Abstract
Objectives: The objective of this study is to analyze the degree to which care needs are met in an aging rural African population. Method: Using data from the Health and Aging in Africa: Longitudinal Study of an INDEPTH Community (HAALSI) baseline survey, which interviewed 5,059 adults aged older than 40 years in rural South Africa, we assessed the levels of limitations in activities of daily living (ADLs) and in unmet care for these ADLs, and evaluated their association with sociodemographic and health characteristics. Results: ADL impairment was reported by 12.2% of respondents, with the proportion increasing with age. Among those with ADL impairment, 23.9% reported an unmet need and 51.4% more a partially met need. Relatives provided help most often; formal care provision was rare. Unmet needs were more frequent among younger people and women, and were associated with physical and cognitive deficits, but not income or household size. Discussion: Unmet care needs in rural South Africa are often found among individuals less expected to require care.
Keywords: disability, gender, comorbidities, socioeconomic status
Introduction
South Africa’s population is aging rapidly (Bor, Herbst, Newell, & Bärnighausen, 2013; United Nations, 2015). With a concomitant rise in noncommunicable disease rates, this is likely to lead to sharp increases in both physical and cognitive impairment. Both physical and cognitive impairment may lead to loss of ability to perform everyday activities independently, and thus result in a need for personal care from others. Activities that are essential for the maintenance of life are commonly referred to as basic activities of daily living (ADLs) and typically include the ability to feed, bathe, dress, toilet, walk, and transfer oneself (Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). If activity impairments are unable to be buffered by modifications to the environment, provision of mechanical assistance, or help from others, adverse consequences result—compromising both the ability to maintain life and participation in society (World Health Organization [WHO], 2016). Understanding the burden of ADL impairment and the extent to which care needs are met is critical in formulating a response to ensure that aging populations receive appropriate care and that the impact of ADL impairments can be successfully mitigated.
Compared with high-income countries (HICs), the volume of research on long-term care in low- and middle-income countries (LMICs) lags behind the potential need for such care (Lloyd-Sherlock, 2014). Less is known about the extent and nature of ADL impairment and disability of older people in rural sub-Saharan Africa in general, and in South Africa in particular (Payne, Gómez-Olivé, Kahn, & Berkman, 2017). Heterogeneity in how disability is defined and measured also makes cross-country comparisons difficult. Nevertheless, rates of ADL impairment and disability in sub-Saharan Africa appear to be high (Gómez-Olivé, Thorogood, Clark, Kahn, & Tollman, 2010; Nyirenda, Mutevedzi, Hosegood, Falkingham, & Newell, 2015; Payne, Mkandawire, & Kohler, 2013; Phaswana-Mafuya, Peltzer, Ramlagan, Chirinda, & Kose, 2013). The WHO/World Bank World Report on Disability estimated that severe disability (e.g., untreated AIDS, dementia, severe depression, blindness) in Africa is approximately twice as prevalent as in HICs, and higher than in other LMICs (WHO, 2011). The World Report also estimated that rates of moderate disability (e.g., due to angina, infertility, arthritis, tuberculosis) in African countries were higher than in HICs. This high prevalence of disability in Africa is likely to be driven in part by the complex mix of infectious disease, noncommunicable chronic disease, and injuries present on the continent (Murray et al., 2012), compounded by social factors that limit timely and appropriate care. The burden of disability in Africa falls most heavily on older people: compared with 15- to 49-year-olds, severe disability is estimated to be 5 times, and moderate disability 2.3 times, as prevalent among those aged ≥60 years (WHO, 2011).
An interrogation of the linkage between ADL impairments and the use of care services (either formal or informal) can be approached via integration of contextual and individual factors, broadly grouped into predisposing factors (e.g., demographic, societal factors, and beliefs), enabling factors (e.g., finances and care organizations or structures), and both the perceived and objectively evaluated need for care (Andersen, Davidson, & Baumeister, 2013). In many areas of sub-Saharan Africa, there is a substantial “care deficit”—state and private care provision are patchy or nonexistent, are often limited to urban centers, and even where such provision exists, it may be inaccessible for many due to poverty (Schatz & Seeley, 2015). Consequently, most care provision for older people in sub-Saharan Africa is provided by informal carers—the vast majority from within the family. Understanding the role of family composition and dynamics on the need for and delivery of care is a key challenge for aging research in sub-Saharan Africa, as has been discussed elsewhere (Aboderin & Hoffman, 2015). Changes in demographics, migration, and the impact of HIV have led to complex changes in family structures—a greater number of older family members, but a “hollowing out” of middle generations as a result of labor migration and HIV deaths (Kautz, Bendavid, Bhattacharya, & Miller, 2010; Schatz, Ralston, Madhavan, Collinson, & Gómez-Olivé, 2017; Schatz & Seeley, 2015). These patterns of care and need are further modified by the impact of gender—particularly with respect to the way that traditional societal roles place expectations on women as the main care providers in families, and also in how the loss of the male provider role as a result of ADL impairment might alter care-seeking or care-receipt behavior (Mugisha, Schatz, Seeley, & Kowal, 2015; Schatz et al., 2017). Further understanding the extent of ADL impairment, sources of care, the impact of financial flows through families (Lloyd-Sherlock & Agrawal, 2014), and whether care provided is sufficient to mitigate the impact of these impairments is important in constructing policy and services to enable healthy aging, both in South Africa and in other sub-Saharan African countries.
Given the limited evidence of the prevalence of ADL impairments and caregiver burden among older adults in LMICs (Maart & Jelsma, 2014), we aimed to describe the following: first, the extent and type of ADL impairment in an older rural South African population; second, the extent to which care needs around these ADL impairments are met; and third, factors associated with both ADL impairment and unmet needs. Given the results from previous work, we hypothesized that substantial levels of unmet need for ADLs would be present, and that this unmet need would be associated with low household income, social isolation, and comorbidities that increase the complexity of care needs.
Method
Population
The analysis we present below used data from the baseline round of Health and Aging in Africa: Longitudinal Study of an INDEPTH Community (HAALSI) in South Africa, conducted in 2014-2015. HAALSI is a survey of older people conducted within the rural Health and Demographic Surveillance Site (HDSS) of the MRC/Wits Rural Public Health and Health Transitions Research Unit (Agincourt) in Mpumalanga province, northeast South Africa (hereafter, Agincourt; Kahn et al., 2012). The Agincourt HDSS comprises 31 rural villages spread across 450 km2. Most households now have access to electricity, although cost constrains utilization. However, there are few tarred roads within villages, and very limited piped water access and sanitation. Limited formal services, including only two health centers and five clinics, are available in the area, with hospital access at least 25 km away.
HAALSI was established as a harmonized sister study to the Health and Retirement Study (HRS) and similar studies worldwide (Gómez-Olivé et al., 2018). HAALSI inclusion criteria were permanent residence in the Agincourt HDSS area during the 12 months prior to the 2013 HDSS census update round, and age 40 or above on July 1, 2014. A simple random sample of 6,281 eligible individuals was selected to be approached for the HAALSI baseline survey; gender-specific sampling fractions were used to ensure the sample was gender-representative of the study area. Of those invited, 5,059 agreed to participate (85% response rate). Ethics approval for HAALSI was obtained from the University of the Witwatersrand Human Research Ethics Committee (Reference No. M141159), the Harvard T.H. Chan School of Public Health Office of Human Research Administration (Reference No. 13-1608), and the Mpumalanga Provincial Research and Ethics Committee.
Outcome Variables
HAALSI asked about each of the six ADLs, that is, walking across a room (mobility), bathing or showering, getting dressed, eating, getting into or out of sleeping location (transfers), and using the toilet. For each ADL, participants were asked (a) whether they had no difficulty, had difficulty, or were unable to perform the ADL; (b) what aids (e.g., cane, walker, brace, railing, walls, wheelchair), if any, they used to assist with the ADL; and (c) whether they received help from another person (human assistance) to perform the ADL (full list of questions in Supplemental Material 1). Participants were defined as having an ADL impairment if they stated that they had difficulty or were unable to perform the ADL, or if they answered no to this question but yes to receiving help from others for performing the ADL. Finally, we generated a binary variable separating anyone defined as having one or more ADL impairments from those defined as having none.
We classified respondents into four categories of need for each ADL. Those who reported no difficulty with an ADL and no help received for that ADL were categorized as having “no need.” Those reporting no difficulty but who received help with an ADL were categorized as having “met needs.” Respondents reporting difficulty with an ADL and having received help or used an aid were categorized as having “partially met need.” Finally, those unable to perform the ADL, or those reporting difficulty with an ADL but who had no aids or help, were categorized as having “unmet need.” We then generated a binary variable separating anyone defined as having one or more entirely unmet needs from those defined as having all needs at least partially met.
Figure 1 shows the flowchart used to decide the above categorization for each ADL. HAALSI respondents were not asked directly whether they felt their needs were met; however, similar methods were used in previous analyses of unmet needs in HICs (Vlachantoni et al., 2011).
Figure 1.
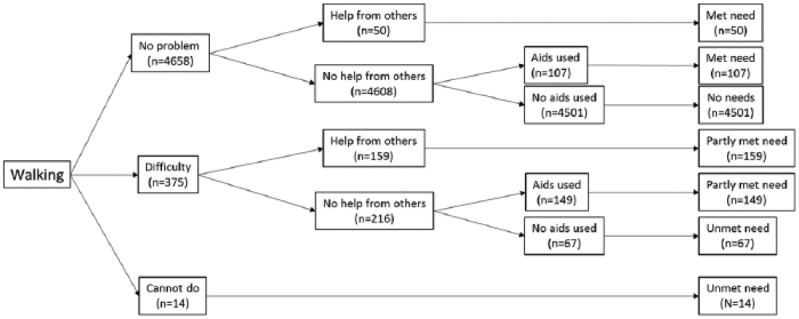
Classification of met need, partially met need, and unmet need, using walking activity of daily living as an example.
Independent Variables
We considered key sociodemographic and health variables likely to predict both ADLs and care provision. These included gender, age (categorized by decade as ages 40-49, 50-59, 60-69, 70-79 and 80+ years), educational level attained, and household size as sociodemographic factors. We dichotomized marital status into married/cohabiting versus not married or cohabiting to focus this measure on the physical presence of a spouse or partner as a potential source of care in the household. High household socioeconomic status might be expected to predict both likelihood of having an ADL and care provision—either by allowing the purchase of formal care, or by allowing other household members to take on caring roles rather than working in paid outside employment. We considered total household income (at purchasing power parity rates; Organisation for Economic Co-Operation and Development [OECD], 2017), consisting of labor and business income, including remittances from nonresident household members and government transfers (i.e., social grants). Income data were collated into four categories: no household income, monthly income between zero and below the level of the monthly old-age grant (R1,350 or US$245), income at or above the level of the old-age grant, and income at least 50% greater than the old-age grant. We preferred income to wealth, as income and wealth were highly collinear and income is more likely to represent resources available for everyday needs. We also preferred income over expenditure or consumption data, as in this nonsubsistence setting, income represents a stable flow of resources to the household.
Comorbid diseases are major primary drivers of impaired physical and cognitive performance, and consequently disability (Verbrugge & Jette, 1994). The presence of chronic disease would also be expected to drive health and care-seeking behavior, and potentially to flag to others that an individual is in some way ill or incapacitated, and requires care. Chronic conditions that we considered were biologically measured HIV status, diabetes mellitus, hypertension, anemia, and self-reported physician diagnosis of stroke, chronic bronchitis, or angina; we also administered the Rose Angina Questionnaire to capture current angina symptoms (Rose, Blackburn, Gillum, & Prineas, 1982).
In older populations in HICs impaired cognition, particularly dementia, is a key driver of ADL impairment and hence the need for long-term care (Holup, Hyer, Meng, & Volicer, 2017; Van Rensbergen & Nawrot, 2010). Cognition was assessed by three tests: orientation to the present, immediate word recall, and delayed word recall (Kobayashi et al., 2017). The former aims to capture severe cognitive impairment, the latter two short-term memory function (Weir, Lay, & Langa, 2014). A summary total cognition score was calculated, ranging from 0 to 24 points; those unable to complete the cognitive test were classified as a separate group.
Social contact might be expected to influence the relationship between impaired physical performance and disability (Mendes de Leon et al., 1999). Available social support was calculated from questions about self-reported levels of contact with up to seven important others in the past year. For each contact, participants reported frequency of contact and receipt of support. First, we calculated the number of person-days of in-person communication with others per month; second, we calculated the number of person-days of physical support received from others per month (Harling, Morris, Manderson, Perkins, & Berkman, 2018). For analysis, we divided participants into ordered quartiles, as our interest was in the broad association of relative levels of support with need and care, rather than believing that each person-day reported was likely to have the same meaning to participants.
A more detailed description of independent variable definitions and data collection methods is given in Supplemental Material 2.
Analysis
We first described all measures, including both need and care delivered, using means and standard deviations or medians and interquartile ranges for continuous data, and proportions for categorical data. We then conducted bivariate analyses of the relationship between any ADL impairment or unmet needs and demographic, health, and health care variables, using Pearson’s chi-square tests for categorical variables and one-way ANOVA for continuous variables. Finally, we conducted multivariable logistic regression using forced entry for all independent variables to determine which factors were independently associated with ADL impairment in all participants, and with any unmet need among those with at least one ADL impairment. All regression analyses including social contact data were adjusted for interviewer identity and month of interview, as these have previously been shown to strongly affect level of social contact reported in this sample (Harling, Perkins, et al., 2018). All analyses were conducted in SPSS v24 (IBM, New York, USA).
Results
Descriptive data on the 5,059 individuals who participated in the HAALSI baseline survey and are included in these analyses are given in Table 1.
Table 1.
Descriptive Statistics for the HAALSI Sample (N = 5,059).
| n | % or SD | |
|---|---|---|
| Female | 2,714 | 53.6 |
| Age | ||
| 40-49 | 918 | 18.1 |
| 50-59 | 1,410 | 27.9 |
| 60-69 | 1,304 | 25.8 |
| 70-79 | 878 | 17.4 |
| 80+ | 549 | 10.9 |
| Living arrangementsa | ||
| Living alone | 533 | 10.5 |
| Living with one other person | 538 | 10.6 |
| Living in 3-6 person household | 2,437 | 48.2 |
| Living in 7+ person household | 1,549 | 30.6 |
| Married or cohabitinga | 2,575 | 50.9 |
| Total monthly household income (US$)b | ||
| None | 490 | 9.7 |
| <245 | 791 | 15.6 |
| 245-362 | 1,128 | 22.3 |
| >362 | 2,650 | 52.4 |
| Level of educationa | ||
| None | 2,306 | 45.6 |
| Up to Grade 7 | 1,612 | 31.9 |
| Grade 8 to 11 | 540 | 10.7 |
| Matriculation (Grade 12) or above | 584 | 11.5 |
| HIV positive | 1,047 | 20.7 |
| Anemiaa | 1,875 | 41.7 |
| HAALSI diagnosis of | ||
| Hypertension | 3,145 | 62.2 |
| Diabetes mellitus | 559 | 11.0 |
| Previous diagnosis of | ||
| Angina | 456 | 9.0 |
| Stroke | 149 | 2.9 |
| Hypertension | 2,134 | 42.2 |
| Chronic bronchitis | 28 | 0.6 |
| Physical support quartiles (contacts per month) | ||
| 0 to 3 | 1,234 | 24.4 |
| 4 to 16 | 1,308 | 25.9 |
| 17 to 33 | 1,191 | 23.5 |
| 34 and above | 1,225 | 26.2 |
| Communications quartiles (contacts per month) | ||
| 0 to 28 | 1,159 | 22.9 |
| 29 to 39 | 1,263 | 25.0 |
| 40 to 63 | 1,354 | 26.8 |
| 64 and above | 1,283 | 25.4 |
| Cognition | ||
| Top four quintiles (≥8/24) | 3,991 | 78.9 |
| Lowest quintile (≤7/24) | 912 | 18.0 |
| Unable to complete test | 156 | 3.1 |
| Five meter walk speed (m/s) (M, SD) | ||
| Males | 0.65 | 0.33 |
| Females | 0.52 | 0.33 |
| Maximum grip strength (kg) (M, SD) | ||
| Males | 29.5 | 12.7 |
| Females | 22.0 | 9.5 |
| Body mass index (kg/m2) (M, SD) | ||
| Males | 24.9 | 5.5 |
| Females | 29.3 | 7.5 |
Note. HAALSI = Health and Aging in Africa: Longitudinal Study of an INDEPTH Community; m/s = meters per second; kg = kilogram.
Missingness for living arrangements (n = 2), marriage (n = 5), education (n = 17), anemia (n = 560), and body mass index (n = 370).
Household income converted from South Africa Rand to US$ at purchasing power parity.
ADL Impairments
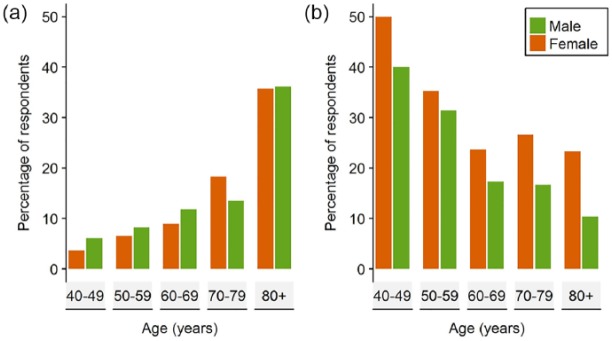
Some 615 people (12.2%) reported at least one ADL impairment, with mobility limitation the most frequent impairment (Table 2). One hundred and forty-five of those were aged below 60 years, representing 6.2% of all 40- to 59-year-olds; the same figures for those aged above 60 years were 470 and 17.2%. Two thirds (65%) of those with at least one ADL impairment reported two or more impairments. ADL impairments were more frequent with advancing age, particularly after age 80 years (Figure 2a), but with no observed difference in prevalence between men and women (x12 = 0.08, p = .77).
Table 2.
Number of ADL Impairments and Level of Unmet Need.
| ADL impairment |
Of which (%) |
||||
|---|---|---|---|---|---|
| n | % of all respondents | Met needa | Partially met needb | Unmet needc | |
| Any impairment | 615 | 12.2 | 24.7 | 51.4 | 23.9 |
| Walking | 546 | 10.8 | 28.8 | 56.4 | 14.8 |
| Eating | 65 | 1.3 | 0.0 | 56.9 | 43.1 |
| Bathing | 224 | 4.4 | 23.7 | 61.2 | 15.2 |
| Toileting | 345 | 6.8 | 41.2 | 51.3 | 7.5 |
| Bed transfer | 290 | 5.7 | 39.0 | 53.8 | 7.2 |
| Dressing | 203 | 4.0 | 25.1 | 57.1 | 17.7 |
| Impairment count | |||||
| 1 | 212 | 4.2 | 40.1 | 38.2 | 21.7 |
| 2 | 107 | 2.1 | 32.7 | 54.2 | 13.1 |
| 3 | 115 | 2.1 | 17.4 | 67.0 | 15.7 |
| 4 | 49 | 1.0 | 14.3 | 40.8 | 44.9 |
| 5 | 84 | 1.7 | 4.8 | 67.9 | 27.4 |
| 6 | 47 | 0.9 | 0.0 | 48.9 | 51.1 |
Note. ADL data missing for a small number of individuals: eating (n = 7), bathing/toileting/bed transfer (n = 10), walking (n = 11), and dressing (n = 18); 31 individuals had missing data for at least one ADL. Percentages are of those with nonmissing data. ADL = activity of daily living.
For “any impairment” and “impairment count,”
refers to all needs met,
to those with no unmet but ≥1 partially met need,
to ≥1 unmet need.
Figure 2.
ADL impairment and unmet need by age and sex: (a) Percentage of respondents (N = 5,059) with at least one ADL impairment and (b) percentage of those with any ADL impairment (n = 615) with unmet needs.
Note. ADL = activity of daily living.
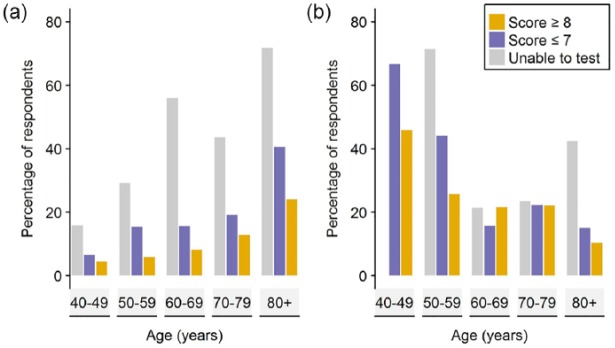
A range of health, social contact, and sociodemographic measures were associated with ADL impairment (Supplemental Table 1). Health factors associated with ADL impairment were hypertension, diabetes, stroke, HIV, anemia, physical performance, and cognitive impairment; sociodemographic and social contact factors included increasing age, lower income, household size, and physical contact. The relationship between cognition and ADL impairment was particularly striking: 23.2% of participants in the lowest cognitive quintile had at least one ADL impairment, compared with 8.3% of those in higher cognitive quintiles and 48.4% of those who were unable to complete the cognitive tests. Cognitive impairment was strongly linked to the presence of ADL impairment (Figure 3a). In multivariable regression (Table 3), ADL impairment was associated with increasing age and male sex, as well as worse physical performance measured by walk speed and grip strength, and several health conditions (diabetes, HIV, hypertension, stroke).
Figure 3.
ADL impairment and unmet need by age and cognition: (a) Percentage of respondents with any ADL impairment (n = 5,034) and (b) percentage of those with at least one ADL impairment with unmet needs (n = 615).
Note. ADL = activity of daily living.
Table 3.
Multivariable Regression Analyses of Factors Associated With ADL Impairment and Unmet Need in Those With ADL Impairment.
| ADL impairment | p value | At least one unmet need | p value | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Female vs. male | 0.57 | [0.44, 0.73] | <.001 | 1.53 | [0.87, 2.67] | .14 |
| Age | ||||||
| 40-49 | 1.00 | 1.00 | ||||
| 50-59 | 1.22 | [0.80, 1.85] | .36 | 0.46 | [0.17, 1.22] | .12 |
| 60-69 | 1.37 | [0.89, 2.11] | .16 | 0.23 | [0.08, 0.63] | .004 |
| 70-79 | 1.77 | [1.13, 2.79] | .01 | 0.26 | [0.09, 0.74] | .01 |
| 80+ | 3.74 | [2.34, 6.00] | <.001 | 0.12 | [0.04, 0.37] | <.001 |
| Physical performance | ||||||
| Grip strength (per kg) | 0.99 | [0.98, 1.00] | .03 | 0.99 | [0.96, 1.01] | .22 |
| Walk speed (per m/s) | 0.02 | [0.01, 0.04] | <.001 | 0.54 | [0.20, 1.44] | .22 |
| Comorbid conditions | ||||||
| HIV positive | 1.56 | [1.16, 2.09] | .003 | 0.99 | [0.50, 1.97] | .99 |
| Hypertensiona | 1.36 | [1.07, 1.72] | .01 | 0.88 | [0.53, 1.45] | .61 |
| Diabetes mellitus | 1.64 | [1.22, 2.19] | .001 | 0.90 | [0.46, 1.74] | .75 |
| Angina | 1.10 | [0.77, 1.57] | .61 | 0.64 | [0.25, 1.62] | .34 |
| Bronchitis | 1.88 | [0.55, 6.37] | .31 | 1.74 | [0.08, 38.74] | .73 |
| Anemia | 0.97 | [0.78, 1.20] | .78 | 1.09 | [0.68, 1.75] | .73 |
| Stroke | 4.95 | [3.17, 7.72] | <.001 | 1.50 | [0.73, 3.10] | .28 |
| Lowest quintile of cognition vs. all others | 1.35 | [1.04, 1.76] | .03 | 0.99 | [0.56, 1.76] | .98 |
| Unable to complete cognitive test | 3.40 | [2.05, 5.62] | <.001 | 2.28 | [0.85, 6.08] | .10 |
| Household income <US$245/monthb | 0.79 | [0.59, 1.05] | .11 | 1.19 | [0.64, 2.20] | .59 |
| Living arrangements | ||||||
| Living alone | 1.00 | 1.00 | ||||
| Living with one other person | 1.27 | [0.83, 1.93] | .27 | 1.03 | [0.39, 2.72] | .96 |
| Living in 3-6 person household | 1.14 | [0.80, 1.62] | .46 | 1.06 | [0.49, 2.29] | .89 |
| Living in 7+ person household | 0.99 | [0.68, 1.45] | .96 | 0.97 | [0.41, 2.32] | .94 |
| Married or cohabiting | 0.67 | [0.52, 0.88] | .003 | 0.91 | [0.51, 1.66] | .77 |
| Level of education | ||||||
| None | 1.00 | 1.00 | ||||
| Up to Grade 7 | 0.83 | [0.64, 1.08] | .16 | 0.76 | [0.42, 1.38] | .37 |
| Grade 8 to 11 | 0.97 | [0.63, 1.50] | .89 | 0.39 | [0.13, 1.20] | .10 |
| Matriculation (Grade 12) or above | 0.84 | [0.53, 1.34] | .46 | 0.65 | [0.22, 1.94] | .44 |
| Physical support quartiles | ||||||
| Lowest | 1.00 | 1.00 | ||||
| Second most | 0.99 | [0.70, 1.38] | .93 | 1.75 | [0.78, 3.92] | .18 |
| Third most | 1.29 | [0.88, 1.87] | .19 | 1.67 | [0.69, 4.04] | .25 |
| Highest | 1.42 | [0.93, 2.17] | .10 | 1.90 | [0.73, 4.95] | .19 |
| In-person communication quartile | ||||||
| Lowest | 1.00 | 1.00 | ||||
| Second most | 1.11 | [0.78, 1.57] | .56 | 0.98 | [0.43, 2.26] | .97 |
| Third most | 1.35 | [0.94, 1.94] | .11 | 0.78 | [0.33, 1.86] | .58 |
| Highest | 1.40 | [0.93, 2.08] | .10 | 1.03 | [0.42, 2.56] | .95 |
| Sample size | 5,009 | 604 | ||||
Note. All models also adjusted for month of interview and identity of interviewer. ADL = activity of daily living; OR = odds ratio; CI = confidence interval; m/s = meters per second; kg = kilogram; HAALSI = Health and Aging in Africa: Longitudinal Study of an INDEPTH Community.
For ADL impairment, regression includes diagnosis from HAALSI-measured blood pressure; for unmet need, regression only includes known to patient.
Income >US$245/month as referent.
Met and Unmet Need for Care Around ADL Impairments
Of the 615 individuals with at least one ADL impairment, 147 (23.9%) had at least one ADL impairment for which they had an unmet need (Table 2 and Supplemental Table 2). A further 316 (51.4%) had at least one partially met need. Having multiple ADL impairments was associated with a higher chance of having at least one unmet need, and a conversely lower chance of having all needs met. As a check that our categorization was describing functionally distinct groups, we calculated median walk speeds for each category of met and unmet need associated with walking difficulty. Results of this analysis are shown in Supplemental Table 3. The results show that those with met need (including those reporting “no difficulty” but getting help), partially met, and unmet need had lower walk speeds than those with no needs, suggesting that those with “met need” were a distinct group from those with “no needs” and that the difference in classification was not due to differences in how respondents interpreted the questions.
The most frequent source of help was from respondents’ spouse and relatives (Table 4). However, over a third of respondents with an ADL impairment reported receiving no human assistance. The difference between this figure and the 23.9% of respondents with unmet need, described above, is accounted for by those individuals who used aids, but not human assistance, to partially meet their needs. Of those with ADL impairment who were married or cohabiting, 78/234 (33.3%) reported receiving no human assistance, compared with 143/381 (37.3%) of those who were not married or cohabiting (p = .32). Physical help from sources external to the family (e.g., government, private, or charity-sector care) was rare; less than 10% of those with ADL impairment or met need reported such help. Respondents noting no source of help were more likely to have unmet needs or partially met needs; those receiving help from a nonspousal relative were more likely to have partially met needs or unmet needs than to have all their needs met.
Table 4.
Receipt of Care and Social Contact in the HAALSI Sample.
| No needs |
ADL impairment or met need |
All needs met |
No unmet but ≥1 partially met need |
≥1 unmet need |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | p valuea | n | % | p valuea | |
| 4,419 | 615 | 152 | 316 | 147 | ||||||||
| Care provided by | ||||||||||||
| No source disclosed | 3,062 | 81.5 | 220 | 35.8 | 79 | 52.0 | 96 | 30.4 | <.001 | 45 | 30.6 | <.001 |
| Paid helper | 35 | 0.8 | 27 | 4.4 | 9 | 5.9 | 15 | 4.7 | .59 | 3 | 2.0 | .14 |
| Volunteer/facility employee | 14 | 0.3 | 7 | 1.1 | 0 | 0.0 | 3 | 0.9 | .55 | 4 | 2.7 | .06 |
| Spouse | 386 | 8.7 | 138 | 22.4 | 25 | 16.4 | 84 | 26.6 | .02 | 29 | 19.7 | .46 |
| Other relative | 592 | 13.4 | 272 | 44.2 | 43 | 28.3 | 148 | 46.8 | <.001 | 81 | 55.1 | <.001 |
| Other | 18 | 0.4 | 26 | 4.2 | 7 | 4.6 | 16 | 5.1 | .83 | 3 | 2.0 | .34 |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||||||||
| Person-contacts/month | ||||||||||||
| Communication with others | 40 | (30, 64) | 38 | (16, 63) | 40 | (23, 61) | 39 | (15, 64) | .79 | 34 | (10, 64) | .59 |
| In-person physical support | 16 | (4, 34) | 18 | (2, 40) | 14 | (2, 33) | 17 | (2, 40) | .26 | 30 | (3, 44) | .06 |
Note. Sample size for this table is all those with no missing ADLs data. Percentages may sum to >100%, as individuals may receive help from multiple categories of others. All comparisons are to the “All met needs category.” HAALSI = Health and Aging in Africa: Longitudinal Study of an INDEPTH Community; ADL = activity of daily living; IQR = interquartile range.
p values are for Mann–Whitney tests (continuous variables) and Pearson χ2 tests (categorical variables) unless cell size <5, in which case Fisher’s exact test.
Despite having fewer ADL impairments, unmet need was more likely to be present in younger people, and in women at any given age (Figure 2b). In contrast to ADL impairment, no consistent pattern was seen between the proportion of unmet need and cognitive status at a given age (Figure 3b). In multivariable regression analysis, unmet need among the subgroup with ADL impairment was significantly associated with younger age and being female. It was also associated with weaker grip strength, inability to complete cognitive tests, and greater receipt of physical support (Table 3).
Discussion
Our analysis found that more than 10% of this older rural South African population were living with ADL impairment, with higher rates accompanying advancing age, cognitive impairment, physical weakness, and chronic disease presence including stroke, hypertension, diabetes mellitus, and HIV. In our sample, 6.3% of 40- to 59-year-olds had an ADL impairment, of whom 36.6% had an unmet need and 45.5% a partially met need. For those aged above 60 years, 20.9% had an ADL impairment, of whom 20.0% had an unmet need and 53.2% a partially met need.
Our results are congruent with other studies, which have found advancing age, female sex, and stroke to be associated with greater disability (GBD 2015 DALYs and HALE Collaborators, 2016; Santosa, Schröders, Vaezghasemi, & Ng, 2016). Most care that was provided came from spouses or other family members, with very little formal care provided by public, private, or third sector providers.
Few other studies have addressed the issue of unmet need for care in LMICs, and most have examined perceived rather than evaluated unmet need. Results from India suggest rates of unmet need of approximately a third of those aged 60 years and above in a rural setting (Singh, Bairwa, Goel, Bypareddy, & Mithra, 2016), although this analysis included unmet need for instrumental as well as basic ADLs. In China, rates of 50% to 65% were reported from a study of those aged 80 years and above in rural and urban settings (Zhu, 2015); this analysis combined partially met need with unmet need however, and variations in definitions are likely to have led to this high figure. The prevalence of unmet need for basic ADLs in our analysis is similar to that found in samples from Medicare and Medicaid recipients in the United States (Allen, Piette, & Mor, 2014), from the National Health Interview Survey in the United States (Desai, Lentzner, & Weeks, 2001), and from older people in Canada (Dubuc, Dubois, Raîche, & Hébert, 2011). However, it is lower than that found in some U.K. surveys (Vlachantoni et al., 2011), despite the widespread availability of formal social services support in the United Kingdom. In considering cross-country comparisons, especially of self-reported care, the thresholds for reporting either absolute, or unmet, need for care need to be considered. Schneider’s (2009, 2016) cognitive interview work on disability data collection methods clearly illustrates how questions are differently understood and responded to across settings.
A number of factors were independently associated with the presence of at least one ADL impairment, including older age, having sustained a stroke, and the presence of HIV, hypertension, or diabetes mellitus. Being married or cohabiting was associated with a lower risk of ADL impairment. Other factors that associated as expected with ADL impairment were cognitive impairment, low grip strength, and low walk speed; these factors can be either associated due to a common shared antecedent (e.g., a stroke) and also lie on the causal pathway to disability as part of the construct of frailty (Clegg, Young, Iliffe, & Rikkert, 2013). Cardiometabolic disease is now prevalent in sub-Saharan Africa, including in rural South Africa (Gaziano et al., 2017), and these findings suggest that control of cardiometabolic risk factors, as well as HIV, might provide an avenue to reduce the future burden of ADL impairment in this population.
Several factors were associated with unmet care need. First, women were significantly more likely to have unmet needs than men in bivariate analysis, although the strength of this association was weakened after adjustment for other factors such as marital status. This may in part be due to more men than women living with, and receiving care from, spouses. Women have longer life expectancy and, in this setting, are on average several years younger than their spouses. As a result, by age 80 years, less than 10% of women in this sample were living with a spouse, compared with more than 60% of men, and marital status has been shown to be highly predictive of social support (Harling, Morris, et al., 2018). Some, but not all, studies from HICs have found a similar higher prevalence of unmet need among women (Casado, van Vulpen, & Davis, 2011; Dubuc et al., 2011; Zhu, 2015). Future examination of the roles of spouses, as well as adult children—particularly those living in the same household—might help us better understand the contexts in which unmet needs arise.
Second, counterintuitively, those below 60 years of age living with ADLs had a higher rate of unmet need than those above 60 years. One explanation is that younger people may not fit the stereotype of requiring care, and thus may not be offered care in the way that older people would be. Another explanation might be that caregivers for these middle-aged individuals might themselves be older (e.g., their parents), and thus less able to provide all the care that these younger individuals require. Alternatively, younger people may be more reluctant to ask for or receive care due to being less willing to accept they cannot achieve basic tasks, or their basic ADL limitations may have been transient in nature. Both of these factors may be exacerbated by HIV, which is most prevalent among younger HAALSI members (Rosenberg et al., 2017), if those living with the infection avoid admitting such care needs because of stigma associated with HIV. Future work within the HAALSI cohort may shed light on this finding.
Third, cognitive impairment (either low score on cognitive tests or inability to complete the tests) was associated with unmet need in bivariate analysis, although again this relationship was weakened after adjustment for other factors. These associations may reflect the substantial care burden imposed by low cognitive capacity. Finally, those with unmet need reported higher levels of physical support that those with met needs. One explanation for this association is that physical support was a response to their greater needs; the fact that unmet needs remained suggests that the physical assistance provided was insufficient to meet care needs. This finding highlights not only an area for future, in-depth enquiry, but potentially also an opportunity for interventions to facilitate those within social networks to better meet the care needs of individuals.
Some factors we expected to predict unmet care need proved not to do so, notably income, household size, and chronic disease diagnoses. In the context of an underresourced public health and social care system, limited disposable income might be expected to make formal care access difficult or impossible (Goudge, Gilson, Russell, Gumede, & Mills, 2009; van der Hoeven, Kruger, & Greeff, 2012), particularly for chronic care (Wagner et al., 2011). However, there appeared to be almost no formal care in the study area on which to spend money, which may explain why household income did not predict unmet need: Even those with substantial resources cannot purchase formal assistance that does not exist. Alternatively, individuals with ADL impairment may lack the capacity to use money in a way that would either directly meet their care needs, or to free other family members from work or household duties to provide them with care. Money flowing into families (e.g., from the old-age grant) may be spent on other priorities within the family; unemployment rates for working-aged individuals in the study area are above 50% and thus younger dependents may need financial support. Previous work has shown that, parallel to our findings, the old-age grant in South Africa has a limited impact on health, although the old-age grant was associated with greater health service use but not with better health outcomes (Lloyd-Sherlock & Agrawal, 2014); these analyses also suggested no relationship between the old-age grant and either physical function or quality of life.
Household size was not significantly associated with unmet need, nor was marital status. In rural South Africa, traditional extended family structures might be assumed to exist, reducing the need for formal care, and providing a robust system for delivering informal care. However, the loss of young- and middle-aged adults to HIV-related mortality (Bor et al., 2013; Schatz, Madhavan, & Williams, 2011), migration for work (Camlin, Snow, & Hosegood, 2013; Collinson, Tollman, & Kahn, 2007), and consequent changes in household composition and dependency ratios (Schatz, Madhavan, Collinson, Gómez-Olivé, & Ralston, 2015) may all reduce the ability of families to meet the needs of older people with disabilities. In addition, larger households may include a greater number of dependents, as each household is built around a core of working age adults; in this case, those able to provide care may be thinly spread. Furthermore, we cannot assume that families are structured so that household members are available and willing to provide care (Manderson & Block, 2016); the structure of households can be complex and this complexity is not adequately captured by simple counts of household members (Schatz et al., 2017). These factors may explain why we did not find household size to be associated with unmet needs, although this null finding also highlights the need for in-depth investigation of household dynamics in the context of caregiving in rural South Africa.
Although chronic health diagnoses and comorbid conditions were associated with increased rates of ADL impairment, unmet need was largely not associated with these underlying conditions. These null associations may reflect either truly no association between health diagnoses and unmet care need, or two offsetting effects: a greater need and a greater level of support. Specifically, coming into contact with health care services, either to be diagnosed or due to an acute health event, might flag a need for care to family and friends, allowing ADL impairments to be addressed. Another possible reason for the observed null association might be survivor bias: Those with the most severe chronic conditions may die sooner, so those left are likely to have fewest unmet needs and are thus on average as likely to have unmet needs as those not living with chronic illness.
Strengths and Limitations
Our analysis has a number of strengths. The study sample was large, covered a wide age range, and focused on a rural South African population with levels of noncommunicable disease morbidity risk factors that reflect the transformation in disease patterns now starting to affect many sub-Saharan African countries, particularly those with a high prevalence of HIV infection. The many independent variables collected, including disease-based, social, economic, and demographic variables, allowed us to examine a broad range of potential associations between activity impairment, unmet need, and baseline factors.
Among the limitations, we were not able to assess instrumental ADLs—the additional activities that allow for independent living, including housekeeping, shopping, food preparation, managing money and medications, using the telephone, and dealing with transportation (Lawton & Brody, 1969). Our estimate for the prevalence of both activity impairment and unmet need is therefore almost certainly an underestimate, as instrumental ADL impairment typically precedes basic ADL impairment and is more frequent. Studies for HICs suggest that unmet need for instrumental ADL impairment is even greater than for basic ADL impairment (Allen et al., 2014).
Second, HAALSI did not ask participants directly whether their care needs were met. Although this limits comparison with other surveys, our methodology for deriving unmet need has been used previously in other large population-based cohorts (Desai et al., 2001; Xu, Covinsky, Stallard, Thomas, & Sands, 2012) and is consistent with Andersen et al.’s (2013) conception of objectively evaluated need. The questions that were available for use from the HAALSI survey are open to differences in interpretation by participants, but the fact that responses were associated with different levels of physical performance suggests that our definitions of unmet need had some degree of validity.
Of all the definitions we were able to derive using HAALSI data, that of partially met need is most difficult to interpret. Partially met need encompasses a wide spectrum of situations, ranging from those with almost all needs met to those for whom only a small fraction of needs are met. Our definition does not allow us to distinguish where an individual lies on this spectrum. Our definition conceptualizes unmet need as a mismatch between the impairments reported by participants and the help that they report getting; this is not necessarily the same as an individual would report as unmet need were they to be asked directly (i.e., perceived need in Andersen et al.’s, 2013, framework). Future studies could usefully compare these different ways of assessing unmet need to facilitate cross-study comparisons. Our choice of method to dichotomize unmet need was a conservative one; by choosing entirely unmet needs rather than partially met needs, we aimed to avoid the issues of variability in the degree to which a need was met as discussed above. A loss of even a single activity so critical to survival as a basic ADL is of great importance to an individual, and our choice of dichotomization at a single unmet need also facilitates comparison with previous studies.
Third, these baseline HAALSI data do not allow us to ascertain the timing of impairment onset, or the extent to which the impairments interfered with work, family, and wider community roles. Subsequent longitudinal follow-up of the HAALSI cohort may allow such questions to be answered. Fourth, ascertainment of some independent variables could be considered suboptimal. For example, cognitive testing was necessarily brief and focused on simple tasks, and thus low cognitive scores or inability to complete the tests may reflect nonneurodegenerative issues including deafness, dysphasia, physical ill health, learning difficulties, or depression. Most variables collected in HAALSI (in common with most large cohorts) are based on self-report, with consequent possibilities for selective reporting by respondents and recall bias. As discussed above, a simple count of household members does not fully capture the complexity of household structures, and future analyses could usefully examine this issue in more depth. Fifth, as with any cross-sectional analysis, it is not possible to ascertain temporal ordering between baseline factors and either ADL impairment or unmet need. Sixth, while efforts were made to ensure that all parts of the local population were represented in HAALSI, and the study response rate was more than 85%, the proportions of men and women, and younger and older individuals, do not necessarily represent those of all household members in the local area.
Finally, the HAALSI data are drawn from the specific geographic location of Agincourt in rural Mpumalanga, South Africa. The generalizability of our various findings will depend on the extent to which health burdens, social dynamics, and formal care support structures differ elsewhere. It seems likely that our findings of greater unmet need among younger and female adults living with ADLs, and of kin provision of caregiving, will extend to much of rural South Africa. However, this initial quantitative foray into care need and provision in Africa needs to be followed up elsewhere to test such hypotheses.
Conclusion
Our analysis represents the start of a process to better describe, understand, and ameliorate unmet need for care, both in our geographical area of study and in other sub-Saharan African populations. Future studies might benefit from asking direct questions regarding whether care needs are met, and additionally examining instrumental ADLs. Such studies are needed in a range of populations in different countries. There is, however, a limit to what large-scale quantitative data can tell us about either the lived experience of disability and need in old age, or about the nature of interpersonal interactions that might drive the observed findings. These questions will need ethnographic approaches to complement the survey data collected.
A better understanding of the scale, nature, consequences, and drivers of unmet need can potentially provide a platform for designing interventions to reduce unmet need in resource-poor health and long-term care systems. Such interventions are likely to include ensuring that formal long-term care support systems are both effective and efficient, and also ensuring that communities are supported to deliver informal care effectively by removing social and economic barriers to such delivery.
Supplemental Material
Supplemental material, HAALSI_unmet_needs_-_R1_-_18Oct2018_-_SM_clean for Impairment in Activities of Daily Living, Care Receipt, and Unmet Needs in a Middle-Aged and Older Rural South African Population: Findings From the HAALSI Study by Guy Harling, Collin F. Payne, Justine I. Davies, F. Xavier Gomez-Olive, Kathleen Kahn, Lenore Manderson, Farrah J. Mateen, Stephen M. Tollman and Miles D. Witham in Journal of Aging and Health
Acknowledgments
The authors would like to thank the HAALSI study team, participants, and the Agincourt community.
Footnotes
Author Contributions: M.D.W. conceptualized and led the analyses and wrote the first draft of the article in collaboration with G.H. G.H., F.H.M., C.F.P., J.I.D., and L.M. helped to shape the analysis design and contributed to analysis and interpretation of the results. F.X.G.O., K.K., and S.T. were involved in all phases of design and data collection for Health and Aging in Africa: Longitudinal Study of an INDEPTH Community (HAALSI). All authors contributed to interpretation and critical revision of the text.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Aging at the National Institutes of Health (P01 AG041710), and is nested within the MRC/Wits Rural Public Health & Health Transitions Research Unit (Agincourt), supported by The Wellcome Trust (Grants 058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z; 085477/B/08/Z), the University of the Witwatersrand, and the South African Medical Research Council.
ORCID iD: Guy Harling  https://orcid.org/0000-0001-6604-491X
https://orcid.org/0000-0001-6604-491X
Supplemental Material: Supplemental material for this article is available online.
References
- Aboderin I., Hoffman J. (2015). Families, intergenerational bonds and aging in sub-Saharan Africa. Canadian Journal on Aging, 34, 282-289. doi: 10.1017/S0714980815000239 [DOI] [PubMed] [Google Scholar]
- Allen S. M., Piette E. R., Mor V. (2014). The adverse consequences of unmet need among older persons living in the community: Dual-eligible versus Medicare-only beneficiaries. The Journals of Gerontology: Series B, 69(Suppl. 1), S51-S58. doi: 10.1093/geronb/gbu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R. M., Davidson P. L., Baumeister S. E. (2013). Improving access to care. In Kominski G. F. (Ed.), Changing the US healthcare system: Key issues in health services policy and management (4th ed.) (pp. 33-70). Hoboken, NJ: Wiley. [Google Scholar]
- Bor J., Herbst A. J., Newell M.-L., Bärnighausen T. (2013). Increases in adult life expectancy in rural South Africa: Valuing the scale-up of HIV treatment. Science, 339, 961-965. doi: 10.1126/science.1230413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camlin C. S., Snow R. C., Hosegood V. (2013). Gendered patterns of migration in rural South Africa. Population, Space and Place, 20, 528-551. doi: 10.1002/psp.1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casado B. L., van Vulpen K. S., Davis S. L. (2011). Unmet needs for home and community-based services among frail older Americans and their caregivers. Journal of Aging and Health, 23, 529-553. doi: 10.1177/0898264310387132 [DOI] [PubMed] [Google Scholar]
- Clegg A., Young J., Iliffe S., Rikkert M. O., Rockwood K. (2013). Frailty in elderly people. The Lancet, 381, 752-762. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinson M. A., Tollman S. M., Kahn K. (2007). Migration, settlement change and health in post-apartheid South Africa: Triangulating health and demographic surveillance with national census data. Scandinavian Journal of Public Health, 35, 77-84. doi: 10.1080/14034950701356401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai M. M., Lentzner H. R., Weeks J. D. (2001). Unmet need for personal assistance with activities of daily living among older adults. The Gerontologist, 41, 82-88. doi: 10.1093/geront/41.1.82 [DOI] [PubMed] [Google Scholar]
- Dubuc N., Dubois M.-F., Raîche M., Hébert R. (2011). Meeting the home-care needs of disabled older persons living in the community: Does integrated services delivery make a difference? BMC Geriatrics, 11(1), Article 67. doi: 10.1186/1471-2318-11-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaziano T. A., Abrahams-Gessel S., Gomez-Olive F. X., Wade A., Crowther N. J., Alam S., . . . Rohr J. (2017). Cardiometabolic risk in a population of older adults with multiple co-morbidities in rural South Africa: The HAALSI (Health and Aging in Africa: Longitudinal Studies of INDEPTH Communities) study. BMC Public Health, 17(1), Article 206. doi: 10.1186/s12889-017-4117-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 DALYs and HALE Collaborators. (2016). Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: A systematic analysis for the global burden of disease study 2015. The Lancet, 388, 1603-1658. doi: 10.1016/s0140-6736(16)31460-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Olivé F. X., Montana L., Wagner R. G., Kabudula C. W., Rohr J. K., Kahn K., . . . Gaziano T. (2018). Cohort profile: Health and Ageing in Africa: A Longitudinal Study of an INDEPTH Community in South Africa (HAALSI). International Journal of Epidemiology, 47, 689-690j. doi: 10.1093/ije/dyx247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Olivé F. X., Thorogood M., Clark B., Kahn K., Tollman S. (2010). Assessing health and well-being among older people in rural South Africa. Global Health Action, 3(Suppl. 2), 23-35. doi: 10.3402/gha.v3i0.2126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudge J., Gilson L., Russell S., Gumede T., Mills A. (2009). The household costs of health care in rural South Africa with free public primary care and hospital exemptions for the poor. Tropical Medicine and International Health, 14, 458-467. [DOI] [PubMed] [Google Scholar]
- Harling G., Morris K. A., Manderson L., Perkins J. M., Berkman L. (2018). Age and gender differences in social network composition and social support among older rural South Africans: Findings from the HAALSI study. The Journals of Gerontology: Series B. Advance online publication. doi: 10.1093/geronb/gby013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harling G., Perkins J. M., Gómez-Olivé F. X., Morris K. A., Wagner R. G., Montana L., . . . Berkman L. F. (2018). Interviewer-driven variability in social network reporting: Results from Health and Aging in Africa: A Longitudinal Study of an INDEPTH community (HAALSI) in South Africa. Field Methods, 30, 140-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holup A. A., Hyer K., Meng H., Volicer L. (2017). Profile of nursing home residents admitted directly from home. Journal of the American Medical Directors Association, 18, 131-137. doi: 10.1016/j.jamda.2016.08.017 [DOI] [Google Scholar]
- Kahn K., Collinson M. A., Gómez-Olivé F. X., Mokoena O., Twine R., Mee P., . . .Khosa A. (2012). Profile: Agincourt health and socio-demographic surveillance system. International Journal of Epidemiology, 41, 988-1001. doi: 10.1093/ije/dys115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S., Ford A. B., Moskowitz R. W., Jackson B. A., Jaffe M. W. (1963). Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association, 185, 914-919. doi: 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kautz T., Bendavid E., Bhattacharya J., Miller G. (2010). AIDS and declining support for dependent elderly people in Africa: Retrospective analysis using demographic and health surveys. British Medical Journal, 340, Article c2841. doi: 10.1136/bmj.c2841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi L. C., Glymour M. M., Kahn K., Payne C. F., Wagner R. G., Montana L., . . . Berkman L. F. (2017). Childhood deprivation and later-life cognitive function in a population-based study of older rural South Africans. Social Science & Medicine, 190, 20-28. doi: 10.1016/j.socscimed.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton M., Brody E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9, 179-186. doi: 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- Lloyd-Sherlock P. (2014). Beyond neglect: Long-term care research in low and middle income countries. International Journal of Gerontology, 8, 66-89. [Google Scholar]
- Lloyd-Sherlock P., Agrawal S. (2014). Pensions and the health of older people in South Africa: Is there an effect? Journal of Development Studies, 50, 1570-1586. doi: 10.1080/00220388.2014.936399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maart S., Jelsma J. (2014). Disability and access to health care—A community based descriptive study. Disability and Rehabilitation, 36, 1489-1493. [DOI] [PubMed] [Google Scholar]
- Manderson L., Block E. (2016). Relatedness and care in Southern Africa and beyond. Social Dynamics, 42, 205-217. doi: 10.1080/02533952.2016.1218139 [DOI] [Google Scholar]
- Mendes de, Leon C. F., Glass T. A., Beckett L. A., Seeman T. E., Evans D. A., Berkman L. F. (1999). Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. The Journals of Gerontology: Series B, 54, S162-S172. doi: 10.1093/geronb/54B.3.S162 [DOI] [PubMed] [Google Scholar]
- Mugisha J. O., Schatz E., Seeley J., Kowal P. (2015). Gender perspectives in care provision and care receipt in people infected and affected by HIV in Uganda. African Journal of AIDS Research, 14, 159-167. [DOI] [PubMed] [Google Scholar]
- Murray C. J., Vos T., Lozano R., Naghavi M., Flaxman A. D., Michaud C., . . . Lopez A. D. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. The Lancet, 380, 2197-2223. [DOI] [PubMed] [Google Scholar]
- Nyirenda M. M. E., Mutevedzi P., Hosegood V., Falkingham J., Newell M.-L. (2015). Who cares? Implications of care-giving and -receiving by HIV-infected or -affected older people on functional disability and emotional wellbeing. Ageing and Society, 35, 169-202. doi: 10.1017/S0144686X13000615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organisation for Economic Co-Operation and Development. (2017). Purchasing Power Parities (PPP) (Indicator, Publication No. 10.1787/1290ee5a-en). Paris, France: OECD. [Google Scholar]
- Payne C. F., Gómez-Olivé F. X., Kahn K., Berkman L. (2017). Physical function in an aging population in rural South Africa: Findings from HAALSI and cross-national comparisons with HRS sister studies. The Journals of Gerontology: Series B, 72, 665-679. doi: 10.1093/geronb/gbx030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne C. F., Mkandawire J., Kohler H.-P. (2013). Disability transitions and health expectancies among adults 45 years and older in Malawi: A cohort-based model. PLoS Medicine, 10, e1001435. doi: 10.1371/journal.pmed.1001435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phaswana-Mafuya N., Peltzer K., Ramlagan S., Chirinda W., Kose Z. (2013). Social and health determinants of gender differences in disability amongst older adults in South Africa. Health SA Gesondheid, 18, 1-9. doi: 10.4102/hsag.v18i1.728 [DOI] [Google Scholar]
- Rose G. A., Blackburn H., Gillum R., Prineas R. (1982). Cardiovascular survey methods (Vol. 56). Geneva, Switzerland: World Health Organization. [Google Scholar]
- Rosenberg M. S., Gómez-Olivé F. X., Rohr J. K., Houle B. C., Kabudula C. W., Wagner R. G., . . . Tollman S. M. (2017). Sexual behaviors and HIV status: A population-based study among older adults in rural South Africa. Journal of Acquired Immune Deficiency Syndromes (1999), 74(1), e9-e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santosa A., Schröders J., Vaezghasemi M., Ng N. (2016). Inequality in disability-free life expectancies among older men and women in six countries with developing economies. Journal of Epidemiology and Community Health, 70, 855-861. doi: 10.1136/jech-2015-206640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Madhavan S., Collinson M., Gómez-Olivé F. X., Ralston M. (2015). Dependent or productive? A new approach to understanding the social positioning of older South Africans through living arrangements. Research on Aging, 37, 581-605. doi: 10.1177/0164027514545976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Madhavan S., Williams J. (2011). Female-headed households contending with AIDS-related hardship in rural South Africa. Health & Place, 17, 598-605. doi: 10.1016/j.healthplace.2010.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Ralston M., Madhavan S., Collinson M. A., Gómez-Olivé F. X. (2017). Living arrangements, disability and gender of older adults among rural South Africa. The Journals of Gerontology: Series B, 73, 1112-1122. doi: 10.1093/geronb/gbx081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Seeley J. (2015). Gender, ageing and carework in East and Southern Africa: A review. Global Public Health, 10, 1185-1200. doi: 10.1080/17441692.2015.1035664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M. (2009). The difference a word makes: Responding to questions on “disability” and “difficulty” in South Africa. Disability and Rehabilitation, 31, 42-50. doi: 10.1080/09638280802280338 [DOI] [PubMed] [Google Scholar]
- Schneider M. (2016). Cross-national issues in disability data collection. In Altman B. M. (Ed.), International measurement of disability (pp. 15-28). Basel, Switzerland: Springer. [Google Scholar]
- Singh A., Bairwa M., Goel S., Bypareddy R., Mithra P. (2016). Prevalence and predictors of unmet needs among the elderly residents of the rural field practice area of a tertiary care centre from Northern India. The Malaysian Journal of Medical Sciences, 23, 44-50. doi: 10.21315/mjms2016.23.5.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. (2015). World population prospects: The 2015 revision. New York, USA: United Nations. [Google Scholar]
- van der Hoeven M., Kruger A., Greeff M. (2012). Differences in health care seeking behaviour between rural and urban communities in South Africa. International Journal for Equity in Health, 11, 31. doi: 10.1186/1475-9276-11-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Rensbergen G., Nawrot T. (2010). Medical conditions of nursing home admissions. BMC Geriatrics, 10(1), Article 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge L. M., Jette A. M. (1994). The disablement process. Social Science & Medicine, 38(1), 1-14. doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Vlachantoni A., Shaw R., Willis R., Evandrou M., Falkingham J., Luff R. (2011). Measuring unmet need for social care amongst older people. Population Trends, 145, 60-76. doi: 10.1057/pt.2011.17 [DOI] [PubMed] [Google Scholar]
- Wagner A. K., Graves A. J., Reiss S. K., LeCates R., Zhang F., Ross-Degnan D. (2011). Access to care and medicines, burden of health care expenditures, and risk protection: Results from the World Health Survey. Health Policy, 100, 151-158. doi: 10.1016/j.healthpol.2010.08.004 [DOI] [PubMed] [Google Scholar]
- Weir D., Lay M., Langa K. (2014). Economic development and gender inequality in cognition: A comparison of China and India, and of SAGE and the HRS sister studies. The Journal of the Economics of Ageing, 4, 114-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2011). World report on disability. Geneva, Switzerland: Author. [Google Scholar]
- World Health Organization. (2016). International classification of functioning, disability and health. Retrieved from http://www.who.int/classifications/icf/en/
- Xu H., Covinsky K. E., Stallard E., Thomas J., Sands L. P. (2012). Insufficient help for activity of daily living disabilities and risk of all-cause hospitalization. Journal of the American Geriatrics Society, 60, 927-933. doi: 10.1111/j.1532-5415.2012.03926.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H. (2015). Unmet needs in long-term care and their associated factors among the oldest old in China. BMC Geriatrics, 15, Article 46. doi: 10.1186/s12877-015-0045-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, HAALSI_unmet_needs_-_R1_-_18Oct2018_-_SM_clean for Impairment in Activities of Daily Living, Care Receipt, and Unmet Needs in a Middle-Aged and Older Rural South African Population: Findings From the HAALSI Study by Guy Harling, Collin F. Payne, Justine I. Davies, F. Xavier Gomez-Olive, Kathleen Kahn, Lenore Manderson, Farrah J. Mateen, Stephen M. Tollman and Miles D. Witham in Journal of Aging and Health