related quality of life in bipolar disorder. Bipolar Disord 14:6–18. [DOI] [PubMed] [Google Scholar]
- Ives-Deliperi VL, Howells F, Stein DJ, Meintjes EM, Horn N (2013) The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: a controlled functional MRI investigation. J Affect Disord 150:1152–1157. [DOI] [PubMed] [Google Scholar]
- Jaeger J, Berns S, Loftus S, Gonzalez C, Czobor P (2007) Neurocognitive test performance predicts functional recovery from acute exacerbation leading to hospitalization in bipolar disorder. Bipolar Disord 9:93–102. [DOI] [PubMed] [Google Scholar]
- Jiménez-López E, Sánchez-Morla EM, Aparicio AI, López-Villarreal A, Martínez-Vizcaíno V, Rodriguez-Jimenez R, Vieta E, Santos JL (2018) Psychosocial functioning in patients with psychotic and non-psychotic bipolar I disorder. A comparative study with individuals with schizophrenia. J Affect Disord 229:177–185. [DOI] [PubMed] [Google Scholar]
- Keck PE Jr, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, Bourne ML, Haggard P (1998) 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry 155:646–652. [DOI] [PubMed] [Google Scholar]
- Kern RS, Glynn SM, Horan WP, Marder SR (2009) Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull 35:347–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CL, Dhingra SS, Simoes EJ (2010) Change in level of positive mental health as a predictor of future risk of mental illness. Am J Public Health 100:2366–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kizilkurt OK, Gulec MY, Giynas FE, Gulec H (2018) Effects of personality functioning on the global functioning of patients with bipolar disorder I. Psychiatry Res 266:309–316. [DOI] [PubMed] [Google Scholar]
- Kozicky JM, Torres IJ, Silveira LE, Bond DJ, Lam RW, Yatham LN (2014) Cognitive change in the year after a first manic episode: association between clinical outcome and cognitive performance early in the course of bipolar I disorder. J Clin Psychiatry 75:e587–e593. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA (2002) Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry 63:120–125. [DOI] [PubMed] [Google Scholar]
- Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, Parr-Davis G, Sham P (2003) A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry 60:145–152. [DOI] [PubMed] [Google Scholar]
- Lauder S, Chester A, Castle D, Dodd S, Gliddon E, Berk L, Chamberlain J, Klein B, Gilbert M, Austin DW, Berk M (2015) A randomized head to head trial of moodswings.net.au: an internet based self-help program for bipolar disorder. J Affect Disord 171:13–21. [DOI] [PubMed] [Google Scholar]
- Leen J, Soczynska JK, Gallaugher LA, Woldeyohannes HO, Alsuwaidan MT, Cha DS, Dale RM, Muzina DJ, Kennedy SH, McIntyre RS (2013) The effect of personality dimensions on functional outcomes in mood disorders. Adv Ther 30:671–683. [DOI] [PubMed] [Google Scholar]
- Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB (1999) The range of impaired functioning tool (LIFE-RIFT): a brief measure of functional impairment. Psychol Med 29:869–878. [DOI] [PubMed] [Google Scholar]
- Lewandowski KE, Sperry SH, Cohen BM, Norris LA, Fitzmaurice GM, Ongur D, Keshavan MS (2017) Treatment to enhance cognition in bipolar disorder (TREC-BD): efficacy of a randomized controlled trial of cognitive remediation versus active control. J Clin Psychiatry 78:e1242–e1249. [DOI] [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E (2015) Cognition as a target in schizophrenia, bipolar disorder and depression. Eur Neuropsychopharmacol 25:151–157. [DOI] [PubMed] [Google Scholar]
- Martínez-Arán A, Vieta E, Reinares M, Colom F, Torrent C, Sánchez-Moreno J, Benabarre A, Goikolea JM, Comes M, Salamero M (2004) Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry 161:262–270. [DOI] [PubMed] [Google Scholar]
- Martinez-Aran A, Vieta E, Torrent C, Sanchez-Moreno J, Goikolea JM, Salamero M, Malhi GS, Gonzalez-Pinto A, Daban C, Alvarez-Grandi S, Fountoulakis K, Kaprinis G, Tabares-Seisdedos R, Ayuso-Mateos JL (2007) Functional outcome in bipolar disorder: the role of clinical and cognitive factors. Bipolar Disord 9:103–113. [DOI] [PubMed] [Google Scholar]
- Marwaha S, Durrani A, Singh S (2013) Employment outcomes in people with bipolar disorder: a systematic review. Acta Psychiatr Scand 128:179–193. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, Ladea M, Medina-Mora ME, Ono Y, Posada-Villa J, Sagar R, Wells JE, Zarkov Z (2011) Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry 68:241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak EE, Yatham LN, Lam RW (2005) Quality of life in bipolar disorder: a review of the literature. Health Qual Life Outcomes 3:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, Thase ME, Calabrese JR, Marangell LB, Ostacher MJ, Patel J, Thomas MR, Araga M, Gonzalez JM, Wisniewski SR (2007) Intensive psychosocial intervention enhances functioning in patients with bipolar depression: results from a 9-month randomized controlled trial. Am J Psychiatry 164:1340–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miskowiak K, Burdick K, Martinez-Aran A, Bonnin C, Bowie C, Carvalho A, Gallagher P, Lafer B, López-Jaramillo C, Sumiyoshi T, McIntyre R, Schaffer A, Porter R, Torres I, Yatham L, Young A, Kessing L, Vieta E (2017) Methodological recommendations for cognition trials in bipolar disorder by the International Society for Bipolar Disorders Targeting Cognition Task Force. Bipolar Disord 19:614–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miskowiak KW, Ehrenreich H, Christensen EM, Kessing LV, Vinberg M (2014) Recombinant human erythropoietin to target cognitive dysfunction in bipolar disorder: a double-blind, randomized, placebo-controlled phase 2 trial. J Clin Psychiatry 75:1347–1355. [DOI] [PubMed] [Google Scholar]
- Miskowiak KW, Vinberg M, Macoveanu J, Ehrenreich H, Køster N, Inkster B, Paulson OB, Kessing LV, Skimminge A, Siebner HR (2015) Effects of erythropoietin on hippocampal volume and memory in mood disorders. Biol Psychiatry 78:270–277. [DOI] [PubMed] [Google Scholar]
- Mora E, Portella MJ, Martinez-Alonso M, Teres M, Forcada I, Vieta E, Mur M (2017) The impact of obesity on cognitive functioning in euthymic bipolar patients: a cross-sectional and longitudinal study. J Clin Psychiatry 78:e924–e932. [DOI] [PubMed] [Google Scholar]
- Moreno-Alcázar A, Treen D, Valiente-Gómez A, Sio-Eroles A, Pérez V, Amann BL, Radua J (2017) Efficacy of eye movement desensitization and reprocessing in children and adolescent with post-traumatic stress disorder: A meta-analysis of randomized controlled trials. Front Psychol 8:1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton E, Michalak EE, Murray G (2017) What does quality of life refer to in bipolar disorders research? A systematic review of the construct’s definition, usage and measurement. J Affect Disord 212:128–137. [DOI] [PubMed] [Google Scholar]
- Mur M, Portella MJ, Martinez-Aran A, Pifarre J, Vieta E (2009) Influence of clinical and neuropsychological variables on the psychosocial and occupational outcome of remitted bipolar patients. Psychopathology 42:148–156. [DOI] [PubMed] [Google Scholar]
- Murru A, Pacchiarotti I, Verdolini N, Reinares M, Torrent C, Geoffroy PA, Bellivier F, Llorca PM, Vieta E, Samalin L (2018) Modifiable and non-modifiable factors associated with functional impairment during the inter-episodic periods of bipolar disorder. Eur Arch Psychiatry Clin Neurosci 268:749–755. [DOI] [PubMed] [Google Scholar]
- Novo P, Landin-Romero R, Radua J, Vicens V, Fernandez I, Garcia F, Pomarol-Clotet E, McKenna PJ, Shapiro F, Amann BL (2014) Eye movement desensitization and reprocessing therapy in subsyndromal bipolar patients with a history of traumatic events: a randomized, controlled pilot-study. Psychiatry Res 219:122–128. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Ventura J, McEwen SC, Gretchen-Doorly D, Vinogradov S, Subotnik KL (2016) Enhancing cognitive training through aerobic exercise after a first schizophrenia episode: theoretical conception and pilot study. Schizophr Bull 42:S44–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes CS, Maes M, Roomruangwong C, Moraes JB, Bonifacio KL, Vargas HO, Barbosa DS, Anderson G, de Melo LGP, Drozdstoj S, Moreira E, Carvalho AF, Nunes SOV (2018) Lowered quality of life in mood disorders is associated with increased neuro-oxidative stress and basal thyroid-stimulating hormone levels and use of anticonvulsant mood stabilizers. J Eval Clin Pract 24:869–878. [DOI] [PubMed] [Google Scholar]
- O’Donnell LA, Axelson DA, Kowatch RA, Schneck CD, Sugar CA, Miklowitz DJ (2017) Enhancing quality of life among adolescents with bipolar disorder: a randomized trial of two psychosocial interventions. J Affect Disord 219:201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott CV, Vinberg M, Bowie CR, Christensen EM, Knudsen GM, Kessing LV, Miskowiak KW (2018) Effect of action-based cognitive remediation on cognition and neural activity in bipolar disorder: study protocol for a randomized controlled trial. Trials 19:487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV (2001) UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull 27:235–245. [DOI] [PubMed] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR (2013) The association between meditation practice and treatment outcome in mindfulness-based cognitive therapy for bipolar disorder. Behav Res Ther 51:338–343. [DOI] [PubMed] [Google Scholar]
- Radua J, Grunze H, Amann BL (2017) Meta-analysis of the risk of subsequent mood episodes in bipolar disorder. Psychother Psychosom 86:90–98. [DOI] [PubMed] [Google Scholar]
- Rajagopalan K, Bacci ED, Ng-Mak D, Wyrwich K, Pikalov A, Loebel A (2016) Effects on health-related quality of life in patients treated with lurasidone for bipolar depression: results from two placebo controlled bipolar depression trials. BMC Psychiatry 16:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinares M, Colom F, Sánchez-Moreno J, Torrent C, Martínez-Arán A, Comes M, Goikolea JM, Benabarre A, Salamero M, Vieta E (2008) Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: a randomized controlled trial. Bipolar Disord 10:511–519. [DOI] [PubMed] [Google Scholar]
- Reinares M, Papachristou E, Harvey P, Mar Bonnín C, Sánchez-Moreno J, Torrent C, Ayuso-Mateos JL, Ploubidis GB, Vieta E, Frangou S (2013) Towards a clinical staging for bipolar disorder: defining patient subtypes based on functional outcome. J Affect Disord 144:65–71. [DOI] [PubMed] [Google Scholar]
- Reinares M, Martínez-Arán A, Vieta E. In press. Psychotherapy for Bipolar Disorders: An Integrative Approach. Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- Rosa AR, Sánchez-Moreno J, Martínez-Aran A, Salamero M, Torrent C, Reinares M, Comes M, Colom F, Van Riel W, Ayuso-Mateos JL, Kapczinski F, Vieta E (2007) Validity and reliability of the Functioning Assessment Short Test (FAST) in bipolar disorder. Clin Pract Epidemiol Ment Health 3:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salagre E, Dodd S, Aedo A, Rosa A, Amoretti S, Pinzon J, Reinares M, Berk M, Kapczinski FP, Vieta E, Grande I (2018) Toward precision psychiatry in bipolar disorder: staging 2.0. Front Psychiatry 9:641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samalin L, Boyer L, Murru A, Pacchiarotti I, Reinares M, Bonnin CM, Torrent C, Verdolini N, Pancheri C, de Chazeron I, Boucekine M, Geoffroy PA, Bellivier F, Llorca PM, Vieta E (2017) Residual depressive symptoms, sleep disturbance and perceived cognitive impairment as determinants of functioning in patients with bipolar disorder. J Affect Disord 210:280–286. [DOI] [PubMed] [Google Scholar]
- Samalin L, de Chazeron I, Vieta E, Bellivier F, Llorca PM (2016) Residual symptoms and specific functional impairments in euthymic patients with bipolar disorder. Bipolar Disord 18:164–173. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Bonnín C, González-Pinto A, Amann BL, Solé B, Balanzá-Martínez V, Arango C, Jimenez E, Tabarés-Seisdedos R, Garcia-Portilla MP, Ibáñez A, Crespo JM, Ayuso-Mateos JL, Vieta E, Martinez-Aran A, Torrent C, CIBERSAM Functional Remediation Group (2017) Do patients with bipolar disorder and subsyndromal symptoms benefit from functional remediation? A 12-month follow-up study. Eur Neuropsychopharmacol 27:350–359. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Bonnin CM, González-Pinto A, Amann BL, Solé B, Balanzá-Martinez V, Arango C, Jiménez E, Tabarés-Seisdedos R, Garcia-Portilla MP, Ibáñez A, Crespo JM, Ayuso-Mateos JL, Martinez-Aran A, Torrent C, Vieta E, CIBERSAM Functional Remediation Group (2018) Factors associated with poor functional outcome in bipolar disorder: sociodemographic, clinical, and neurocognitive variables. Acta Psychiatr Scand 138:145–154. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Martinez-Aran A, Tabarés-Seisdedos R, Torrent C, Vieta E, Ayuso-Mateos JL (2009a) Functioning and disability in bipolar disorder: an extensive review. Psychother Psychosom 78:285–297. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Martinez-Aran A, Colom F, Scott J, Tabares-Seisdedos R, Sugranyes G, Torrent C, Daban C, Benabarre A, Goikolea JM, Franco C, González-Pinto A, Ayuso-Mateos JL, Vieta E (2009b) Neurocognitive dysfunctions in euthymic bipolar patients with and without prior history of alcohol use. J Clin Psychiatry 70:1120–1127. [DOI] [PubMed] [Google Scholar]
- Sanchez-Moreno J, Martinez-Aran A, Gadelrab HF, Cabello M, Torrent C, Bonnin Cdel M, Ferrer M, Leonardi M, Ayuso-Mateos JL, Vieta E (2010) The role and impact of contextual factors on functioning in patients with bipolar disorder. Disabil Rehabil 32:S94–S104. [DOI] [PubMed] [Google Scholar]
- Solé B, Jiménez E, Torrent C, Reinares M, Bonnin CDM, Torres I, Varo C, Grande I, Valls E, Salagre E, Sanchez-Moreno J, Martinez-Aran A, Carvalho AF, Vieta E (2017) Cognitive impairment in bipolar disorder: treatment and prevention strategies. Int J Neuropsychopharmacol 20:670–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soreca I, Fagiolini A, Frank E, Houck PR, Thompson WK, Kupfer DJ (2008) Relationship of general medical burden, duration of illness and age in patients with bipolar I disorder. J Psychiatr Res 42:956–961. [DOI] [PubMed] [Google Scholar]
- Stern Y. (2009) Cognitive reserve. Neuropsychologia 47:2015–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvia LG, Salcedo S, Bernstein EE, Baek JH, Nierenberg AA, Deckersbach T (2013) Nutrition, exercise, and wellness treatment in bipolar disorder: proof of concept for a consolidated intervention. Int J Bipolar Disord 1:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvia LG, Montana RE, Deckersbach T, Thase ME, Tohen M, Reilly-Harrington N, McInnis MG, Kocsis JH, Bowden C, Calabrese J, Gao K, Ketter T, Shelton RC, McElroy SL, Friedman ES, Rabideau DJ, Nierenberg AA (2017) Poor quality of life and functioning in bipolar disorder. Int J Bipolar Disord 5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohen M, Waternaux CM, Tsuang MT (1990) Outcome in Mania. A 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry 47:1106–1111. [DOI] [PubMed] [Google Scholar]
- Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM (2000) Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry 157:220–228. [DOI] [PubMed] [Google Scholar]
- Tohen M, Frank E, Bowden CL, Colom F, Ghaemi SN, Yatham LN, Malhi GS, Calabrese JR, Nolen WA, Vieta E, Kapczinski F, Goodwin GM, Suppes T, Sachs GS, Chengappa KR, Grunze H, Mitchell PB, Kanba S, Berk M (2009) The international society for bipolar disorders (ISBD) task force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord 11:453–473. [DOI] [PubMed] [Google Scholar]
- Torrent C, et al. (2013) Efficacy of functional remediation in bipolar disorder: a multicenter randomized controlled study. Am J Psychiatry 170:852–859. [DOI] [PubMed] [Google Scholar]
- Torres IJ, DeFreitas CM, DeFreitas VG, Bond DJ, Kunz M, Honer WG, Lam RW, Yatham LN (2011) Relationship between cognitive functioning and 6-month clinical and functional outcome in patients with first manic episode bipolar I disorder. Psychol Med 41:971–982. [DOI] [PubMed] [Google Scholar]
- Torres IJ, Kozicky J, Popuri S, Bond DJ, Honer WG, Lam RW, Yatham LN (2014) 12-month longitudinal cognitive functioning in patients recently diagnosed with bipolar disorder. Bipolar Disord 16:159–171. [DOI] [PubMed] [Google Scholar]
- Träger C, Decker L, Wæhrens EE, Knorr U, Miskowiak K, Vinberg M (2017) Influences of patient informed cognitive complaints on activities of daily living in patients with bipolar disorder. An exploratory cross-sectional study. Psychiatry Res 249:268–274. [DOI] [PubMed] [Google Scholar]
- Ustün TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Saxena S, von Korff M, Pull C, WHO/NIH Joint Project (2010) Developing the World Health Organization disability assessment schedule 2.0. Bull World Health Organ 88:815–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancampfort D, Van Damme T, Probst M, Firth J, Stubbs B, Basangwa D, Mugisha J (2017) Physical activity is associated with the physical, psychological, social and environmental quality of life in people with mental health problems in a low resource setting. Psychiatry Res 258:250–254. [DOI] [PubMed] [Google Scholar]
- Vieta E. (2015) Personalised medicine applied to mental health: precision psychiatry. Rev Psiquiatr Salud Ment 8:117–118. [DOI] [PubMed] [Google Scholar]
- Vieta E, Cieza A, Stucki G, Chatterji S, Nieto M, Sánchez-Moreno J, Jaeger J, Grunze H, Ayuso-Mateos JL (2007) Developing core sets for persons with bipolar disorder based on the international classification of functioning, disability and health. Bipolar Disord 9:16–24. [DOI] [PubMed] [Google Scholar]
- Vieta E, Garriga M (2016) Adjunctive antidepressants in bipolar depression. Lancet Psychiatry 3:1095–1096. [DOI] [PubMed] [Google Scholar]
- Vieta E, Torrent C (2016) Functional remediation: the pathway from remission to recovery in bipolar disorder. World Psychiatry 15:288–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M, Andrews G, Delves M (2011) Assessing activity limitations and disability among adults. In: The conceptual evolution of DSM-5 (Regier DA, Narrow WA, et al., eds), 163–168. Washington, DC: American Psychiatric Publishing, Inc. [Google Scholar]
- Walker DJ, DelBello MP, Landry J, D’Souza DN, Detke HC (2017) Quality of life in children and adolescents with bipolar I depression treated with olanzapine/fluoxetine combination. Child Adolesc Psychiatry Ment Health 11:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson S, Gallagher P, Porter RJ, Smith MS, Herron LJ, Bulmer S, Young AH, Ferrier IN, North-East Mood Disorders Clinical Research Group (2012) A randomized trial to examine the effect of mifepristone on neuropsychological performance and mood in patients with bipolar depression. Biol Psychiatry 72:943–949. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Miller IW (2008) Functional impairment as a predictor of short-term symptom course in bipolar I disorder. Bipolar Disord 10:437–442. [DOI] [PubMed] [Google Scholar]
- Williams TF, Simms LJ (2018) Personality traits and maladaptivity: unipolarity versus bipolarity. J Pers 86:888–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, Hepburn S, Goodwin GM (2008) Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. J Affect Disord 107:275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo AP, Baldessarini RJ, Holtzheimer PE, Harvey PD (2010) Factors associated with functional recovery in bipolar disorder patients. Bipolar Disord 12:319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang YT, Li LJ, Zhou JJ, Wang CY, Dixon LB, Dickerson F, Zhou FC, Ungvari GS, Zhang XY, Shum DH, Au RW, Tang WK, Man D, Chiu HF (2014) Quality of life of patients with euthymic bipolar disorder and its associations with demographic and clinical characteristics, psychopathology, and cognitive deficits. Perspect Psychiatr Care 50:44–50. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Mackala S, Basivireddy J, Ahn S, Walji N, Hu C, Lam RW, Torres IJ (2017) Lurasidone versus treatment as usual for cognitive impairment in euthymic patients with bipolar I disorder: a randomized, open-label, pilot study. Lancet Psychiatry 4:208–217. [DOI] [PubMed] [Google Scholar]
- Zarate CA Jr, Tohen M, Land M, Cavanagh S (2000) Functional impairment and cognition in bipolar disorder. Psychiatr Q 71:309–329. [DOI] [PubMed] [Google Scholar]
- Zyto S, Jabben N, Schulte PF, Regeer BJ, Kupka RW (2016) A pilot study of a combined group and individual functional remediation program for patients with bipolar I disorder. J Affect Disord 194:9–15. [DOI] [PubMed] [Google Scholar]