Abstract
PURPOSE
The International Union Against Cancer highlighted tumor budding as a tumor-related prognostic factor. International assessment criteria for tumor budding were recently defined by the 2016 International Tumor Budding Consensus Conference (ITBCC2016). This study aimed to clarify the prognostic and predictive values of tumor budding in a randomized controlled trial evaluating the superiority of adjuvant chemotherapy with oral tegafur-uracil over surgery alone for stage II colon cancer (SACURA trial; ClinicalTrials.gov identifier: NCT00392899).
PATIENTS AND METHODS
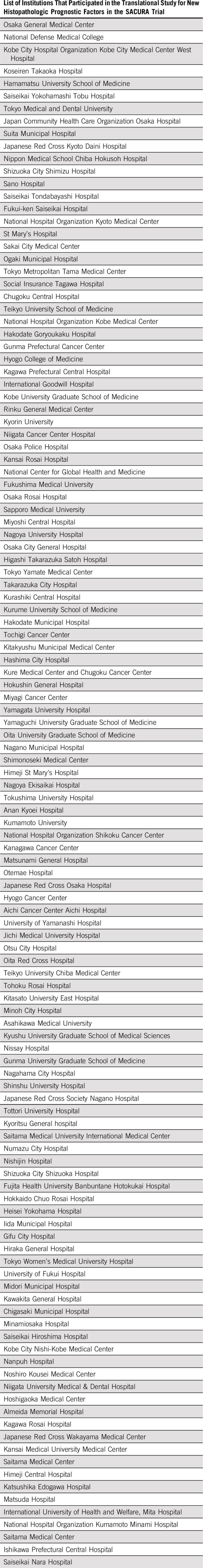
Between 2006 and 2010, we enrolled 991 patients from 123 institutions with stage II colon cancer. Tumor budding was diagnosed by central review on the basis of the criteria adopted in the ITBCC2016. We prospectively recorded all clinical and pathologic data, including the budding grade, and performed prognostic analyses after 5 years of completing the patients’ registration.
RESULTS
Of 991 tumors, 376, 331, and 284 were classified as BD1, BD2, and BD3, respectively; the 5-year relapse-free survival (RFS) rate was 90.9%, 85.1%, and 74.4%, respectively (P < .001), and ranged widely in T4 tumors (86.6% to 53.3%). The budding grade significantly correlated with recurrence in the liver, lungs, lymph nodes, and peritoneum (P < .001 to .01). Multivariable analysis revealed that budding and T stage exerted an independent impact on RFS, and on the basis of the Harrell concordance index, these two factors substantially contributed to the improvement of the Cox model for predicting RFS. Both the BD2 and BD3 groups demonstrated greater improvement in the 5-year recurrence rate in the adjuvant chemotherapy group than the surgery-alone group by approximately 5%, but the difference was statistically nonsignificant.
CONCLUSION
Tumor budding grade on the basis of the ITBCC2016 criteria should be routinely evaluated in pathologic practice and could improve the benefit of adjuvant chemotherapy for stage II colon cancer.
INTRODUCTION
Stage II colorectal cancer (CRC) accounts for one third of curatively resected patients with CRC, and robust decision-making factors are required for optimal postoperative adjuvant treatment because identifying patients who need chemotherapy at this stage remains debatable.1 In April 2016, the International Tumor Budding Consensus Conference (ITBCC; Bern, Switzerland) reached a consensus on an international, evidence-based standardized scoring system for tumor budding in CRC.2 In 2017, the Union for International Cancer Control (UICC) publication of TNM Classification of Malignant Tumors (8th edition) adopted tumor budding as a potential tumor-related prognostic factor.3 Under these circumstances, tumor budding is highly expected to be a potential prognostic factor in CRC that could identify patients with stage II disease at high risk for recurrence who need postoperative adjuvant chemotherapy.2 However, additional work is necessary to transform it from a promising to a robust decision-making factor in treatment. The prognostic impact of tumor budding has only been evaluated retrospectively, mostly in single-institution cohort studies. In addition, no study has prospectively evaluated the value of the assessment criteria for budding recommended by the ITBCC2016.
The SACURA trial is a multicenter, randomized controlled study evaluating the superiority of 1 year of adjuvant treatment with oral tegafur-uracil (UFT) compared with surgery alone for stage II colon cancer (ClinicalTrials.gov: NCT00392899). The 5-year disease-free survival (DFS) rate was 78.4% in the surgery-alone group and 80.2% in the UFT group (hazard ratio [HR], 0.91; P = .31), and the superiority of adjuvant treatment with UFT over surgery alone was not shown, although the recurrence rate was lower in the UFT group than in the surgery-alone group (10.4% v 13.4%).4 The SACURA trial projected several translational studies in which tumor budding was prospectively evaluated to determine its prognostic value in stage II colon cancer.5 The assessment criteria for tumor budding used in the SACURA trial were subsequently adopted as the international standard criteria in the ITBCC2016.
Budding is reportedly a morphologic characteristic of the epithelial-mesenchymal transition (EMT).6,7 Reports suggest that tumors undergoing EMT may resist conventional chemotherapy8,9; thus, an important clinical question to clarify would be whether high-grade budding is associated with decreased efficiency of adjuvant chemotherapy. Specifically, budding would probably not be an optimal decision-making factor if it was associated with decreased efficacy of adjuvant chemotherapy because it is not helpful for selecting patients who would benefit from postoperative adjuvant chemotherapy. Hence, this prospective clinical study attempted to validate the prognostic stratification power of tumor budding on the basis of the ITBCC criteria and clarify the predictive impact of adjuvant chemotherapy efficiency in stage II colon cancer.
PATIENTS AND METHODS
Patients
This study was conducted according to the Declaration of Helsinki and comparable Japanese ethical standards and was approved by the institutional review boards of each participating institution. Furthermore, we obtained written informed consent from all study patients.
Overall, 2,024 patients with stage II colon cancer and no preoperative treatment were enrolled in the SACURA trial between October 2006 and July 2010.5 After excluding 42 ineligible patients, 1,982 were randomly assigned to the surgery-alone group or the UFT group and compared regarding DFS (primary end point) and secondary end points, including overall survival, relapse-free survival (RFS), and incidence and severity of adverse events (Appendix Fig A1, online only). Consequently, at the primary analysis after 5 years from the last patient’s enrollment, results showed that there was no superiority in any of the end points in the UFT group.4
Of 1,982 patients, 1,003 underwent surgery at 123 separate institutions participating in the preplanned translational study for new histopathologic prognostic factors in the SACURA trial.5 After excluding 12 patients because of noncompliance with the allocated protocol treatment, we enrolled 991 patients with curatively resected stage II colon cancer at 123 institutions (surgery-alone group, 501 patients; UFT group, 490 patients). Of these, 807 patients had colon cancer and 184 had rectosigmoid cancer. Regarding the extent of lymph node dissection per the Japanese Classification of Colorectal Carcinoma (2nd English edition),10 most patients underwent D3 or D2 procedures (800 and 188 patients, respectively). Institutional pathologists diagnosed conventional factors, including venous invasion, for which positive judgment was made regardless of whether it was observed intramurally or extramurally, and elastin stains to identify vascular invasion were left to the discretion of the pathologists. The median follow-up was 69.7 months (range, 2.1 to 105.6 months), and the 5-year RFS was 84.2% in all patients, 85.3% in the UFT group, and 83.2% in the surgery-alone group (P = .3083).
Pathologic Examination for Tumor Budding
Postoperatively, among glass slides stained with hematoxylin and eosin (HE) prepared in routine pathologic practice, only slides prepared from a whole-tumor section to include the deepest part of the tumor were collected in the study office, Tokyo Medical and Dental University, and from each institution, and submitted to National Defense Medical College, the institution responsible for the central review of new histopathologic factors and blinded to patient and tumor information. All of the HE slides collected for this study were prospectively examined by one of the authors (H.U.) to evaluate the tumor budding grade according to the criteria detailed in the following paragraph.
Tumor budding was defined as an isolated cancer cell or cluster comprising less than five cells in the invasive front and graded according to its number in a microscopic field with a ×20 objective lens (0.785 mm2) in the hotspot. We classified tumors with less than five, five to nine, and 10 or more budding foci as grades BD1, BD2, and BD3, respectively. These assessment criteria were subsequently adopted in the Japanese guidelines (2009)1 and international criteria in the ITBCC2016.2 Category BD3 was subclassified as BD3a for tumors with 10 to 19 and BD3b for those with 20 or more budding foci in the hotspot (in a field of 0.785 mm2) at the invasive front. No cytokeratin stains were used to determine the hotspots or to count the number of buds.
Statistical Analyses
The end point definition in the SACURA trial was reported previously.4,5 DFS was defined as the time from randomization to recurrence, second cancers, or death, whichever occurred first. Second cancers included metachronous cancers developed in both the colorectum and other organs. The SACURA trial revealed that approximately 9% of the patients experienced second cancers, comprising 40.7% of the DFS events.4 Because we considered RFS, the time from randomization to first recurrence or death, more suitable for appraising the clinical value of the prognostic factors, we used it as a substitute end point.
The Kruskal-Wallis test was used for continuous variables and the χ2 test for categorical variables to assess differences between tumor budding in clinicopathologic characteristics and postoperative oncologic events. The RFS and recurrence rates were estimated using Kaplan-Meier analysis. We evaluated the 95% CIs at a specific time using the SE computed by the Greenwood formula and performed comparisons using the log-rank test. Univariable and multivariable analyses using the Cox proportional hazards regression model were performed to calculate HRs and 95% CIs for RFS of eight prespecified, elemental prognostic factors, including conventional factors used in the current international guidelines (number of lymph nodes examined, tumor differentiation, T stage, lymphatic and venous invasion, and microsatellite instability),11,12 treatment arm, and tumor budding. Additional multivariable analyses were also performed as sensitivity analyses in other sets of prognostic factors. Furthermore, we compared the multivariable Cox models for the prediction of RFS to assess the prognostic power of the individual prognostic factors using the Harrell concordance index (C-index).13 The 95% CI for the difference in Harrell C-index from the interest model was estimated using the bootstrap percentile method with resampling 10,000 times. We conducted an interaction analysis to compare the treatment effect of UFT between subgroups determined according to the three-tier tumor budding grade by using a Cox model with treatment, three-tier tumor budding (two terms), and their interaction (two terms) as covariables to have an interaction test with degrees of freedom of 2. We also estimated subgroup-specific treatment effects to inspect the profile of the interaction. All statistical analyses were performed using SAS, version 9.3 (SAS Institute, Cary, NC).
RESULTS
Incidence of Grades of Tumor Budding in the SACURA Trial
On the basis of the budding grade, 376, 331, and 284 tumors were classified as BD1, BD2, and BD3, respectively. The proportion of T4, positive lymphatic invasion, and preoperative serum carcinoembryonic antigen value of more than 5.0 ng/mL was higher based on the increased tumor budding grade (P < .001 to .03; Table 1). The budding grade was marginally associated with the tumor differentiation grade (P = .0598).
TABLE 1.
Tumor Budding and Clinicopathologic Characteristics

Tumor Budding and Prognostic Outcomes
On the basis of the tumor budding grade, the 5-year RFS rate was 90.9% (95% CI, 87.4% to 93.5%), 85.1% (95% CI, 80.7% to 88.6%), and 74.4% (95% CI, 68.9% to 79.1%) for BD1, BD2, and BD3, respectively (P < .001; Fig 1). Moreover, a significant difference was observed in RFS between BD3a and BD3b (P = .0465); the 5-year RFS rate was 77.5% (95% CI, 71.3% to 82.6%) for BD3a and 64.6% (95% CI, 52.0% to 74.7%) for BD3b. A positive correlation was observed between the three-tier budding grade and RFS in both T3 and T4 (P = .0100 and < .001, respectively); however, the 5-year RFS rate stratified according to the three-tier budding grade was wider in patients with T4 tumors (86.6% to 53.3%) compared with those with T3 tumors (91.4% to 82.1%).
FIG 1.
Kaplan-Meier estimates of the relapse-free survival (RFS) rate in patients with colon cancer according to grade of tumor budding.
The incidence of recurrence was 6.4%, 12.1%, and 23.6% in the BD1, BD2, and BD3 groups, respectively (P < .001; Table 2). Of first relapse organs, the three-tier budding grade was significantly associated with the incidence of liver, lung, lymph node, and peritoneal recurrence, respectively (P < .001 to .02; Table 2).
TABLE 2.
Incidence of Postoperative Oncologic Events According to the Grade of Tumor Budding
Identification of Significant Prognostic Factors for RFS
Among eight prespecified prognostic factors, T stage, microsatellite instability status, and tumor budding correlated with RFS on the basis of univariable analysis using the Cox proportional hazards regression model (Table 3). However, other factors were not significant, including tumor differentiation, lymphatic and venous invasions, and number of lymph nodes examined.
TABLE 3.
Univariable and Multivariable Analyses of Relapse-Free Survival Using Cox Proportional Hazards Regression Model
Multivariable analysis for RFS revealed budding (BD2: HR, 1.5; 95% CI, 1.0 to 2.3; P = .0692; BD3: HR, 2.6; 95% CI, 1.7 to 3.9; P < .001) along with T stage (T4: HR, 2.5; 95% CI, 1.8 to 3.6; P < .001) as independently affecting the prognostic outcome (Table 3). In sensitivity analysis with the other two sets of combined prognostic factors, we had similar results in which tumor budding was selected as an independent factor for RFS (Appendix Table A1, online only).
Value of Tumor Budding as a Prognostic Model Factor on the Basis of Harrell C-Index
Table 4 lists a comparison of multivariable Cox models for predicting RFS according to the Harrell C-index. The C-index of a prognostic model consisting of eight elemental prognostic factors was 0.6805 (full model). Among the prognostic models excluding a component factor from the full model, the reduction in C-index was the most significant in the model excluding tumor budding (0.0423), and its 95% CI did not contain zero (0.0086 to 0.0712). Similarly, T factor was associated with a substantially reduced C-index, of which 95% CI did not contain zero.
TABLE 4.
Comparison of Multivariable Cox Models for Relapse-Free Survival to Estimate the Contribution of Individual Prognostic Factors According to the Harrell C-Index
Impact of Adjuvant Chemotherapy on Recurrence Rate According to Tumor Budding Grade
On interaction analysis, the treatment effect of UFT was not significantly different between subgroups according to the grade of tumor budding (P = .5733 in the interaction test; Fig 2). Although the interaction was not significant, we observed a tendency of the beneficial effect of UFT with HRs of 0.84 (95% CI, 0.53 to 1.33) and 0.72 (95% CI, 0.41 to 1.27) in patients with BD2 tumors and those with BD3 tumors, respectively, but no such a tendency in patients with BD1 tumors with an HR of 1.14 (95% CI, 0.60 to 2.16).
FIG 2.
Comparison of time to recurrence between the surgery-alone group and the chemotherapy group in patients with (A) BD1, (B) BD2, and (C) BD3 tumors. The 5-year recurrence rates (95% CI) for the surgery-alone and tegafur-uracil (UFT) group were 6.8% (4.0% to 11.4%) and 6.5% (3.6% to 11.5%) in BD1, 10.3% (6.5% to 16.0%) and 14.8% (10.1% to 21.5%) in BD2, and 21.0% (15.0% to 29.0%) and 26.4% (20.1% to 34.4%) in BD3, respectively. Log-rank test: BD1, P = .8124; BD2, P = .1889; BD3, P = .2954.
DISCUSSION
Initially, tumor budding was loosely defined as a histologic characteristic on HE glass slides.14,15 However, from early reports on the prognostic impact of tumor budding15,16 until the latest edition of the UICC TNM staging system, which listed tumor budding as a tumor-associated prognostic factor in CRC,3 several attempts were made to define the grading system and maximize its value, accounting for various internationally proposed assessment criteria.17 First, the size of the buds needs to be characterized, because the definition of budding is not always uniform among studies (ie, not strictly defined15; less than five cells16; five or more cells18). Second, grading was determined according to either the subjective manner,15 bud intensity criteria,16,18 or percentage of the area with budding at the infiltrating margin.19
Third, even in studies using the intensity-based grading system, the most widely used system in prior studies, several inconsistencies in the detailed criteria exist, including field selection (eg, not specified15; hotspot method16,18; randomly determined20), objective lens magnification for counting buds (×2021,22; ×2516,23; ×4018,24), and number of fields assessed (one per case16; five per slide20; 10 per case25). Finally, perhaps a more important issue in the intensity-based grading system, cytokeratin staining was applied in some studies to improve the diagnostic accuracy of isolated cancer cells, and an issue was raised regarding whether either HE or cytokeratin should be used for bud scoring.23,24,26
Although these multidirectional approaches have substantially contributed to establishing the value of tumor budding, its routine implementation has been hindered by inconsistencies in the assessment criteria. In the ITBCC2016, consensus was reached in the following four assessment criteria for tumor budding2: (1) tumor budding is defined as a single tumor cell or a cell cluster comprising four or fewer tumor cells; (2) tumor budding is counted on HE; (3) tumor budding is assessed in one hotspot (in a field measuring 0.785 mm2) at the invasive front; and (4) a three-tier system should be used along with budding count to facilitate risk stratification in CRC.
In the SACURA trial (2006 to 2010), the tumor budding status of stage II colon cancer was prospectively assessed based on the criteria later adopted in the ITBCC2016. This study revealed that RFS decreased according to an increase in the three-tier grade. Also, the SACURA trial assigned subgrades to the BD3 category on the basis of the number of budding foci in a field measuring 0.785 mm2 (ie, BD3a, 10 to 19; BD3b, ≥ 20) and revealed a marked difference in RFS between BD3a and BD3b, resulting in statistically different 5-year RFS rates, with BD1, BD2, BD3a, and BD3b decreasing in this order. Zlobec et al27 argued that one of the essential properties of budding is that it is a continuous variable affecting the event of metastases, that is, the higher the number of buds, the higher the risk of lymph node and distant metastases. Although tumor budding was an intensity-dependent prognostic factor that potentially facilitated patient stratification into four groups with different survival outcomes in 638 patients with stage I to III rectal cancer at St Mark’s Hospital,16 all prior studies reporting the prognostic value of tumor budding in stage II CRC demonstrated that the entire population was successfully stratified into only two different prognosis groups.19,20,28-32 Notably, the ITBCC2016 criteria resolved the intrastage prognostic heterogeneity, enabling the stratification of patients with stage II colon cancer into four groups with wide-ranging differences in 5-year RFS rates (65% to 91%). We believe our results show that the hotspot method for tumor budding adopted in the ITBCC2016 criteria is practical and allows us to make the most of its property, although additional studies are needed to confirm the clinical benefit of the subclassification categories for BD3.
In this study, we evaluated the prognostic value of tumor budding on the basis of two statistical methods. First, we evaluated whether tumor budding was an independent prognostic factor using a Cox proportional hazard model together with other prespecified factors. Consequently, tumor budding was shown to be an independent factor, along with T stage, and the result was similar in other sensitivity analyses. Second, we compared the Harrell C-index between Cox models, in which tumor budding was shown to be essential for improving the performance of prognostic prediction, as well as T factor.
Conversely, our study shows that some of the prognostic factors in stage II CRC that have been adopted in clinical guidelines are worthy of reconsideration, for example, tumor differentiation grade is listed in the National Comprehensive Cancer Network guidelines11 and the European Society for Medical Oncology guidelines,12 but that has no impact on this study. A conclusion reached by the ITBCC2016 is that tumor budding is not the same as tumor grade,2 which is well supported in this study, presenting only marginal correlation and a different survival impact. Another factor for reevaluation is whether vascular invasion is a reliable treatment indicator for adjuvant therapy in stage II colon cancer.33
A retrospective analysis of 979 patients in the QUASAR (Quick And Simple And Reliable) trial (majority stage II) revealed a nonsignificant trend toward increased chemotherapy efficacy with increased bud counts,34 which is consistent with our study, that is, although time to recurrence was similar in BD1 tumors, adjuvant chemotherapy with UFT for 1 year seemed to be associated with an improved 5-year recurrence rate by approximately 5% in both BD2 and BD3 tumors. Although the P values were statistically insignificant, perhaps because of the small number of patients enrolled in the individual subgroups and the limited adjuvant power of UFT, the results of two discrete randomized controlled studies suggest that the proportional reduction in recurrence with chemotherapy in patients with higher bud counts might seem at least equivalent in those with low counts.
Budding is reportedly a morphologic characteristic of the EMT,6,7 and tumors undergoing EMT may resist conventional chemotherapy.8,9 However, the results of the QUASAR and SACURA trials indicate that the value of tumor budding as a decision-making factor for adjuvant chemotherapy was upheld in terms of its predictive effect in patients with stage II colon cancer, for whom none have been confirmed as predictive markers to direct use of adjuvant therapy. Because this study has limitations regarding the small sample size and single-agent UFT as an adjuvant therapy as stated previously, additional validation will be required, including perhaps a prospective randomized trial using tumor budding as a stratification factor and more effective adjuvant therapy for the high-risk groups, that is, oxaliplatin combination therapy.
In conclusion, the clinical value of the definition and grading system for tumor budding adopted in the Japanese guidelines and ITBCC2016 criteria is well validated in this multicenter prospective study for stage II colon cancer. The role of tumor budding, a tumor-related prognostic factor adopted in the UICC TNM classification, should be emphasized in the adjuvant treatment setting.
ACKNOWLEDGMENT
We are grateful to all the patients and the co-investigators for their cooperation in the SACURA trial. A list of participating institutions is given in the Appendix (online only). The authors also thank the following collaborators for their contributions to this trial: Kenichi Kono, Satoshi Nakagawa, Yasuyo Kusunoki, Fumie Kinoshita, and Naoko Kashiwagi in data management; Tasuku Inaji, Hayami Tsumura, Akinori Ogasawara, Yuri Ueda, and Syuichiro Sugimoto as the project office staff; Yoshihiro Matsubara, Satomi Sakabayashi, Yoko Nakagawa, and Tatsuo Kagimura as the statistical staff; Yoko Takagi, Aiko Saito, Sachiko Kishiro, and Yasuyo Okamoto as the translational study office staff; and Masanori Fukushima, MD, PhD, as a director of the Translational Research Center for Medical Innovation.
Appendix
FIG A1.
CONSORT diagram. Numbers in brackets indicate the number of patients in the translational study for new histopathologic factors. UFT, tegafur-uracil.
TABLE A1.
Multivariable Analyses for Relapse-Free Survival as Sensitivity Analysis
Footnotes
Presented in part at the ASCO 2017 Annual Meeting, Chicago, IL, June 2 to 6, 2017.
Supported by the Foundation for Biomedical Research and Innovation at Translational Research Center for Medical Innovation at Kobe under the funding contract with Taiho Pharmaceutical, Tokyo, Japan. The funding sources had no role in the design of the study; collection, analysis, or interpretation of the data; writing of the report; or in the decision to submit for publication. The corresponding author had full access to all of the study data and final responsibility for the decision to submit the report for publication.
AUTHOR CONTRIBUTIONS
Conception and design: Hideki Ueno, Megumi Ishiguro, Eiji Nakatani, Hiroyuki Uetake, Naohiro Tomita, Kenichi Sugihara
Administrative support: Kenichi Sugihara
Provision of study materials or patients: Hideki Ueno, Megumi Ishiguro, Toshiaki Ishikawa, Hiroyuki Uetake, Masanori Kotake, Kiyotaka Kurachi, Kohei Murata, Osamu Ikawa, Naohiro Tomita, Kenichi Sugihara
Collection and assembly of data: Hideki Ueno, Megumi Ishiguro, Toshiaki Ishikawa, Hiroyuki Uetake, Chu Matsuda, Yoshihiko Nakamoto, Masanori Kotake, Kiyotaka Kurachi, Tomohisa Egawa, Keigo Yasumasa, Kohei Murata, Osamu Ikawa, Seiichi Shinji, Naohiro Tomita, Kenichi Sugihara
Data analysis and interpretation: Hideki Ueno, Megumi Ishiguro, Eiji Nakatani, Kenta Murotani, Shigeyuki Matsui, Satoshi Teramukai, Kenichi Sugihara
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Prospective Multicenter Study on the Prognostic and Predictive Impact of Tumor Budding in Stage II Colon Cancer: Results From the SACURA Trial
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Megumi Ishiguro
Honoraria: Taiho Pharmaceutical, Yakult Honsha, Merck Serono
Consulting or Advisory Role: Taiho Pharmaceutical
Research Funding: Taiho Pharmaceutical (Inst), Yakult Honsha (Inst), Sysmex (Inst)
Toshiaki Ishikawa
Honoraria: Chugai Pharma, Sanofi, Taiho Pharmaceutical, Takeda, Daiichi Sankyo
Consulting or Advisory Role: Takeda
Satoshi Teramukai
Honoraria: Daiichi Sankyo, Takeda, Sanofi, Solasia Pharma, Sysmex, Gunze
Research Funding: Nippon Boehringer Ingelheim (Inst)
Naohiro Tomita
Research Funding: Taiho Pharmaceutical (Inst), Chugai Pharma
No other potential conflicts of interest were reported.
REFERENCES
- 1.Watanabe T, Muro K, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018;23:1–34. doi: 10.1007/s10147-017-1101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lugli A, Kirsch R, Ajioka Y, et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod Pathol. 2017;30:1299–1311. doi: 10.1038/modpathol.2017.46. [DOI] [PubMed] [Google Scholar]
- 3.Union for International Cancer Control . : TNM Classification of Malignant Tumours (ed 8). West Sussex, United Kingdom, John Wiley & Sons, 2017. [Google Scholar]
- 4.Matsuda C, Ishiguro M, Teramukai S, et al. A randomised-controlled trial of 1-year adjuvant chemotherapy with oral tegafur-uracil versus surgery alone in stage II colon cancer: SACURA trial. Eur J Cancer. 2018;96:54–63. doi: 10.1016/j.ejca.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Ishiguro M, Mochizuki H, Tomita N, et al. Study protocol of the SACURA trial: A randomized phase III trial of efficacy and safety of UFT as adjuvant chemotherapy for stage II colon cancer. BMC Cancer. 2012;12:281. doi: 10.1186/1471-2407-12-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Smedt L, Palmans S, Andel D, et al. Expression profiling of budding cells in colorectal cancer reveals an EMT-like phenotype and molecular subtype switching. Br J Cancer. 2017;116:58–65. doi: 10.1038/bjc.2016.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zlobec I, Lugli A. Tumour budding in colorectal cancer: Molecular rationale for clinical translation. Nat Rev Cancer. 2018;18:203–204. doi: 10.1038/nrc.2018.1. [DOI] [PubMed] [Google Scholar]
- 8.Yang AD, Fan F, Camp ER, et al. Chronic oxaliplatin resistance induces epithelial-to-mesenchymal transition in colorectal cancer cell lines. Clin Cancer Res. 2006;12:4147–4153. doi: 10.1158/1078-0432.CCR-06-0038. [DOI] [PubMed] [Google Scholar]
- 9.Thiery JP, Acloque H, Huang RY, et al. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 10. Japanese Society for Cancer of the Colon and Rectum: Japanese Classification of Colorectal Carcinoma (ed 2). Tokyo, Japan, Kanehara & Co, 2009. [Google Scholar]
- 11. National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology, colon cancer version 3. 2018. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf. [DOI] [PubMed]
- 12.Labianca R, Nordlinger B, Beretta GD, et al. Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(suppl 6):vi64–vi72. doi: 10.1093/annonc/mdt354. [DOI] [PubMed] [Google Scholar]
- 13.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 14.Morodomi T, Isomoto H, Shirouzu K, et al. An index for estimating the probability of lymph node metastasis in rectal cancers. Lymph node metastasis and the histopathology of actively invasive regions of cancer. Cancer. 1989;63:539–543. doi: 10.1002/1097-0142(19890201)63:3<539::aid-cncr2820630323>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 15.Hase K, Shatney C, Johnson D, et al. Prognostic value of tumor “budding” in patients with colorectal cancer. Dis Colon Rectum. 1993;36:627–635. doi: 10.1007/BF02238588. [DOI] [PubMed] [Google Scholar]
- 16.Ueno H, Murphy J, Jass JR, et al. Tumour ‘budding’ as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002;40:127–132. doi: 10.1046/j.1365-2559.2002.01324.x. [DOI] [PubMed] [Google Scholar]
- 17.Mitrovic B, Schaeffer DF, Riddell RH, et al. Tumor budding in colorectal carcinoma: Time to take notice. Mod Pathol. 2012;25:1315–1325. doi: 10.1038/modpathol.2012.94. [DOI] [PubMed] [Google Scholar]
- 18.Jass JR, Barker M, Fraser L, et al. APC mutation and tumour budding in colorectal cancer. J Clin Pathol. 2003;56:69–73. doi: 10.1136/jcp.56.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakamura T, Mitomi H, Kanazawa H, et al. Tumor budding as an index to identify high-risk patients with stage II colon cancer. Dis Colon Rectum. 2008;51:568–572. doi: 10.1007/s10350-008-9192-9. [DOI] [PubMed] [Google Scholar]
- 20.Wang LM, Kevans D, Mulcahy H, et al. Tumor budding is a strong and reproducible prognostic marker in T3N0 colorectal cancer. Am J Surg Pathol. 2009;33:134–141. doi: 10.1097/PAS.0b013e318184cd55. [DOI] [PubMed] [Google Scholar]
- 21.Ueno H, Mochizuki H, Hashiguchi Y, et al. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology. 2004;127:385–394. doi: 10.1053/j.gastro.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 22.Shinto E, Mochizuki H, Ueno H, et al. A novel classification of tumour budding in colorectal cancer based on the presence of cytoplasmic pseudo-fragments around budding foci. Histopathology. 2005;47:25–31. doi: 10.1111/j.1365-2559.2005.02162.x. [DOI] [PubMed] [Google Scholar]
- 23.Prall F, Nizze H, Barten M. Tumour budding as prognostic factor in stage I/II colorectal carcinoma. Histopathology. 2005;47:17–24. doi: 10.1111/j.1365-2559.2005.02161.x. [DOI] [PubMed] [Google Scholar]
- 24.Lugli A, Karamitopoulou E, Panayiotides I, et al. CD8+ lymphocytes/ tumour-budding index: An independent prognostic factor representing a ‘pro-/anti-tumour’ approach to tumour host interaction in colorectal cancer. Br J Cancer. 2009;101:1382–1392. doi: 10.1038/sj.bjc.6605318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karamitopoulou E, Zlobec I, Kölzer V, et al. Proposal for a 10-high-power-fields scoring method for the assessment of tumor budding in colorectal cancer. Mod Pathol. 2013;26:295–301. doi: 10.1038/modpathol.2012.155. [DOI] [PubMed] [Google Scholar]
- 26.Puppa G, Senore C, Sheahan K, et al. Diagnostic reproducibility of tumour budding in colorectal cancer: A multicentre, multinational study using virtual microscopy. Histopathology. 2012;61:562–575. doi: 10.1111/j.1365-2559.2012.04270.x. [DOI] [PubMed] [Google Scholar]
- 27.Zlobec I, Hädrich M, Dawson H, et al. Intratumoural budding (ITB) in preoperative biopsies predicts the presence of lymph node and distant metastases in colon and rectal cancer patients. Br J Cancer. 2014;110:1008–1013. doi: 10.1038/bjc.2013.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka M, Hashiguchi Y, Ueno H, et al. Tumor budding at the invasive margin can predict patients at high risk of recurrence after curative surgery for stage II, T3 colon cancer. Dis Colon Rectum. 2003;46:1054–1059. doi: 10.1007/s10350-004-7280-z. [DOI] [PubMed] [Google Scholar]
- 29.Okuyama T, Nakamura T, Yamaguchi M. Budding is useful to select high-risk patients in stage II well-differentiated or moderately differentiated colon adenocarcinoma. Dis Colon Rectum. 2003;46:1400–1406. doi: 10.1007/s10350-004-6757-0. [DOI] [PubMed] [Google Scholar]
- 30.Betge J, Kornprat P, Pollheimer MJ, et al. Tumor budding is an independent predictor of outcome in AJCC/UICC stage II colorectal cancer. Ann Surg Oncol. 2012;19:3706–3712. doi: 10.1245/s10434-012-2426-z. [DOI] [PubMed] [Google Scholar]
- 31.Lai Y-H, Wu L-C, Li P-S, et al. Tumour budding is a reproducible index for risk stratification of patients with stage II colon cancer. Colorectal Dis. 2014;16:259–264. doi: 10.1111/codi.12454. [DOI] [PubMed] [Google Scholar]
- 32.Horcic M, Koelzer VH, Karamitopoulou E, et al. Tumor budding score based on 10 high-power fields is a promising basis for a standardized prognostic scoring system in stage II colorectal cancer. Hum Pathol. 2013;44:697–705. doi: 10.1016/j.humpath.2012.07.026. [DOI] [PubMed] [Google Scholar]
- 33.Venook AP, Niedzwiecki D, Lopatin M, et al. Biologic determinants of tumor recurrence in stage II colon cancer: Validation study of the 12-gene recurrence score in cancer and leukemia group B (CALGB) 9581. J Clin Oncol. 2013;31:1775–1781. doi: 10.1200/JCO.2012.45.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mitrovic B, Handley K, Assarzadegan N, et al. Prognostic and predictive value of tumour budding in stage II colorectal carcinoma. J Clin Oncol. 2015;33(suppl; abstr 3605)) [Google Scholar]









