Summary
Background
Evidence on the effectiveness of opioid agonist treatment (OAT) in reducing crime is mixed. We aimed to assess the effect of OAT on crime in terms of delaying time to first charge and reducing overall charge rates, as well as the relationship between OAT retention and overall charge rates.
Methods
We did a retrospective cohort study of opioid-dependent people who entered OAT for the first time between Jan 1, 2004, and Dec 30, 2010, in New South Wales (NSW), Australia. We used three linked NSW and national administrative datasets. Data on OAT were obtained from the Pharmaceutical Drugs of Addiction System, data on charges were obtained from the Reoffending Database, and data on mortality were obtained from the National Death Index. The cohort was followed up until Dec 31, 2011. Time-dependent OAT exposure was modelled using Cox proportional hazards models (time to first charge) and Andersen-Gill intensity models (total charge-days). Retention in OAT was modelled using two features of treatment engagement, number of OAT episodes and proportion of follow-up time in OAT (presented in quartile groupings: lowest, low-mid, low-high, highest) using zero-inflated negative binomial regression (total charges). All models were adjusted for sociodemographic, criminographic, and treatment-related variables.
Findings
10 744 new OAT entrants were included in the study. 5751 (53·5%) people were charged with an offence. In adjusted analyses, OAT was associated with an initial benefit in delaying the time to first charge (hazard ratio 0·43, 95% CI 0·33–0·55) and reducing total charge-days (0·39, 95% CI 0·30–0·52); however, these protective effects reduced over time. Total charge rates were higher as the number of OAT episodes increased (incident rate ratio [IRR] 1·13, 95% CI 1·11–1·15), and when relatively lower proportions of time were spent in OAT (IRR among the lowest three quartiles ranged from 1·11 [95% CI 1·02–1·21] to 1·22 [95% CI 1·12–1·33]).
Interpretation
OAT was associated with a reduction in overall charge rates and was more protective as treatment engagement increased. Maximising treatment retention is crucial to achieving long-term health and social benefits of OAT.
Introduction
Opioid dependence is a chronic disorder with many health and social consequences.1,2 In addition to the negative effects on morbidity and mortality,1 studies show a strong link between illicit opioid use and criminal activity.3–5 The onset of opioid use increases offending,6 and people who are opioid dependent are often in frequent contact with the criminal justice system, in terms of increased rates of offending, largely because of acquisitive crimes, and imprisonment.3,7 The corresponding societal costs and economic burden associated with crime arising from opioid dependence are especially pronounced.8,9
Opioid agonist treatment (OAT; methadone and buprenorphine) is one of the most widely used treatments for opioid dependence worldwide. Regarded as essential medicines by WHO, strong evidence exists that methadone and buprenorphine are effective in reducing heroin use,10 injecting risk,11 HIV and hepatitis C incidence,12 and mortality.1,13 In addition to these benefits, there is ongoing interest in examining the effectiveness of OAT in reducing contact with the criminal justice system to reduce the economic burden associated with opioid dependence.
Investigating the relationship between OAT and crime is complex, with randomised controlled trials14–16 and observational studies17–21 reporting varying effects depending on how treatment exposure has been assessed, and across treatment programmes and settings. For example, in a population-based study in Norway, reductions in crime were found in the period immediately before entry (or re-entry) into OAT, with increases in crime in the months before treatment interruption.17 Furthermore, continuous treatment was associated with the greatest crime reductions.18 Studies in Australia21 and Canada20 have documented lower offending rates during periods in which individuals were receiving methadone treatment than during periods without treatment. In the UK, crime reductions have been observed only during periods of continuous treatment with methadone, with non-continuous treatment having little benefit in reducing crime.19
Although these studies have documented important findings regarding the complexity of reducing crime in individuals in OAT, no study has comprehensively examined the effect of various OAT exposures on crime in a whole population and the effect of retention in OAT on crime is poorly understood. Using a population-based cohort of new OAT treatment entrants (including methadone and buprenorphine), we aimed to examine the effectiveness of OAT in reducing charge rates among opioid-dependent people. The specific objectives were to examine the effectiveness of OAT in delaying the time to first charge after entry into treatment, relative to time not spent in OAT; examine the effectiveness of OAT in reducing overall charge rates relative to time not spent in OAT; and examine the relationship between retention in OAT and reductions in overall charge rates.
Methods
Study design and setting
We did a retrospective population-based cohort study of opioid-dependent people who entered OAT for the first time between Jan 1, 2004, and Dec 30, 2010, in New South Wales (NSW), Australia. In Australia, treatment for opioid dependence is primarily focused on the provision of pharmacotherapy in the form of OAT. OAT is available from community pharmacies, public and private clinics, and correctional facilities; additional psychological services are generally limited to clinical and correctional settings. There is no charge for treatment in public clinics or correctional facilities; however, private clinics and community pharmacies charge their clients daily dispensing fees (typically AUS$5–8 per day). NSW is the most populous state of Australia (accounting for approximately 32% of the total population) and 40% of OAT recipients in Australia are estimated to reside in NSW.22
Ethics approval was obtained from the ethics committees of the NSW Aboriginal Health and Medical Research Council, University of New South Wales, NSW Health’s Population and Health Services Research Ethics Committee, the Australian Institute of Health and Welfare, the Alfred Hospital (Victoria), Corrective Services NSW, Justice Health and Forensic Mental Health Network (NSW Health), and the Department of Justice (Victoria).
Data sources
We used three linked NSW and national administrative datasets that record information on OAT episodes, involvement in the criminal justice system (charges and incarcerations), and death notifications. Records were linked probabilistically by external agencies using each individual’s full name, date of birth, sex, and date and state of last known contact and then de-identified.
Data on OAT (2004–11) were obtained from the Pharmaceutical Drugs of Addiction System (PHDAS). The PHDAS is a database of all recipients of methadone and buprenorphine or buprenorphine-naloxone in NSW. The database records each patient’s full name, date of birth, sex, and postcode of residence. Because proof of identity must be shown to the prescribing doctor before a prescription can be issued, the name and date of birth variables are of high accuracy in this dataset. The PHDAS records patient admissions and exits from the treatment programme and the medication dispensed.
Data on charges (2000–11) were obtained from the Reoffending Database (ROD). The ROD is maintained by the NSW Bureau of Crime Statistics and Research and contains records of all finalised court appearances (ie, court matters that are completed and have an outcome) in NSW. These appearances relate to a charge against an individual and include data on the date of appearance, date of offence, type of offence, and charge outcome (ie, proven or not). A proven charge is one in which the defendant pleaded guilty or was found guilty by a magistrate or jury. Validation studies have deemed that the internal matching process of records for individuals in the ROD has a specificity of 99·9% and sensitivity of 93·8%.25 All analyses are based on the offence date and include only proven charges. The ROD also contains incarceration records (2000–11) from the NSW Department of Corrective Services. These data include the dates of entry and exit for each prison episode.
Data on mortality (2000–11) were obtained from the National Death Index (NDI). The NDI is a database held by the Australian Institute of Health and Welfare that contains data on deaths from each Australian State or Territory. Dates of death were used for non-informative censoring.
Observation commenced on the date exactly 4 years before first entering OAT and ended on Dec 31, 2011, or the date of death, whichever was earlier. Charge rates could therefore be compared over a minimum 1-year period after initial entry into OAT (except in the case of death), while establishing a baseline charge history in the 4 years immediately before OAT entry (representing the average time lag before an individual enters treatment after becoming opioid dependent in NSW23). Ongoing opioid dependence was also assumed following first entry into OAT, given that opioid dependence is a chronic relapsing disorder with low remission rates.2,24
Statistical analysis
OAT exposure was examined in a time-dependent manner, accounting for each day a person was either in or out of treatment during the observation period. All models were adjusted for a range of sociodemographic (age, sex, Indigeneity), criminographic (time in prison during follow-up, and number of charges and prison episodes in the 4 years before OAT entry), and treatment-related variables (year of first OAT entry). Sensitivity analyses were done truncating the follow-up period to June 30, 2011, to examine the potential effect of not capturing offences that occurred on or before Dec 31, 2011, but were finalised after this date.
We used Cox proportional hazards regression to investigate the association between OAT exposure and the time to first charge following each person’s first entry into OAT. The effect of OAT on reducing overall charges, taking into account recurrent charges, was investigated using an Andersen-Gill intensity model.26 Because people could have multiple charges on the same day, the outcome of interest was charge-days. The resulting hazard ratio (HR) represents the proportionate change in the charge rate due to a change in treatment.
The proportional hazards assumption in the Cox and Andersen-Gill models were assessed visually with scaled Schoenfeld residuals plots and statistically with correlation tests of the Schoenfeld residuals with time. These investigations suggested that the HR of OAT versus not in OAT was time-dependent and time-varying models were considered. Parameter coefficients were exponentiated and were reported as HRs, and robust standard errors in the Andersen-Gill models allowed for dependency of multiple events within the same individual. Significance tests were done using two-sided tests at a level of 0·05.
The effect of OAT retention on the total number of charges during follow-up was investigated using zero-inflated negative binomial regression because of zero-inflation and overdispersion in the charge data. The appropriateness of the model was compared with negative binomial regression using the Vuong test and zero-inflated Poisson regression using likelihood-ratio tests.27 Parameter coefficients were reported as odds ratios (ORs) for the no charge component of the model, and incidence rate ratios (IRRs) for the number of charges component.
OAT retention was examined using two indicators of treatment engagement: total number of OAT episodes and proportion of follow-up time spent in OAT. A continuous treatment episode was defined as an episode with a break of 6 days or fewer between a treatment exit date and date of re-entry.28 The proportion of follow-up time each individual spent in OAT was categorised into four groups (lowest, low-mid, high-mid, and highest), with the quartile cutoff points determined using data on individuals with the same number of treatment episodes. Charges were categorised as occurring in or out of OAT on the basis of whether OAT was received on the date of the offence, irrespective of whether it occurred during a short (ie, ≤6 day) treatment break. All analyses were done using SAS (version 9.4).
Role of the funding source
The funders of the study had no role in study design, data analysis, data interpretation, or writing of the report. All authors had full access to all study data and had final responsibility for the decision to submit for publication.
Results
Of the 10 744 individuals in the cohort, most were men (7607 [70·8%]) and non-Indigenous (8277 [77·0%]; appendix p 4). The median age at OAT entry was 29·1 years (IQR 24·3–36·2). In the 4 years before OAT entry, 6459 (60·1%) individuals were charged with at least one offence and 3900 (36·3%) were incarcerated. The median length of follow-up was 4·4 years, ranging from 3 days to 8 years, with 379 (3·5%) recorded deaths. Approximately half of the cohort (49·4%) were not in treatment 1 year after OAT initiation (appendix p 6). 5751 (53·5%) people were charged with at least one offence during follow-up, with a cumulative total of 39 794 charges and 23 869 charge-days across the cohort (appendix p 5).
Table 1 presents the results examining the effectiveness of OAT in delaying the time to first charge. In the unadjusted analysis, OAT was found to delay the time to first charge (table 1 [model 1]). After adjusting for sex and age, OAT showed an initial benefit in delaying the time to first charge; however, this effect was not consistent over time (table 1 [model 2]). Similar results for OAT were observed in the model adjusting for all sociodemographic and criminographic variables (table 1 [model 3]). After a year from OAT initiation, the protective effect of OAT diminished and at 2 years post-initiation, OAT became positively associated with the time to first charge (appendix p 7).
Table 1:
Association between time spent in OAT and hazard of first charge
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| OAT* | |||
| In OAT | 0.82 (0.78–0.87) | 0.36 (0.28–0.46) | 0.43 (0.33–0.55) |
| In OAT x ln(time since OAT initiation)* | NA | 1.17 (1.12–1.22) | 1.15 (1.10–1.20) |
| Not in OAT (ref) | 1 | 1 | 1 |
| Sex | |||
| Male | 1.36 (1.28–1.44) | 1.40 (1.32–1.49) | 1.20 (1.13–1.27) |
| Female (ref) | 1 | 1 | 1 |
| Indigenous | |||
| Yes | 1.91 (1.80–2.02) | NA | 1.37 (1.29–1.46) |
| No (ref) | 1 | NA | 1 |
| Age at OAT initiation | |||
| <25 years | 2.08 (1.93–2.23) | 2.09 (1.95–2.25) | 1.57 (1.46–1.69) |
| 25–29 years | 1.62 (1.50–1.75) | 1.62 (1.50–1.75) | 1.40 (1.30–1.52) |
| 30–34 years | 1.45 (1.34–1.58) | 1.46 (1.34–1.59) | 1.31 (1.20–1.42) |
| ≥35 years (ref) | 1 | 1 | 1 |
| Year of OAT initiation | |||
| 2004–05 (ref) | 1 | NA | 1 |
| 2006–07 | 0.94 (0.89–1.01) | NA | 0.95 (0.89–1.02) |
| 2008–09 | 0.81 (0.75–0.86) | NA | 0.85 (0.79–0.91) |
| 2010–11 | 0.61 (0.55–0.67) | NA | 0.65 (0.59–0.72) |
| Number of charges in the 4 years before OAT initiation | |||
| 0 (ref) | 1 | NA | 1 |
| 1–4 | 2.29 (2.13–2.46) | NA | 2.14 (1.99–2.31) |
| 5–14 | 3.58 (3.34–3.84) | NA | 3.13 (2.86–3.42) |
| ≥15 | 4.51 (4.14–4.92) | NA | 4.02 (3.58–4.52) |
| In prison* | |||
| Yes | 0.56 (0.50–0.62) | NA | 0.23 (0.21–0.26) |
| No (ref) | 1 | NA | 1 |
| Number of prison episodes in the 4 years before OAT initiation | |||
| 0 (ref) | 1 | NA | 1 |
| 1–5 | 1.69 (1.57–1.82) | NA | 1.07 (0.98–1.17) |
| 6–10 | 2.29 (2.13–2.46) | NA | 1.31 (1.20–1.44) |
| ≥11 | 2.98 (2.75–3.22) | NA | 1.56 (1.40–1.74) |
Data include 10 744 people and 5751 charge-days. Data are HR (95% CI). Results are from Cox proportional hazards regressions. Model 1 used bivariate models. Model 2 included age, sex, treatment, and a time-dependent coefficient for “in OAT”. Model 3 was further adjusted for all sociodemographic and criminographic variables. OAT initiation refers to first entry into OAT. OAT=opioid agonist treatment. NA=not applicable. HR=hazard ratio.
Time-dependent variable.
Being in prison was associated with a reduction in the hazard of first charge, and those who were male, Indigenous, younger at OAT entry, and had more charges before entering OAT had an increased hazard of first charge (table 1 [model 3]).
Figure 1 compares the unadjusted simple 30-day moving average charge rate between time in and out of OAT across all 23 869 charge-days. Up until approximately 3 years after OAT initiation, people out of treatment had distinctively higher charge rates than did those in OAT.
Figure 1. Simple 30-day moving average daily charge rate for individuals in and out of OAT.
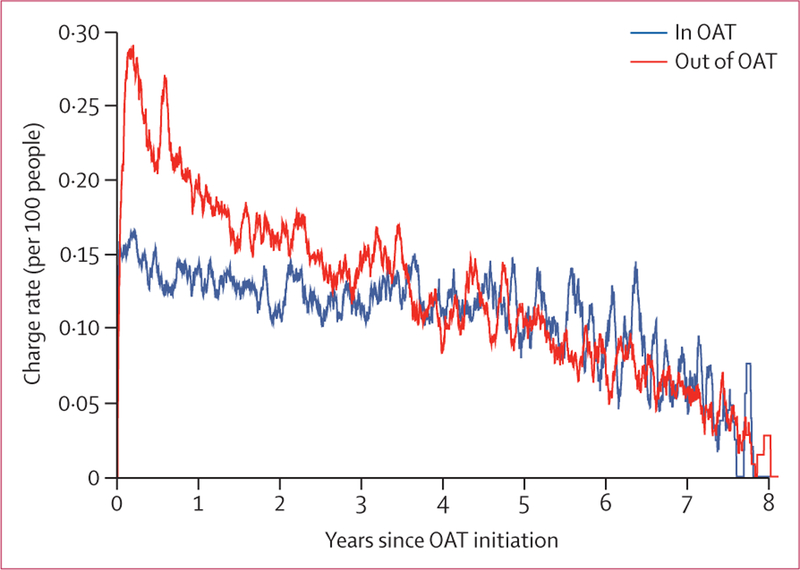
For any given day, the daily charge rate was calculated as the number of charges divided by the number of people in or out of OAT (multiplied by 100). Simple 30-day moving average on any given day refers to the arithmetic mean of charge rates from the past 30 days. OAT=opioid agonist treatment.
In the unadjusted Andersen-Gill models, being in OAT was associated with an initial benefit in reducing overall charge-days, but this effect was not consistent over time and the HR was not proportional over the entire follow-up period (table 2 [model 1]). Two approaches to overcome this non-proportionality were assessed: modelling time in OAT as half-year step-functions (table 2, models 2 and 3) and as a continuous time-dependent coefficient by including an interaction term with the natural logarithm of (time [table 2, models 4 and 5]).
Table 2:
Associations between time spent in OAT and overall charge rates
| Number of charges |
Person-years | Charges per 100 person-years (95% CI) |
6-month step-function for OAT | Continuous time-dependent coefficient for OAT |
||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||
| OAT* | ||||||||
| Not in OAT (ref) | 13 582 | 25 304.9 | 53.7 (52.8–54.6) |
1 | 1 | 1 | 1 | 1 |
| In OAT | 10 287 | 22 465.0 | 45.8 (44.9–46.7) |
0.79 (0.75–0.83) |
.. | .. | 0.28 (0.22–0.36) |
0.39 (0.30–0.52) |
| In OAT × ln(time since OAT initiation)* | .. | .. | .. | .. | NA | NA | 1.18 (1.14–1.23) |
1.12 (1.07–1.17) |
| Years since OAT initiation | ||||||||
| 0–0.5 | .. | .. | .. | .. | 0.63 (0.57–0.70) |
0.69 (0.62–0.76) |
.. | .. |
| >0.5–1.0 | .. | .. | .. | .. | 0.67 (0.60–0.73) |
0.71 (0.65–0.78) |
.. | .. |
| >1.0–15 | .. | .. | .. | .. | 0.78 (0.71–0.87) |
0.82 (0.74–0.90) |
.. | .. |
| >1.5–2.0 | .. | .. | .. | .. | 0.76 (0.68–0.86) |
0.78 (0.70–0.88) |
.. | .. |
| >2.0–2.5 | .. | .. | .. | .. | 0.82 (0.73–0.92) |
0.85 (0.75–0.95) |
.. | .. |
| >2.5–3.0 | .. | .. | .. | .. | 0.87 (0.76–1.00) |
0.85 (0.74–0.98) |
.. | .. |
| >3.0–3.5 | .. | .. | .. | .. | 0.84 (0.72–0.97) |
0.82 (0.71–0.96) |
.. | .. |
| >3.5–4.0 | .. | .. | .. | .. | 1.13 (0.97–1.31) |
1.10 (0.93–1.30) |
.. | .. |
| >4.0–4.5 | .. | .. | .. | .. | 0.99 (0.84–1.16) |
0.93 (0.78–1.10) |
.. | .. |
| >4.5–5.0 | .. | .. | .. | .. | 1.03 (0.84–1.28) |
0.90 (0.72–1.12) |
.. | .. |
| >5.0–5.5 | .. | .. | .. | .. | 1.13 (0.91–1.42) |
0.96 (0.76–1.20) |
.. | .. |
| >5.5–6.0 | .. | .. | .. | .. | 1.27 (1.01–1.59) |
1.08 (0.84–1.39) |
.. | .. |
| >6.0–6·5 | .. | .. | .. | .. | 1.18 (0.90–1.53) |
1.02 (0.77–1.36) |
.. | .. |
| >6.5–7.0 | .. | .. | .. | .. | 1.08 (0.78–1.50) |
1.07 (0.75–1.54) |
.. | .. |
| >7.0–7.5 | .. | .. | .. | .. | 1.15 (0.69–1.90) |
1.41 (0.84–2.36) |
.. | .. |
| >7.5–8.0 | .. | .. | .. | .. | 1.18 (0.34–4.07) |
1.56 (0.44–5.52) |
.. | .. |
| Sex | ||||||||
| Male | 18 337 | 33 719.9 | 54.4 (53.6–55.2) |
1.38 (1.28–1.48) |
1.42 (1.33–1.53) |
1.16 (1.09–1.23) |
1.42 (1.33–1.53) |
1.16 (1.09–1.23) |
| Female (ref) | 5532 | 14 050.0 | 39.4 (38.3–40.4) |
1 | 1 | 1 | 1 | 1 |
| Indigenous | ||||||||
| Yes | 9147 | 10 851.4 | 84.3 (82.6–86) |
2.1 (1.98–2.23) |
.. | 1.36 (1.30–1.44) |
.. | 1.37 (1.30–1.44) |
| No (ref) | 14 722 | 36 918.5 | 39.9 (39.2–40.5) |
1 | .. | 1 | .. | 1 |
| Age at OAT initiation | ||||||||
| <25 years | 10 508 | 14 638.8 | 71.8 (70.4–73.2) |
2.78 (2.54–3.02) |
2.78 (2.55–3.03) |
1.68 (1.56–1.80) |
2.78 (2.56–3.03) |
1.68 (1.56–1.80) |
| 25–29 years | 6199 | 12 143.6 | 51.0 (49.8–52.3) |
1.94 (1.76–2.12) |
1.92 (1.75–2.10) |
1.50 (1.40–1.62) |
1.92 (1.75–2.10) |
1.50 (1.40–1.62) |
| 30–34 years | 3775 | 8366.8 | 45.1 (43.7–46.6) |
1.71 (1.54–1.90) |
1.70 (1.53–1.89) |
1.39 (1.28–1.50) |
1.70 (1.53–1.89) |
1.39 (1.28–1.50) |
| ≥35 years (ref) | 3387 | 12 620.7 | 26.8 (25.9–27.7) |
1 | 1 | 1 | 1 | 1 |
| Year of OAT initiation | ||||||||
| 2004–05 (ref) | 12 028 | 23 749.2 | 50.6 (49.7–51.6) |
1 | .. | 1 | .. | 1 |
| 2006–07 | 6604 | 12 678.3 | 52.1 (50.8–53.3) |
0.88 (0.82–0.95) |
.. | 0.91 (0.87–0.96) |
.. | 0.91 (0.87–0.96) |
| 2008–09 | 4249 | 8783.9 | 48.4 (46.9–49.8) |
0.72 (0.66–0.78) |
.. | 0.79 (0.75–0.84) |
.. | 0.79 (0.75–0.84) |
| 2010–11 | 988 | 2558.5 | 38.6 (36.2–41.0) |
0.51 (0.45–0.57) |
.. | 0.58 (0.52–0.64) |
.. | 0.58 (0.52–0.64) |
| Number of charges in the 4 years before OAT initiation | ||||||||
| 0 (ref) | 3931 | 18 827.9 | 20.9 (20.2–21.5) |
1 | .. | 1 | .. | 1 |
| 1–4 | 6023 | 12 690.4 | 47.5 (46.3–48.7) |
2.27 (2.07–2.50) |
.. | 1.82 (1.67–1.98) |
.. | 1.82 (1.67–1.99) |
| 5–14 | 8808 | 11 516.0 | 76.5 (74.9–78.1) |
3.66 (3.36–3.99) |
.. | 2.33 (2.13–2.55) |
.. | 2.33 (2.13–2.55) |
| ≥15 | 5107 | 4735.7 | 107.8 (104.9–110.8) |
5.16 (4.70–5.66) |
.. | 2.57 (2.28–2.88) |
.. | 2.57 (2.28–2.89) |
| Number of charges since OAT initiation* | 23 869 | 47 770.0 | 50.0 (49.3–50.6) |
1.15 (1.14–1.17) |
.. | 1.14 (1.12–1.16) |
.. | 1.14 (1.12–1.16) |
| In prison* | ||||||||
| Yes | 2647 | 6129.6 | 43.2 (41.5–44.8) |
0.80 (0.76–0.85) |
.. | 0.32 (0.29–0.34) |
.. | 0.32 (0.30–0.34) |
| No (ref) | 21 222 | 41 640.3 | 51.0 (50.3–51.7) |
1 | .. | 1 | .. | 1 |
| Number of prison episodes in the 4 years before OAT initiation | ||||||||
| 0 (ref) | 9871 | 30 205.2 | 32.7 (32.0–33.3) |
1 | .. | 1 | .. | 1 |
| 1–5 | 3750 | 6403.8 | 58.6 (56.7–60.4) |
1.79 (1.64–1.95) |
.. | 1.12 (1.02–1.24) |
.. | 1.12 (1.02–1.24) |
| 6–10 | 5033 | 6392.8 | 78.7 (76.6–80.9) |
2.40 (2.22–2.58) |
.. | 1.36 (1.27–1.47) |
.. | 1.37 (1.27–1.47) |
| ≥11 | 5215 | 4768.1 | 109.4 (106.4–112.3) |
3.36 (3.13–3.62) |
.. | 1.60 (1.46–1.75) |
.. | 1.60 (1.46–1.75) |
| −2 log likelihood | .. | .. | .. | .. | 424 362.35 | 407 881.40 | 424 401.01 | 407 903.85 |
Data include 10 744 people and 23 869 charge-days. Results from Anderson-Gill intensity models. OAT initiation refers to first entry into OAT. OAT=opioid agonist treatment. NA=not applicable.
Time-dependent variable. Model 1 used bivariate models. Model 2 included age, sex, treatment, and a step-function for OAT. Model 3 further adjusted for all sociodemographic characteristics. Model 4 included age, sex, treatment, and a continuous time-dependent coefficient for OAT. Model 5 further adjusted for all sociodemographic characteristics.
In the unadjusted step-function model and continuous time-dependent coefficient model, OAT was associated with an initial reduction in charge-days that decreased with time since first OAT entry. Once adjusting for sociodemographic and criminographic variables, the step-function model showed that OAT was associated with an initial reduction in charge-days during the first half-year of OAT entry, with this effect gradually decreasing as time since first OAT entry increased (table 2 [model 3], appendix p 8). This effect was no longer significant approximately 3 years after OAT initiation (table 2 [model 3], appendix p 8).
Similarly, in the adjusted continuous time-dependent coefficient model, OAT was associated with fewer charge-days, although the strength of this effect decreased over time to the point of no benefit around 5·5 years following OAT initiation (table 2 [model 5], appendix p 8).
Being in prison was associated with fewer charge-days in the continuous time-dependent coefficient model (table 2 [model 5]). Conversely, being male, Indigenous, younger at first OAT entry, and an increase in the number of charges before OAT entry were all associated with an increased number of charge-days (table 2 [model 5]).
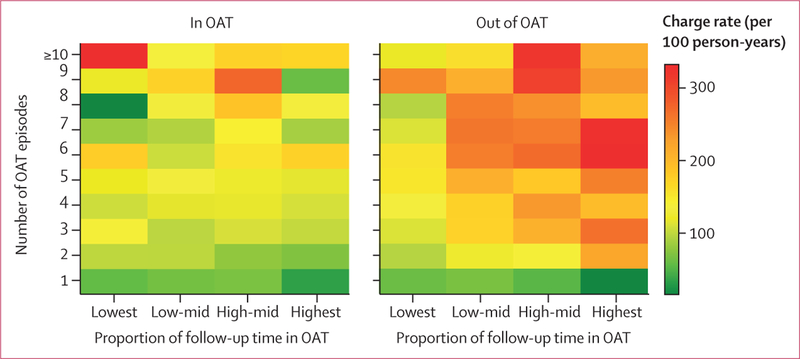
Figure 2 shows a continuous heat map comparing the unadjusted charge rates (per 100 person-years) during periods in and out of OAT, by the number of OAT episodes during follow-up and proportion of follow-up time spent in OAT. Charge rates and the quartile cutoff points used to define each of the follow-up groups are provided in the appendix (pp 9, 10). Overall, compared with charge rates out of OAT, charge rates while in OAT were generally lower among people with fewer OAT episodes and those who spent a greater proportion of follow-up time in OAT (figure 2).
Figure 2. Continuous heat map of unadjusted charge rate for individuals in and out of OAT.
The heat map summarises the relative intensity of charge rates by different profiles of OAT engagement, focusing on two features: number of OAT episodes and proportion of follow-up time in OAT. The relative intensity of the charge rates is displayed in colour scale ranging from green (lowest charge rates) to yellow, orange, and red (highest charge rates). Profiles of treatment engagement associated with lower charge rates are represented by areas with a greater intensity of green, and those associated with higher charge rates are represented by areas with a greater intensity of red. Thresholds used to define lowest, low-mid, high-mid, and highest groups are based on the quartile cutoffs for the proportion of follow-up time spent in OAT among people with the same number of treatment episodes (appendix p 10). OAT=opioid agonist treatment.
The results of the adjusted zero-inflated negative binomial model support this finding. The overall charge rate increased as the number of OAT episodes increased and when relatively lower proportions of time were spent in OAT (table 3). There were no notable differences in the effect sizes produced by any of the models in the sensitivity analyses (appendix pp 11–13).
Table 3:
Associations between number of OAT episodes and time spent in OAT and number of charges during follow-up
| No charges during follow-up (OR [95% CI]) |
Number of charges during follow-up (IRR [95% CI]) |
|
|---|---|---|
| Number of OAT episodes | 0.44* (0.38–0.50) | 1.13* (1.11–1.15) |
| Proportion of follow-up time spent in OAT | ||
| Lowest | 1.11 (0.88–1.40) | 1.11* (1.02–1.21) |
| Low-mid | 0.77* (0.60–1.00) | 1.18* (1.08–1.28) |
| High-mid | 0.78* (0.61–1.00) | 1.22* (1.12–1.33) |
| Highest (ref) | 1 | 1 |
| Percent of days in OAT spent in prison | 1.10* (1.05–1.14) | 0.98* (0.96–0.99) |
| Percent of follow-up time spent in prison | 1.02 (0.96–1.10) | 1.15* (1.13–1.18) |
| Sex | ||
| Male | 0.61* (0.51–0.70) | 0.98 (0.92–1.05) |
| Female (ref) | 1 | 1 |
| Indigenous | ||
| Yes | 0.46* (0.36–0.60) | 1.15* (1.07–1.23) |
| No (ref) | 1 | 1 |
| Age at OAT initiation | ||
| <25 years | 0.53* (0.42–0.68) | 1.36* (1.25–1.48) |
| 25–29 years | 0.72* (0.58–0.89) | 1.27* (1.16–1.39) |
| 30–34 years | 0.70* (0.54–0.89) | 1.21* (1.10–1.33) |
| ≥35 years (ref) | 1 | 1 |
| Any charge in the 4 years before OAT initiation | ||
| No | 7.92* (6.24–10.10) | NA |
| Yes (ref) | 1 | NA |
| Number of charges in the 4 years before OAT initiation | ||
| None (ref) | NA | 1 |
| 1–4 | NA | 1.18* (1.09–1.29) |
| 5–14 | NA | 1.64* (1.50–1.78) |
| ≥15 | NA | 1.92* (1.72–2.14) |
Results are from zero-inflated negative binomial model. OAT initiation refers to first entry into OAT. OR=odds ratio. IRR=incident rate ratio. OAT=opioid agonist treatment. NA=not applicable.
Significant at the 0.05 level, two-sided test.
Discussion
Reflecting the dynamic and cyclical nature of OAT in clinical practice, our study undertook a comprehensive and unique examination of the potential effect of OAT on charge rates, considering various time periods within an OAT episode and varying patterns of engagement in OAT across treatment episodes and episode lengths. In addition to reinforcing the notion that a complex relationship exists between opioid dependence, OAT, and contact with the criminal justice system, our findings also provide several novel and important insights regarding the effectiveness of OAT in reducing charge rates.
OAT was associated with an initial benefit in delaying the time to first charge and reducing the overall number of charge-days; however, this protective effect decreased over time. Although findings from randomised controlled trials have shown mixed findings with regards to the benefit of OAT on crime,14–16 most observational studies have identified that OAT, either directly or indirectly, is associated with some degree of crime reduction.17,19–21 Notwithstanding the methodological differences across observational studies, various system-level factors also play an important role in the nature and extent to which OAT reduces contact with the criminal justice system, particularly in regards to thresholds for programme entry. For example, although NSW had no specific eligibility criteria to enter the OAT programme other than opioid dependence, the timing of the reductions in crime observed in Norway can be attributed to the strict entrance requirements for the programme (eg, participants had to be aged ≥25 years, dependent on heroin for several years, and have undergone previous abstinence-oriented treatment), resulting in participants being more motivated to cease offending before commencing OAT.17
People in OAT commonly cycle in and out of treatment and our findings identified a clear relationship between the nature and extent of engagement in OAT and overall charge rates, in and out of OAT. Those who spent a greater proportion of their follow-up time in treatment, and with fewer separate episodes of treatment, had the lowest rates of charges both in and out of OAT. By contrast, during periods in OAT, charge rates were generally higher among people with more treatment episodes even if a greater amount of their follow-up time was spent in treatment. Hence, offending is not simply influenced by the total amount of time spent in OAT, but also by continuous time spent in OAT. This finding is supported by studies in the UK19 and Norway,18 whereby the greatest crime reductions were observed during periods of continuous treatment.
The characteristics and long-term goals of OAT are often debated29 and, overall, our findings provide further evidence that increased retention in OAT is associated with notably improved treatment outcomes. To date, much of the evidence supporting the need for treatment retention has focused on health outcomes (eg, mortality);2 however, our study identified that these benefits also extend to other domains—namely, contact with the criminal justice system. The provision of OAT with oral or buccal formulations of methadone and buprenorphine is the gold standard treatment approach for opioid dependence but there is ongoing interest in investigating methods and approaches to promote improved adherence and reduced cycling in and out of OAT. For example, clinical trials of long-acting buprenorphine depot formulations have shown promising results and might provide alternative treatment options to assist in improved adherence in the future.30
Importantly, almost half of the cohort had no charges during an extended period of follow-up. Offending is often not solely influenced by opioid or other drug use and evidence exists that the onset of offending often occurs before the onset of opioid use (although opioid use does appear to increase intensity of offending).6 Therefore, drug treatment and concomitant reductions in illicit opioid use might not directly affect the offending patterns of some individuals, which might in part also explain the reduction in the protective effect of OAT that was observed in our study for some of the outcome measures. The reasons motivating an individual to offend are multifactorial and although OAT provides many important health benefits for those with opioid dependence, pharmacotherapy alone is unlikely to address the broader social issues that influence offending for all individuals and many will require additional support. Hence, addressing other factors associated with offending, including poverty, social network norms, and criminogenic needs, might also be necessary to ensure stable reductions in offending.
A key strength of this study was the use of linked administrative datasets to examine the long-term effectiveness of OAT on charge rates among a population-based cohort of new OAT entrants, and for the first time, accounting for time in prison. All individuals who receive OAT in NSW must be formally registered at the time of entry into treatment and evidence exists that most individuals who develop opioid dependence engage in OAT services at some point in time. Consequently, our findings are likely to be highly representative of people who are opioid dependent in NSW. However, the findings might not be representative of individuals who receive OAT in other jurisdictions across Australia. Although the use of administrative data enabled us to assess treatment, incarceration, and charges on a day-by-day basis and control for several potential confounders, dose information was not available and individual-level factors motivating entry or influencing the extent of OAT engagement could not be accounted for and warrant further investigation. Given that not all offences are reported to police, the true rates of offending are likely to have been underestimated. It is also possible that some people were convicted of offences that they did not commit and that some offences were overturned upon successful appeal, which would not have been captured in our data. However, no evidence exists to suggest that these events are more likely to occur among opioid-dependent people in or out of OAT and are therefore not expected to affect our results.
Our findings collectively show that OAT is associated with a significant reduction in charge rates and is most protective with increased treatment engagement. Furthermore, engaging in OAT on a continuous basis appears to be most beneficial in reducing overall charge rates. An increased focus on encouraging retention in OAT is therefore necessary to maximise the long-term health and social benefits of OAT.
Supplementary Material
Research in context.
Evidence before this study
We searched PubMed from inception up to Dec 14, 2018, for studies examining the effect of opioid agonist treatment (OAT) on criminal activity among opioid-dependent people using longitudinal study designs that were able to gather information on exposure to OAT and on offending or criminal behaviour in a continuous manner across time. We used the Medical Subject Headings terms “opiate substitution treatment or OST” AND “crime OR crim*” and limited to humans. We also reviewed Cochrane reviews of OAT outcomes in randomised controlled trials (RCTs).
The three Cochrane reviews of RCTs varied in their conclusions. Those that used dichotomous measures of any offending during the trial found no significant effects, whereas the review that used a continuous measure of criminal activity found reductions during treatment.
A more precise method of assessing criminal behaviour is through daily assessment, as is the case for exposure to OAT. Police registry data afford this possibility, although such data are subject to the limitations that they only include crimes for which a person received a charge from the police (a subset of all offending behaviour). We obtained 267 results in the PubMed search, of which 16 studies were eligible for inclusion.
Several smaller linkage studies focusing on opioid-dependent people in prison suggested that being released from prison while on OAT reduces the risk of reincarceration; however, not all studies have reported this finding. Those who have been incarcerated could represent a subgroup of opioid-dependent people who have already become more heavily involved in criminal activity than have those who have not been incarcerated.
In the community-based studies of opioid-dependent people that used linked data, a range of methodological approaches were used to assess potential effects upon criminal behaviour. Most used a pre-post study design, in which offending rates before and after first entry into OAT were compared. Some studies additionally compared criminal activity after leaving OAT with that during receipt of OAT. None examined different patterns of engagement with treatment (considering length and number of episodes, indicative of extent and rapidity of cycling in and out of treatment), and none examined time to first offence after first treatment initiation and overall offending, considering a range of treatment characteristics.
Added value of this study
Our study represents the most detailed and well-powered study to date of the potential effects of OAT upon police charges during specific periods in and out of treatment for opioid dependence. Just over half of all people who entered OAT had a criminal charge at some point during follow-up. OAT had an initial beneficial effect in both delaying the time to first charge and reducing the overall number of charge-days, although this protective effect decayed over time. Being in OAT was also found to significantly reduce the total number of charges and was more protective as treatment engagement increased—ie, people whose pattern of OAT involved multiple interrupted treatment episodes and a relatively lower proportion of time spent in OAT were charged with more offences.
Implications of all the available evidence
Our findings suggest that it is not only time spent in OAT that is related to offending, but also the continuous time spent in OAT. People who cycle in and out of treatment appear to be at higher risk of offending. This finding might explain the somewhat inconsistent findings across different measures of offending and of treatment exposure that have been found in previous studies, which have not tended to measure treatment engagement in the detailed manner that was undertaken in this study. Cross-cohort analyses to corroborate our findings are warranted.
Acknowledgments
We wish to acknowledge all data custodians for providing access to the datasets used in this study: the NSW Ministry of Health (PHDAS dataset), the NSW Bureau of Crime Statistics and Research (BOCSAR; Reoffending Database), and the Australian Institute of Health and Welfare (NDI dataset). We are grateful for Judy Trevena’s work on the initial preparation of the datasets, and also to Pia Salmelainen (NSW Health) for expert advice regarding the PHDAS dataset and Jackie Fitzgerald (BOCSAR) for advice regarding the Reoffending Database. We also wish to thank Richard Mattick, Tony Butler, Lucy Burns, Amy Gibson, and Jo Kimber for their advice on the design and conduct of the original study and the members of our Indigenous Reference Group. This study received funding from the National Health and Medical Research Council (NHMRC; grant numbers 1005668 and 1081984) and the Australian Institute of Criminology (AIC) through the Criminology Research Grants Program. The views expressed are the responsibility of the author and are not necessarily those of the AIC. NG and SL are supported by UNSW Scientia Fellowships. CB is supported by National Drug and Alcohol Research Centre (NDARC) and UNSW Scientia PhD Scholarships. SL and LD are supported by NHMRC Research Fellowships (grant numbers 11409389 and 1135991) and by NIH grant NIDA R01DA1104470. The NDARC is supported by funding from the Australian Government Department of Health under the Drug and Alcohol Program.
Declaration of interests
LD has been an investigator on untied investigator-driven educational grants from Reckitt Benckiser. MF and LD have received an untied educational grant from Mundipharma for post-marketing surveillance studies of Reformulated OxyContin. MF and LD have received an untied educational grant from Seqirus for post-marketing surveillance studies of tapentadol. SL, MF, and LD have been investigators on an untied investigator-driven educational grant funded by Indivior. These untied grants are all unrelated to the current study. All other authors declare no competing interests.
Funding Australian National Health and Medical Research Council, Australian Institute of Criminology, National Institute on Drug Abuse, Australian Government Department of Health, UNSW Sydney.
Contributor Information
Natasa Gisev, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australia.
Chrianna Bharat, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australia.
Sarah Larney, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australia.
Timothy Dobbins, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australia.
Don Weatherburn, New South Wales Bureau of Crime Statistics and Research, Sydney, NSW, Australia.
Prof Matthew Hickman, Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK.
Prof Michael Farrell, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australia.
Louisa Degenhardt, National Drug and Alcohol Research Centre, UNSW Sydney, Sydney, NSW, Australi.
References
- 1.Connock M, Juarez-Garcia A, Jowett S, et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess 2007; 11: 1–171. [DOI] [PubMed] [Google Scholar]
- 2.Hser Y, Hoffman V, Grella C, Anglin M. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry 2001; 58: 503–08. [DOI] [PubMed] [Google Scholar]
- 3.Bennett T, Holloway K, Farrington D. The statistical association between drug misuse and crime: a meta-analysis. Aggress Violent Behav 2008; 13: 107–18. [Google Scholar]
- 4.Pierce M, Hayhurst K, Bird SM, et al. Quantifying crime associated with drug use among a large cohort of sanctioned offenders in England and Wales. Drug Alcohol Depend 2015; 155: 52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bukten A, Skurtveit S, Stangeland P, et al. Criminal convictions among dependent heroin users during a 3-year period prior to opioid maintenance treatment: a longitudinal national cohort study. J Subst Abuse Treat 2011; 41: 407. [DOI] [PubMed] [Google Scholar]
- 6.Hayhurst K, Pierce M, Hickman M, et al. Pathways through opiate use and offending: a systematic review. Int J Drug Policy 2017; 39: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Degenhardt L, Gisev N, Trevena J, et al. Engagement with the criminal justice system among opioid-dependent people: a retrospective cohort study. Addiction 2013; 108: 2152–65. [DOI] [PubMed] [Google Scholar]
- 8.Krebs E, Kerr T, Montaner J, Wood E, Nosyk B. Dynamics in the costs of criminality among opioid dependent individuals. Drug Alcohol Depend 2014; 144: 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godfrey C, Stewart D, Gossop M. Economic analysis of costs and consequences of the treatment of drug misuse: 2-year outcome data from the National Treatment Outcome Research Study (NTORS). Addiction 2004; 99: 697–707. [DOI] [PubMed] [Google Scholar]
- 10.Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2009; CD002209. [DOI] [PubMed]
- 11.Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R. Oral substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev 2011; CD004145. [DOI] [PubMed]
- 12.Platt L, Minozzi S, Reed J, et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev 2017; CD012021. [DOI] [PMC free article] [PubMed]
- 13.Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction 2011; 106: 32–51. [DOI] [PubMed] [Google Scholar]
- 14.Maglione MA, Raaen L, Chen C, et al. Effects of medication assisted treatment (MAT) for opioid use disorder on functional outcomes: a systematic review. J Subst Abuse Treat 2018; 89: 28–51. [DOI] [PubMed] [Google Scholar]
- 15.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014; CD002207. [DOI] [PubMed]
- 16.Perry AE, Neilson M, Martyn-St James M, et al. Pharmacological interventions for drug-using offenders. Cochrane Database Syst Rev 2015; CD010862. [DOI] [PMC free article] [PubMed]
- 17.Bukten A, Roislien J, Skurtveit S, Waal H, Gossop M, Clausen T. A day-by-day investigation of changes in criminal convictions before and after entering and leaving opioid maintenance treatment: a national cohort study. BMC Psychiatry 2013; 13: 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bukten A, Skurtveit S, Gossop M, et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study. Addiction 2012; 107: 393–99. [DOI] [PubMed] [Google Scholar]
- 19.Oliver P, Keen J, Rowse G, Ewins E, Griffiths L, Mathers N. The effect of time spent in treatment and dropout status on rates of convictions, cautions and imprisonment over 5 years in a primary care-led methadone maintenance service. Addiction 2010; 105: 732–39. [DOI] [PubMed] [Google Scholar]
- 20.Russolillo A, Moniruzzaman A, McCandless LC, Patterson M, Somers JM. Associations between methadone maintenance treatment and crime: a 17-year longitudinal cohort study of Canadian provincial offenders. Addiction 2018; 113: 656–67. [DOI] [PubMed] [Google Scholar]
- 21.Lind B, Weatherburn D, Mattick R, Chen S. The effectiveness of methadone maintenance treatment in controlling crime: an Australian aggregate-level analysis. Br J Criminol 2004; 45: 201–11. [Google Scholar]
- 22.Australian Institute of Health and Welfare. National Opioid Pharmacotherapy Statistics (NOPSAD) 2017 Canberra: Australian Institute of Health and Welfare, 2018. [Google Scholar]
- 23.Larance B, Gisev N, Cama E, et al. Predictors of transitions across stages of heroin use and dependence prior to treatment-seeking among people in treatment for opioid dependence. Drug Alcohol Depend 2018; 191: 145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calabria B, Degenhardt L, Briegleb C, et al. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict Behav 2010; 35: 741–49. [DOI] [PubMed] [Google Scholar]
- 25.Hua J, Fitzgerald J. Matching court records to measure re-offending. Crime Justice Bull 2006; 95: 1–12. [Google Scholar]
- 26.Andersen P, Gill R. Cox’s regression model for counting processes: a large sample study. Ann Stat 1982; 10: 1100–20. [Google Scholar]
- 27.Desmarais B, Harden J. Testing for zero inflation in count models: bias correction for the Vuong test. Stata J 2013; 13: 810–35. [Google Scholar]
- 28.Burns L, Gisev N, Larney S, et al. A longitudinal comparison of retention in buprenorphine and methadone treatment for opioid dependence in New South Wales, Australia. Addiction 2015; 110: 646–55. [DOI] [PubMed] [Google Scholar]
- 29.Kourounis G, Richards BDW, Kyprianou E, Symeonidou E, Malliori M-M, Samartzis L. Opioid substitution therapy: lowering the treatment thresholds. Drug Alcohol Depend 2016; 161: 1–8. [DOI] [PubMed] [Google Scholar]
- 30.Lofwall MR, Walsh SL, Nunes EV, et al. Weekly and monthly subcutaneous buprenorphine depot formulations vs daily sublingual buprenorphine with naloxone for treatment of opioid use disorder: a randomized clinical trial. JAMA Intern Med 2018; 178: 764–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.