Abstract
BACKGROUND & AIMS:
Little is known about trends in mortality among Hispanic subpopulations and etiologies of chronic liver disease (CLD). We investigated trends in mortality of CLD among the 3 largest Hispanic subgroups based on origin (Mexicans, Puerto Ricans, and Cubans) in the United States (US) from 2007 to 2016.
METHODS:
We collected data from the US Census and national mortality database, calculated age-standardized mortalities for CLD among Hispanic subgroups, and compared these with non-Hispanic whites. We determined mortality rate patterns by joinpoint analysis with estimates of annual percentage change.
RESULTS:
Hispanics were relatively younger with a lower likelihood of high school education than non-Hispanic whites at time of death. Puerto Ricans had the highest rates of age-standardized hepatitis C virus-related mortality in 2016, followed by non-Hispanic whites, Mexicans, and Cubans. Age-standardized mortality rates associated with hepatitis B virus infection decreased steadily among all subjects. Age-standardized mortality rates from alcoholic liver disease and nonalcoholic fatty liver disease among non-Hispanic whites and all Hispanics increased and accelerated. Mexicans had the highest rates of age-standardized alcoholic liver disease-related mortality, followed by non-Hispanic whites, Puerto Ricans, and Cubans. Cirrhosis- and hepatocellular carcinoma-related mortality rates increased steadily from 2007 to 2016, with the highest among Puerto Ricans and non-Hispanic whites and Mexicans, and lowest in Cubans.
CONCLUSIONS:
We found high levels of heterogeneity in CLD-related mortality patterns among the 3 largest Hispanic subgroups. Therefore, combining Hispanics as an aggregate group obscures potentially meaningful heterogeneity in etiology-specific CLD-related mortality rates among Hispanic subgroups.
Keywords: HCV, HBV, ALD, Latino, National Vital Statistic System, End-Stage Liver Disease
The Hispanic population is the fastest-growing and largest minority group in the United States. According to the U.S. Census Bureau, the Hispanic population is projected to increase from 57.5 million in 2016 to 119 million by 2060, an increase of 115%.1,2 This represents an increase from 17% of the U.S. population in 2014 to more than one-quarter of the total population (29%) in 2060.2 While Hispanics were twice as likely to live below the poverty line and 4 times as likely not to have completed high school, overall Hispanic mortality was 24% lower than for non-Hispanic whites in the United States.3 A recent meta-analysis showed that Hispanic populations had a 17.5% lower risk of mortality compared with other racial groups.4 Likewise, Hispanics experienced lower age-adjusted cardiovascular mortality rates than non-Hispanic whites.5 The lower than expected mortality despite higher propensity of metabolic risk factors as well as lower education level, economic status, and health care access has been referred to as “the Hispanic paradox.”4,6 Although Hispanics are often examined as a homogeneous population in many studies, they are a diverse group in terms of country of origin and race. According to the 2010 U.S. Census, Mexicans represent the largest proportion of the Hispanic population (63.0%), followed by the Puerto Ricans (9.2%), and then Cubans (3.5%).7 The Hispanic Community Health Study suggested that there are remarkable differences in chronic disease conditions (coronary heart disease, asthma, chronic obstructive pulmonary disease) and risk factors for cardiovascular disease (hypertension, diabetes, obesity, smoking status) among Hispanic subgroups (eg, Mexican, Puerto Ricans, Cubans).8 A recent study based on national mortality data demonstrated remarkable heterogeneity in cardiovascular disease-related mortality patterns among the 3 largest Hispanic subgroups, which suggests that combining Hispanics into a single group obscures meaningful hetero-geneity in disease risks among Hispanic subgroups.9 While Hispanics may have an overall survival advantage compared with non-Hispanic whites, they may be at increased risk for certain diseases including diabetes, hypertension, renal disease, and chronic liver disease.3 Indeed, a study based on the 2013 U.S. National Center for Health Statistics reported that chronic liver disease and cirrhosis’ is the eighth most common cause of mortality in the Hispanics, while chronic liver disease and cirrhosis is not included among the 10 most frequent causes of death in non-Hispanic whites.3 However, these estimates are based on the diagnosis named chronic liver disease and cirrhosis, which underestimates complications and mortality rates observed in patients with viral hepatitis, cirrhosis and cirrhosis-related complications including hepatocellular carcinoma (HCC).10 Thus, patterns and trends in mortality data are still lacking on etiology-specific chronic liver diseases stratified by their impact within Hispanic subgroups.
We hypothesized that significant differences in chronic liver disease-related mortality rates exist within the Hispanic subgroups, potentially unmasking heterogeneity that is not characterized by aggregating Hispanics into a single group. In this study, we used national mortality data from the U.S. National Vital Statistics System (NVSS) to estimate recent temporal trends in chronic liver disease-related mortality rates among Hispanic subgroups from 2007 to 2016. We investigated recent temporal trends in mortality rates for hepatitis C virus (HCV) infection, alcoholic liver disease (ALD), nonalcoholic fatty liver disease (NAFLD), hepatitis B virus (HBV) infection, cirrhosis, and HCC among the 3 largest Hispanic subgroups (Mexicans, Puerto Ricans, Cubans) in the United States between 2007 and 2016.
Methods
Study Data
To examine trends in chronic liver disease-related mortality rates in the U.S. adults aged ≥20 years among the 3 largest Hispanic subgroups, we analyzed de-identified mortality records from the NVSS that were based on death certificates. This database captures more than 99% of deaths in all states and the District of Columbia. More information are shown inSupplementary Methods and Materials. The underlying cause of death lists the 1 disease or condition that leads to death. The entity axis includes all causes of death listed on the death certificate. To promote specificity of the data or resolve contradictions, the record axis provides a refined version of the entity axis in which related conditions are combined for coding efficiency, overlapping conditions are eliminated, and causes violating certain logical checks are deleted.11 The cause of death is incorporated into 3 fields: underlying cause of death, entity axis, and record axis.1,11 Because the record axis provides dataset with the higher specificity, we utilized the record axis for underlying or contributing causes of death.11
Definitions of Etiologies of Chronic Liver Disease
International Classification of Diseases–Tenth Revision (ICD-10) codes were used to identify HCV, ALD, NAFLD, HBV, cirrhosis, and HCC from this database. HCV infection was identified by using the ICD-10 codes (B18.2). HBV infection was identified by using the diagnostic codes (B16, B18.0, and B18.1). Similarly, ICD-10 codes were used to identify ALD (K70.0, K70.1, K70.2, K70.3, K70.4, and K70.9) and NAFLD (K76.0 and K75.81). We categorized subjects with HCV infection and ALD as HCV infection. Similarly, subjects with HBV infection and ALD were categorized as HBV infection. Therefore, ALD was defined as subjects with ALD and without HBV and HCV infections. We classified subjects with cirrhosis complicated by portal hypertension. Eligibility criteria were based on ICD-10 codes for diagnosis of either cirrhosis (K70.3, K74.0, K74.1, K74.2, K74.3, K74.4, K74.5, and K74.6) or portal hypertension (K76.6), or 1 of the complications of cirrhosis or portal hypertension: spontaneous bacterial peritonitis (K65.2), hepatorenal syndrome (K76.7), or variceal bleeding (I85.0 and I85.1). Last, HCC was identified by utilizing ICD-10 code (C22.0). Additionally, we defined chronic liver disease, cirrhosis, and HCC using underlying cause of death. From this database, we analyzed demographic information such as age, race or ethnicity, sex, and education status. We analyzed the entire dataset excluding individuals with missing variables for race or Hispanic origin in this study. Race or ethnicity was categorized into mutually exclusive groups: non-Hispanic whites and Hispanics.12 Hispanics were categorized as 1 of the following: Mexican, Puerto Rican, Cuban, or other (Central or South American, Dominican, Other Hispanics). We analyzed the 3 largest Hispanic subgroups (Mexican, Puerto Rican, Cuban) to avoid the aggregation of various heterogeneous Hispanic subgroups in the other Hispanics category.9 Non-Hispanic whites were used as a comparison group.
Statistical Analysis
We divided the number of deaths from chronic liver disease by the total U.S. Census population among Hispanic subgroups and non-Hispanic whites for each year to calculate age-specific mortality rates. Age-specific mortality rates per 100,000 persons by age group (20–29, 30–39, 40–39, 50–59, 60–69, 70–79, and ≥80 years of age) and age-specific mortality rates by race or ethnicity were calculated. Each Hispanic subgroups’ population count data were calculated by linear interpolation for 2007–2009, U.S. Census data for 2010, and extrapolation for 2011–2016 using the full population count data by Hispanic subgroup available during the study period from the 2000 and 2010 U.S. Census reports 7 using previously described methods.9 Age-specific mortality rates were standardized to the age distribution of the 2000 U.S. standard population using the direct method. Demographic characteristics of the study population were described as frequencies with percentages. To investigate temporal changes in trends over time, we calculated the annual percentage change (APC) using the National Cancer Institute’s joinpoint regression (Join-point Trend Analysis Software version 4.5.0.1; National Cancer Institute, Bethesda, MD). More information are shown in Supplementary Methods and Materials.
Results
A total of 21,685,190 deaths among U.S. adults aged ≥20 years between 2007 and 2016 were analyzed in this study. The study population consisted of 1,540,388 deaths for all Hispanics; 862,924 for Mexicans; 198,043 for Puerto Ricans; 145,061 for Cubans; and 20,144,802 for non-Hispanic whites. Other ethnicities among the “All Hispanics category” included 32,226 deaths for Dominicans; 66,415 for Central Americans; 48,453 for South Americans; and 5462 for Latin American and other Hispanics. The demographic characteristics are presented in Table 1. With the exception of Cubans, Hispanics were more likely to be younger than non-Hispanic whites at time of death; 32.2% of Mexicans and 29.4% of Puerto Ricans were 20–59 years of age compared with just 12.1% of Cubans and 15.7% of non-Hispanic whites. When compared with non-Hispanic whites, Hispanics were more likely to have less than a high school education. Mexicans had the lowest levels of education, with 60.3% having less than a high school education, followed by Puerto Ricans, and Cubans. Hispanics (20.2%) were more likely to be never married compared with non-Hispanic whites (9.2%).
Table 1.
Characteristics of Study Populations, 2007–2016
| All Hispanics | Mexicans | Puerto Ricans | Cubans | Non-Hispanic Whites | |
|---|---|---|---|---|---|
| Total | 1,540,388 | 862,924 | 198,043 | 145,061 | 20,144,802 |
| Age at death | |||||
| 20–39 y | 139,259 (9.04) | 88,779 (10.29) | 14,800 (7.47) | 3042 (2.10) | 574,670 (2.85) |
| 40–59 y | 315,849 (20.50) | 189,415 (21.95) | 43,471 (21.95) | 14,519 (10.01) | 2,587,062 (12.84) |
| ≥60 y | 1,085,280 (70.45) | 584,730 (67.76) | 139,772 (70.58) | 127,500 (87.89) | 16,983,070 (84.30) |
| Sex | |||||
| Men | 843,201 (54.74) | 486,217 (56.35) | 107,062 (54.06) | 74,460 (51.33) | 9,978,037 (49.53) |
| Women | 697,187 (45.26) | 376,707 (43.65) | 90,981 (45.94) | 70,601 (48,67) | 10,166,765 (50.47) |
| Education | |||||
| Less than high school | 726,962 (52.31) | 479,309 (60.26) | 76,512 (44.52) | 54,037 (39.41) | 2,982,194 (19.61) |
| Completed high school | 405,311 (29.16) | 197,500 (24.83) | 65,114 (37.89) | 45,974 (33.53) | 6,821,958 (44.86) |
| Some college | 109,097 (7.85) | 62,953 (7.91) | 11,370 (6.62) | 7047 (5.14) | 1,965,458 (12.92) |
| Completed college or beyond | 148,443 (10.68) | 55,667 (7.00) | 18,856 (10.97) | 30,052 (21.92) | 3,438,285 (21.61) |
| Marital status | |||||
| Married | 603,823 (39.20) | 359,572 (41.67) | 64,813 (32.73) | 53,307 (36.75) | 7,755,277 (38.50) |
| Never married | 310,802 (20.18) | 172,158 (19.95) | 50,176 (25.34) | 16,165 (11.14) | 1,858,241 (9.22) |
| Divorced | 215,428 (13.99) | 109,957 (12.74) | 32,243 (16.28) | 23,211 (16.00) | 2,885,460 (14.32) |
| Widowed | 393,870 (25.57) | 214,270 (24.83) | 48,348 (24.41) | 50,149 (34.57) | 7,475,718 (37.11) |
| Unknown | 16,465 (1.07) | 6967 (0.81) | 2463 (1.24) | 2229 (1.54) | 170,106 (0.84) |
| Liver-related death | |||||
| Hepatitis C virus | 25,342 (1.65) | 15,371 (1.78) | 4924 (2.49) | 667 (0.46) | 111,942 (0.56) |
| Alcoholic liver disease | 30,243 (1.96) | 20,983 (2.43) | 2349 (1.19) | 566 (0.39) | 144,484 (0.72) |
| NAFLD | 3221 (0.21) | 2143 (0.25) | 273 (0.14) | 72 (0.05) | 23,984 (0.12) |
| Hepatitis B virus | 1495 (0.10) | 707 (0.08) | 330 (0.17) | 63 (0.04) | 8492 (0.04) |
| Cirrhosis | 78,127 (5.07) | 51,987 (6.02) | 9068 (4.58) | 2538 (1.75) | 383,251 (1.90) |
| Hepatocellular carcinoma | 13,441 (0.87) | 8936 (1.04) | 1987 (1.00) | 417 (0.29) | 61,828 (0.31) |
Values are n (%).
NAFLD, nonalcoholic fatty liver disease.
Trends in Age-Standardized Mortality for Viral Hepatitis Among Hispanic Subgroups
Figure 1Ademonstrates that age-standardized HCV-related mortality rates in non-Hispanic whites reached a plateau in 2013 and markedly decreased from 2014 to 2016. For all Hispanics, the age-standardized mortality rates for HCV infection steadily declined from 7.04 per 100,000 persons in 2007 to 5.05 per 100,000 persons in 2016, with an annual 3.3% decline rate (Table 2). However, a dramatic decline after the introduction of direct-acting antiviral (DAA) agents was observed at a rate of 5.7% (95% confidence interval [CI], −8.9 to −2.9 for non-Hispanic whites) and 9.7% (95% CI, −17.3 to −1.4 for all Hispanics) between 2014 and 2016. The Puerto Ricans (11.17 per 100,000 persons) had the highest rates of age-standardized HCV-related mortality in 2016, followed by non-Hispanic whites (5.92 per 100,000 persons), Mexicans (5.09 per 100,000 persons), and Cubans (4.21 per 100,000 persons). Among Mexicans, the age-standardized mortality rates for HCV infection remained stable from 2007 to 2014 and declined insignificantly from 2014 to 2016 (APC −9.5%; 95% CI, −21.5 to 4.5). Among Cubans, there was a linear decline in the age-standardized mortality rates for HCV (APC −4.6%; 95% CI, −6.4 to −2.8) over 10 years. As shown in Supplementary Table 1, age-standardized HCV-related mortality rates based on underlying cause of death reached a plateau in 2013 and demonstrated a significant decline from 2014 to 2016 compared with all-cause mortality across all Hispanics, Mexicans, and Puerto Ricans. Regarding HBV-related mortality rates (Table 2), age-standardized mortality rates steadily declined with statistical significance during the 10-year period among non-Hispanic whites, all Hispanics, Puerto Ricans, and Mexicans. Puerto Ricans had the highest rates of age-standardized HBV-related mortality, followed by non-Hispanic whites, Cubans, and Mexicans (Figure 1B).
Figure 1.
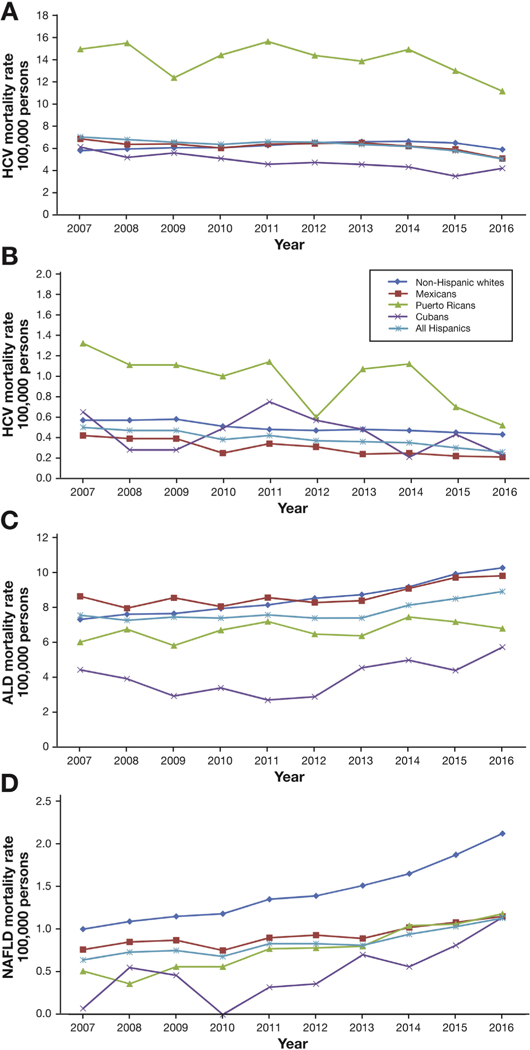
Annual age-standardized mortality rates for etiology-specific chronic liver disease in the United States stratified by Ethnicity and Hispanic Subgroups in the United States between 2007 and 2016: (A) hepatitis C virus (HCV) infection, (B) hepatitis B virus (HBV) infection, (C) alcoholic liver disease (ALD), (D) nonalcoholic fatty liver disease (NAFLD).
Table 2.
Age-Standardized Viral Hepatitis–Related Mortality Rates and APC Among Adults Aged ≥20 Years in the United States According to Ethnicity Status, 2007–2016
| Age- Standardized Rate |
Average APC (95% CI) |
Trend Segment 1 |
Trend Segment 2 |
||||
|---|---|---|---|---|---|---|---|
| 2007 | 2016 | 2007–2016 | Year | APC (95% CI) | Year | APC (95% CI) | |
| Hepatitis C virus | |||||||
| Non-Hispanic whites | 5.81 | 5.92 | 0.4 (−0.3 to 1.0) | 2007–2014 | 2.1 (1.7 to 2.6) | 2014–2016 | −5.7 (−8.9 to −2.9) |
| All Hispanics | 7.04 | 5.05 | −3.3 (−4.8 to −1.7) | 2007–2014 | −1.3 (−2.5 to −0.2) | 2014–2016 | −9.7 (−17.3 to −1.4) |
| Mexicans | 6.87 | 5.09 | −2.5 (−5.1 to 0.1) | 2007–2014 | −0.5 (−2.3 to 1.5) | 2014–2016 | −9.5 (−21.5 to 4.5) |
| Puerto Ricans | 14.97 | 11.17 | −1.9 (−4.3 to 0.6) | ||||
| Cubans | 6.14 | 4.21 | −4.6 (−6.4 to −2.8) | ||||
| Hepatitis B virus | |||||||
| Non-Hispanic whites | 0.57 | 0.43 | −3.2 (−4.2 to −2.3) | ||||
| All Hispanics | 0.50 | 0.26 | −6.3 (−7.8 to −4.8) | ||||
| Mexicans | 0.42 | 0.21 | −7.4 (−10.2 to −4.5) | ||||
| Puerto Ricans | 1.32 | 0.52 | −7.0 (−12.5 to −1.2) | ||||
| Cubans | 0.65 | 0.23 | −4.8 (−15.1 to 6.7) | ||||
NOTE. For each trend segment, the APC and the average APC were obtained to outline temporal changes accounting for transitions within each trend segment analyzed by joinpoint regression.
APC, annual percentage change; CI, confidence interval.
Trends in Age-Standardized Mortality for ALD and NAFLD Among Hispanic Subgroups
Figure 1C and D demonstrate that age-standardized mortality rates for ALD and NAFLD in non-Hispanic whites and all Hispanics increased in an accelerated fashion. During the study period, the Mexicans had the highest rates of age-standardized ALD-related mortality, followed by Puerto Ricans, and Cubans. While in 2012, the ALD-related mortality rates among non-Hispanic whites surpassed that among Mexicans. As shown in Table 3, the age-standardized ALD-related mortality rates among Cubans demonstrated an abrupt rise from 2011 to 2016 (APC 15.8%; 95% CI, 2.1%−31.4%) compared with stable mortality rates among other Hispanic groups. Additionally, there was a linear increase in the age-standardized ALD-related mortality rates based on underlying cause of death with similar trends in all-cause mortality (Supplementary Table 1). For NAFLD, the age-standardized mortality rates increased from 0.76 (for Mexicans) and 0.51 (for Puerto Ricans) per 100,000 persons in 2007 to 1.15 (for Mexicans) and 1.18 (for Puerto Ricans) per 100,000 persons in 2016. APC during the study period was dramatically higher among Puerto Ricans at 12.4% (95% CI, 8.6%−16.4%) compared with non-Hispanic whites (APC 8.6%; 95% CI, 7.2%−10.0%).
Table 3.
Age-Standardized ALD or NAFLD-Related Mortality Rates and APC Among Adults Aged ≥20 Years in the United States According to Ethnicity Status, 2007–2016
| Age- Standardized Rate |
Average APC (95% CI) |
Trend Segment 1 |
Trend Segment 2 |
||||
|---|---|---|---|---|---|---|---|
| 2007 | 2016 | 2007–2016 | Year | APC (95% CI) | Year | APC (95% CI) | |
| ALD | |||||||
| Non-Hispanic whites | 7.34 | 10.30 | 3.9 (3.2 to 4.7) | 2007–2013 | 3.0 (2.2 to 3.8) | 2013–2016 | 5.9 (3.6 to 8.3) |
| All Hispanics | 7.58 | 8.94 | 2.2 (1.3 to 3.1) | 2007–2013 | 0.1 (−0.8 to 1.1) | 2013–2016 | 6.4 (3.4 to 9.4) |
| Mexicans | 8.66 | 9.84 | 1.9 (−0.1 to 3.9) | 2007–2012 | −0.3 (−3.4 to 2.8) | 2012–2016 | 4.8 (0.3 to 9.4) |
| Puerto Ricans | 6.04 | 6.82 | 1.5 (−0.2 to 3.3) | ||||
| Cubans | 4.45 | 5.75 | 3.6 (−4.4 to 12.3) | 2007–2011 | −9.8 (−24.5 to 7.7) | 2011–2016 | 15.8 (2.1 to 31.4) |
| NAFLD | |||||||
| Non-Hispanic whites | 1 | 2.12 | 8.6 (7.2 to 10.0) | 2007–2013 | 6.8 (5.3 to 8.4) | 2013–2016 | 12.1 (7.5 to 16.9) |
| All Hispanics | 0.64 | 1.13 | 5.7 (3.9 to 7.5) | ||||
| Mexicans | 0.76 | 1.15 | 4.2 (2.4 to 6.0) | ||||
| Puerto Ricans | 0.51 | 1.18 | 12.4 (8.6 to 16.4) | ||||
| Cubans | 0.07 | 1.14 | |||||
NOTE. Joinpoint regression analysis was not performed for NAFLD-related mortality among Cubans due to missing reports on outcomes in certain years. For each trend segment, the APC and the average APC were obtained to outline temporal changes accounting for transitions within each trend segment analyzed by joinpoint regression.
ALD, alcoholic liver disease; APC, annual percentage change; CI, confidence interval; NAFLD, nonalcoholic fatty liver disease.
Trends in Age-Standardized Mortality for Cirrhosis and HCC Among Hispanic Subgroups
Figure 2A demonstrates that the mortality rates for cirrhosis steadily increased from 2007 to 2016 among non-Hispanic whites and all Hispanics. As shown in Table 4, we observed a statistically significant average APC increase of 2.8% (95% CI, 2.5%−3.2% for non-Hispanic whites) and 1.0% (95% CI, 0.5%−1.5% for all Hispanics). In terms of Hispanic subgroups, trends in cirrhosis-related mortality rates were highest among the Puerto Ricans, followed by non-Hispanic whites, Mexicans, and Cubans. Despite a relatively stable cirrhosis-related mortality in Puerto Ricans, the age-standardized mortality rate in Puerta Ricans was the highest among the study subpopulations with the exception of higher mortality among non-Hispanic whites in 2016. In Mexicans, age-standardized mortality rates increased annually with an average APC of 1.7% (95% CI, 1.0%−2.3%) during the 10-year period. Currently, the annual estimates of cirrhosis-related deaths in the NVSS13 database are based on ICD-10 codes categorizing chronic liver disease and cirrhosis diagnosis, which may underestimate overall cirrhosis-related mortality by 5% due to the exclusion of deaths associated with complications of cirrhosis or portal hypertension.10 The same patterns hold true for HCC mortality rates. HCC-related mortality was highest among Puerto Ricans and Mexicans, who were comparable to those of non-Hispanic whites (almost identical), and lowest in Cubans (Figure 2B). As shown in Table 4, joinpoint analysis showed a statistically significant average APC increase of 2.4% (95% CI, 1.9%−2.8%) without any trend segment among non-Hispanic whites, while there was a statistically insignificant average of APC increases of 1.2% (95% CI, −0.1% to 2.4%) among all Hispanics. Among Hispanics subgroups, there was a linear increase in the age-standardized HCC-related mortality rates for Mexicans (2.3%; 95% CI, 1.0%−3.6%), while Puerto Ricans and Cubans remained stable during the study period. As shown in Supplementary Table 2, age-standardized cirrhosis- and HCC-related mortality rates based on underlying cause of death was similar to those using record axis across Hispanic subgroups.
Figure 2.
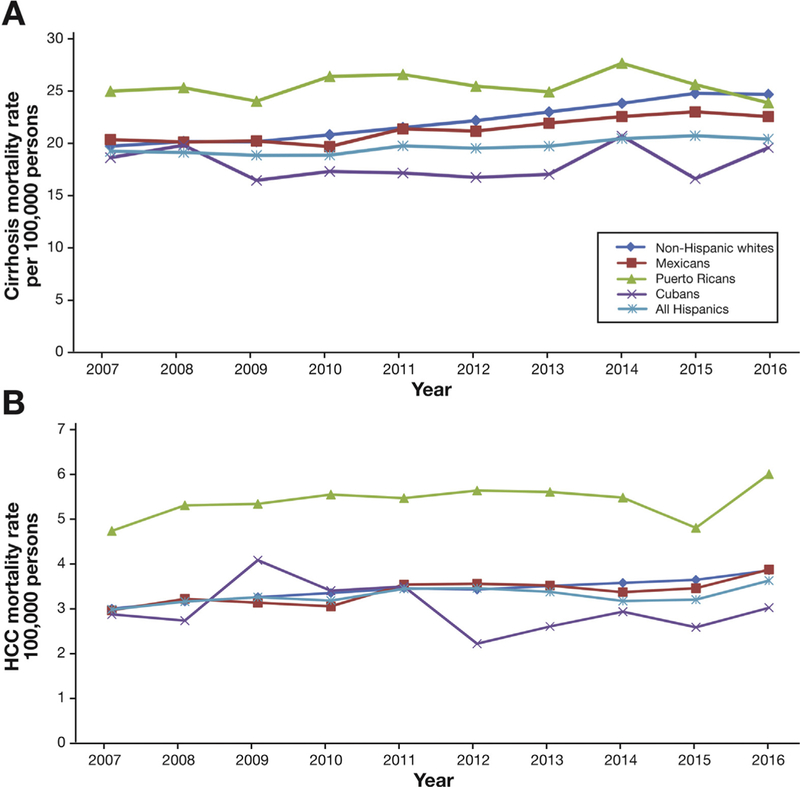
Annual age-standardized mortality rates for (A) cirrhosis and (B) hepatocellular carcinoma (HCC) according to ethnicity and Hispanic Subgroups in the United States between 2007 and 2016.
Table 4.
Age-Standardized Cirrhosis and Hepatocellular Carcinoma-Related Mortality Rates and APC Among Adults Aged ≥20 Years in the United States According to Ethnicity Status, 2007–2016
| Age- Standardized Rate |
Average APC (95% CI) |
Trend Segment 1 |
Trend Segment 2 |
||||
|---|---|---|---|---|---|---|---|
| 2007 | 2016 | 2007–2016 | Year | APC (95% CI) | Year | APC (95% CI) | |
| Cirrhosis | |||||||
| Non-Hispanic whites | 19.70 | 24.67 | 2.8 (2.5 to 3.2) | ||||
| All Hispanics | 19.19 | 20.39 | 1.0 (0.5 to 1.5) | ||||
| Mexicans | 20.34 | 22.55 | 1.7 (1.0 to 2.3) | ||||
| Puerto Ricans | 24.97 | 23.85 | 0.1 (−1.1 to 1.3) | ||||
| Cubans | 18.59 | 19.55 | 0.2 (−2.1 to 2.5) | ||||
| Hepatocellular carcinoma | |||||||
| Non-Hispanic whites | 3.01 | 3.87 | 2.4 (1.9 to 2.8) | ||||
| All Hispanics | 2.99 | 3.64 | 1.2 (−0.1 to 2.4) | ||||
| Mexicans | 2.97 | 3.89 | 2.3 (1.0 to 3.6) | ||||
| Puerto Ricans | 4.76 | 6.04 | 1.0 (−0.8 to 2.8) | ||||
| Cubans | 2.88 | 3.03 | −1.7 (−6.1 to 2.8) | ||||
NOTE. For each trend segment, the APC and the average APC were obtained to outline temporal changes accounting for transitions within each trend segment analyzed by joinpoint regression.
APC, annual percentage change; CI, confidence interval.
Discussion
In this population-based study using nationally representative mortality data in the United States, we demonstrated remarkable heterogeneity in chronic liver disease-related mortality patterns among the 3 largest Hispanic subgroups based on their origin. Puerto Ricans experienced higher HCV-, HBV-, cirrhosis-, and HCC-related mortality rates compared with non-Hispanic whites and Mexicans. Mexicans experienced HCV-, cirrhosis-, and HCC-related mortality rates comparable to non-Hispanic whites, but were observed to have the highest rates of ALD-related mortality among the Hispanic subgroups. Therefore, the amalgamation of Hispanic subgroups into 1 composite group may mask significant differences in mortality associated with the specific etiology of chronic liver disease in the Hispanic subgroups. Previous studies have shown that Hispanics have lower mortality rates than non-Hispanic whites.4,6 However, our study focusing on Hispanic subgroups demonstrated that Puerto Ricans were noted to have higher mortality rates for most chronic liver diseases compared with non-Hispanic whites and other Hispanic subgroups, and Cubans experienced lower chronic liver disease-related mortality rates compared with non-Hispanic whites. In our study, chronic liver disease-related mortality consistently varies among the 3 largest Hispanic subgroups. Our findings support the concept of heterogeneity in Hispanic subgroups reported by Rodriguez et al9 for mortality rates associated with cardiovascular disease. Therefore, studying 1 Hispanic subgroup may fail to capture the true burden of chronic liver disease among all Hispanic subgroups, and may under- or overestimate the burden of specific chronic liver disease.
Currently, the data on incidence and prevalence of chronic liver disease among Hispanic subgroups are lacking. The Hispanic Community Health Study showed that age-standardized prevalence of HCV antibody was 2.0%, which was similar in National Health and Nutrition Examination Survey 2007–2010 (1.5%).14 In this study, age-standardized prevalence of HCV differed significantly by Hispanic subgroup (11.6% in Puerto Rican, Mexican 1.9%, and Cuban 1.02%).14 Our study also showed that the Puerto Rican subgroup had the highest rates of HCV-related mortality, followed by Mexicans, and Cubans. Regarding HCC, the Puerto Rican men have the highest incidence of HCC (19.2 per 100,000), followed by Mexican men (10.8) and then Cuban men (10.1),15 which is consistent with our mortality data.
Regarding viral hepatitis and in particular HCV infection, potent and effective antiviral agents may have been responsible for the significant reduction in mortality rates associated with viral hepatitis. In our study, the reductions in HCV-related mortality risk correlate with the introduction of DAA agents across non-Hispanic whites and all Hispanics. Compared with non-Hispanic whites, Cubans and Puerto Ricans did not reach statistically significant improvements after the introduction of DAA agents. These disparities among Hispanic subgroups should be evaluated in future studies and may have resulted from differences in linkage to care, access to health care, inequalities in economic status, and cultural barriers.16 The Hispanic Community Health Study 2008–2011 reported that Cubans and Puerto Ricans had lower rates of suspected NAFLD compared with Mexicans.17 Our study showed a lower mortality rate among Puerto Ricans and Cubans compared with Mexicans between 2007 and 2011, consistent with the results of previous studies. However, NAFLD-related mortality rates among the 3 Hispanic subgroups were similar in 2016 due to a steep increase in NAFLD related mortality among Puerto Ricans and Cubans in recent years. This unexpected finding of higher NAFLD-related mortality rate among non-Hispanic whites compared with all Hispanics remains to be explained. Due to our study design, the ICD-10 code for NAFLD only captured a small subset of NAFLD, which may be subject to underestimation, especially in Hispanics who have more limited access to health care compared with non-Hispanic whites. However, such problems are mitigated when analyzing trends in which underestimation has been assumed to be relatively constant among Hispanic subgroups over the study period. Among all Hispanics, age-standardized cirrhosis and HCC-related mortality rates increased annually at a rate of 1.2%. Using the joinpoint regression analysis, it became apparent that the continuing increase in cirrhosis and HCC-related mortality rates in Hispanics were largely driven by the Mexican subgroup (APC 1.7%; 95% CI, 1.0%−2.3% for cirrhosis; APC 2.3%; 95% CI, 1.0%−3.6% for HCC-related mortality). While Puerto Ricans experienced the highest cirrhosis- and HCC-related mortality rates compared with other ethnicities, they remained stable over the study period.
The key strength of our study is the reporting of national longitudinal trends in mortality rates for etiology-specific chronic liver disease stratified by Hispanic subgroups over a 10-year period. NVSS mortality data are based on information from all resident death certificates (more than 99% of deaths) filed in the United States.13 This allowed us to compare nationwide mortality data, thus gaining unique insight into disparities among Hispanic subgroups with chronic liver disease. We defined cirrhosis as cirrhosis and portal hypertension-related complications such as spontaneous bacterial peritonitis, hepatorenal syndrome, hepatic encephalopathy, or variceal bleeding. Currently published annual mortality estimates from the NVSS13 are based on diagnosis category chronic liver disease and cirrhosis’, which may fail to capture deaths associated with complications of portal hypertension and HCC.10
Our study has several limitations. First, the cause of mortality using death certificate could be subject to underestimation and misclassification among individuals with chronic liver disease, while the reporting method has been constant during the study time, which may not explain the changes in temporal trends among Hispanic subgroups. As exemplified by the ICD-10 code for NAFLD which only captured a small proportion of individuals with NAFLD resulting in an underestimation of NAFLD-related mortality. Second, misclassification of race or ethnicity category in the national database may have under- or overestimated mortality rates among the Hispanic subgroups. However, recent studies have demonstrated that documentation of death from 1999 to 2011 among Hispanics by death certificate was reasonably accurate, with a misclassification of Hispanic origin reported only 3% higher on survey records compared with death certificates.18 Across subgroups, misclassification for the Cubans and Puerto Ricans was up to 1%, although misclassification of Mexican (6%) reported slightly higher than the other 2 subgroups.18 Therefore, mortality rates may have been slightly underestimated, and this relatively small misclassification rate varies across subgroups. Third, all Hispanics as a group includes a heterogeneous population including Central or South Americans, Dominicans, and other Hispanics, which could not be further disaggregated given small sample sizes.18 Finally, age-standardized mortality rates may not represent actual mortality rates, but these rates were appropriate for comparisons between Hispanic subgroups and non-Hispanic whites over time as population distributions change over time. Finally, we were unable to study the differences between U.S.-born Hispanics and non–U.S.-born Hispanics as data on nativity or birthplace were not available in the NVSS database, a limitation of our study. Further studies are needed to link to birth data to investigate differences between U.S.-born Hispanics and non-U.S.-born Hispanics.
In conclusion, we found remarkable heterogeneity in mortality rates of etiology-specific chronic liver disease stratified by the 3 largest Hispanic subgroups. Etiology of chronic liver disease was disproportionately associated with mortality among Hispanic subgroups in the United States. Therefore, aggregation of Hispanics as a single race or ethnicity may fail to illustrate important differences in the burden of various chronic liver diseases within the Hispanic subgroups leading to further delay in timely linkage to care and appropriate access to therapy that may result in survival benefits. Prospective future studies are needed within the Hispanic subgroups in the United States to improve knowledge gaps and our understanding of the prevalence of etiology-specific chronic liver diseases within the Hispanic subgroups.
Supplementary Material
What You Need to Know.
Background
Although Hispanics are often examined as a homogeneous population in many studies, they are a diverse group in terms of country of origin and race.
Findings
We found remarkable heterogeneity in chronic liver disease-related mortality patterns among the 3 largest Hispanic subgroups (Mexicans, Puerto Ricans, and Cubans).
Implications for patient care
Aggregating Hispanics as a single race or ethnicity may fail to illustrate important differences in the burden of chronic liver diseases within the Hispanic subgroups leading to further delay in optimal management.
Footnotes
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at
Conflicts of interest
The authors disclose no conflicts.
References
- 1.U.S. Census Bureau. The nation’s older population is still growing, Census Bureau Reports. Available at: https://www.census.gov/newsroom/press-releases/2017/cb17-100.html. Accessed January 10, 2017.
- 2.Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060: population estimates and predictions. Current population reports 2015. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed •••. [Google Scholar]
- 3.Dominguez K, Penman-Aguilar A, Chang MH, et al. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States - 2009–2013. MMWR Morb Mortal Wkly Rep 2015; 64:469–478. [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health 2013;103:e52–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Writing Group M, Mozaffarian D, Benjamin EJ, et al. Executive Summary: Heart Disease and Stroke Statistics–2016 Update: a report From the American Heart Association. Circulation 2016; 133:447–454. [DOI] [PubMed] [Google Scholar]
- 6.Sorlie PD, Backlund E, Johnson NJ, et al. Mortality by Hispanic status in the United States. JAMA 1993;270:2464–2468. [PubMed] [Google Scholar]
- 7.Ennis SR, Ríos-Vargas M, Albert NG. The Hispanic population: 2010 Census Briefs. Washington, DC: U.S. Dept of Commerce Economics and Statistics Administration, U.S. Census Bureau, 2011. [Google Scholar]
- 8.Hispanic Community Health Study/Study of Latinos Data Book: a report to the communities. NIH Publication No. 13–7951. Bethesda, MD: National Institutes of Health, 2013. [Google Scholar]
- 9.Rodriguez F, Hastings KG, Boothroyd DB, et al. Disaggregation of cause-specific cardiovascular disease mortality among Hispanic subgroups. JAMA Cardiol 2017;2:240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asrani SK, Larson JJ, Yawn B, et al. Underestimation of liver-related mortality in the United States. Gastroenterology 2013; 145:375–382, e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ly KN, Xing J, Klevens RM, et al. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med 2012;156:271–278. [DOI] [PubMed] [Google Scholar]
- 12.Yang Q, Tong X, Schieb L, et al. Vital signs: recent trends in stroke death rates - United States, 2000–2015. MMWR Morb Mortal Wkly Rep 2017;66:933–9339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heron M Deaths: leading causes for 2015. Natl Vital Stat Rep 2017;66:1–76. [PubMed] [Google Scholar]
- 14.Kuniholm MH, Jung M, Everhart JE, et al. Prevalence of hepatitis C virus infection in U.S. Hispanic/Latino adults: results from the NHANES 2007–2010 and HCHS/SOL studies. J Infect Dis 2014; 209:1585–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haile RW, John EM, Levine AJ, et al. A review of cancer in U.S. Hispanic populations. Cancer Prev Res (Phila) 2012;5:150–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flemming JA, Kim WR, Brosgart CL, et al. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology 2017;65:804–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kallwitz ER, Daviglus ML, Allison MA, et al. Prevalence of suspected nonalcoholic fatty liver disease in Hispanic/Latino individuals differs by heritage. Clin Gastroenterol Hepatol 2015; 13:569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arias E, Heron M, National Center for Health Statistics, Hakes J, U.S. Census Bureau. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat 2 2016;(172):1–21. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


