Tick-borne encephalitis virus (TBEV) is a pathogen that causes severe human neuroinfections in Europe and Asia and for which there is currently no specific therapy. We have previously found that galidesivir (BCX4430), a broad-spectrum RNA virus inhibitor, which is under clinical development for treatment of Ebola and yellow fever virus infections, has a strong antiviral effect against TBEV. For any antiviral drug, it is important to generate drug-resistant mutants to understand how the drug works. Here, we produced TBEV mutants resistant to galidesivir and found that the resistance is caused by a single amino acid substitution in an active site of the viral RNA-dependent RNA polymerase, an enzyme which is crucial for replication of the viral RNA genome. Although this substitution led only to a subtle decrease in viral fitness in cell culture, galidesivir-resistant TBEV was highly attenuated in a mouse model. Our results contribute to understanding the molecular basis of galidesivir antiviral activity.
KEYWORDS: BCX4430, galidesivir, attenuation, drug resistance, mutation, tick-borne encephalitis virus
ABSTRACT
The adenosine analogue galidesivir (BCX4430), a broad-spectrum RNA virus inhibitor, has entered a phase 1 clinical safety and pharmacokinetics study in healthy subjects and is under clinical development for treatment of Ebola and yellow fever virus infections. Moreover, galidesivir also inhibits the reproduction of tick-borne encephalitis virus (TBEV) and numerous other medically important flaviviruses. Until now, studies of this antiviral agent have not yielded resistant viruses. Here, we demonstrate that an E460D substitution in the active site of TBEV RNA-dependent RNA polymerase (RdRp) confers resistance to galidesivir in cell culture. Galidesivir-resistant TBEV exhibited no cross-resistance to structurally different antiviral nucleoside analogues, such as 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, and 4′-azido-aracytidine. Although the E460D substitution led to only a subtle decrease in viral fitness in cell culture, galidesivir-resistant TBEV was highly attenuated in vivo, with a 100% survival rate and no clinical signs observed in infected mice. Furthermore, no virus was detected in the sera, spleen, or brain of mice inoculated with the galidesivir-resistant TBEV. Our results contribute to understanding the molecular basis of galidesivir antiviral activity, flavivirus resistance to nucleoside inhibitors, and the potential contribution of viral RdRp to flavivirus neurovirulence.
IMPORTANCE Tick-borne encephalitis virus (TBEV) is a pathogen that causes severe human neuroinfections in Europe and Asia and for which there is currently no specific therapy. We have previously found that galidesivir (BCX4430), a broad-spectrum RNA virus inhibitor, which is under clinical development for treatment of Ebola and yellow fever virus infections, has a strong antiviral effect against TBEV. For any antiviral drug, it is important to generate drug-resistant mutants to understand how the drug works. Here, we produced TBEV mutants resistant to galidesivir and found that the resistance is caused by a single amino acid substitution in an active site of the viral RNA-dependent RNA polymerase, an enzyme which is crucial for replication of the viral RNA genome. Although this substitution led only to a subtle decrease in viral fitness in cell culture, galidesivir-resistant TBEV was highly attenuated in a mouse model. Our results contribute to understanding the molecular basis of galidesivir antiviral activity.
INTRODUCTION
Flaviviruses (family Flaviviridae, genus Flavivirus) cause widespread human morbidity and mortality throughout the world. These viruses are typically transmitted to humans by mosquito or tick vectors. Tick-borne encephalitis virus (TBEV) is a typical flavivirus transmitted by Ixodes spp. ticks. TBEV is a causative agent of tick-borne encephalitis (TBE), a severe and potentially lethal neuroinfection in humans (1). The disease is prevalent in the sylvatic areas of Europe and Asia, with more than 13,000 cases of TBE being reported annually (2, 3). The clinical presentation of TBE ranges from mild fever to severe encephalitis or encephalomyelitis. In many cases, survivors of TBE suffer long-term or even permanent debilitating sequelae (4). As for other flaviviral infections, there is no specific treatment for TBE other than supportive therapy. Thus, the search for antiviral agents for specific chemotherapy of TBE and related viruses is urgent.
Among the different strategies aimed at inhibiting virus or cell components involved in TBEV replication, the viral nonstructural NS5 protein, an RNA-dependent RNA polymerase (RdRp), has become an attractive target for specific and effective inhibition of viral replication, with limited measurable effect on the host cells (5). Several molecules, mainly nucleoside analogues, were found to be potent inhibitors of the TBEV NS5 polymerase activity (6–9). The mechanism of action of these nucleoside analogues is based on their initial metabolization to the active triphosphate (nucleotide) form by cellular kinases and subsequent incorporation into the nascent genome by the RdRp, leading to premature chain termination (5). Galidesivir (also known as BCX4430 or Immucillin-A, Fig. 1A) is an adenosine analogue with two structural modifications: (i) it is a C-nucleoside characterized by a C-glycosidic bond instead of the usual N-glycosidic bond, and (ii) the furanose oxygen has been replaced by an imino group (10). Galidesivir is known to have a broad-spectrum antiviral effect against more than 20 different medically important RNA viruses across nine different virus families (flaviviruses, togaviruses, bunyaviruses, arenaviruses, paramyxoviruses, coronaviruses, filoviruses, orthomyxoviruses, and picornaviruses) (10–15). Low micromolar levels of galidesivir were previously shown to inhibit TBEV with no or negligible cytopathic effect (CPE) on the host cells (7). A phase 1 clinical safety and pharmacokinetics study in healthy subjects has been completed, and at present, galidesivir is under clinical development as an antiviral drug for treatment of Ebola virus infection (14), as well as for the treatment of yellow fever (https://clinicaltrials.gov/ct2/show/NCT03891420). Its broad-spectrum antiviral activity makes this drug a promising candidate for development of therapy not only for Ebola or yellow fever viruses infection but also other important diseases caused by various RNA viruses, including TBEV.
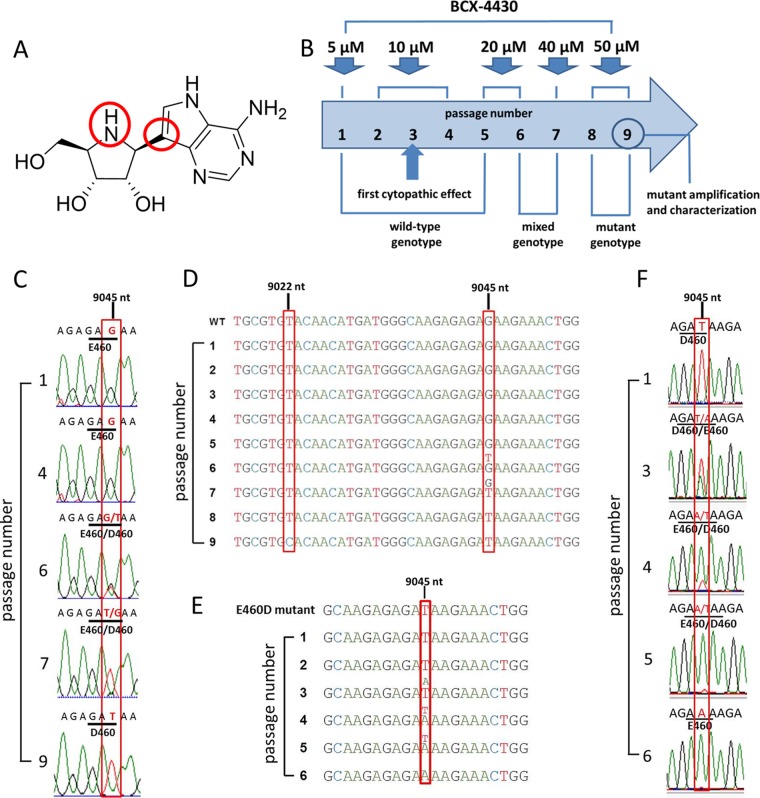
FIG 1.
TBEV resistance to galidesivir is associated with a single mutation in the NS5 gene. (A) The structure of the nucleoside analogue galidesivir. (B) Scheme of the selection process for generation of TBEV resistance to galidesivir. TBEV was serially passaged in PS cells in the presence of increasing galidesivir concentrations. (C) Whole-genome sequence analysis of the passaged viruses revealed a mutation at the amino acid position 460 in the NS5 protein, changing the glutamic acid residue to aspartic acid. (D) In the E460D/Y453H mutant, both amino acid changes E460D (nucleotide position G9045T) and Y453H (nucleotide position T9022C) were detected in the NS5 protein after 5 and 8 passages in the presence of galidesivir, respectively. (E) Rapid reinduction of the wild-type genotype in PS cells after serial passage of TBEV in PS cells in the absence of galidesivir. (F) During serial passage of the in vitro-selected E460D mutant virus in PS cells in the absence of galidesivir, the amino acid codon GAT (in the mutant) was changed to the codon GAA (in the revertant).
Although galidesivir has been studied intensively and is known to inhibit a wide range of RNA viruses, there are no published reports of resistance to this compound. Experience with the treatment of other RNA virus infections shows that resistance can develop rapidly with any of the direct-acting antiviral agents (16–18). Due to the low fidelity of viral RdRps in general, the mutation frequency is estimated to be 10−4 to 10−6 errors per nucleotide (19). The high mutation frequency and high replication rate of viral RNA copies enable the viruses quickly to adapt to changes in the environment, including the introduction of antiviral drugs. Identification of mutations conferring antiviral resistance provides information not only about the risk of generation of drug-resistant mutants but also helps to elucidate molecular mechanisms of the antiviral action. This is an integral and essential part of development and testing of any new antiviral drug (17).
In the present study, we identified and described a specific amino acid substitution in the TBEV NS5 polymerase that confers resistance to galidesivir. This substitution had only a limited effect on viral reproduction in vitro but had a cost on viral fitness when tested in vivo using mice. Our findings are important for understanding the mechanism of action of galidesivir and for the use of this molecule as an antiviral drug against TBEV and other emerging RNA viruses. In addition, we highlight the discovery of a potential contribution of viral RdRp to flavivirus neurovirulence.
(This article was submitted to an online preprint archive [20].)
RESULTS
TBEV resistant to galidesivir has two amino acid substitutions in the NS5 protein.
Studies of drug-resistant virus mutants are crucial for understanding molecular interactions of antiviral drugs with target viral proteins, as well as for development of efficient and specific antiviral therapies. In order to select TBEV resistant to galidesivir, the virus was serially passaged in porcine kidney stable (PS) cell monolayers in the presence of increasing concentrations of galidesivir up to 50 μM (Fig. 1B); this process resulted in selection of two independent drug-resistant TBEV mutant strains. Whole-genome sequencing of the passaged viruses revealed that both selected TBEV mutants carried a single amino acid change E460D, which corresponds to the nucleotide substitution G9045T in the NS5 gene (Fig. 1C and D). Sequencing of viruses after each passage showed that this mutation was acquired after 5 passages. In passages 6 and 7, mixed mutated and wild-type genotypes were detected; from passage 8 onward, the mutated genotype dominated until the end of the experiment (passage 9) (Fig. 1D). Interestingly, in one of the selected TBEV mutants, an additional amino acid change Y453H was detected; this mutation, which was acquired after eight passages, corresponds to the nucleotide substitution T9022C in the NS5 gene (Fig. 1D). Mutations E460D and Y453H were not present in the wild-type virus passaged in the absence of the selection agents. Both mutations mapped to the active site of the RdRp domain of the NS5 protein. The in vitro-selected TBEV mutants (denoted as E460D and E460D/Y453H) were further evaluated for their sensitivity/resistance to galidesivir at concentrations ranging from 0 to 50 μM and compared to the mock-selected wild-type virus (Fig. 2A). Whereas in vitro replication of wild-type was completely inhibited by galidesivir at a concentration of 12.5 μM (50% effective concentration [EC50] of 0.95 ± 0.04 μM), both mutants were approximately 7-fold less sensitive to the compound, showing EC50 values of 6.66 ± 0.04 and 7.20 ± 0.09 μM, respectively, for E460D and E460D/Y453H (Fig. 2A, Table 1).
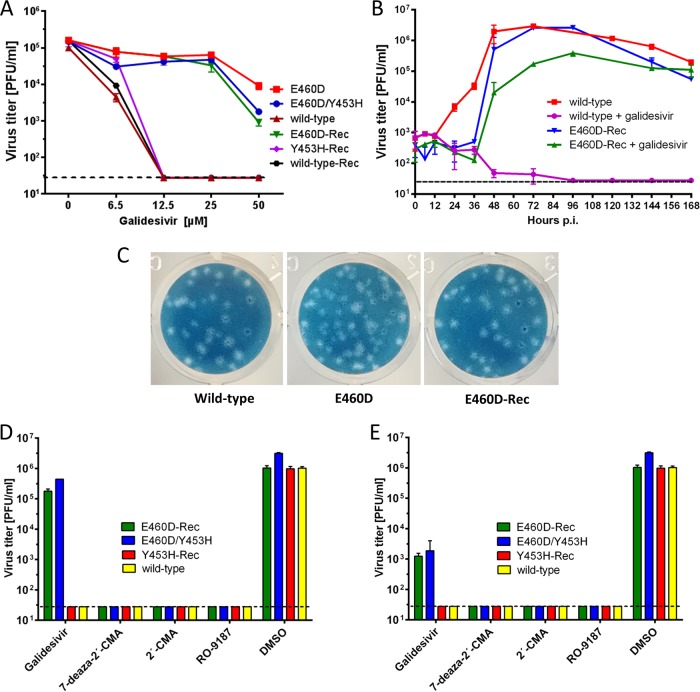
FIG 2.
Phenotypic properties of TBEV mutant resistant to galidesivir in vitro. (A) Dose-response curves for TBEV mutants E460D, E460D/E453H, E460D-Rec, Y453H-Rec, and corresponding wild types grown in PS cells in the presence of galidesivir at the indicated compound concentrations. Only TBEVs bearing the E460D mutation (i.e., E460D, E460D/E453H, and E460D-Rec) were resistant to galidesivir, indicating that this mutation is responsible for the resistance phenotype. (B) Growth kinetics of the E460D-Rec mutant and wild-type TBEV in the presence (25 μM) or absence (0 μM) of galidesivir within the 7-day experimental period to assess the replication efficacy of the mutant TBEV in PS cells. (C) Plaque morphology of the E460D and E460D-Rec mutants was assessed in PS cell monolayers and compared to the wild-type virus. (D and E) The sensitivity/resistance profiles of the E460D/Y453H, E460D-Rec, and Y453H-Rec to diverse nucleoside inhibitors (concentrations of 25 μM [D] and 50 μM [E]) were evaluated in PS cells and compared to the corresponding wild-type TBEV. The mean titers from two independent experiments, each performed in triplicate, are shown, and error bars indicate the standard errors of the mean. The horizontal dashed line indicates the minimum detectable threshold of 1.44 log10 PFU/ml.
TABLE 1.
Inhibitory properties of galidesivir for the obtained TBEVs
| Method used to generate wild-type/mutated virus | Virus | EC50 (μM)a |
|---|---|---|
| In vitro selection (passaging in PS cells) | E460D | 6.66 ± 0.04 (7.01) |
| E460D/Y453H | 7.20 ± 0.09 (7.57) | |
| Wild type | 0.95 ± 0.04 | |
| Reverse genetics | E460D-Rec | 6.32 ± 1.01 (7.90) |
| Y453H-Rec | 0.81 ± 0.01 (1.01) | |
| E460D/Y453H-Rec | Not rescued | |
| Wild-type-Rec | 0.80 ± 0.01 |
Determined from three independent experiments. Values are expressed as a 50% reduction in viral titer and were calculated according to the Reed-Muench method. PS cells were infected with the virus (MOI of 0.1) and cultivated at galidesivir concentrations ranging from 0 to 50 μM for 3 days. The fold increase compared to the wild-type value is indicated in parentheses.
Site-directed mutagenesis confirms that E460D determines TBEV drug resistance.
In order to demonstrate the direct effect of the amino acid substitutions E460D and Y453H on TBEV phenotype, the appropriate mutations were introduced into recombinant TBEV strains generated by the rapid reverse-genetics approach based on the use of subgenomic overlapping DNA fragments (21, 22). The entire TBEV strain Hypr genome flanked at the 5′ and 3′ untranslated regions by the pCMV and HDR/SV40pA was de novo synthesized in three double-stranded DNA fragments of approximately 4.4, 4.5, and 3.1 kb in length, overlapping by 80 to 120 pb. The substitutions E460D (G9045T) and Y453H (T9022C) were introduced into the NS5 gene located on fragment III using mutagenic PCR primers (Table 2). After transfection of the subgenomic fragments into permissive BHK-21 cells, the following recombinant TBEV strains were successfully rescued: E460D-Rec (E460D substitution in the NS5 gene), Y453H-Rec (Y453H substitution in the NS5 gene), and recombinant wild type (no introduced mutations). The presence of the E460D and Y453H substitutions in the viral genomes was confirmed by whole-genome sequencing of all recombinant viruses. Despite repeated attempts, the E460D/Y453H-Rec mutant (both mutations E460D and Y453H in the NS5 gene) was not rescued from the transfected BHK-21 cell culture. E460D-Rec was found to be 7.9-fold less sensitive to galidesivir than the engineered wild type, showing an EC50 value of 6.32 ± 1.01 μM (Table 1). On the other hand, Y453H-Rec was highly sensitive to galidesivir; the replication of this mutant strain was completely inhibited at 12.5 μM, showing an EC50 value of 0.81 ± 0.01 μM (Table 1). Thus, the results indicate that the E460D (not Y453H) substitution is solely responsible for the drug-resistant phenotype of TBEV (Fig. 2A).
TABLE 2.
Unmodified and mutated primers used to generate two overlapping amplicons of fragment III (fragment IIIa and IIIb), i.e., to produce recombinant wild-type and mutated viruses
| Primer type | Fragment III position | Forward or reverse | Generation of wild-type/mutated virus | Primer sequencea |
|---|---|---|---|---|
| Primers to amplify fragment IIIa | 14–36 | Forward | ATACACCATTGGTGGAAGAGGGC | |
| 975–1034 | Reverse | Wild-type-Rec | CTTTCTCTCTCTTCATCCACGAGGTGCCAGAATGCAGGATCCTCTACAGCCTCTCTTGC | |
| 1070–1097 | Reverse | E460D-Rec | CAGTTTCTTATCTCTCTTGCCCATCATG | |
| 1059–1090 | Reverse | Y453H-Rec | TCTCTCTCTTGCCCATCATGTTGTGCACGCA | |
| 1048–1096 | Reverse | E460D/Y453H-Rec | AGTTTCTTATCTCTCTTGCCCATCATGTTGTGCACGCAGTGCGCGCATC | |
| Primers to amplify fragment IIIb | 1009–1072 | Forward | Wild-type-Rec | ACCTCGTGGATGAAGAGAGAGAAAGGCACCTCATGGGGAGATGCGCGCACTGCGTGTAC |
| 1079–1100 | Forward | E460D-Rec | CAAGAGAGATAAGAAACTGGGA | |
| 1049–1074 | Forward | Y453H-Rec | ATGCGCGCACTGCGTGCACAACATGA | |
| 1059–1107 | Forward | E460D/Y453H-Rec | TGCGTGCACAACATGATGGGCAAGAGAGATAAGAAACTGGGAGAGTTCG | |
| 3050–3071 | Reverse | CTCAGGGTCAATGCCAGCGCTT |
The T9022C and G9045T mutations and their complementary counterparts are indicated in boldface.
The E460D mutation decreases TBEV replication fitness in cell culture during the first 36 h postinfection.
To characterize the phenotypic properties of the drug-resistant mutant in vitro, the growth kinetics (Fig. 2B) and plaque morphology (Fig. 2C) of the recombinant TBEV mutant E460D-Rec were assayed in cultures of PS cells and compared to the wild-type virus. The wild-type virus amplified in the absence of galidesivir (Fig. 2B, red line) showed a short lag period within the interval from 0 to 12 h postinfection (p.i.). Starting 24 h p.i., the wild-type TBEV exerted an exponential increase in virus infectivity, reaching a peak titer of 3 × 106 PFU/ml within 72 h p.i. and gradually declining thereafter. In contrast, the presence of galidesivir (25 μM) completely inhibited replication of the wild-type virus (Fig. 2B, violet line).
In comparison to the wild-type virus, the E460D-Rec mutant cultured in the absence of galidesivir (Fig. 2B, blue line) showed a prolonged lag-period within the interval from 0 to 36 h p.i. However, subsequently, the infectivity of the mutant virus increased exponentially, reaching a peak of 2.6 × 106 PFU/ml at 72 h p.i. After that, the titer gradually declined to 5.5 × 104 PFU/ml. The considerably longer lag period of the E460D-Rec mutant could be explained by a slightly decreased replication capacity (attenuation) of the mutant when amplified in PS cell culture. The decrease in replication capacity of E460D-Rec was manifested particularly in the first few hours after cell culture infection and was no longer detectable in the later stages of the infection.
The E460D-Rec mutant cultured in the presence of galidesivir (25 μM) (Fig. 2B, green line) also exerted an extended lag period within the interval from 0 to 36 h p.i.; there was even a moderate decrease in viral titers after 36 h p.i. Beginning at 48 h p.i., the mutant showed an exponential infectivity and reached a peak titer of 3.9 × 105 PFU/ml at day 96 h p.i. The results clearly indicate that the resistance of TBEV to galidesivir is only partial; the growth of the mutant strain in the presence of galidesivir was partially inhibited compared to the wild type (Fig. 2B, red line) or the E460D-Rec mutant grown in the absence of galidesivir (Fig. 2B, blue line).
The plaque morphology of the drug-resistant TBEV mutant was similar to that of wild-type virus; both viruses produced large and clear plaques which were round and regular in shape and did not change in shape and size during all the consecutive passages (Fig. 2C). The similarity in plaque morphology of drug-resistant and wild-type TBEVs is in agreement with similar growth kinetics of both viruses and supports our assumption that the mutation E460D affects the viral replication in PS cell culture only to a limited extent.
The E460D TBEV mutant is sensitive to 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine and 4′-azido-aracytidine.
To test whether or not E460D and Y453H substitutions affect sensitivity of TBEV to structurally different nucleoside inhibitors, we evaluated selected nucleoside analogues with previously reported anti-TBEV activity (6) for their capacity to inhibit the in vitro replication of galidesivir-resistant TBEV. Inhibitory effects of 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, and 4′-azido-aracytidine (RO-9187) at concentrations of 25 and 50 μM were not affected in the E460D/Y453H mutant, which was obtained by serial subculture in PS cells in the presence of galidesivir (Fig. 2D and E). The same drug sensitivity profile, characterized by complete inhibition of virus replication, was determined for two recombinant TBEVs generated by reverse genetics: E460D-Rec and Y453H-Rec. Wild-type virus was used as a positive control in this in vitro antiviral study (Fig. 2D and E). The EC50 values of 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, and 4′-azido-aracytidine for the galidesivir-resistant mutant were analogous to those for the wild-type virus (not shown) and corresponded to the values reported previously (6).
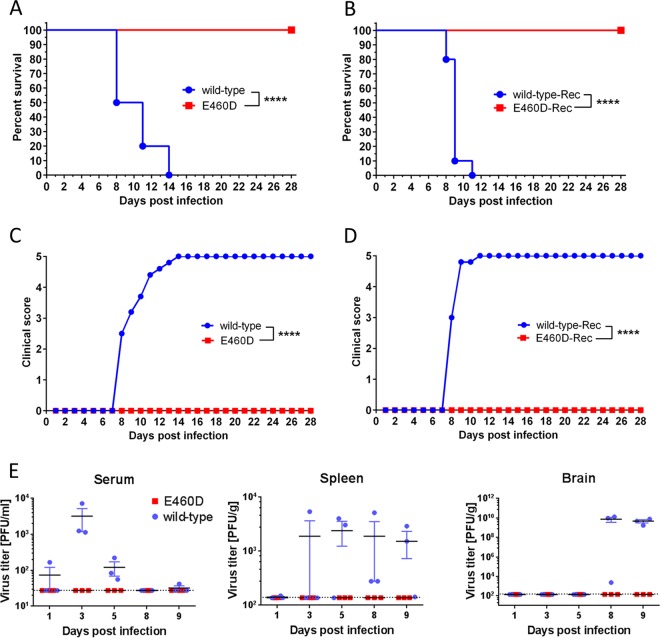
Mouse neuroinvasiveness of the E460D TBEV mutant is highly attenuated.
The degree of neuroinvasiveness of the E460D TBEV mutant was assessed in BALB/c mice and was compared to that of the wild-type virus. Adult BALB/c mice were infected subcutaneously (s.c.) with 103 PFU of either virus and survival rates, and clinical signs of neuroinfection were monitored for 28 days. Wild-type virus produced fatal infections in all mice, with mean survival times of 11 ± 2.2 days; infected mice showed severe signs of disease, such as ruffled fur, hunched posture, tremor, and hind leg paralysis (Fig. 3A and C). In contrast, all mice infected with the drug-resistant TBEV mutant E460D (obtained by serial in vitro subculture in the presence of galidesivir) survived (P < 0.0001), displaying no clinical signs of TBEV infection through the entire 28-day experimental period (Fig. 3A and C). The same survival data (100% survival rate, P < 0.0001) and clinical scores (no signs of neuroinfection) were obtained when recombinant TBEV mutant (E460D-Rec) was used for mouse infection using the same infectious dose and administration route (Fig. 3B and D).
FIG 3.
Phenotypic properties of the TBEV mutant resistant to galidesivir in mice. The extent of neuroinvasiveness of the E460D and E460D-Rec TBEV mutants was investigated in BALB/c mice and compared to that of the wild-type virus. Adult BALB/c mice were infected s.c. with 103 PFU of either virus, and survival (A and B) and clinical scores of the neuroinfection (C and D) were monitored for 28 days. ****, P < 0.0001. (E) Viral titers in blood sera, brains, and spleens of wild-type or E460D-infected BALB/c mice (infectious dose of 103 PFU) were determined by plaque assay at days 1, 3, 5, 8, and 9 p.i. The titers for three mice per interval are shown, and bars indicate means ± the standard errors of the mean. The dotted lines indicate detection limits.
Mouse serum, spleen, and brain samples were harvested for titration at various time points after s.c. inoculation of the galidesivir-resistant and wild-type TBEV. At early stages of the infection (day 1 p.i.), the wild-type virus showed a slight viremia in one of the three animals tested (102 PFU/ml). The wild-type virus caused a peak viremia on day 3 p.i. (approximately 2 × 103 PFU/ml); the viral titers in sera gradually decreased to the detection limit of plaque assay by day 9 p.i. No wild-type virus was detected in brains collected on days 1, 3, and 5 p.i.; however, the virus was detected in brains on days 8 and 9 p.i. at high titers reaching up to 1010 PFU/g. In spleens, the wild-type TBEV was first detected on day 3 p.i. and was present at a constant level (viral titers around 2 × 103 PFU/g) until the end of the experiment (Fig. 3E). In contrast, the E460D TBEV mutant was not detected neither in any serum, spleen, or brain samples collected during the whole experimental period (Fig. 3E).
Rapid reinduction of wild-type genotype in the absence of galidesivir.
In general, mutant genotypes rapidly revert to the wild type in the absence of the selection agents. Indeed, after three passages in PS cells in the absence of galidesivir, a pool comprising mutated and wild-type genotypes was detected. Moreover, from passage 5 onward the wild-type genotype dominated in the infected PS cell culture (Fig. 1E). Interestingly, the codon GAT encoding an aspartic acid in the E460D mutant had changed to the codon GAA in the revertant, not to GAG as seen in mock-selected wild-type virus; both codons, GAA (in the revertant) and GAG (in the wild type), are synonymous and encode a glutamic acid residue (Fig. 1F). In contrast, after six passages in the presence of galidesivir at concentrations up to 25 μM, the E460D substitution was retained, even at low concentrations of galidesivir (6.25 μM), and did not result in reversion to the wild-type genotype (data not shown).
DISCUSSION
Galidesivir is an adenosine analogue originally developed for filovirus infection treatment (Ebola and Marburg) with high antiviral potency against a broad spectrum of RNA viruses (10, 14), including TBEV (7) and other medically important arthropod-borne flaviviruses (10, 12, 13). Currently, this compound entered first-in-human clinical studies that focused on intramuscular administration in healthy volunteers showing promising pharmacokinetics properties and good tolerability (14). This makes galidesivir a promising candidate drug to treat patients with TBE or with other flaviviral infections. However, antiviral therapy based on small molecule inhibitors of viral replication can be accompanied by rapid evolution of drug resistance, which can abolish the progress of infection treatment and finally lead to the failure of the therapy (23). Therefore, for each new antiviral agent, the risks of resistance are important to assess in terms of (i) identification of key mutations conferring virus drug resistance and (ii) phenotype characterization of drug-resistant mutants.
Serial in vitro passaging of TBEV in the presence of increasing concentrations of galidesivir (up to 50 μM) resulted in generation of two drug-resistant TBEV mutants which were ∼7-fold less sensitive to galidesivir than the mock-selected wild-type virus. The first TBEV mutant was characterized by a single amino acid change E460D; the other one carried two amino acid changes, E460D and Y453H. Both mutations mapped to the active site of the viral RdRp. The location of the resistance-associated mutations within the viral RdRp active site is essential to understand the mechanism of action of galidesivir; this compound prevents the binding of subsequent nucleotides to the RdRp active site, being considered a nonobligate chain terminator of viral RNA synthesis (10, 24). Single amino acid changes within the RdRp were previously identified in flaviviruses resistant to structurally different nucleoside analogues, as exemplified by the mutations S600T, S603T, S604T, and S282T conferring a high-level resistance to the 2′-C-methylated nucleosides in dengue virus, TBEV, Zika virus, and hepatitis C virus, respectively (8, 25–28). In Alkhurma haemorrhagic fever virus, the mutation S603T was associated with additional amino acid substitutions located in the NS5 RdRp active site, particularly with C666S and M644V (29).
Using a previously described reverse-genetics system (21, 22), we have demonstrated that the E460D mutation alone is crucial for resistance of TBEV to galidesivir; the recombinant E460D-Rec mutant was ∼7-fold less sensitive to galidesivir compared to the wild type. On the other hand, the growth kinetics of the Y453H-Rec mutant was almost indistinguishable from that of wild-type virus; it is likely that Y453H can represent a compensation mutation or was acquired randomly. Because of the unique structural features of galidesivir (a C-glycosidic bond and a furanose oxygen on the ribose ring replaced by nitrogen) (11), no cross-resistance was seen to structurally different nucleoside analogues, such as 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, and 4′-azido-aracytidine.
The E460D TBEV mutant showed similar growth kinetics to the wild-type virus when cultured in vitro on PS cell monolayers. Although a decreased replication capacity of the E460D mutant was observed in the first few hours after cell culture infection (0 to 36 h p.i.), both viruses reached a peak titer of about 105 to 106 PFU/ml at days 2 to 4 after infection. Similarly, the plaque morphology of the E460D mutant and wild-type virus were almost identical to each other; large, clear, and round plaques reflected the rapid and aggressive spread of both mutant and wild-type viruses in PS cell cultures. Thus, the E460D TBEV mutant differs from the recently isolated S603T TBEV mutant resistant to 2′-C-methylated nucleosides; the S603T mutant exerted significantly decreased replication capacity in PS cells and a completely different plaque morphology (small, turbid plaques) compared to the wild-type virus (8). Our results demonstrate that antiviral resistance developed against two structurally different nucleoside analogues with the same mechanism of action can result in different effects on viral replication capacity in cell culture. Interestingly, in some drug-resistant virus mutants the cell type-dependent replication fitness was observed, as seen in chikungunya virus resistant to T-705 showing the attenuated phenotype in mosquito cell culture, whereas the replication fitness in Vero cells was similar to that of the wild type (30).
Although the introduction of the E460D mutation affects amplification of the virus in PS cell culture (i.e., in vitro) only slightly (within the interval 0 to 36 h p.i.), the E460D substitution resulted in a total loss of neuroinvasiveness for mice, in vivo; the E460D-infected animals all survived and displayed no clinical signs of neuroinfection during the 28-day experimental period. In contrast, infection with wild-type virus resulted in fatal infections for all animals. No virus was detected in the sera, spleens, or brains of mice inoculated with the E460D TBEV. In contrast, wild-type TBEV replicated efficiently in the inoculated mice, causing viremia and infection in the spleen and brain. The replication of the E460D mutant seems to be slower compared to the wild-type (as indicated by the comparison of the growth curves of these two viruses in cell culture) and, it is therefore likely that the virus is rapidly eliminated by the innate immunity soon after the inoculation. Attenuation of in vivo replication have previously been reported for drug-resistant RNA or DNA viral mutants, e.g., for TBEV resistance to 2′-C-methylated nucleosides (8), chikungunya virus resistance to T-705 (30), ribavirin resistance to porcine reproductive and respiratory syndrome virus (31), vaccinia virus resistance to acyclic nucleoside phosphonates (32), and pleconaril resistance to coxsackievirus (33).
The mutant genotype rapidly reverted to wild type when the virus was cultured in PS cell monolayers in the absence of selection agents. However, reversion was not observed when the virus was cultured in the presence of galidesivir in concentrations ranging from 6.25 to 25 μM. Thus, under the selection pressure of galidesivir the mutation provides a replicative advantage over wild-type variants in the virus quasispecies population resulting in predominance of the mutant in the infected cell culture, despite the fact that the replication characteristics of both variants in cell culture are similar. The rapid reversion to glutamic acid in the absence of drug also suggests there is strong preference of an acidic residue at this position, which is consistent with the high conservation of E460 among flaviviral NS5 polymerases (among different TBEV strains, as well as among other representatives of the Flaviviridae family).
We conclude that the resistance of TBEV to the nucleoside analogue galidesivir is conferred by the single amino acid substitution E460D in the NS5 protein. Although this subtle mutation in the active site of the viral RdRp occurs after a few in vitro passages of TBEV in the presence of galidesivir, the E460D TBEV mutant displays a dramatically attenuated phenotype in mice showing high survival rates and a reduction in the clinical signs of neuroinfection. The E460D substitution did not confer cross-resistance to unrelated antiviral nucleoside analogues, such as 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, and 4′-azido-aracytidine. This suggests that a combination treatment based on two or more inhibitors could be a possible strategy in order to minimize the risk of the emergence of viral drug resistance after therapeutic treatment with galidesivir.
MATERIALS AND METHODS
Ethics statement.
This study was carried out in strict accordance with the Czech national law and guidelines on the use of experimental animals and protection of animals against cruelty (Animal Welfare Act no. 246/1992 Coll.). The protocol was approved by the Committee on the Ethics of Animal Experiments of the Institute of Parasitology and of the Departmental Expert Committee for the Approval of Projects of Experiments on Animals of the Academy of Sciences of the Czech Republic (permit 29/2016).
Virus, cells, and antiviral compounds.
A well-characterized, low-passage-number TBEV strain Hypr (34), a member of the European TBEV subtype, was used in this study. Before use, the virus was subcultured intracerebrally six times in suckling mice. Porcine kidney stable (PS) cells (35) were used for viral subculture, selection of drug-resistant viruses, viral growth kinetics studies, and plaque assays. The cells were cultured at 37°C in Leibovitz (L-15) medium supplemented with 3% newborn calf serum and a 1% mixture of penicillin and glutamine (Sigma-Aldrich, Prague, Czech Republic). BHK-21 cells (obtained from the American Type Culture Collection [ATCC]), used for transfection of Hypr-derived subgenomic fragments, were cultured at 37°C with 5% CO2 in minimal essential medium (MEM) containing 7% bovine serum, 1% penicillin/streptomycin, and glutamine. Galidesivir (BCX4430) and 4′-azido-aracytidine (RO-9187) were purchased from MedChemExpress (Stockholm, Sweden); 2′-C-methyladenosine and 7-deaza-2′-C-methyladenosine were obtained from Carbosynth (Compton, UK). For in vitro studies, the test compounds were solubilized in 100% DMSO to yield 10 mM stock solutions.
Selection of drug-resistant viruses.
The in vitro selection of drug-resistant TBEV clones was performed as described previously (8). Briefly, PS cells seeded in 96-well plates (2 × 104 cells per well) and incubated to form a confluent monolayer were infected with TBEV at a multiplicity of infection (MOI) of 0.1 and cultivated in the presence of 5 μM galidesivir. After 3 to 5 days, the culture medium was harvested and used for infection of fresh cell monolayers. Individual passages were performed with gradually increasing concentrations of galidesivir as follows: passage 1 at 5 μM, passages 2 to 4 at 10 μM, passages 5 and 6 at 20 μM, passage 7 at 40 μM, and passages 8 and 9 at 50 μM (Fig. 1B). In parallel, control TBEV was also passaged in the absence of galidesivir (with 0.5% [vol/vol] dimethyl sulfoxide [DMSO]) as a mock-selected wild-type virus. After passage 9, the drug-resistant and control TBEVs were subjected to an additional subculture to prepare virus stocks for further testing (average titers were between 105 and 106 PFU/ml). The in vitro selection protocol was carried out in duplicate, resulting in two independent TBEV mutants, denoted as E460D and E490D/Y453H. In order to recover the revertant wild-type virus from the E460D population, the E460D virus pool was repeatedly subcultured in PS cells in the absence of galidesivir; after six serial subcultures, the obtained revertant was amplified in PS cells to prepare a virus stock for further testing. Each of these viruses was subjected to full-length sequence analysis, sensitivity/resistance assessment to galidesivir and other nucleoside analogues, and virulence characterization in mice.
RNA isolation, PCR, and whole-genome sequencing.
RNA was isolated from growth media by using a QIAmp viral RNA minikit (Qiagen). Reverse transcription was performed by using a ProtoScript first-strand cDNA kit (New England Biolabs) according to the manufacturer’s instructions for the synthesis of first-strand cDNA, which was subsequently used for PCR amplification. To cover the whole genome of TBEV, 35 overlapping DNA fragments were produced by PCR as described previously (36). DNA was purified by using a High Pure PCR product purification kit (Roche, Prague, Czech Republic) according to the recommendations of the manufacturer. The PCR products were directly sequenced by commercial service (SEQme, Czech Republic) using the Sanger sequencing method. Both nucleotide and deduced amino acid sequences were analyzed by using the BioEdit sequence alignment editor, version 7.2.0.
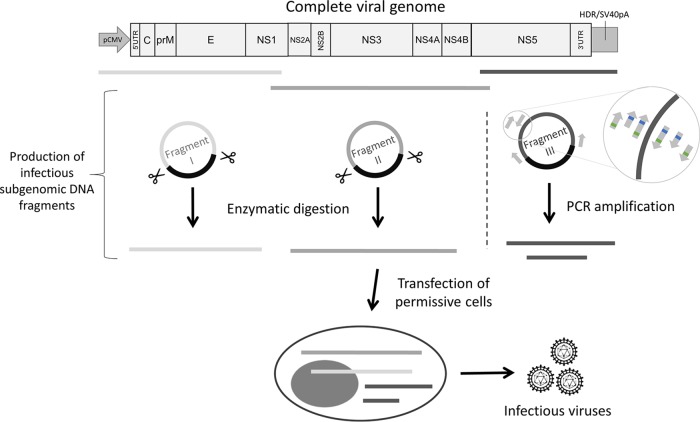
Reverse-genetics system for TBEV hypr.
The reverse-genetics system used in this study was based on the generation of infectious subgenomic overlapping DNA fragments that encompass the entire viral genome, as previously described (21, 22). Three de novo-synthesized DNA fragments cloned into a pUC57 vector were used in this study (GenScript, Piscataway, NJ): fragment I (nucleotide positions 1 to 3662), fragment II (nucleotide positions 3545 to 8043), and fragment III (nucleotide positions 7961 to 11100). The first and last fragments were flanked, respectively, at the 5′ and 3′ ends with the human cytomegalovirus promoter (pCMV) and the hepatitis delta ribozyme, followed by the simian virus 40 polyadenylation signal (HDR/SV40pA) (Fig. 4).
FIG 4.
General overview of the reverse-genetics method presented in the present study. The reverse-genetics method used here was based on the generation of infectious subgenomic overlapping DNA fragments that encompass the entire viral genome. Three de novo-synthesized DNA fragments cloned into a pUC57 vector were used. The first and last fragments were flanked, respectively, at the 5′ and 3′ ends with the human cytomegalovirus promoter (pCMV) and the hepatitis delta ribozyme, followed by the simian virus 40 polyadenylation signal (HDR/SV40pA). Fragments I and II were generated by using the SuPReMe method: plasmids were digested using restriction enzymes. Fragment III was used as the template to generate by PCR two overlapping amplicons according to the original ISA method. Unmodified primers were used to generate two unmodified amplicons (i.e., the production of wild-type virus). Mutated primers located on the targeted region were used to generate two mutated amplicons (green and blue squares represent, respectively, mutations G9045T and T9022C). An equimolar mix of these four DNA fragments was used to transfect BHK-21 cells.
Fragments I and II were generated using the SuPReMe method (22). Briefly, plasmids that contained the DNA fragments I and II were digested by using AgeI/FseI and SmaI/DraI restriction enzymes, respectively (New England BioLabs, Ipswich, MA) (Fig. 4). Fragment III was used as the template to generate by PCR two overlapping amplicons according to the original ISA method (21). Unmodified primers were used to generate two unmodified amplicons (i.e., production of wild-type virus). Mutated primers located on the targeted region were used to generate two mutated amplicons (i.e., production of mutated viruses, denoted as E460D-Rec, Y453H-Rec, and E460D/Y453H-Rec) (Table 2, Fig. 4).
The PCR was performed using a Platinum SuperFI PCR master mix (Thermo Fisher Scientific, Prague, Czech Republic). The mixture (final volume, 50 μl) contained 45 μl of SuperMix and 2 μl of DNA template (fragment III) at 1 ng/μl. Assays were performed on a Biometra TProfessional standard gradient thermocycler and the following conditions: 94°C for 2 min, followed by 40 cycles of 94°C for 15 s, 60°C for 30 s, and 68°C for 5 min and a final elongation step of 68°C for 10 min. The size of the PCR products was verified by gel electrophoresis and purified using an Amicon Ultra 0.5-ml kit (Millipore, Prague, Czech Republic).
An equimolar mixture of these four DNA fragments was used for cell transfection. A DNA-lipid complex was prepared as follows: 12 μl of Lipofectamine 3000 (Thermo Fisher Scientific, Prague, Czech Republic) was diluted in 250 μl of Opti-MEM medium (Life Technologies) and then mixed with a master solution of DNA that contained 3 μg of DNA and 6 μl of P3000 reagent diluted in 250 μl of Opti-MEM medium. After a 45-min incubation at room temperature, BHK-21 cells were transfected as described previously (37) and incubated for 5 to 7 days. Cell supernatant media were then harvested and serially passaged twice in fresh BHK-21 culture.
Growth kinetics, dose-response studies, and viral inhibition assays.
To evaluate growth kinetics of drug-resistant TBEV mutants, PS cell monolayers incubated for 24 h in 96-well plates were treated with 200 μl of medium containing galidesivir at concentrations of 25 μM (compound-treated cells) or 0.5% (vol/vol) DMSO (mock-treated cells) and simultaneously infected with TBEV; an MOI of 0.1 was used for all TBEV mutant/wild-type samples tested. The medium was collected from the wells daily at days 1 to 7 p.i. (three wells per interval). Viral titers (expressed as PFU/ml) were determined by plaque assay as described previously (9, 38) and used to construct TBEV growth curves.
For dose-response studies, 200-μl portions of fresh medium containing galidesivir at concentrations ranging from 0 to 50 μM were added to PS cell monolayers, infected with TBEV at an MOI of 0.1, and incubated for 3 to 4 days p.i. The medium was then collected from the wells, and the viral titers were determined by plaque assay. The obtained viral titer values were used for the construction of TBEV dose-response/inhibition curves and to estimate the EC50 of the drug.
To measure the sensitivity/resistance of the obtained TBEV mutants to galidesivir and several structurally unrelated nucleoside analogues in cell culture by viral titer inhibition assay, confluent PS cell monolayers cultured for 24 h at 37°C in 96-well plates were treated with galidesivir, 7-deaza-2′-C-methyladenosine, 2′-C-methyladenosine, or 4′-azido-aracytidine (RO-9187) at concentrations of 25 or 50 μM and simultaneously infected with TBEV at an MOI of 0.1 (three wells per compound). As a mock-treated control, DMSO was added to virus- and mock-infected cells at a final concentration of 0.5% (vol/vol). The formation of a cytopathic effect (CPE) was monitored visually using an Olympus BX-5 microscope to yield a 70 to 90% CPE in virus-infected cultures, and viral titers were determined by plaque assays from cell culture supernatants.
Mouse infections.
To evaluate the virulence of the Hypr E460D mutant in mice, four groups of 6-week-old BALB/c female mice (purchased from AnLab, Prague, Czech Republic) were infected s.c. with TBEV (1,000 PFU/mouse, which represents a lethal dose causing 90 to 100% mortality of BALB/c mice, if the TBEV Hypr strain is used for the infection [8]) as follows: group 1 (n = 10), infected with in vitro mock-selected wild type; group 2 (n = 10), infected with in vitro-selected mutant (E460D); group 3 (n = 10), infected with recombinant wild-type TBEV; and group 4 (n = 10), infected with recombinant mutant (E460D-Rec). The survival rates of TBEV-infected mice were monitored daily over the 28-day experimental period. At the same time, monitoring symptoms of illness and evaluation of clinical scores were performed in infected animals. Signs of sickness were scored as follows: 0, no symptoms; 1, ruffled fur; 2, slowing of activity or hunched posture; 3, asthenia or mild paralysis; 4, lethargy, tremor, or complete paralysis of the limbs; and 5, death. All mice exhibiting disease consistent with clinical score 4 were terminated humanely (cervical dislocation) immediately upon detection.
In order to investigate the spread of the virus in the infected animals, two groups of 6-week-old BALB/c female mice were inoculated subcutaneously with TBEV (1,000 PFU/mouse) as follows: group 1 (n = 15), infected with in vitro mock-selected wild type, and group 2 (n = 15), infected with in vitro-selected mutant (E460D). Three mice of each group were terminated on day 1, 3, 5, 8, and 9 p.i., and the sera, brains, and spleens of the infected animals were collected. The organs were weighed, homogenized using Precellys 24 (Bertin Technologies), and prepared as 20% (wt/vol) suspension in L-15 medium containing 3% newborn calf serum. The homogenates were clarified by centrifugation at 5,000 × g, and the supernatant medium was used for plaque assay.
Statistical analyses.
Data are expressed as means ± the standard deviations, and the significance of differences between groups was evaluated using the Mann-Whitney U test or analysis of variance. Survival rates were analyzed by using the log-rank Mantel-Cox test. All tests were performed using GraphPad Prism 5.04 (GraphPad Software, Inc., San Diego, CA). P values of <0.05 were considered statistically significant.
ACKNOWLEDGMENTS
This study was supported by a grant from the Ministry of Education, Youth, and Sports of the Czech Republic (grant LTAUSA18016) (to L.E.), by a grant from the Ministry of Health of the Czech Republic (grant 16-34238A), and by Project FIT (Pharmacology, Immunotherapy, Nanotoxicology; CZ.02.1.01/0.0/0.0/15_003/0000495) from the Ministry of Education, Youth, and Sports of the Czech Republic and the Ministry of Agriculture of the Czech Republic (RO0518) (both to D.R.).
REFERENCES
- 1.Ruzek D, Avšič Županc T, Borde J, Chrdle A, Eyer L, Karganova G, Kholodilov I, Knap N, Kozlovskaya L, Matveev A, Miller AD, Osolodkin DI, Överby AK, Tikunova N, Tkachev S, Zajkowska J. 2019. Tick-borne encephalitis in Europe and Russia: review of pathogenesis, clinical features, therapy, and vaccines. Antiviral Res 164:23–51. doi: 10.1016/j.antiviral.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Dumpis U, Crook D, Oksi J. 1999. Tick-borne encephalitis. Clin Infect Dis 28:882–890. doi: 10.1086/515195. [DOI] [PubMed] [Google Scholar]
- 3.Heinz FX, Mandl CW. 1993. The molecular-biology of tick-borne encephalitis virus. APMIS 101:735–745. doi: 10.1111/j.1699-0463.1993.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 4.Ruzek D, Dobler G, Mantke OD. 2010. Tick-borne encephalitis: pathogenesis and clinical implications. Travel Med Infect Dis 8:223–232. doi: 10.1016/j.tmaid.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Eyer L, Nencka R, de Clercq E, Seley-Radtke K, Růžek D. 2018. Nucleoside analogs as a rich source of antiviral agents active against arthropod-borne flaviviruses. Antivir Chem Chemother 26:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eyer L, Šmídková M, Nencka R, Neča J, Kastl T, Palus M, De Clercq E, Růžek D. 2016. Structure-activity relationships of nucleoside analogues for inhibition of tick-borne encephalitis virus. Antiviral Res 133:119–129. doi: 10.1016/j.antiviral.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Eyer L, Zouharová D, Širmarová J, Fojtíková M, Štefánik M, Haviernik J, Nencka R, de Clercq E, Růžek D. 2017. Antiviral activity of the adenosine analogue BCX4430 against West Nile virus and tick-borne flaviviruses. Antiviral Res 142:63–67. doi: 10.1016/j.antiviral.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Eyer L, Kondo H, Zouharova D, Hirano M, Valdes JJ, Muto M, Kastl T, Kobayashi S, Haviernik J, Igarashi M, Kariwa H, Vaculovicova M, Cerny J, Kizek R, Kroger A, Lienenklaus S, Dejmek M, Nencka R, Palus M, Salat J, De Clercq E, Yoshii K, Ruzek D. 2017. Escape of tick-borne flavivirus from 2′-C-methylated nucleoside antivirals is mediated by a single conservative mutation in NS5 That has a dramatic effect on viral fitness. J Virol 91:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eyer L, Valdés JJ, Gil VA, Nencka R, Hřebabecký H, Šála M, Salát J, Černý J, Palus M, De Clercq E, Růžek D. 2015. Nucleoside inhibitors of tick-borne encephalitis virus. Antimicrob Agents Chemother 59:5483–5493. doi: 10.1128/AAC.00807-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warren TK, Wells J, Panchal RG, Stuthman KS, Garza NL, Van Tongeren SA, Dong L, Retterer CJ, Eaton BP, Pegoraro G, Honnold S, Bantia S, Kotian P, Chen X, Taubenheim BR, Welch LS, Minning DM, Babu YS, Sheridan WP, Bavari S. 2014. Protection against filovirus diseases by a novel broad-spectrum nucleoside analogue BCX4430. Nature 508:402–405. doi: 10.1038/nature13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Clercq E. 2016. C-nucleosides to be revisited. J Med Chem 59:2301–2311. doi: 10.1021/acs.jmedchem.5b01157. [DOI] [PubMed] [Google Scholar]
- 12.Julander JG, Siddharthan V, Evans J, Taylor R, Tolbert K, Apuli C, Stewart J, Collins P, Gebre M, Neilson S, Van Wettere A, Lee YM, Sheridan WP, Morrey JD, Babu YS. 2017. Efficacy of the broad-spectrum antiviral compound BCX4430 against Zika virus in cell culture and in a mouse model. Antiviral Res 137:14–22. doi: 10.1016/j.antiviral.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Julander JG, Bantia S, Taubenheim BR, Minning DM, Kotian P, Morrey JD, Smee DF, Sheridan WP, Babu YS. 2014. BCX4430, a novel nucleoside analog, effectively treats Yellow Fever in a hamster model. Antimicrob Agents Chemother 58:6607–6614. doi: 10.1128/AAC.03368-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor R, Kotian P, Warren T, Panchal R, Bavari S, Julander J, Dobo S, Rose A, El-Kattan Y, Taubenheim B, Babu Y, Sheridan WP. 2016. BCX4430: a broad-spectrum antiviral adenosine nucleoside analog under development for the treatment of Ebola virus disease. J Infect Public Health 9:220–226. doi: 10.1016/j.jiph.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westover JB, Mathis A, Taylor R, Wandersee L, Bailey KW, Sefing EJ, Hickerson BT, Jung KH, Sheridan WP, Gowen BB. 2018. Galidesivir limits Rift Valley fever virus infection and disease in Syrian golden hamsters. Antiviral Res 156:38–45. doi: 10.1016/j.antiviral.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bagaglio S, Uberti-Foppa C, Morsica G. 2017. Resistance mechanisms in hepatitis C virus: implications for direct-acting antiviral use. Drugs 77:1043–1055. doi: 10.1007/s40265-017-0753-x. [DOI] [PubMed] [Google Scholar]
- 17.Irwin KK, Renzette N, Kowalik TF, Jensen JD. 2016. Antiviral drug resistance as an adaptive process. Virus Evol 2:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poveda E, Wyles DL, Mena A, Pedreira JD, Castro-Iglesias A, Cachay E. 2014. Update on hepatitis C virus resistance to direct-acting antiviral agents. Antiviral Res 108:181–191. doi: 10.1016/j.antiviral.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 19.Lauring AS, Frydman J, Andino R. 2013. The role of mutational robustness in RNA virus evolution. Nat Rev Microbiol 11:327–336. doi: 10.1038/nrmicro3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eyer L, Nougairède A, Uhlířová M, Driouich J-S, Zouharová D, Valdés JJ, Haviernik J, Gould EA, De Clercq E, de Lamballerie X, Ruzek D. 2019. An E460D substitution in the NS5 protein of tick-borne encephalitis virus confers resistance to the inhibitor galidesivir (BCX4430) and also attenuates the virus for mice. bioRxiv doi: 10.1101/563544. [DOI] [PMC free article] [PubMed]
- 21.Aubry F, Nougairede A, de Fabritus L, Querat G, Gould EA, De Lamballerie X. 2014. Single-stranded positive-sense RNA viruses generated in days using infectious subgenomic amplicons. J Gen Virol 95:2462–2467. doi: 10.1099/vir.0.068023-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Driouich J-S, Ali SM, Amroun A, Aubry F, de Lamballerie X, Nougairède A. 2018. SuPReMe: a rapid reverse genetics method to generate clonal populations of recombinant RNA viruses. Emerg Microbes Infect 7:1–11. doi: 10.1038/s41426-018-0040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pawlotsky JM. 2011. Treatment failure and resistance with direct-acting antiviral drugs against hepatitis C virus. Hepatology 53:1742–1751. doi: 10.1002/hep.24262. [DOI] [PubMed] [Google Scholar]
- 24.De Clercq E, Neyts J. 2009. Antiviral agents acting as DNA or RNA chain terminators. Handb Exp Pharmacol 189:53–84. doi: 10.1007/978-3-540-79086-0_3. [DOI] [PubMed] [Google Scholar]
- 25.Hercik K, Brynda J, Nencka R, Boura E. 2017. Structural basis of Zika virus methyltransferase inhibition by sinefungin. Arch Virol 162:2091–2096. doi: 10.1007/s00705-017-3345-x. [DOI] [PubMed] [Google Scholar]
- 26.Hercik K, Kozak J, Sala M, Dejmek M, Hrebabecky H, Zbornikova E, Smola M, Ruzek D, Nencka R, Boura E. 2017. Adenosine triphosphate analogs can efficiently inhibit the Zika virus RNA-dependent RNA polymerase. Antiviral Res 137:131–133. doi: 10.1016/j.antiviral.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 27.Migliaccio G, Tomassini JE, Carroll SS, Tomei L, Altamura S, Bhat B, Bartholomew L, Bosserman MR, Ceccacci A, Colwell LF, Cortese R, De Francesco R, Eldrup AB, Getty KL, Hou XS, LaFemina RL, Ludmerer SW, MacCoss M, McMasters DR, Stahlhut MW, Olsen DB, Hazuda DJ, Flores OA. 2003. Characterization of resistance to non-obligate chain-terminating ribonucleoside analogs that inhibit hepatitis C virus replication in vitro. J Biol Chem 278:49164–49170. doi: 10.1074/jbc.M305041200. [DOI] [PubMed] [Google Scholar]
- 28.Xu HT, Hassounah SA, Colby-Germinario SP, Oliveira M, Fogarty C, Quan YD, Han YS, Golubkov O, Ibanescu I, Brenner B, Stranix BR, Wainberg MA. 2017. Purification of Zika virus RNA-dependent RNA polymerase and its use to identify small-molecule Zika inhibitors. J Antimicrob Chemother 72:727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flint M, McMullan LK, Dodd KA, Bird BH, Khristova ML, Nichol ST, Spiropoulou CF. 2014. Inhibitors of the tick-borne, hemorrhagic fever-associated flaviviruses. Antimicrob Agents Chemother 58:3206–3216. doi: 10.1128/AAC.02393-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Delang L, Yen PS, Vallet T, Vazeille M, Vignuzzi M, Failloux AB. 2018. Differential transmission of antiviral drug-resistant chikungunya viruses by Aedes mosquitoes. mSphere 3:e00230-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khatun A, Shabir N, Seo BJ, Kim BS, Yoon KJ, Kim WI. 2016. The attenuation phenotype of a ribavirin-resistant porcine reproductive and respiratory syndrome virus is maintained during sequential passages in pigs. J Virol 90:4454–4468. doi: 10.1128/JVI.02836-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gammon DB, Snoeck R, Fiten P, Krecmerova M, Holy A, De Clercq E, Opdenakker G, Evans DH, Andrei G. 2008. Mechanism of antiviral drug resistance of vaccinia virus: identification of residues in the viral DNA polymerase conferring differential resistance to antipoxvirus drugs. J Virol 82:12520–12534. doi: 10.1128/JVI.01528-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Groarke JM, Pevear DC. 1999. Attenuated virulence of pleconaril-resistant coxsackievirus B3 variants. J Infect Dis 179:1538–1541. doi: 10.1086/314758. [DOI] [PubMed] [Google Scholar]
- 34.Pospisil L, Jandasek L, Pesek J. 1954. Isolation of new strains of meningoencephalitis virus in the Brno region during the summer of 1953. Lek List 9:3–5. [PubMed] [Google Scholar]
- 35.Kozuch O, Mayer V. 1975. Pig kidney epithelial (Ps) cells: perfect tool for study of flaviviruses and some other arboviruses. Acta Virol 19:498. [PubMed] [Google Scholar]
- 36.Ruzek D, Gritsun TS, Forrester NL, Gould EA, Kopecky J, Golovchenko M, Rudenko N, Grubhoffer L. 2008. Mutations in the NS2B and NS3 genes affect mouse neuroinvasiveness of a Western European field strain of tick-borne encephalitis virus. Virology 374:249–255. doi: 10.1016/j.virol.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Aubry F, Nougairede A, de Fabritus L, Piorkowski G, Gould EA, De Lamballerie X. 2015. ISA-Lation of single-stranded positive-sense RNA viruses from non-infectious clinical/animal samples. PLoS One 10:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Madrid AT, Porterfield JS. 1969. A simple micro-culture method for the study of group B arboviruses. Bull World Health Organ 40:113–121. [PMC free article] [PubMed] [Google Scholar]