Abstract
Background
Population-based studies of ultrasound measures of carotid atherosclerosis are informative about future risks of cardiovascular disease.
Objectives
To conduct carotid ultrasound screening in a random sample of 24,822 Chinese adults from 10 diverse regions in the China Kadoorie Biobank study (CKB) in 2013-2014.
Methods
Mean intima-media thickness (cIMT) of the common carotid arteries, number of plaques and maximum plaque thickness were examined in various population subgroups in CKB. The cIMT findings in Chinese (mean age 59 years) were compared with those from 2579 Europeans (mean age 63 years) from the UK Biobank.
Results
Overall, the mean cIMT in Chinese was 0.70 mm (SD 0.16) and increased with age by 0.08 mm (SE 0.008) per 10-years older age. About 31% of the Chinese had carotid plaques and the prevalence varied 10-fold with age (6% at 40-49 to 58% at 70-89 years) and 5-fold by region of China (range, 11%-50%). Plaque burden and cIMT were only moderately correlated with each other (r=0.40). After adjustment for age, sex and region, plaque prevalence was 50% higher in smokers than in non-smokers (34% vs 23%) and over 2-fold higher in individuals with SBP≥160 mmHg than those with SBP<120 mmHg (39% vs 19%) in CKB. The overall mean (SE) cIMT values were higher in Chinese than in Europeans (0.70 [0.001] vs 0.66 [0.003] mm, p<0.001).
Conclusions
About one-third of Chinese adults had carotid plaques and the overall burden of carotid atherosclerosis was comparable with Europeans, but was even more extreme in some regions of China.
Keywords: Atherosclerosis, plaques, carotid intima-media thickness
Introduction
The health status of the Chinese population, which accounts for one fifth of the global population, has improved substantially over the last half century, with a 50% increase in life expectancy from 49 years in 1949 to 75 years in 2012 (1). In contrast with Western populations where cardiovascular disease (CVD) mortality rates have declined over recent decades, CVD mortality rates have increased exponentially in China over this period (1). Stroke and ischaemic heart disease (IHD) are now the leading causes of premature death in both Chinese and Western populations (2). Since atherosclerosis develops silently over several decades before presentation as a clinical CVD event, population-based studies using carotid artery ultrasound examinations should be informative about future risks of CVD (3–5). Carotid intima-media thickness (cIMT: reflecting hypertrophy of both the intima and media layers of the arterial wall) provides the first morphological evidence of atherosclerosis (5,6), but carotid plaques (focal thickening >1.5 mm of the intima layer of the carotid arteries) are stronger predictors of CVD than cIMT (6,7). Both cIMT and carotid plaques have been widely used in population-based surveys in Western populations for prediction of risk of CVD (8–14). Previous studies of carotid atherosclerosis in Chinese adults have also reported associations of cIMT and plaque with CVD risk factors (15–18), but few population-based studies in China included a sufficient number of participants to reliably assess the age-specific burden of atherosclerosis.
Technological advances in edge detection software in carotid artery ultrasound imaging platforms allow semi-automated methods to measure cIMT and plaques that have facilitated their use in large-scale observational studies and clinical trials (5–7). Automated methods typically locate the carotid bifurcation and measure the thickness of the far wall of the artery at a fixed point proximal to the bifurcation of the common carotid artery to record cIMT. However, detection of carotid plaques is not fully automated and requires a sonographer to acquire ultrasound images bilaterally to include four main segments of the carotid arteries (distal common carotid artery [CCA], carotid artery bifurcation [carotid bulb], proximal internal carotid artery [ICA] and proximal external carotid artery [ECA]) to record the location and number of plaques and measure their maximum thickness.
We conducted B-mode ultrasound imaging of both extra-cranial carotid arteries using such semi-automated methods to measure cIMT, and recorded the presence and number of any of carotid plaques in a random sample of 24,822 participants in the China Kadoorie Biobank (CKB) study. We compared the cIMT findings in Chinese with 2579 age-matched Europeans from the UK Biobank (UKB) study. The aims of the present report were: (i) to estimate the prevalence of various measures of carotid atherosclerosis in population sub-groups defined by age, region and CVD risk factors; and (ii) and to compare mean cIMT values in the Chinese (CKB) with a European population (UKB) recorded using identical methods and (iii) to review the implications for future risk of CVD in China.
Methods
CKB study population
The CKB study is a prospective study of 0.5 million adults, aged 30-79 years, who were recruited from 10 geographical regions in China that were chosen to include a wide range of behavioural, lifestyle and environmental risk factors (19,20). In each region, temporary assessment clinics were set up in residential centres. A representative 5-6% sample of survivors (i.e. about 33,000) were invited for the 2nd resurvey in 2013-2014 (~8 years after baseline), and 24,822 attended (76% response rate). All participants attending the re-survey underwent a repeat interview and had physical measurements recorded and provided biological samples. Ethics approval was obtained from the appropriate UK authorities (University of Oxford Tropical Research Ethics Committee) and Chinese authorities (Chinese Academy of Medical Sciences). All participants provided written informed consent.
Carotid intima-media thickness (cIMT)
A Panasonic CardioHealth Station was used to acquire and record ultrasound images for four segments of the carotid arteries each involving about 1 cm distance (distal CCA, carotid bifurcation, proximal ICA, and proximal ECA) on both left and right sides. The cIMT measures were recorded only in the distal 1 cm of the CCA, but all 4 segments were screened for the presence or absence of plaques (Supplementary Material: Supplementary methods).
Carotid plaques
Longitudinal scanning of the entire length of the carotid arteries (from the base of the neck to the angle of the jaw) was conducted bilaterally to screen for plaques and pre-plaques in each of the 4 segments of the carotid arteries. Consistent with the Mannheim consensus, a plaque was defined as any focal thickening or protrusion from the wall into the lumen with cIMT >1.5 mm thickness and a pre-plaque was defined as any focal thickening of cIMT >1.0≤1.5 mm (6). The number and location (i.e. segment) of plaques or pre-plaques were also recorded. Horizontal scanning of the carotid arteries was used to record the thickness of the largest plaque or pre-plaque.
Carotid imaging quality control
The average time for completion of carotid artery image acquisition, including both cIMT and plaque assessments, was 10 minutes per participant. Random samples (~3%) of carotid ultrasound examinations were checked for quality assessment by one of three radiologists who confirmed that measurements of cIMT, presence and number of plaques and the thickness of the maximum plaque were correctly recorded (Supplementary Material: Supplementary methods). The radiologists provided a quality score for cIMT and plaque thickness measurements recorded by the sonographers in each of the 10 geographic regions in China.
UKB study population
The UK Biobank (UKB) study is a prospective study of 500,000 UK individuals, aged between 40-69 years, who were recruited during 2006-10 (21). The data from the UK-Biobank resource are publically accessible for scientific research (21). The UKB study conducted ultrasound imaging of the carotid arteries in a subset of participants in 2014-2015, using a Panasonic CardioHealth Station, which involved identical ultrasound devices and procedures to those used in CKB. Data available for the UKB study participants were restricted to results for cIMT on 2579 participants from the pilot phase of the imaging programme (22) (and no data for carotid plaques are currently available).
Statistical methods
Mean values of cIMT, carotid plaque thickness and plaque number were compared between the left and right sides, and the agreement between these measurements was assessed using Pearson correlation coefficients. Linear and logistic regressions were used to assess levels of cIMT and presence of plaque, respectively, by 10-year age groups and standard systolic blood pressure (SBP) groups (<120, 120-139, 140-159, ≥160 mmHg) after appropriate adjustments (specified for particular results). F-statistics, which indicate the extent to which a risk factor accounts for variance in the outcome of a regression model, were used to compare the strength of associations of carotid measures with the different risk factors. Carotid plaque burden was derived by first standardising the plaque number and maximum width (i.e. dividing each by its standard deviation [SD]) and estimating the average, then multiplying the average value by the SD of the maximum plaque thickness to provide a plaque burden recorded in millimetres units (i.e. interpretable as an enhanced estimate of the maximum plaque thickness). All analyses used SAS 9.3 (SAS Institute, Cary, NC, USA).
Results
Population characteristics
Among the 24,822 CKB participants with carotid ultrasound measures, the mean (SD) age at measurement was 59 (10) years, 38% were men and the mean SBP was 136 (21) mmHg. Overall, 7% had diabetes, 47% of men and 1% of women were current cigarette smokers, and 16% had a prior history of stroke or IHD at the time of the examination.
Quality assurance of carotid measures
Among the 24,822 participants, 694 (3%) had quality assessments of the carotid ultrasound measurements recorded (eTable 1). The overall quality score, reflecting the extent to which the radiologist confirmed that the sonographer had correctly recorded cIMT and plaques, was 85% (range, 75% to 93%) for the 10 centres (eTable 1). The cIMT was correctly measured in 99% (range: 96% to 100%). Plaques were satisfactorily located in 96% (range: 89-100%) and counted accurately in 96% (range 87% to 100%: eTable 1).
Left versus right side measurements
There were no significant differences in the mean values of cIMT, proportions with plaque, number of plaques or maximum plaque thickness between the left and right sides (eTable 2). Likewise, the correlation coefficients between right and left sides were 0.60 for cIMT, 0.50 for presence of plaque, 0.62 for plaque number and 0.58 for maximum plaque thickness, respectively.
Associations with age and region
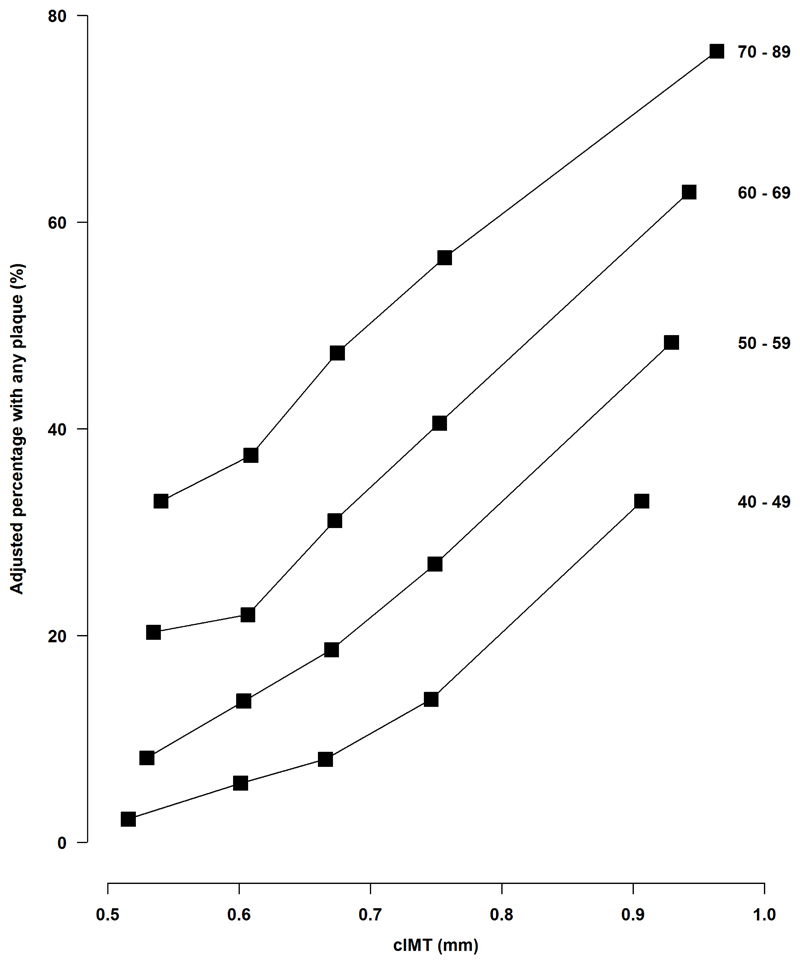
Mean cIMT was 0.70 (SD 0.16) mm overall and it increased with age by about 0.08 mm (SE 0.008) per 10-year older age (Table 1). Overall, 31% had a carotid plaque, 9% had a pre-plaque and 60% had neither detected. The prevalence of plaques also increased with age, from 6%, 20%, 38% to 58% in the 10-year groups from 40 to 69 and 70-89 (Table 1). The prevalence of plaques also increased with increasing cIMT (Figure 1). Among the 4 carotid artery segments examined, plaques were most frequently located in the carotid bulb (61%) and CCA (35%), and were rarely present in the ICA (3%) or in the ECA (1%).
Table 1.
Distribution of mean (SD) values of cIMT and percentage with plaque, by age, sex, hypertension, cigarette smoking and geographic region, after adjustment for age, sex and region as appropriate. Values for plaque in the final column are additionally adjusted for all other group variables. Values for systolic blood pressure (SBP) and current cigarette smoking are the average of those at baseline and at resurvey
| N | cIMT, mm Mean (SD) |
Any plaque, % Mean (SD) |
Any plaque, % Adjusted mean (SD) |
||
|---|---|---|---|---|---|
| Age (years) | 40 - 49 | 5469 | 0.59 (0.10) | 6% (5%) | 6% (6%) |
| 50 - 59 | 7680 | 0.67 (0.13) | 20% (13%) | 20% (14%) | |
| 60 - 69 | 7388 | 0.74 (0.16) | 39% (16%) | 38% (18%) | |
| 70 - 89 | 4285 | 0.82 (0.18) | 62% (16%) | 58% (17%) | |
| Sex | Men | 9496 | 0.73 (0.18) | 33% (24%) | 28% (24%) |
| Women | 15326 | 0.68 (0.15) | 21% (20%) | 23% (21%) | |
| SBP (mmHg) | < 120 | 5442 | 0.67 (0.13) | 19% (15%) | 19% (15%) |
| 120-139 | 9461 | 0.69 (0.15) | 25% (20%) | 24% (20%) | |
| 140-159 | 6594 | 0.72 (0.16) | 31% (23%) | 31% (23%) | |
| 160+ | 3325 | 0.74 (0.19) | 39% (24%) | 39% (24%) | |
| Ever regular smoker | No | 15696 | 0.69 (0.15) | 23% (21%) | 23% (22%) |
| Yes | 9126 | 0.71 (0.18) | 35% (24%) | 34% (24%) | |
| Residence | Rural | 14154 | 0.69 (0.15) | 21% (17%) | 21% (18%) |
| Urban | 10668 | 0.72 (0.17) | 36% (21%) | 35% (21%) | |
| Geographic region | Hunan | 2880 | 0.70 (0.17) | 12% (15%) | 11% (15%) |
| Zhejian | 2922 | 0.68 (0.15) | 17% (17%) | 16% (17%) | |
| Sichuan | 2775 | 0.64 (0.13) | 17% (16%) | 16% (18%) | |
| Suzhou | 2804 | 0.68 (0.15) | 19% (17%) | 18% (18%) | |
| Qingdao | 1592 | 0.72 (0.16) | 23% (19%) | 23% (20%) | |
| Gansu | 2481 | 0.71 (0.14) | 24% (19%) | 25% (20%) | |
| Henan | 3096 | 0.70 (0.16) | 38% (21%) | 38% (22%) | |
| Liuzhou | 2746 | 0.71 (0.16) | 42% (22%) | 41% (23%) | |
| Haikou | 1377 | 0.73 (0.19) | 46% (24%) | 47% (26%) | |
| Harbin | 2149 | 0.76 (0.19) | 53% (23%) | 50% (24%) | |
| All | 24822 | 0.70 (0.16) | 31% (46%) | 31% (46%) | |
Figure 1. Age-specific percentage with any carotid plaques, by quintiles of cIMT.
Values are adjusted for sex and geographic region.
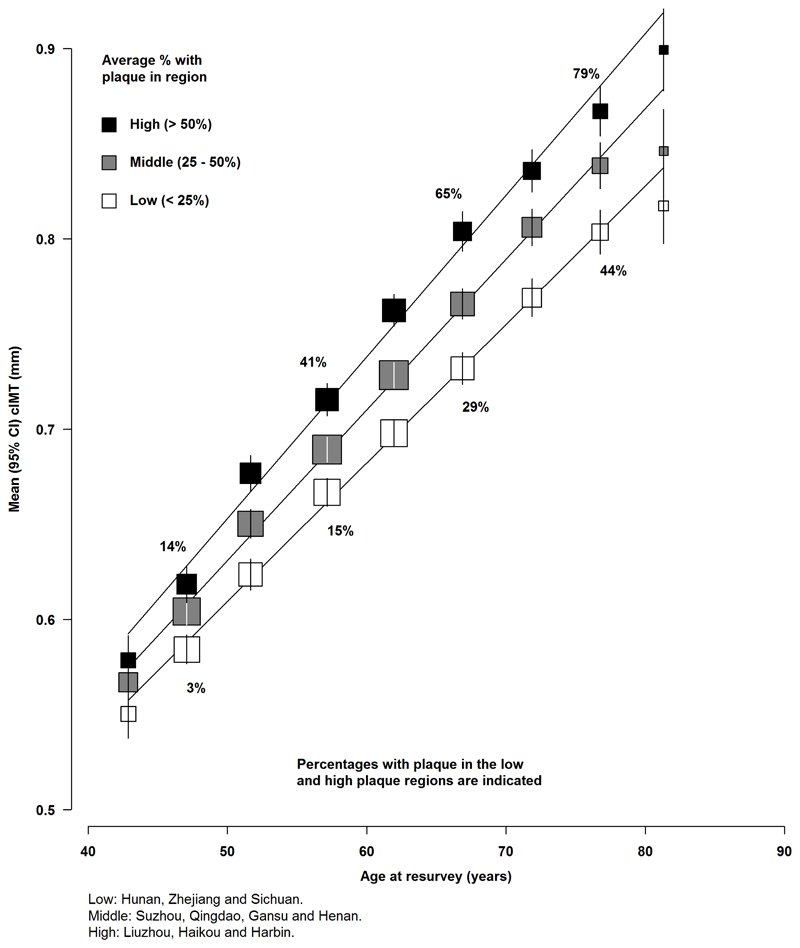
Both the number of plaques and the maximum plaque thickness also increased linearly with increasing age (Data not shown). In addition to the variation by age, the mean cIMT and percentage with plaque also varied substantially by geographic region (Figure 2, Table 1). The mean cIMT varied by 0.12 mm between the 10 geographic regions (range, 0.64 to 0.76 mm: Table 1). Likewise, the percentage with plaque varied 5-fold by region (range, 11% to 50%: Table 1) after adjustment for other covariates. The 10 geographic regions were classified by percentage with plaque into 3 groups: <20%, 20-40%, and >40% and the mean values of cIMT increased steadily with age even in geographic regions with low average rates of plaque (Figure 2).
Figure 2. Mean values of cIMT and percentage with plaque by geographic region.
Values for geographic region are classified into 3 groups (low, middle and high) and adjusted for sex.
Associations of number of plaques with maximum plaque thickness
The maximum plaque thickness was only moderately correlated with the number of plaques (r = 0.40: eFigure 1). Hence, we devised a score to combine both measures, referred to as the carotid plaque burden score (see Statistical methods). The overall mean cIMT thickness was only moderately correlated with this carotid plaque burden, with a correlation coefficient of 0.40, overall, and 0.55 excluding cases with no plaque (eFigure 2).
Associations with SBP
Overall, 42% of study participants had hypertension (SBP≥140 mmHg or DBP≥90 mmHg). Mean values of cIMT varied substantially by levels of SBP (Table 1) from 0.67 to 0.74 mm for those with SBP < 120 mmHg to those with SBP 160 mmHg or greater. Likewise, the proportions with plaque varied over 2-fold from 19%, 24%, 31% and 39% for those in the corresponding SBP categories after adjustment for other covariates (Table 1).
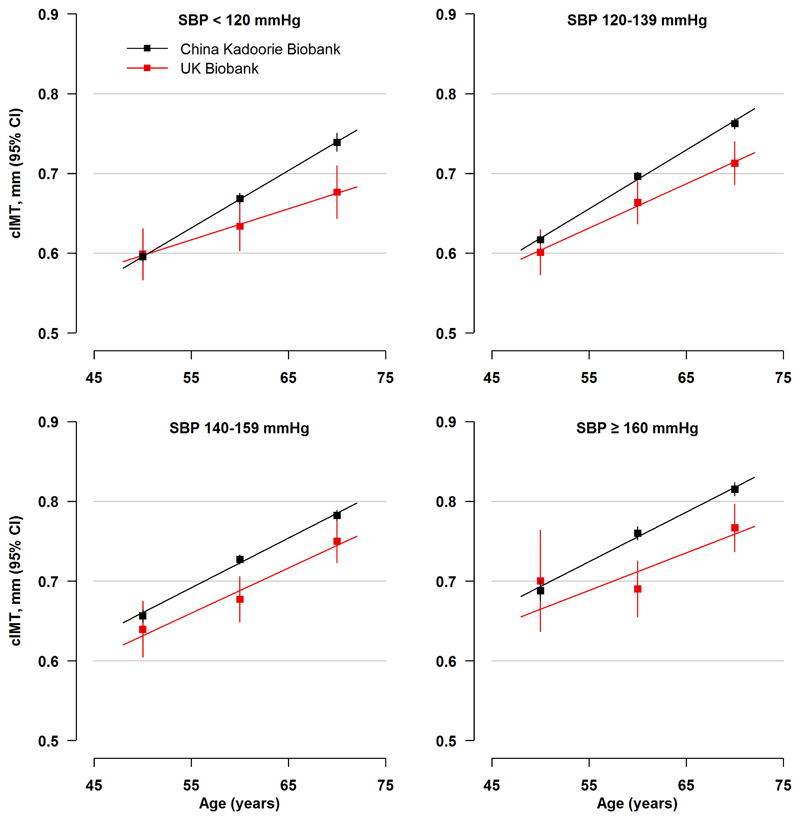
Comparison of cIMT values in Chinese versus European populations
The distribution of mean levels of SBP in CKB and UKB is shown for individuals aged 45-54 years, 55-64 years and 65-74 years, respectively in eFigure 3. Mean values of SBP were slightly higher in CKB (130 mmHg, 137 mmHg and 144 mmHg) compared with UKB (130 mmHg, 135 mmHg, and 140 mmHg) in the corresponding age groups (eFigure 3). The increase in mean level of cIMT with increasing age and blood pressure was more extreme in the Chinese population, CKB, compared with the European population in UKB (Figure 3). At all ages, the overall mean (SE) cIMT values were significantly greater in CKB than in UKB (0.70 [0.001] vs 0.66 [0.003] mm; p<0.001) in this age-sex-adjusted comparison of the sub-set of overlapping age groups in both studies.
Figure 3. Mean (95%CI) values of cIMT by age and hypertension groups in the Chinese and UK populations aged 45-74 years.
The values for cIMT in the Chinese were based on 21,062 individuals (mean age, 59 years) and in the UK population were based on 2579 individuals (mean age 63 years). The mean (SE) values in the Chinese (0.70 [0.001] mm) were greater than in the UK population (0.68 [0.003] mm, p<0.001)
Discriminating power of different plaque measures
All carotid plaque measures in CKB also varied by region, and by categories of CVD risk factors, including hypertension and cigarette smoking (eTable 3). The results show the extent to which the number of carotid plaques, plaque thickness and plaque burden varied by these determinants in all participants and in the sub-set with no prior history of CVD at the time of the examination, after adjustment for age, sex and region. The plaque burden showed slightly greater heterogeneity than either the maximum plaque thickness or the number of plaques for hypertension categories (F statistics: 127 vs 112 vs 113, respectively, in participants with no history of CVD).
Prediction of incident cases with carotid plaque versus ischaemic stroke or IHD
Among the sub-set of 23,896 participants aged 40-84 years at re-survey (i.e. excluding those outside this age range), 29.8% had a carotid plaque (Table 2). Using the observed prevalence of carotid plaques and of ischaemic stroke and IHD events in each 5-year age groups, we estimated the projected numbers of additional incident cases of plaque (among people with no plaque), stroke or IHD events likely to occur in the next 0-5 years and 5-10 years, respectively, after this examination. The projected results demonstrated that incident plaques are likely to be ~6-times more frequent than either incident ischaemic stroke or IHD events (1970 vs 296 vs 347, respectively) in the next 0-5 years by the time of the next planned resurvey in 2018, and similarly increased in 5-10 years by 2023 (1926 vs 289 vs 350, respectively).
Table 2.
Estimated number of additional cases of plaque, ischaemic stroke and ischaemic heart disease in the 0-5 and 5-10 year periods following resurvey
| At resurvey | Extra cases in years post-resurvey | |||
|---|---|---|---|---|
| N | Prevalence | 0-5 | 5-10 | |
| Any plaque | 7117 | 29.8% | 1970 | 1926 |
| Ischaemic stroke | 943 | 3.9% | 296 | 289 |
| Ischaemic heart disease | 2215 | 9.3% | 347 | 350 |
| Total | 8726 | 36.5% | 2614 | 2565 |
Values were based on prevalence in 23896 participants aged 40-84 at resurvey.
Discussion
One-third of the Chinese adult study population in CKB had evidence of carotid plaques, and the age-specific prevalence of plaques increased progressively from 6% to 57% in individuals aged 40-49 years to 70-89 years, respectively. The prevalence of plaques varied 5-fold by geographic region and the mean prevalence of plaques was 48% in 3 of the 10 geographic regions studied (Haikou, Harbin and, Liuzhou). Likewise, the prevalence of plaques varied over 2-fold by extreme blood pressure categories. The overall mean cIMT levels in Chinese were slightly greater than those in age-matched European populations assessed using similar methods over the same calendar period. The present study demonstrated the burden of carotid atherosclerosis was even more extreme in several regions in China compared with European populations, suggesting that much of the Chinese population is likely to continue to suffer high absolute risks of CVD over the next few decades.
The age-specific prevalence of carotid plaques observed in CKB in the regions with highest plaque prevalence was comparable to that observed in the Atherosclerosis Risk In Communities (ARIC) study in the USA in the early 1990’s, prior to the widespread use of LDL-lowering therapy for the prevention of CVD (14). The ARIC study had reported that 34% of their study population (aged 45-64 years) had a carotid plaque and the prevalence of plaques varied from 22% to 47% among those aged 40 to 64 years, respectively (14). The substantial variation in cIMT and prevalence of plaques by age and region in CKB highlights the importance of studying associations of cardiovascular risk factors (and particularly blood pressure) with both cIMT and carotid plaque and, subsequently, with CVD events across diverse regions of China. The higher age-specific mean values of CIMT observed in the CKB than the UKB population and other Western populations may reflect the higher proportions with untreated CVD risk factors in the Chinese population (8–14, 23–25).
The chief strength of the CKB study population was the availability of measures of both plaque thickness and plaque number, in addition to cIMT measures, in a large population which permitted analysis across a wide range of age groups and diverse urban and rural regions in China. The present study highlights the relevance of carotid plaque burden as a measure of atherosclerosis for between and within-population surveys and in studies assessing associations with genetic and plasma biomarkers for CVD. Consistent with previous reports in Western populations, plaque burden was only modestly correlated with cIMT. The evidence from Western populations suggests that plaque number and plaque thickness are stronger predictors than cIMT for both stroke and IHD (10,11). Future studies will compare the predictive value of cIMT and plaque for incident stroke and IHD events in this population. As a quantitative trait for CVD, measurement of plaque burden should also be particularly informative for future studies examining associations with genetic and plasma biomarkers, as this measure is likely to have much greater statistical power compared with studies using incident stroke or IHD events alone as outcomes (26,27).
One of the limitations of the present study is that data on plaque were limited to presence of plaques, plaque thickness and plaque number. Atherosclerotic plaques leading to stroke events may not necessarily be multiple or unduly large plaques, but plaques with a necrotic centre (including a high lipid and macrophage content) detectable as an echolucent plaques are believed to have a particularly high risk of rupture (28–30). Previous studies have demonstrated that echo-lucent plaques were more strongly predictive for stroke than echogenic plaques (28–30). Future analyses in the present cohort may assess the feasibility of using grey scale median analysis software to quantify grading of echolucent plaques (30).
Conclusions
The substantial burden of carotid plaques in the CKB population, and 5-fold difference observed by region, suggests that other factors (in addition to established CVD risk factors) remain to be discovered that account for differences in measures of atherosclerosis. The burden of carotid atherosclerosis was substantial in the Chinese and comparable with European populations and worse in some regions of China, suggesting future high absolute risks of CVD in China as in European populations. Moreover, unless concerted efforts are made to lower levels of established risk factors in China, the age-specific death rates from CVD in China are likely to continue to increase over the next few decades.
Supplementary Material
Perspectives.
Competency in Medical Knowledge 1: While both cIMT and carotid plaques increase with age, the mean levels of each are only moderately correlated with the other.
Competency of Medical Knowledge 2: Overall, one-third of the Chinese population had carotid plaques with two-thirds of these present in the carotid bulb and one-third present in the distal 1 cm of the common carotid artery.
Competency in Patient Care: Carotid artery ultrasound should assess both plaque number and maximum plaque width in addition to the more widely measured cIMT.
Competency in Interpersonal and Communication Skills: It is important to discuss the available options for individuals who are undergoing carotid artery ultrasound examinations.
Translational Outlook 1: The burden of carotid atherosclerosis in Chinese population was comparable with European populations, suggesting future high absolute risks of cardiovascular disease in the Chinese comparable with those in European populations.
Acknowledgements
This research was undertaken (in part) using the UK Biobank Resource.
Sources of Funding: This work was supported by the UK Medical Research Council [Clinical Trial Service Unit A310]; the British Heart Foundation [CH/1996001/9454]; Cancer Research UK [C500/A16896]; the Kadoorie Charitable Foundation (during 2002-2009); the Wellcome Trust [104085/Z/14/Z]; and the Chinese National Natural Science Foundation [81390541].
Abbreviations
- CCA
Common carotid artery
- cIMT
Carotid-intima media thickness
- CKB
China Kadoorie Biobank study
- cPLQ
Carotid plaque score
- CVD
Cardiovascular disease
- ECG
Electrocardiogram
- IHD
Ischaemic heart disease
- SD
Standard deviation
- SE
Standard error
- SBP
Systolic blood pressure
- UKB
UK-Biobank study
Footnotes
Disclosures: None
References
- 1).People’s Republic of China health system review. The World Health Organization. Regional Office for the Western Pacific. Health Systems in Transition. 2015;5(7) [Google Scholar]
- 2).Global Burden of Disease Mortality and Causes of Death Collaborators. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 4).O'Leary DH, Bots ML. Imaging of atherosclerosis: carotid intima-media thickness. Eur Heart J. 2010;31:1682–9. doi: 10.1093/eurheartj/ehq185. [DOI] [PubMed] [Google Scholar]
- 5).Bots ML, Evans GW, Riley WA, Grobbee DE. Carotid intima-media thickness measurements in interventional studies. Design options, progression rates, and sample size considerations: a point of view. Stroke. 2003;34:2985–94. doi: 10.1161/01.STR.0000102044.27905.B5. [DOI] [PubMed] [Google Scholar]
- 6).Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 7).Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:2748–64. doi: 10.1161/CIR.0b013e3182051bab. [DOI] [PubMed] [Google Scholar]
- 8).Den Ruijter HM, Peters SA, Anderson TJ, et al. Common carotid-intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2012;308:796–803. doi: 10.1001/jama.2012.9630. [DOI] [PubMed] [Google Scholar]
- 9).Lorenz MW, Polak JF, Kavousi M, et al. Carotid intima media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet. 2012;379:2053–62. doi: 10.1016/S0140-6736(12)60441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 2012;220:128–33. doi: 10.1016/j.atherosclerosis.2011.06.044. [DOI] [PubMed] [Google Scholar]
- 11).Polak JF, Szklo M, Kronmal RA, et al. The value of carotid artery plaque and intima-media thickness for incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. JAMA. 2013;2(2):e00008710. doi: 10.1161/JAHA.113.000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Plichart M, Celermajer DS, Zureik M, et al. Carotid intima-media thickness in plaque-free site, carotid plaques and coronary heart disease risk prediction in older adults. The Three-City Study. Atherosclerosis. 2011;219:917–24. doi: 10.1016/j.atherosclerosis.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 13).Ohira T, Shahar E, Iso H, et al. Carotid artery wall thickness and risk of stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2011;42:397–403. doi: 10.1161/STROKEAHA.110.592261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Li R, Duncan BB, Metcalf PA, et al. for the Atherosclerosis Risk in Communities (ARIC) Study Investigators B-mode-detected carotid artery plaque in a general population. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Stroke. 1994;25:2377–83. doi: 10.1161/01.str.25.12.2377. [DOI] [PubMed] [Google Scholar]
- 15).Niu L, Zhang Y, Qian M, et al. Impact of multiple cardiovascular risk factors on carotid artery intima-media thickness and elasticity. PLoS One. 2013;8:e67809. doi: 10.1371/journal.pone.0067809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Liang Y, Yan Z, Sun B, et al. Cardiovascular risk profiles for peripheral artery disease and caroitid atherosclerosis among Chinese older people: a population-based study. PloS One. 2014;9:e85927. doi: 10.1371/journal.pone.0085927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Ren L, Cai J, Liang J, Li W, Sun Z. Impact of cardiovascular risk factors on carotid intima-media thickness and degree of severity: a cross-sectional study. PloS One. 2015;10:e014418210. doi: 10.1371/journal.pone.0144182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Xie W, Liu J, Wang W, et al. Five-year change in systolic blood pressure is independently associated with carotid atherosclerosis progression: a population-based cohort study. Hypertens Res. 2014;37:960–5. doi: 10.1038/hr.2014.93. [DOI] [PubMed] [Google Scholar]
- 19).Chen Z, Li L, Chen Y, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC) Int J Epidemiol. 2005;34:1243–9. doi: 10.1093/ije/dyi174. [DOI] [PubMed] [Google Scholar]
- 20).Chen Z, Chen J, Collins R, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40:1652–66. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).UK Biobank imaging modality: carotid ultrasound. http://biobank.ctsu.ox.ac.uk/crystal/docs/carult_explan_doc.pdf.
- 23).Sillesen H, Muntendam P, Adourian A, et al. Carotid plaque burden as a measure of subclinical atherosclerosis. JACC Cardiovasc Imaging. 2012;5:681–9. doi: 10.1016/j.jcmg.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 24).Engelen L, Ferreira I, Stehouwer CD, Boutouyrie P, Laurent S, on behalf of the Reference Values for Arterial Measurements Collaboration Reference intervals for common carotid intima-media thickness measured with echotracking: relation with risk factors. Eur Heart J. 2013;34:2368–80. doi: 10.1093/eurheartj/ehs380. [DOI] [PubMed] [Google Scholar]
- 25).Lim TK, Lim E, Dwivedi G, Kooner J, Senior R. Normal value of carotid intima-media thickness — a surrogate marker of atherosclerosis: quantitative assessment by B-mode carotid ultrasound. J Am Soc Echocardiogr. 2008;21:112–6. doi: 10.1016/j.echo.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 26).Bis JC, Kavousi M, Franceschini N, et al. Meta-analysis of genome-wide association studies from the CHARGE consortium identifies common variants associated with carotid intima media thickness and plaque. Nat Genet. 2011;43:940–7. doi: 10.1038/ng.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).den Hoed M, Strawbridge RJ, Almgren P, et al. GWAS-identified loci for coronary heart disease are associated with intima-media thickness and plaque presence at the carotid artery bulb. Atherosclerosis. 2015;239:304–1027. doi: 10.1016/j.atherosclerosis.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28).Mathiesen EB, Bønaa KH, Joakimsen O. Echolucent plaques are associated with high risk of ischemic cerebrovascular events in carotid stenosis: the Tromsø study. Circulation. 2001;103:2171–5. doi: 10.1161/01.cir.103.17.2171. [DOI] [PubMed] [Google Scholar]
- 29).Peters SAE, Bots ML, Lind L, Groenewegen KA, Karlijn A, de Korte C, on behalf of the METEOR study group The impact of variability in ultrasound settings on the measured echolucency of the carotid intima-media. J Hypertens. 2013;31:1861–7. doi: 10.1097/HJH.0b013e3283623548. [DOI] [PubMed] [Google Scholar]
- 30).Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34:290–6. doi: 10.1159/000343145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.