Abstract
Background.
Prior research indicates that, compared to individuals born in the United States (US), immigrants are less likely to experience mental health and inhibitory control problems. However, our understanding of overeating and binge eating—both related to mental health and inhibitory control—among immigrants in the US remains limited. Drawing from a large national study, we report the prevalence of overeating and binge eating among immigrants vis-à-vis the US-born.
Methods.
The data source used for the present study is the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III, 2012–2013), a nationally representative survey of 36,309 civilian, non-institutionalized adults ages 18 and older in the US. Logistic regression was employed to examine the relationship between immigrant status and key outcomes.
Results.
The prevalence of any (Immigrants = 7.8%, US-born = 17.0%) and recurrent overeating (Immigrants = 2.9%, US-born = 5.3%) was lower among immigrants than US-born individuals. Among those reporting recurrent overeating, the prevalence of binge eating with loss of control was comparable among immigrant (37.2%) and US-born participants (39.9%) in general. However, stratified analyses revealed that risk of binge eating with loss of control was lower among immigrant women compared to US-born women (AOR = 0.54, 95% CI = 0.29–0.98).
Conclusions.
Findings from the present study provide clear results that immigrants are substantially less likely to overeat as compared to US-born individuals and that, among women but not men, immigrant status is associated with lower risk of binge eating with loss of control.
Keywords: immigrants, overeating, binge eating, acculturation, mental health, impulsivity
Introduction
Overeating and binge eating are important public health problems affecting the well-being of millions of people across the United States (US). Overeating can be understood as eating an unusually large amount of food over a short period of time and binge eating is typically defined as overeating frequently leading to physical discomfort and often accompanied by a loss of control (American Psychiatric Association, 2013). We know that both behaviors are related to myriad adverse consequences including weight gain and unstable weight, severe obesity, elevated diastolic blood pressure, limitations in daily activities, difficulty sleeping, subjective distress, depressed mood, and poor overall health (Ackard, Neumark-Sztainer, Story, & Perry, 2003; De Zwaan et al., 1994; Goldschmidt et al., 2016; Johnson et al., 2001; Wonderlich et al., 2009; Udo et al., 2016; Mustelin et al., 2017). Indeed, recent estimates suggest that binge eating and other eating-related problems are elevated in the US and elsewhere (Smink, van Hoeken, & Hoek, 2012), and represent an important source of social and economic burden in terms of increases in healthcare costs and losses in productivity (Samnaliev et al., 2015).
Overeating and Binge Eating among Immigrants
An important underexplored area of research is overeating and binge eating among immigrants. This line of inquiry is important for a number of reasons. First, the US is home to a large number of immigrants, and the children of immigrants are projected to account for a very large proportion of population growth in the 21st century (López & Bialik, 2017). Indeed, recent estimates suggest that there are more than 40 million foreign-born individuals living in the US, and roughly one in four (27%) persons residing in the US is either an immigrant or the child of an immigrant (Zong et al., 2015). Thus, it is critical we have an in-depth understanding of an array of health risk behaviors and problem outcomes among immigrants, including overeating and binge eating, to inform public health and prevention efforts. Second, prior research on overeating and binge eating among immigrants in the US is rather limited. Swanson and colleagues (2012) conducted a study with Mexican nationals suggesting that migration to the US, and greater exposure to US culture, are associated with increased risk of binge eating and binge eating disorder (BED). This finding is in keeping with other epidemiologic research on Latinos, which has shown that rates of binge eating are higher among US-born Latinos (compared to foreign-born Latinos) and that risk of binge eating is higher among children of Latino immigrants than among first-generation arrivals (Alegría et al., 2007), both of which point to the negative impact of acculturation to US culture on healthy eating.
A third—and particularly salient—reason to examine the immigrant-binge eating link is that it is reasonable to suspect that rates of overeating/binge eating, and the characteristics of those who overeat, may be distinct among foreign-born individuals in general (not just those from Latin America) as compared to individuals born in the US. Prior research points to substantial cross-national variation in binge eating, and in feeding and eating disorders more broadly (Makino et al., 2004; Hoek, 2016). Recent research has also found that risk of BED is greater in the US than in a number of lower-middle and high income countries (Kessler et al., 2013). Also, while findings are not entirely uniform (Alegría, Canino, Stinson, & Grant, 2006; Alegría et al., 2007), a large and growing body of research has shown that, compared to US-born individuals, immigrants tend to report substantially lower levels of health problems (i.e., mental health disorders, obesity) and to take part in unhealthy behaviors (e.g., substance use, problem gambling, crime and violence) at far lower rates than individuals born in the US (Kaplan et al., 2004; Takeuchi et al., 2007; Breslau et al., 2009; Salas-Wright et al., 2014a; Salas-Wright & Vaughn, 2014; Vaughn et al., 2014; Salas-Wright et al., 2018).
Theories on Migration and Health and Involvement in Unhealthy Behavior
A number of hypotheses have been advanced as scholars have attempted to explain why immigrants, on average, tend to fare better than US-born individuals in terms of health and participation in unhealthy behaviors (see Alarcón et al., 2016; Alegría et al., 2017; Salas-Wright & Schwartz, 2019). Perhaps the most well-known is the healthy migrant hypothesis, which argues that immigrants fare better than non-migrants due to self-selection. The logic here is rather straightforward: individuals who pursue opportunities in a foreign land are more likely to be physically healthy and psychologically resilient (e.g., less propensity for mental health problems, greater inhibitory control) than non-migrants. This logic may be applicable to binge eating as it is reasonable to surmise that healthy/resilient immigrants would be less likely to binge eat, both because it is a health risk behavior influenced by impulsivity/inhibitory control (Lavagnino et al., 2016) and because it is related to other outcomes (e.g., mental health and substance use disorders [Hudson et al., 2007; Gearhardt et al., 2011; Davis, 2013]) that are also, quite likely, influenced by migration-related self-selection.
A related framework that has been applied to alcohol and other drug use is the inoculation hypothesis which argues that immigrants—many of whom originate from Latin America, Asia, Africa, and other regions that often have more conservative substance use views—who migrate later on in their development (e.g., during late adolescence or young adulthood) internalize their home country’s conservative substance use norms that protect (or “inoculate”) them from post-migration substance use initiation and misuse (Alegría et al., 2008; Canino et al., 2008; Marsiglia et al., 2008). It is possible that similar inoculation processes may take place for binge eating if immigrants originate from countries/contexts where temperance is highly valued and extreme overeating is discouraged. However, this hypothesized pattern remains uncertain, as evidence on the cross-national rates of binge eating remains mixed, with some studies showing lower risk among people in non-Western countries (Makino et al., 2004) and others showing elevated levels of binge eating in these regions (Hoek, 2016).
Migration scholars have also noted that, unfortunately, the protective effect of foreign birth for outcomes such as alcohol and drug use and mental health disorders tends to weaken over time, particularly among those who migrate early on in life. Acculturation theorists note that, with time, many immigrants adopt cultural practices and values of their receiving country/context and that rates of cultural change are particularly noteworthy among individuals who migrate during childhood (Schwartz & Unger, 2017; Schwartz et al., 2010). Prior research has demonstrated that greater assimilation, as well as longer duration in the US, is related with increased risk of involvement in a number of unhealthy behaviors related to inhibitory control problems, including alcohol and other drug misuse and problem gambling (Salas-Wright et al., 2014b; Wilson et al., 2015; Salas-Wright, et al., 2016). It is certainly plausible that overeating and binge eating could also be related to greater acculturation and/or exposure to the US, as such a pattern is in keeping with the transnational research with Mexican nationals discussed above (see Swanson et al., 2012) and prior research focused on obesity (Kaplan et al., 2004; Roshania et al., 2008).
Beyond acculturation, cultural stress theorists have noted that adverse migration-related experiences such as discrimination and negative context of reception are also related to increased risk of health problems and health risk behavior (Lorenzo-Blanco et al., 2017; Salas-Wright & Schwartz, 2019). That is, it is argued that the driving force in changing health-risk behaviors may not be acculturation per se, but rather experiences of identity-based marginalization that can heighten stress in individuals and families (and, in turn, increase risk for unhealthy behaviors by means of coping and other mechanisms) (Salas-Wright et al., 2015). Research on migration-related stress and overeating/binge eating is limited, but there is evidence that immigrants may change their dietary habits to assimilate to US culture, particularly when questioned about their status as a foreign-born individual or immigrant (Damas et al., 2018; Guendelman et al., 2011).
The Present Study
The present study, drawing from a nationally representative survey (National Epidemiologic Survey on Alcohol and Related Conditions [NESARC], 2012–2013) designed and implemented by the National Institutes of Health, examines the relationship between foreign birth, key migration-related factors, and risk of overeating and binge eating in the US. We examined two interrelated research questions and corresponding hypotheses.
Are immigrants less likely than US-born individuals to report overeating and binge eating? Based on prior research on immigrants and health risk behavior, we hypothesize that rates of overeating and binge eating will be lower among foreign-born individuals than those born in the US. Given the important differences in risk of overeating and binge eating among men and women (Barry et al., 2002; Striegel-Moore et al., 2003; Udo & Grilo, 2018), we also conduct tests for effect modification status by gender. We do not advance a specific hypothesis related to gender modification.
Does risk of overeating and binge eating differ by key migration-related factors? Based on prior research on migration and health-risk behavior (Salas-Wright & Schwartz, 2019), we hypothesize that risk will be lowest among immigrants who arrive as adults, who have spent less time in the US, and among first generation immigrants (as compared to 2nd and 3rd generation).
Method
Sample and Procedures
This study draws from NESARC-III data collected between 2012 and 2013 (Grant et al., 2014). The NESARC is a nationally representative survey of 36,309 civilian, non-institutionalized adults ages 18 and older, and is one of few national studies with information on overeating and binge eating among immigrants. Utilizing a multistage cluster sampling design, the NESARC investigators interviewed individuals living in all 50 states and the District of Colombia. Data were collected through face-to-face structured psychiatric interviews in which interviewers administered the NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS-5), which is described at length elsewhere (Grant et al., 2015). The AUDADIS-5 is a diagnostic interview developed by the National Institutes of Health for purposes of examining substance use and other select psychiatric disorders, including binge eating disorder, based on DSM-5 criteria. The AUDADIS-5 has shown to produce scores with strong procedural validity and acceptable reliability in the assessment of an array of disorders (Grant et al., 2015; Hasin et al., 2015). Participants had the option of completing the NESARC-III interview in English, Spanish, Korean, Vietnamese, Mandarin, or Cantonese.
Survey Measures
Overeating and Binge Eating.
Several sequential items were used to measure overeating and binge eating. All participants were asked: “Have you ever eaten an unusually large amount of food within any 2-hour period, not including the holidays?” Those responding affirmatively (“yes”) were classified as reporting any overeating and coded as 1. Those responding “no” were skipped out of the eating/overeating section of the NESARC interview. Those reporting at least a single episode were subsequently asked: “Was there ever a time when you ate an unusually large amount of food on average at least once a week for at least 3 months?” (no = 0, yes = 1). Those responding affirmatively were classified as having experienced recurrent episodes of overeating and were subsequently asked if they ever experienced loss of control while overeating (i.e., “During any of this time did you feel that you couldn’t stop eating or control how much or what you were eating?”). Those reporting recurrent overeating with loss of control were classified as having taken part in binge eating and coded as 1.
The NESARC also includes a dichotomous (no = 0, yes = 1) BED variable based on criteria from the DSM-V, including recurrent overeating, loss of control while overeating, and negative emotionality related to overeating and/or behaviors such as eating alone to avoid embarrassment or eating despite lack of hunger (Udo & Grilo, 2018). We examine this variable as well; however, due to the low prevalence of BED, we focus primarily on the higher prevalence outcomes (overeating, binge eating) that allow for more complex analyses (i.e., tests across migration-related differences, links between binge eating and other outcomes) and stable prevalence estimates.
Immigrant status.
Immigrant status was based on the following question: “Were you born in the US?” Consistent with prior NESARC-based studies of immigrants, we classified those responding affirmatively as US-born and those reporting they were not born in the US— including individuals born in US territories (e.g., Guam, Puerto Rico, etc.)—as immigrants or foreign born (Breslau et al., 2009; Blanco et al., 2013). Individuals reporting foreign birth were asked to report their country of birth and age of arrival in the US (which allows researchers, in conjunction with respondent age, to estimate the number of years in the US). As in prior NESARC studies, we were also able to classify individuals by second (child of one or more immigrants) or third (grandchild of one or more immigrants) generation immigrant status based on family history data collected as part of the survey (Vaughn et al. 2014).
Mental Health/Substance Use Disorders and Impulsive Behavior.
As an exploratory analysis, we examined lifetime mental health and substance use disorder history and participant impulsive behavior among immigrant and US-born participants. These analyses are based on prior research suggesting that risk of overeating and binge eating is elevated among individuals with mental health problems and among those who struggle with inhibitory control. In terms of mental health disorders, we generated an “any disorder” variable for which participants reporting one or more mood, anxiety, or trauma-related disorders (as measured by the AUDADIS-5) were coded as 1 and those reporting no history of mental health disorders were coded as 0. Notably, the NESARC does not gather data on schizophrenia spectrum and other psychotic disorders (Kirkbride, 2017). Similarly, respondents reporting one or more lifetime substance use disorders (e.g., alcohol, cannabis) were coded as 1, and all others coded as 0. For impulsivity, participants were asked: “Have you often done things impulsively, not caring about the consequences?” Those responding “no” were coded as 0 and those responding “yes” were coded as 1.
Sociodemographic Controls.
Sociodemographic variables included age, gender, race/ethnicity, household income, education level, and marital status.
Statistical Analyses
Survey adjusted binomial logistic regression was employed to examine the association between immigrant status (specified as an independent or predictor variable) and overeating and binge eating (specified in separate equations as dependent or outcome variables) while controlling for sociodemographic confounds (see Table 1). We also employed logistic regression to assess the association between migration-related factors (i.e., age of arrival, immigrant generation) and risk of overeating (see Table 2 and Figure 1) and binge eating (see Table 3), and examined the associations among mental health, substance use disorders, impulsivity, and risk of overeating (see Figure 2). Adjusted odds ratios (AORs) were considered to be significant (p < .05) if the associated 95% confidence intervals did not cross 1.00 when controlling for sociodemographic factors. For all statistical analyses, weighted prevalence estimates and standard errors were computed using Stata 15.1 MP software. This analytic method implements a Taylor series linearization to adjust standard errors for complex survey sampling design effects.
Table 1.
Overeating and Binge Eating Episodes among Foreign and US-Born Adults in the United States
| Place of Birth | Odds Ratio | |||||||
|---|---|---|---|---|---|---|---|---|
| US-Born (n = 29,896; 84.05%) | Foreign Born (n = 6404; 15.95%) | Unadjusted | Adjusted | |||||
| % | (95% CI) | % | (95% CI) | OR | (95% CI) | AOR | (95% CI) | |
| Full Sample | ||||||||
| Any Overeating | ||||||||
| No | 83.95 | (82.0–83.8) | 92.15 | (91.2–93.0) | 1.00 | 1.00 | ||
| Yes | 17.05 | (16.2–18.0) | 7.85 | (7.0–8.8) | 0.41 | (0.36–0.47) | 0.46 | (0.40–0.53) |
| Recurrent Overeating | ||||||||
| No | 94.65 | (94.2–95.1) | 97.10 | (96.7–97.5) | 1.00 | 1.00 | ||
| Yes | 5.35 | (4.9–5.8) | 2.90 | (2.5–3.4) | 0.53 | (0.44–0.63) | 0.51 | (0.41–0.63) |
| Binge Eating Episode (i.e. Overeating w/ Loss of Control) | ||||||||
| No | 60.12 | (57.0–63.2) | 62.79 | (54.6–70.3) | 1.00 | 1.00 | ||
| Yes (n = 1,735) | 39.88 | (36.8–43.0) | 37.21 | (29.7–45.4) | 0.89 | (0.62–1.29) | 0.93 | (0.62–1.39) |
| Male | ||||||||
| Any Overeating | ||||||||
| No | 77.88 | (76.4–79.3) | 89.27 | (87.6–90.7) | 1.00 | 1.00 | ||
| Yes | 22.12 | (20.7–23.6) | 10.73 | (9.3–12.4) | 0.42 | (0.35–0.50) | 0.48 | (0.40–0.59) |
| Recurrent Overeating | ||||||||
| No | 93.46 | (92.7–94.1) | 96.03 | (95.1–96.8) | 1.00 | 1.00 | ||
| Yes | 6.54 | (5.9–7.3) | 3.97 | (3.2–4.9) | 0.59 | (0.46–0.75) | 0.55 | (0.42–0.74) |
| Binge Eating Episode (i.e. Overeating w/ Loss of Control) | ||||||||
| No | 72.82 | (69.2–76.2) | 64.48 | (54.4–73.4) | 1.00 | 1.00 | ||
| Yes (n = 943) | 27.18 | (23.8–30.8) | 35.52 | (26.6–45.6) | 1.48 | (0.93–2.34) | 1.19 | (0.76–1.88) |
| Female | ||||||||
| Any Overeating | ||||||||
| No | 87.61 | (86.8–88.4) | 94.93 | (94.0–95.7) | 1.00 | 1.00 | ||
| Yes | 12.39 | (11.6–13.2) | 5.07 | (4.3–6.0) | 0.38 | (0.31–0.46) | 0.42 | (0.34–0.52) |
| Recurrent Overeating | ||||||||
| No | 95.75 | (95.3–96.1) | 98.14 | (97.6–98.6) | 1.00 | 1.00 | ||
| Yes | 4.25 | (3.8–4.7) | 1.86 | (1.4–2.4) | 0.43 | (0.31–0.58) | 0.43 | (0.30–0.63) |
| Binge Eating Episode (i.e. Overeating w/ Loss of Control) | ||||||||
| No | 42.14 | (38.0–46.4) | 59.31 | (45.5–71.8) | 1.00 | 1.00 | ||
| Yes (n = 792) | 57.86 | (53.6–62.0) | 40.69 | (28.2–54.5) | 0.50 | (0.28–0.89) | 0.54 | (0.29–0.98) |
Note: Adjusted odds ratios (AOR) adjusted for age, gender, race/ethnicity, household income, education level, and marital status. Odds ratios and 95% confidence intervals in bold are statistically significant. Analyses for binge eating conducted only with those reporting recurrent episodes of overeating. Interaction tests identified a significant interaction between gender and immigrant status (AOR = 2.92, 95% CI = 1.46–5.85) when predicting binge eating among those with recurrent episodes of overeating.
Table 2.
Testing Variation in the Immigrant-Overeating Link across Migration-Related Differences
| Prevalence | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| % | (95% CI) | OR | (95% CI) | AOR | (95% CI) | |
| Any Overeating | ||||||
| Age of Arrival | ||||||
| US-Born | 17.05 | (16.2–18.0) | 1.00 | 1.00 | ||
| Childhood (17 or younger) | 12.14 | (10.4–14.1) | 0.67 | (0.56–0.80) | 0.64 | (0.53–0.76) |
| Adulthood (18 or older) | 5.93 | (5.1–6.8) | 0.31 | (0.26–0.36) | 0.36 | (0.30–0.43) |
| Immigrant Generation | ||||||
| First Generation (Foreign Born) | 7.85 | (7.0–8.8) | 1.00 | 1.00 | ||
| Second Generation | 16.75 | (15.3–18.3) | 2.36 | (2.01–2.77) | 2.12 | (1.79–2.50) |
| Third Generation or Greater | 17.10 | (16.2–18.1) | 2.42 | (2.13–2.75) | 2.22 | (1.92–2.56) |
| Recurrent Overeating | ||||||
| Age of Arrival | ||||||
| US-Born | 5.35 | (4.9–5.8) | 1.00 | 1.00 | ||
| Childhood (17 or younger) | 4.66 | (3.6–6.0) | 0.86 | (0.66–1.13) | 0.73 | (0.54–0.97) |
| Adulthood (18 or older) | 2.11 | (1.7–2.6) | 0.38 | (0.30–0.49) | 0.38 | (0.29–0.51) |
| Immigrant Generation | ||||||
| First Generation (Foreign Born) | 2.90 | (2.5–3.4) | 1.00 | 1.00 | ||
| Second Generation | 5.85 | (4.9–7.0) | 2.08 | (1.64–2.65) | 2.02 | (1.57–2.59) |
| Third Generation or Greater | 5.27 | (4.6–5.4) | 1.86 | (1.55–2.24) | 1.93 | (1.52–2.44) |
Note: Adjusted odds ratios (AOR) adjusted for age, gender, race/ethnicity, household income, education level, and marital status. Odds ratios and 95% confidence intervals in bold are statistically significant.
Figure 1.
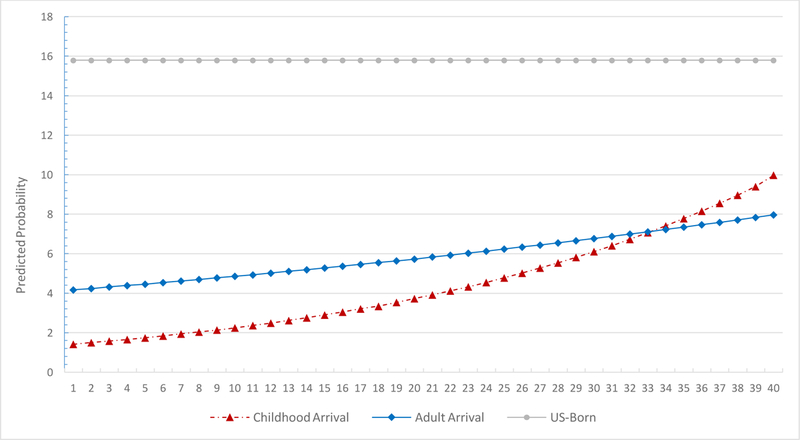
Linearized predicted probability of overeating episode by number of years in the United States (US) among immigrants arriving during childhood (prior to age 18) and as adults (age 18 or older). Probabilities predicted while holding age, gender, race/ethnicity, family income, education level, and marital status at mean values.
Table 3.
Testing Variation in the Immigrant-Binge Eating Link across Migration-Related Differences, by Gender
| Male (n = 943) | Female (n = 792) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence | Unadjusted | Adjusted | Prevalence | Unadjusted | Adjusted | |||||||
| % | (95% CI) | OR | (95% CI) | AOR | (95% CI) | % | (95% CI) | OR | (95% CI) | AOR | (95% CI) | |
| Binge Eating (Overeating with Loss of Control) | ||||||||||||
| Age of Arrival | ||||||||||||
| US-Born | 27.18 | (23.8–30.8) | 1.00 | 1.00 | 57.86 | (53.6–62.0) | 1.00 | 1.00 | ||||
| Childhood (17 or younger) | 32.92 | (21.7–46.5) | 1.31 | (0.72–2.39) | 1.08 | (0.61–1.93) | 45.35 | (24.3–68.2) | 0.60 | (0.22–1.64) | 0.71 | (0.26–1.90) |
| Adulthood (18 or older) | 38.64 | (26.8–52.0) | 1.69 | (0.95–3.00) | 1.34 | (0.72–2.49) | 37.49 | (23.0–54.6) | 0.44 | (0.22–0.86) | 0.44 | (0.21–0.94) |
| Immigrant Generation | ||||||||||||
| First Generation (Foreign Born) | 35.52 | (26.6–45.6) | 1.00 | 1.00 | 40.69 | (28.2–54.5) | 1.00 | 1.00 | ||||
| Second Generation | 33.01 | (23.0–44.9) | 0.89 | (0.46–1.73) | 1.05 | (0.56–1.96) | 51.10 | (40.1–62.0) | 1.52 | (0.72–3.21) | 1.47 | (0.71–3.06) |
| Third Generation or Greater | 26.07 | (22.1–30.5) | 0.64 | (0.40–1.03) | 0.71 | (0.41–1.23) | 58.80 | (54.3–63.1) | 2.08 | (1.16–3.70) | 2.09 | (1.13–3.86) |
Note: Adjusted odds ratios (AOR) adjusted for age, gender, race/ethnicity, household income, education level, and marital status. Odds ratios and 95% confidence intervals in bold significant. Loss of control only measured among participants who endorsed recurrent overeating episodes. Supplemental tests revealed that, among females, adult immigrants were significantly less likely than childhood immigrants to report loss of control (AOR = 0.18, 95% CI = 0.04–0.77).
Figure 2.
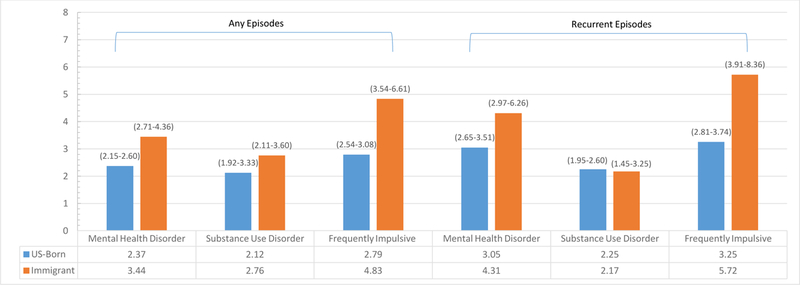
Adjusted odds ratios (AOR) for the association between and lifetime mental health disorder diagnosis and frequent impulsive behavior with overeating. AORs adjusted for age, gender, race/ethnicity, household income, education level, and marital status. Immigrant status significantly moderated the association between binge eating and [1] mental health diagnosis (Any: AOR = 1.55, 95% CI = 1.21–1.98; Recurrent Episodes: AOR = 1.52, 95% CI = 1.00–2.30), [2] substance use disorder (Any: AOR = 1.44, 95% CI = 1.10–1.88; Recurrent Episodes = not significant), and [3] frequent impulsive behavior (Any: AOR = 1.90, 95% CI = 1.37–2.64; Recurrent Episodes: AOR = 1.85, 95% CI = 1.21–2.82).
Results
Are Immigrants Less Likely to Report Overeating, Binge Eating, and BED?
As shown in Table 1, the prevalence of any (Immigrants = 7.8%, US-born = 17.0%) and recurrent episodes of overeating (Immigrants = 2.9%, US-born = 5.3%) was markedly lower among immigrants as compared to US-born individuals. We found this relationship to be significant while controlling for age, gender, race/ethnicity, family income, education level, and marital status: immigrants were roughly two times less likely than their US-born counterparts to report any (AOR = 0.46, 95% CI = 0.40–0.53) or recurrent overeating episodes (AOR = 0.51, 95% CI = 0.41–0.63). Stratifying by gender, we found that the magnitude of the association between immigrant status and overeating was comparable between males and females. This finding was supported by the non-significant interaction term for immigrant status and gender (i.e., immigrant*gender) in predicting overeating.
Among individuals reporting recurrent overeating episodes in the general population, we identified no differences between immigrants and US-born individuals in binge eating. However, we found that gender significantly moderated the association between immigrant status and binge eating (i.e., overeating with loss of control) (AOR = 2.92, 95% CI = 1.46–5.85) and that—whereas no difference was observed among males—significant differences in binge eating risk were observed between US/immigrant females (AOR = 0.54, 95% CI = 0.29–0.98).
In supplemental analyses conducted with the full sample (not shown), we found a similar pattern for BED: compared to US-born individuals (Prevalence = 0.82%), risk of BED was lower among immigrants in general (Prevalence: 0.48%; AOR = 0.55, 95% CI = 0.34–0.83). Analyses by gender indicated a significant immigrant-BED association for women (Prevalence = 1.13% for US-born and 0.40% for immigrants; AOR = 0.33, 95% CI = 0.16–0.70) but not for men.
Does Risk of Overeating and Binge Eating Differ by Key Migration-Related Factors?
Beyond examining gender differences, we also examined the relationship between overeating/binge eating and immigrant status across salient migration-related differences. As shown in Table 2, compared to US-born individuals, immigrants arriving during childhood (i.e. age 17 or younger) and adulthood (i.e. age 18 or older) were significantly less likely to report any or recurrent episodes of overeating. We also found differences between individuals who migrated as children versus those who migrated as adults. More specifically, we found that the likelihood of any overeating (AOR = 0.63, 95% CI = 0.51–0.80) and recurrent overeating (AOR = 0.60, 95% CI = 0.40–0.89) were significantly lower among those who immigrated as adults (as compared to those who immigrated us children).
We also examined differences across immigrant generations, finding that—compared to first-generation immigrants—those who were second (i.e., children of immigrants) or third generation immigrants (i.e., grandchildren of immigrants) were roughly twice as likely to report overeating. Supplemental analyses revealed that the immigrant-overeating link was stable across region of origin (i.e., Africa, Asia, Europe, Latin America) for any overeating; however, with respect to recurrent overeating, significant associations were only observed for immigrants from Africa (AOR = 0.21, 95% CI = 0.07–0.62), Asia (AOR = 0.44, 95% CI = 0.24–0.81), and Latin America (AOR = 0.47, 95% CI = 0.38–0.59).
Table 3 shows the relationship between binge eating and immigrant status by age of arrival and immigrant generation. We found that, among females, immigrants who arrived as adults were less likely to report binge eating (AOR = 0.44, 95% CI = 0.21–0.94) compared to US-born individuals. Supplemental tests revealed that, among females, adult immigrants were significantly less likely than childhood immigrants to report binge eating (AOR = 0.18, 95% CI = 0.04–0.77). We also found, among females, that third generation immigrants were more likely that first generation immigrants (i.e., foreign born individuals) to report binge eating (AOR = 2.09, 95% CI = 1.13–3.86). No differences were identified between immigrant males and US-born males.
As displayed in Figure 1, we also found that, within the subsample of immigrants, number of years in the US was significantly associated with the likelihood of overeating, but only among those who immigrated as children (AOR = 1.05, 95% CI = 1.03–1.08). Number of years in the US was not significantly associated with recurrent episodes of overeating. No significant association was observed between duration in the US and risk of binge eating.
Exploratory Analysis:
The Relationships between Overeating/Binge Eating, Mental Health, and Impulsivity
Figure 2 displays the association between overeating and risk of mental health disorders, substance use disorders, and frequent impulsive behavior among US and foreign-born individuals. Across nativity, all individuals—both US or foreign born—who reported overeating were significantly more likely to meet criteria for one or more mental health or substance use disorders and to report frequent impulsive behavior; however, the association between overeating and mental health/impulsivity problems was significantly greater among immigrants than among those born in the US. For instance, whereas US-born individuals reporting recurrent overeating were roughly 3 times more likely to report frequent impulsive behavior (AOR = 3.25, 95% CI = 2.81–3.74), foreign-born individuals reporting recurrent overeating were nearly 6 times more likely to endorse frequent impulsive behavior (AOR = 5.72, 95% CI = 3.91–8.36). We did not examine these associations for binge eating due to low sample size for subgroups and the resulting statistical limitations (i.e., unstable estimates, lack of statistical power to detect differences).
Discussion
Findings from the present study indicate that immigrants are substantially less likely to report any or recurrent overeating as compared to US-born individuals. Along the same lines, we also found that, among women reporting recurrent overeating, rates of binge eating—or overeating marked by loss of control—were substantially lower among immigrant women than among their US-born counterparts. This pattern of findings is in keeping with a burgeoning line of inquiry suggesting that immigrants, despite frequently experiencing stress and socioeconomic disadvantage, are markedly less likely to experience a variety of health problems (i.e., mental health disorders, obesity) and take part in unhealthy behaviors (i.e., alcohol and other drug misuse, problem gambling, violence) known to compromise health and well-being (Bates et al., 2008; Vaughn et al., 2014; Salas-Wright et al., 2018). Simply, our results suggest that the “immigrant paradox” may extend to overeating and to binge eating, particularly among women.
Beyond examining the behavior of immigrants vis-à-vis the US-born, we also examined the importance of migration-related factors as related to risk of overeating and binge eating. Prior research examining health problems and unhealthy behaviors among immigrants has found that risk of adverse outcomes increases among immigrants with earlier age of arrival, greater duration in the US, and across immigrant generations. Our results for overeating (among men and women) and binge eating (among women only) fall in line with prior research as we found that [1] risk was lower among those who immigrated as adults (as compared to those who immigrated as children), [2] risk increased significantly with duration among those arriving during childhood, and [3] rates of overeating/binge eating among the children and grandchildren of immigrants were no different than those of individuals without recent family history of migration. Taken together, these findings provide support for selection (i.e., individuals who migrate are psychologically and physically healthy) and inoculation theorizing (i.e., health-related norms from sending countries are internalized and preserved among those who migrate later in life) as well as for acculturation theorizing (i.e., individuals take on beliefs and practices of the receiving context over time, particularly those who arrive early on in life) as related to binge eating (Schwartz et al., 2010).
We also examined the relationship between overeating and mental/substance use disorders and impulsive behavior among immigrant and US-born individuals. Our findings indicate that, compared to their US-born counterparts, immigrants who report recurrent overeating are more likely to have experienced one or more mental health and substance use disorders and to behave impulsively. Paradoxically, this too is in keeping with theorizing related to the healthy migrant hypothesis (i.e., those who migrate are psychologically and physically healthy) as it suggests that immigrants who take part in unhealthy behaviors such as recurrent overeating are more likely to experience underlying psychiatric problems and, potentially, genetic risk related to self-control deficits (as impulsivity/inhibitory control have strong genetic underpinnings) (see Beaver et al., 2008; Brewer & Potenza, 2008). That is, the minority of immigrants who report a sustained pattern of overeating are more atypical among immigrants in terms of mental health, substance use, and impulsivity (well documented risks for and correlates of eating problems) than are US-born individuals who overeat vis-à-vis other US-born individuals. In other words, our findings for mental health and substance use disorders and impulsive behavior seem to be the exception that supports the rule of self-selection among immigrants.
Our findings have several implications for future research and prevention efforts. First, given the compelling evidence that the protective effects of foreign birth tend to fade over time (especially among those who arrive as children) and across immigrant generations, it is critical that further research be conducted to identify and attempt to preserve the protective factors (e.g., cultural norms around food and self-control) for overeating and binge eating. Similarly, our findings suggest that efforts to prevent overeating/binge eating among immigrants would likely be best targeted to those arriving as children and the children of immigrants as foreign-born adults report very low levels of episodic and recurrent binge eating, even when they have spent substantial time in the US. Finally, our findings also suggest that recurrent overeating among immigrants may be viewed as a “flag” for potential psychiatric comorbidity (i.e., mental health and substance use disorders) and risk of impulsive behavior. Primary care providers and psychologists/social workers who encounter immigrants struggling with overeating may, for example, consider evaluating these individuals for a broader array of psychiatric and impulse-related behavior issues.
Study Limitations
Findings from the present study should be interpreted in light of several limitations. First, we were unable to account for potential self-report and cross-cultural biases relevant to the assessment of overeating/binge eating and psychiatric disorders. This is an important limitation as it is certainly plausible that immigrants may have under- or over-reported overeating/binge eating due to concerns about stigma and/or cultural differences. A second limitation is that NESARC-III data also do not allow us to identify migration reason (e.g., labor, family) or to identify refugees/asylum seekers. It is possible, for instance, that refugees or other immigrants who have experienced substantial hardship and/or lack of access to sustenance may have different post-migration outcomes. Despite this limitation, refugees represent a rather small proportion of the total foreign-born population in the US, as only 5–10% of the migrants arriving each year are refugees (Zong et al., 2015). Third, the relatively low prevalence of binge eating, and the corresponding limitations in statistical power, did not allow us to conduct all analyses with binge eating variable. Finally, although the NESARC gathers data on an array of salient sociodemographic factors, the dataset does not provide information on more specific contextual, situational, and genetic factors that may play a role in overeating/binge eating.
Conclusions
The present study provides new evidence on health behaviors among immigrants. We see compelling evidence that rates of overeating and binge eating are substantially lower among immigrants as compared to those born in the US. Consistent with prior research on immigrants and health and health-related behaviors, we also found that the observed protective effects of foreign birth seem to be weakest among those who arrive as children and attenuate with greater time in the US. And, notably, among the minority of immigrants reporting overeating, risk for psychiatric problems and impulsive behavior was elevated as compared to US-born individuals who overeat. In all, this study sheds important light on the links between foreign birth and overeating/binge eating and, in doing so, covers new terrain for the healthy immigrant hypothesis.
Acknowledgments
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health (NIH) under Award Number K01AA026645. The research was also supported by the National Institute on Drug Abuse (NIDA) under Award Number R25 DA030310. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA, NIDA, or the NIH.
Footnotes
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- Ackard DM, Neumark-Sztainer D, Story M and Perry C, 2003. Overeating among adolescents: prevalence and associations with weight-related characteristics and psychological health. Pediatrics, 111(1), pp.67–74. [DOI] [PubMed] [Google Scholar]
- Alarcón RD, Parekh A, Wainberg ML, Duarte CS, Araya R and Oquendo MA, 2016. Hispanic immigrants in the USA: social and mental health perspectives. The Lancet Psychiatry, 3(9), pp.860–870. [DOI] [PubMed] [Google Scholar]
- Alegría M, Álvarez K and DiMarzio K, 2017. Immigration and Mental Health. Current epidemiology reports, 4(2), pp.145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen CN and Meng XL, 2008. Prevalence of mental illness in immigrant and non-immigrant US Latino groups. American Journal of Psychiatry, 165(3), pp.359–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Stinson FS and Grant BF, 2006. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of clinical psychiatry, 67(1), 56–65. [DOI] [PubMed] [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulvaney-Day N, Torres M and Canino G, 2007. Understanding differences in past year psychiatric disorders for Latinos living in the US. Social science & medicine, 65(2), pp.214–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Barry DT, Grilo CM and Masheb RM, 2002. Gender differences in patients with binge eating disorder. International Journal of Eating Disorders, 31(1), pp.63–70. [DOI] [PubMed] [Google Scholar]
- Bates LM, Acevedo-Garcia D, Alegría M and Krieger N, 2008. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. American journal of public health, 98(1), pp.70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaver KM, Wright JP, DeLisi M and Vaughn MG, 2008. Genetic influences on the stability of low self-control: Results from a longitudinal sample of twins. Journal of Criminal Justice, 36(6), pp.478–485.2 [Google Scholar]
- Breslau J, Borges G, Hagar Y, Tancredi D and Gilman S, 2009. Immigration to the USA and risk for mood and anxiety disorders: variation by origin and age at immigration. Psychological Medicine, 39(7), pp.1117–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA and Potenza MN, 2008. The neurobiology and genetics of impulse control disorders: relationships to drug addictions. Biochemical pharmacology, 75(1), pp.63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Vega WA, Sribney WM, Warner LA and Alegria M, 2008. Social relationships, social assimilation, and substance use disorders among adult Latinos in the US. Journal of Drug Issues, 38(1), pp.69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damas OM, Estes D, Avalos D, Quintero MA, Morillo D, Caraballo F, Lopez J, Deshpande AR, Kerman D, McCauley JL and Palacio A, 2018. Hispanics Coming to the US Adopt US Cultural Behaviors and Eat Less Healthy: Implications for Development of Inflammatory Bowel Disease. Digestive Diseases and Sciences, pp.1–9. [DOI] [PMC free article] [PubMed]
- Davis C, 2013. Compulsive overeating as an addictive behavior: overlap between food addiction and binge eating disorder. Current Obesity Reports, 2(2), pp.171–178. [Google Scholar]
- De Zwaan M, Mitchell JE, Seim HC, Specker SM, Pyle RL, Raymond NC and Crosby RB, 1994. Eating related and general psychopathology in obese females with binge eating disorder. International Journal of Eating Disorders, 15(1), pp.43–52. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, White MA, and Potenza NM, 2011. Binge eating disorder and food addiction. Current drug abuse reviews, 4(3), pp.201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Wall MM, Zhang J, Loth KA and Neumark-Sztainer D, 2016. Overeating and binge eating in emerging adulthood: 10-year stability and risk factors. Developmental psychology, 52(3), p.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Amsbary M, Chu A, Sigman R, Kali J, Sugawana Y, Jiao R, Goldstein RB, Jung J, Zhang H and Chou PS, 2014. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B and Hasin DS, 2015. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry, 72(8), pp.757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Shmulewitz D, Stohl M, Greenstein E, Aivadyan C, Morita K, Saha T, Aharonovich E, Jung J, Zhang H and Nunes EV, 2015. Procedural validity of the AUDADIS-5 depression, anxiety and post-traumatic stress disorder modules: substance abusers and others in the general population. Drug and alcohol dependence, 152, pp.246–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek HW, 2016. Review of the worldwide epidemiology of eating disorders. Current opinion in psychiatry, 29(6), pp.336–339. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr and Kessler RC, 2007. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological psychiatry, 61(3), pp.348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL and Williams JBW, 2001. Health problems, impairment and illnesses associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynaecology patients. Psychological medicine, 31(8), pp.1455–1466. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Newsom JT and McFarland BH, 2004. The association between length of residence and obesity among Hispanic immigrants. American journal of preventive medicine, 27(4), pp.323–326. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C and Bruffaerts R, 2013. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological psychiatry, 73(9), pp.904–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, 2017. Migration and psychosis: our smoking lung?. World Psychiatry, 16(2), pp.119–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavagnino L, Arnone D, Cao B, Soares JC and Selvaraj S, 2016. Inhibitory control in obesity and binge eating disorder: A systematic review and meta-analysis of neurocognitive and neuroimaging studies. Neuroscience & Biobehavioral Reviews, 68, pp.714–726. [DOI] [PubMed] [Google Scholar]
- López G and Bialik K, 2017. Key findings about US immigrants Pew Research Center, 3. [Google Scholar]
- Lorenzo-Blanco EI, Meca A, Unger JB, Romero A, Szapocznik J, Piña-Watson B, Cano MÁ, Zamboanga BL, Baezconde-Garbanati L, Des Rosiers SE and Soto DW, 2017. Longitudinal Effects of Latino Parent Cultural Stress, Depressive Symptoms, and Family Functioning on Youth Emotional Well-Being and Health Risk Behaviors. Family process, 56(4), pp.981–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makino M, Tsuboi K and Dennerstein L, 2004. Prevalence of eating disorders: a comparison of Western and non-Western countries. Medscape General Medicine, 6(3). [PMC free article] [PubMed] [Google Scholar]
- Marsiglia FF, Kulis S, Luengo MÁ, Nieri T and Villar P, 2008. Immigrant advantage? Substance use among Latin American immigrant and native-born youth in Spain. Ethnicity and Health, 13(2), pp.149–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustelin L, Bulik CM, Kaprio J and Keski-Rahkonen A, 2017. Prevalence and correlates of binge eating disorder related features in the community. Appetite, 109, pp.165–171. [DOI] [PubMed] [Google Scholar]
- Roshania R, Narayan KV and Oza- Frank R, 2008. Age at arrival and risk of obesity among US immigrants. Obesity, 16(12), pp.2669–2675. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, & Schwartz SJ, 2019. The study and prevention of alcohol and other drug misuse among migrants: Toward a transnational theory of cultural stress. International Journal of Mental Health and Addiction Advance online publication. doi: 10.1007/s11469-018-0023-5 [DOI]
- Salas-Wright CP and Vaughn MG, 2014. A “refugee paradox” for substance use disorders?. Drug and alcohol dependence, 142, pp.345–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Goings TC, Miller DP and Schwartz SJ, 2018. Immigrants and Mental Disorders in the United States: New Evidence on the Healthy Migrant Hypothesis. Psychiatry Research [DOI] [PMC free article] [PubMed]
- Salas-Wright CP, Kagotho N and Vaughn MG, 2014a. Mood, anxiety, and personality disorders among first and second-generation immigrants to the United States. Psychiatry research, 220(3), pp.1028–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Robles EH, Vaughn MG, Córdova D and Pérez-Figueroa RE, 2015. Toward a typology of acculturative stress: results among Hispanic immigrants in the United States. Hispanic Journal of Behavioral Sciences, 37(2), pp.223–242. [Google Scholar]
- Salas-Wright CP, Vaughn MG, Clark TT, Terzis LD and Córdova D, 2014b. Substance use disorders among first-and second-generation immigrant adults in the United States: evidence of an immigrant paradox?. Journal of studies on alcohol and drugs, 75(6), pp.958–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Goings TTC, Córdova D and Schwartz SJ, 2018. Substance use disorders among immigrants in the United States: A research update. Addictive behaviors, 76, pp.169–173.; [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Schwartz SJ and Córdova D, 2016. An “immigrant paradox” for adolescent externalizing behavior? Evidence from a national sample. Social psychiatry and psychiatric epidemiology, 51(1), pp.27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samnaliev M, Noh HL, Sonneville KR and Austin SB, 2015. The economic burden of eating disorders and related mental health comorbidities: An exploratory analysis using the US Medical Expenditures Panel Survey. Preventive medicine reports, 2, pp.32–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ and Unger J eds., 2017. The Oxford handbook of acculturation and health Oxford University Press. [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL and Szapocznik J, 2010. Rethinking the concept of acculturation: Implications for theory and research. American Psychologist, 65(4), p.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smink FR, Van Hoeken D and Hoek HW, 2012. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Current psychiatry reports, 14(4), pp.406–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel- Moore RH and Franko DL, 2003. Epidemiology of binge eating disorder. International Journal of Eating Disorders, 34(S1), pp.S19–S29 [DOI] [PubMed] [Google Scholar]
- Swanson SA, Saito N, Borges G, Benjet C, Aguilar-Gaxiola S, Medina-Mora ME and Breslau J, 2012. Change in binge eating and binge eating disorder associated with migration from Mexico to the US. Journal of psychiatric research, 46(1), pp.31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Walton E, Sue S and Alegría M, 2007. Immigration-related factors and mental disorders among Asian Americans. American Journal of Public Health, 97(1), pp.84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T and Grilo CM, 2018. Prevalence and Correlates of DSM-5–Defined Eating Disorders in a Nationally Representative Sample of US Adults. Biological Psychiatry, 84(5), pp. 345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, White MA, Lydecker JL, Barnes RD, Genao I, Garcia R, Masheb RM and Grilo CM, 2016. Biopsychosocial correlates of binge eating disorder in Caucasian and African American women with obesity in primary care settings. European Eating Disorders Review, 24(3), pp.181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M and Maynard BR, 2014. Violence and externalizing behavior among youth in the United States: Is there a severe 5%?. Youth Violence and Juvenile Justice, 12(1), pp.3–21. [Google Scholar]
- Vaughn MG, Salas-Wright CP, Maynard BR Qian Z, Terzis, L, Kusow K, and DeLisi M, 2014. Criminal epidemiology and the immigrant paradox: Intergenerational discontinuity in violence and antisocial behavior among immigrants. Journal of Criminal Justice, 42(6), pp. 483–490. [Google Scholar]
- Wilson AN, Salas-Wright CP, Vaughn MG and Maynard BR, 2015. Gambling prevalence rates among immigrants: a multigenerational examination. Addictive behaviors, 42, pp.79–85. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD and Engel SG, 2009. The validity and clinical utility of binge eating disorder. International Journal of Eating Disorders, 42(8), pp.687–705. [DOI] [PubMed] [Google Scholar]
- Zong J and Batalova J, 2015. Frequently requested statistics on immigrants and immigration in the United States. Migration Policy Institute, 26, pp.1–18. [Google Scholar]


