Abstract
Background:
Outcomes after anterior cruciate ligament reconstruction (ACLR) are not uniformly good and are worse among young female athletes. Developing better rehabilitation and return-to-sport training programs and evaluating their outcomes are essential.
Purpose:
(1) Test the effect of strength, agility, plyometric, and secondary prevention (SAPP) exercises with and without perturbation training (SAPP + PERT) on strength, hops, function, activity levels, and return-to-sport rates in young female athletes 1 and 2 years after ACLR and (2) compare 2-year functional outcomes and activity levels among young female athletes in the Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports (ACL-SPORTS) trial to homogeneous cohorts who completed criterion-based postoperative rehabilitation alone (Multicenter Orthopaedic Outcomes Network [MOON]) and in combination with extended preoperative rehabilitation (Delaware-Oslo).
Study Design:
Randomized controlled trial, Level of evidence, 1; and cohort study, Level of evidence, 3.
Methods:
A total of 40 level 1 and level 2 female athletes were enrolled after postoperative impairment resolution 3 to 9 months after primary ACLR. Participants were randomized to 10 SAPP or SAPP + PERT sessions and were tested 1 and 2 years after ACLR on quadriceps strength, hop tests, functional outcomes, and return-to-sport rates. Participants were then compared with homogeneous cohorts of young (<25 years) female athletes who completed criterion-based postoperative rehabilitation alone (MOON) and in combination with extended preoperative rehabilitation (Delaware-Oslo) on 2-year functional outcomes.
Results:
No significant or meaningful differences were found between SAPP and SAPP + PERT, so groups were collapsed for comparison with the other cohorts. At 2-year follow-up, ACL-SPORTS had the highest scores (P < .01) on the Marx activity rating scale (ACL-SPORTS, 13.5 ± 3.3; Delaware-Oslo, 12.5 ± 2.7; MOON, 10.6 ± 5.1); International Knee Documentation Committee Subjective Knee Evaluation Form (96 ± 7, 92 ± 9, and 84 ± 14, respectively); and Knee injury and Osteoarthritis Outcome Score (KOOS) subscales for Pain (98 ± 4, 94 ± 9, and 90 ± 10, respectively), Symptoms (94 ± 6, 90 ± 9, and 83 ± 14, respectively), Activities of Daily Living (100 ± 1, 99 ± 4, and 96 ± 7, respectively), Sports and Recreation (94 ± 8, 86 ± 15, and 82 ± 17, respectively), and Quality of Life (89 ± 14, 78 ± 18, and 76 ± 19, respectively). The Patient Acceptable Symptom State threshold on the KOOS–Sports and Recreation was achieved by 100% of the ACL-SPORTS cohort compared with 90% of Delaware-Oslo and 78% of MOON (P = .011).
Conclusion:
Although perturbation training provided no added benefit, 10 sessions of return-to-sport training, compared with criterion-based postoperative rehabilitation alone, yielded statistically significant and clinically meaningfully higher 2-year functional outcomes among young, high-level female athletes after ACLR.
Registration:
NCT01773317 (ClinicalTrials.gov identifier).
Keywords: anterior cruciate ligament (ACL), female athlete, return-to-sport training, physical therapy/rehabilitation, functional outcomes
Recent injury surveillance data suggest that anterior cruciate ligament (ACL) injuries are occurring at alarming rates3,51 among adolescents and young adults who engage in sports involving jumping, cutting, and pivoting,15,24 and rates are higher among female versus male athletes in similar sports.2,3,5 Women are also less likely to return to any sport, or to preinjury sport level, after ACL injury and ACL reconstruction (ACLR).4,10 When they do return to sport, women are more likely than men to experience a second ACL injury.21,38–40 Moreover, female athletes have poorer functional recovery after ACL injury25 and lower activity levels than their male counterparts at 2 to 6 years after ACLR.16,46 Developing and evaluating rigorous rehabilitation and return-to-sport (RTS) training programs, and comparing outcomes from these programs with those from previously successful cohorts, are essential for improving outcomes among high-level female athletes after ACL injury and ACLR.
Previous work has evaluated extended preoperative rehabilitation and postoperative rehabilitation paradigms on outcomes among athletes after ACLR. Failla et al17,18 found superior functional outcomes and higher RTS rates among athletes who participated in extended preoperative rehabilitation including neuromuscular training compared with those who did not. Although a 2018 systematic review determined there is no evidence to support a single, most appropriate rehabilitation protocol after ACLR,48 clinical practice guidelines31,32 exist, and several criterion-based postoperative rehabilitation protocols1,11,28,35,50 have been proposed. Two recent articles provide high-quality evidence supporting the use of such criterion-based approaches to achieve objective criteria, including ≥90% strength and hop test limb symmetry indexes, prior to RTS.23,30 Formal rehabilitation, however, typically ends well before athletes achieve these criteria, and athletes often receive RTS clearance without first meeting these, or any, objective criteria.9,44 Therefore, training programs to bridge the gap between postoperative rehabilitation, the current standard of care, and achievement of objective criteria may be a critical component to improve outcomes after ACLR.
The Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports (ACL-SPORTS) training protocol was developed to fill this gap by evaluating an RTS training program designed to be completed following postoperative rehabilitation and impairment resolution and prior to testing for clearance for unrestricted participation in sports. Specifically, the ACL-SPORTS randomized controlled trial was designed to test the effect of 10 sessions of strength, agility, plyometric, and secondary prevention (SAPP) exercises with and without the addition of perturbation training (SAPP + PERT).49 Among the men of the ACL-SPORTS trial, no significant or meaningful differences were found between SAPP versus SAPP + PERT training on strength, function, or gait mechanics at pretraining, posttraining, or 1 year or 2 years after ACLR.7,8,12,13 Across intervention groups, however, the men did exceedingly well, including symmetric functional performance on strength and hop testing, high patient-reported outcome measures, and a 100% RTS rate, with 95% attaining their preinjury level of sport by 2 years after ACLR.6–8 Among the women of the ACL-SPORTS trial, no between-group differences were seen at pre- or posttraining time points7; however, the effect of the ACL-SPORTS training program on 1- and 2-year outcomes in women is unknown. The comparative effectiveness of postoperative RTS training versus criterion-based postoperative rehabilitation alone or with the addition of extended preoperative rehabilitation is also unknown.
The purpose of the present study was 2-fold. The study first sought to compare the effect of SAPP versus SAPP + PERT training on the 1- and 2-year primary clinical outcomes (ie, quadriceps strength, patient-reported outcomes, and single-legged hop testing) in female athletes of the ACL-SPORTS trial. The a priori first hypothesis was that SAPP + PERT would result in superior outcomes compared with SAPP alone. The second aim was to evaluate the comparative effectiveness of 10 sessions of RTS training on clinical and functional outcomes in young female athletes 2 years after ACLR. The hypothesis for aim 2 was that female athletes who completed postoperative RTS training, compared with those who did not, would have higher functional outcomes and activity levels 2 years after ACLR.
Methods
This study included both a prospective randomized controlled trial (NCT01773317) and a cohort study; institutional review board approval and written informed consent were obtained for all participants.
ACL-SPORTS Trial
Participants
For the ACL-SPORTS randomized controlled trial, 40 female athletes were enrolled, based on power calculations described previously,7,49 at the University of Delaware between December 2011 and January 2017; 2-year follow-up testing was completed by August 2018, at which time the trial ended as initially planned. Athletes were enrolled only if they were 3 to 9 months after primary ACLR (mean ± SD, 6 ± 2 months) and had achieved 80% or greater quadriceps strength index, minimal to no knee effusion,47 full knee range of motion, and initiation of a running progression.1 Although preenrollment (preoperative or postoperative) rehabilitation was not controlled, all participants underwent physical therapy and were required to meet objective clinical criteria, consistent with criterion-based rehabilitation,1 prior to enrollment. Patients with concomitant meniscal injury (including repair and/or partial meniscectomy to one or both menisci at the time of ACLR) were included. Athletes were excluded if they had a previous ACL injury or lower extremity surgery to either knee, had a concomitant grade 3 knee ligament injury or large (>1 cm2) osteochondral defect, were not between ages 13 to 55 years at enrollment, or did not participate regularly (50 hours per year) in jumping, cutting, or pivoting sports prior to ACL injury. Participants completed testing before and after 10 RTS training sessions and at 1 and 2 years after ACLR, as presented in the study flow diagram (Figure 1). Athletes who sustained a second ACL injury (graft rupture or contralateral injury) prior to follow-up testing were excluded from the analyses of strength, hop testing, and patient-reported outcomes to prevent confounding of results.
Figure 1.
Flow chart for Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports (ACL-SPORTS) randomized controlled trial. ACL, anterior cruciate ligament; RTS, return to sport; SAPP, strength, agility, plyometric, and secondary prevention; SAPP + PERT, SAPP with perturbation training.
Methods
Participants were randomized by a research administrator using a random number generator and block randomization, so that an equal number of participants would be allocated to receive SAPP and SAPP + PERT training. They subsequently completed 10 training sessions (∼2 times per week). Athletes in both training groups completed the common elements of the RTS training program, including Nordic hamstrings, standing squats, drop jumps, triple (single-legged) hopping, tuck jumps, and progressive agility drills. Athletes in the SAPP + PERT group additionally completed 10 sessions of perturbation training,19,20 whereas athletes in the SAPP group did a sham exercise using a resistance band.49 Perturbation training is a specific type of neuromuscular training program where the participant stands on an unstable surface (ie, rollerboard or rockerboard) and a physical therapist applies movements, or perturbations, to the surface; readers may consult Fitzgerald et al19,20 and White et al49 for a more thorough description of perturbation training.
Athletes were tested 1 and 2 years after primary ACLR on the primary outcome measures (SAPP vs SAPP + PERT training), knee biomechanics during walking (null findings),14 as well as the secondary outcome measures (quadriceps strength, single-legged hop tests, patient-reported outcomes, and RTS rates).49 Research physical therapists (J.J.C., J.L.J.) who were blinded to treatment group completed all testing. Isometric quadriceps strength was assessed by use of an isokinetic dynamometer with the knee flexed to 90° and burst superimposition.45 The uninvolved limb was tested first, followed by the involved limb; approximately 3 trials per limb were recorded, and the highest value for each limb was used to calculate a quadriceps strength limb symmetry index ([Involved Limb Strength ÷ Uninvolved Limb Strength] × 100%). Participants were subsequently evaluated on 4 hop tests (single, triple, crossover, and timed 6-m).36 Two trials were averaged for each limb and were used to calculate a limb symmetry index (LSI) for each hop test. Participants also completed several valid and reliable patient-reported outcome measures, including the International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC),24 Knee injury and Osteoarthritis Outcome Score (KOOS) subscales,43 Knee Outcome Survey–Activities of Daily Living Subscale (KOS-ADLS),27 Global Rating Scale of Perceived Function (GRS),49 and Marx activity rating scale (Marx).33
Participants were asked questions at each time point about their participation in sports: (1) Have you returned to sports or recreational activities? (yes/no); and (2) Have you returned to the same level of sports or recreational activities as before your injury? (yes/no). These questions, respectively, were used to calculate RTS rates to any level and their self-reported preinjury level of sport by 2 years (ie, from posttraining through 2 years after ACLR). Participants listed reasons for answering “no” to either RTS question.
Statistical Analyses
Between-group comparisons for quadriceps strength index, hop test LSIs, and patient-reported outcome measures 1 and 2 years after ACLR were conducted by use of mixed-measures analysis of variance (ANOVA; α = .05). The Fisher exact test was used to compare the proportion of athletes in each group who had returned to sport by 2 years (α = .05).
Power Calculations
A priori power analysis calculations were based on sagittal plane knee biomechanics and indicated that 36 women were needed to detect a medium effect size (0.3) with β = .20 and α = .05.49 A secondary power analysis based on the IKDC indicated that 5 participants per group would be sufficient to detect a difference in IKDC scores equivalent to the minimal clinically important difference of 11.5 (power = 0.95, α = .05, effect size of f(V) = 6.44) using a 2 × 2 ANOVA.7
Comparative Effectiveness of ACL-SPORTS, MOON, and Delaware-Oslo Cohorts
Participants
This was a secondary analysis of prospectively collected data acquired through the Multicenter Orthopaedic Outcomes Network (MOON), Delaware-Oslo, and ACL-SPORTS cohorts. Data from the MOON cohort and Delaware-Oslo cohort have been published previously17,18 and were used in the present study to evaluate RTS training (ACL-SPORTS cohort) compared with criterion-based postoperative rehabilitation alone (MOON cohort) and extended preoperative rehabilitation plus criterion-based postoperative rehabilitation (Delaware-Oslo cohort). The MOON cohort provides a large database of participants who received standardized postoperative rehabilitation after ACLR50 and represents standard-of-care treatment for individuals after ACLR within the United States. The Delaware-Oslo cohort provides a rich data set of individuals who received extended preoperative rehabilitation in addition to criterion-based postoperative rehabilitation; Failla et al17,18 found superior 2-year outcomes in the Delaware-Oslo cohort versus the MOON cohort, which represents best evidence for current rehabilitation practice.
Inclusion and exclusion criteria were applied strictly to each cohort to create homogeneous comparison groups, as described below. Additionally, age was constrained to include only those aged 13 to 24 years at enrollment (ACL-SPORTS) or time of surgery (Delaware Oslo and MOON) to focus on the young female athletes at particularly high risk for poor outcomes after ACLR.4,10,16,21,25,38–40,46 Inclusion criteria were female sex; age 13 to 24 years at enrollment; available functional outcomes data from approximately 2 years after primary, unilateral ACLR; and participant in level 1 or 2 sport15,24 prior to index ACLR. Exclusion criteria were previous ACL injury to either knee; symptomatic concomitant grade 3 knee ligament (ie, posterior cruciate ligament [PCL], lateral collateral ligament [LCL], medial collateral ligament [MCL] injury or surgery; articular cartilage defect larger than 1 cm2 or microfracture surgery; or second ACL rupture (Delaware-Oslo) or ACLR (ACL-SPORTS and MOON) to either knee prior to 2-year testing.
Methods and Measures
Participants from the MOON cohort participated in standardized, criterion-based postoperative rehabilitation50 alone (ie, without extended preoperative rehabilitation or postoperative RTS training) and represented standard of care. Participants in the Delaware-Oslo cohort participated in 10 preoperative rehabilitation sessions consisting of progressive strengthening and neuromuscular training including perturbation training, followed by a criterion-based postoperative rehabilitation program1 without formal RTS training. Participants in the ACL-SPORTS cohort participated in 10 RTS training sessions consisting of strengthening, agility drills, and plyometric exercises designed to facilitate return to sports participation. Participants in each cohort completed the IKDC, KOOS subscales, and Marx patient-reported outcome measures 2 years after primary ACLR.
Statistical Analyses
Demographic comparisons were made between groups through use of 1-way ANOVA and chi-square tests of proportions for continuous and categorical variables, respectively (α = .05). One-way ANOVAs with post hoc comparisons between groups were used to compare scores on the IKDC, KOOS subscales, and Marx (α = .05). The proportion of athletes in each cohort who met the Patient Acceptable Symptom State (PASS) thresholds for the IKDC and each of the KOOS subscales34 was calculated and compared among cohorts for each variable through use of chi-square tests of proportions (α = .05).
Results
ACL-SPORTS Results: SAPP Versus SAPP + PERT Training
Demographic characteristics did not differ between the SAPP and SAPP + PERT groups (Appendix Table A1). No statistically significant or clinically meaningful differences were found between the SAPP and SAPP + PERT groups on any outcome measure, including quadriceps strength index, LSI on any hop test (single, crossover, triple, 6-m timed), or any functional outcome measure (ie, KOS-ADLS, GRS, IKDC, any KOOS subscale, or the Marx) (Appendix Table A2). All athletes (39/39, 100%) returned to sport by 2 years, including 87% (34/39) who returned at their self-reported preinjury level. No between-group differences were found in RTS rates (SAPP, 19/20; SAPP + PERT, 15/19; P = .182; odds ratio of returning to preinjury sport level, 1.2; 95% CI, 0.9-1.6).
Comparative Effectiveness: ACL-SPORTS, Delaware-Oslo, and MOON Results
There were 431 MOON participants, 39 Delaware-Oslo participants, and 24 ACL-SPORTS participants; not all participants completed every survey. No differences were seen in age, body mass index, preinjury sport level, or medial meniscal treatment among the 3 comparison cohorts; however, differences were noted across groups in time to 2-year follow-up, graft type, and lateral meniscal treatment (Table 1). Significant differences were found in all outcome measures, including the Marx, IKDC, KOOS Pain, KOOS Symptoms, KOOS Activities of Daily Living (ADL), KOOS Sports and Recreation (Sports/Rec), and KOOS Knee-Related Quality of Life (QoL), with the ACL-SPORTS cohort having the highest scores across every outcome (Table 2). Post hoc comparisons revealed that ACL-SPORTS, compared with MOON, had significantly higher scores across all outcome measures (post hoc P ≤ .006); between-group differences exceeded the minimal clinically important difference (MCID) values for the IKDC26 and KOOS subscales for Symptoms, Sports/Rec, and QoL.42 The ACL-SPORTS cohort also scored significantly and meaningfully42 higher on the KOOS QoL (post hoc P = .034) and tended to score higher on the KOOS Sports/Rec (post hoc P = .068) compared with the Delaware-Oslo cohort. The Delaware-Oslo group, compared with the MOON group, had significantly higher scores (post hoc P ≤ .035) on the IKDC, KOOS Pain, KOOS Symptoms, and KOOS ADL, although none of these differences exceeded MCID values.26,42
TABLE 1.
Demographic Characteristics for the Comparative Effectiveness Studya
| Variable | Cohort | n | Mean | SD | P Value |
|---|---|---|---|---|---|
| Age, y | MOON | 431 | 17.2 | 2.6 | .156 |
| DE-Oslo | 39 | 18.0 | 3.1 | ||
| ACL-SPORTS | 24 | 17.3 | 2.6 | ||
| BMI, kg/m2 | MOON | 424 | 23.3 | 4.1 | .125 |
| DE-Oslo | 39 | 22.4 | 2.8 | ||
| ACL-SPORTS | 24 | 24.4 | 3.6 | ||
| Time to 2-year follow-up, y | MOONb | 427 | 2.4 | 0.4 | <.001 |
| DE-Osloc | 39 | 2.1 | 0.3 | ||
| ACL-SPORTSc | 24 | 2.1 | 0.3 | ||
| Frequency | |||||
| Graft type | MOONb | 7% allograft, 62% BPTB, 31% soft tissue autograft | .003 | ||
| DE-Osloc | 10% allograft, 31% BPTB, 59% soft tissue autograft | ||||
| ACL-SPORTSb | 4% allograft, 67% BPTB, 29% soft tissue autograft | ||||
| Preinjury sport level | MOON | 78% level 1, 22% level 2 | .187 | ||
| DE-Oslo | 85% level 1, 15% level 2 | ||||
| ACL-SPORTS | 92% level 1, 8% level 2 | ||||
| Medial meniscal treatment | MOON | 72% none, 8% meniscectomy, 18% repair, 2% rasping/trephination | .233 | ||
| DE-Oslo | 85% none, 3% meniscectomy, 8% repair, 5% rasping/trephination | ||||
| ACL-SPORTS | 76% none, 10% meniscectomy, 10% repair, 5% rasping/trephination | ||||
| Lateral meniscal treatment | MOONb | 65% none, 26% meniscectomy, 9% repair, 1% rasping/trephination | .001 | ||
| DE-Osloc | 87% none, 5% meniscectomy, 3% repair, 5% rasping/trephination | ||||
| ACL-SPORTSb | 57% none, 29% meniscectomy, 14% repair | ||||
aDue to rounding, not all percentages total 100%. ACL-SPORTS, Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports; BMI, body mass index; BPTB, bone–patellar tendon–bone autograft; DE-Oslo, Delaware-Oslo; MOON, Multicenter Orthopaedic Outcomes Network.
b,cPost hoc comparisons within each group are denoted by superscripts. There are significant differences (P < .05) for each variable between cohorts marked b and c. There is no significant difference between unmarked or similarly marked cohorts.
TABLE 2.
All 2-Year Functional Outcomes Differed Across Groupsa
| Variable | Cohort | n | Mean | SD | ANOVA P Value |
|---|---|---|---|---|---|
| Marx | MOONb | 431 | 10.6 | 5.1 | .008 |
| DE-Oslob,c | 19 | 12.5 | 2.7 | ||
| ACL-SPORTSc | 24 | 13.5 | 3.3 | ||
| IKDC | MOONb | 430 | 83.6 | 13.9 | <.001 |
| DE-Osloc | 39 | 91.7 | 8.6 | ||
| ACL-SPORTSc | 24 | 95.9 | 6.8 | ||
| KOOS Pain | MOONb | 431 | 90.4 | 10.3 | <.001 |
| DE-Osloc | 30 | 94.4 | 9.4 | ||
| ACL-SPORTSc | 24 | 97.9 | 3.9 | ||
| KOOS Symptoms | MOONb | 431 | 83.4 | 14.0 | <.001 |
| DE-Osloc | 30 | 89.6 | 9.4 | ||
| ACL-SPORTSc | 24 | 93.5 | 6.3 | ||
| KOOS ADL | MOONb | 430 | 95.7 | 7.1 | .002 |
| DE-Osloc | 30 | 98.8 | 4.2 | ||
| ACL-SPORTSc | 24 | 99.8 | 0.5 | ||
| KOOS Sports/Rec | MOONb | 430 | 81.6 | 17.1 | .001 |
| DE-Oslob,c | 30 | 86.0 | 15.4 | ||
| ACL-SPORTSc | 24 | 94.4 | 7.6 | ||
| KOOS QoL | MOONb | 431 | 76.3 | 18.7 | .004 |
| DE-Oslob | 30 | 78.3 | 17.6 | ||
| ACL-SPORTSc | 24 | 89.1 | 13.9 |
aAll mean and SD values are expressed as percentages. ACL-SPORTS, Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports; ADL, Activities of Daily Living (KOOS subscale); ANOVA, analysis of variance; DE-Oslo, Delaware-Oslo; IKDC, International Knee Documentation Committee Subjective Knee Evaluation Form; KOOS, Knee injury and Osteoarthritis Outcome Score; Marx, Marx activity rating scale; MOON, Multicenter Orthopaedic Outcomes Network cohort; QoL, Knee-Related Quality of Life (KOOS subscale); Sports/Rec, Sports and Recreation (KOOS subscale).
b,cPost hoc comparisons within each group are denoted by superscripts. There are significant differences (P < .05) for each variable between cohorts marked b and c. There is no significant difference between unmarked or similarly marked cohorts.
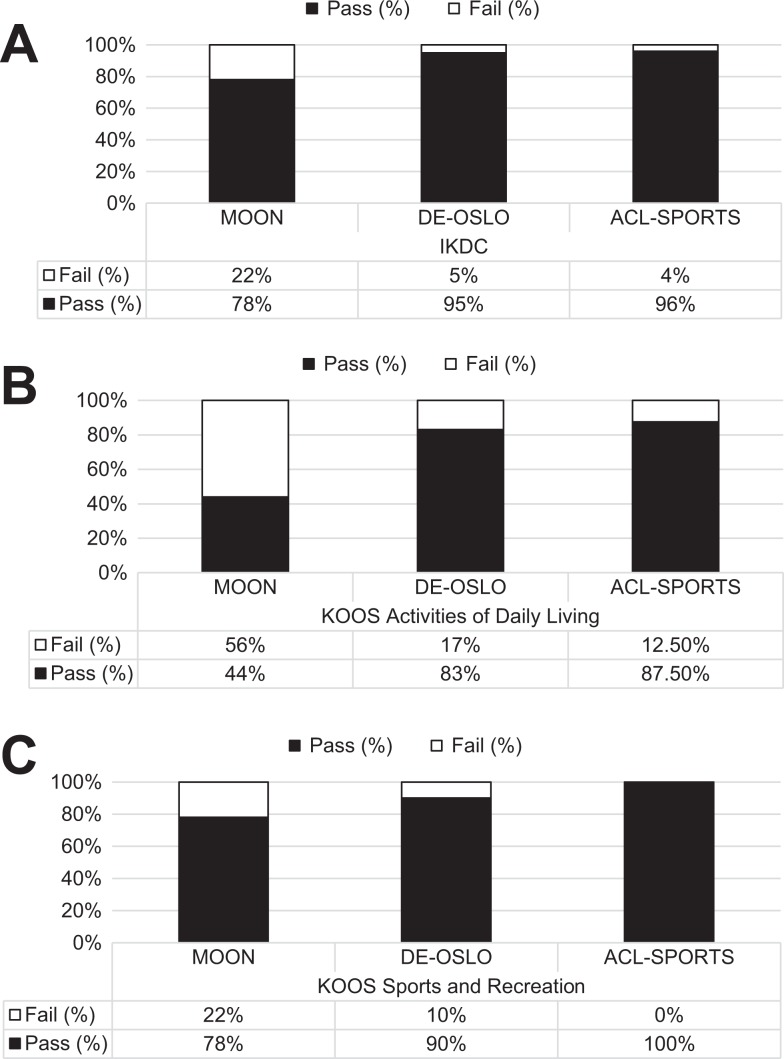
Significant differences were found in proportions of participants who met or exceeded (“pass”) versus fell below (“fail”) the PASS34 scores for the IKDC, KOOS ADL, and KOOS Sports/Rec (Figure 2). A lower proportion of MOON participants passed the IKDC PASS cutoff compared with participants in both the Delaware-Oslo (P = .012) and the ACL-SPORTS (P = .038) cohorts. A lower proportion of MOON participants passed the cutoff score for the KOOS ADL subscale PASS compared with both the Delaware-Oslo (P < .001) and ACL-SPORTS (P < .001) cohort participants. A higher proportion of ACL-SPORTS participants passed the KOOS Sports/Rec PASS score versus the proportion of MOON participants who passed (P = .004). No other statistically significant between-group differences were found.
Figure 2.
Proportions of individuals who met Patient Acceptable Symptom State34 scores differed across groups for the (A) International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC) (P = .003), (B) Knee injury and Osteoarthritis Outcome Score (KOOS) Activities of Daily Living (P < .001), and (C) KOOS Sports and Recreation (P = .011). ACL-SPORTS, Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports cohort; DE-OSLO, Delaware-Oslo cohort; MOON, Multicenter Orthopaedic Outcomes Network cohort.
Discussion
This study had 2 main objectives: first, to assess the primary clinical 1- and 2-year outcomes among female athletes in the ACL-SPORTS randomized controlled trial; and, second, to compare 2-year functional outcomes and activity levels among young female athletes who completed a formal RTS training program after ACLR (the ACL-SPORTS cohort) to homogeneous subsets of 2 existing gold-standard ACL cohorts, Delaware-Oslo and MOON. The key findings were that (1) SAPP and SAPP + PERT training resulted in very high but comparable quadriceps strength, hop test LSI, functional outcomes, activity levels, and RTS rates 2 years after ACLR; and (2) 10 sessions of postoperative RTS training, compared with criterion-based postoperative rehabilitation alone, led to statistically significant and clinically meaningful differences in 2-year functional outcomes among young female athletes after ACLR. The first hypothesis, that the addition of perturbation training would result in superior clinical and functional outcomes, was not supported. The second hypothesis, that the addition of a structured RTS training program would improve outcomes over existing cohorts, was supported. The findings suggest that adding a postoperative RTS training program, incorporating strengthening, agilities, and plyometrics but not necessarily perturbation training, may improve functional outcomes and activity levels among young female athletes after ACLR.
The overwhelming majority of participants in the ACL-SPORTS cohort achieved the PASS thresholds for patients after ACLR,34 indicating a high likelihood of satisfaction with their postoperative outcomes. Muller and colleagues34 recently identified PASS threshold scores with sensitivity and specificity values for the IKDC and each KOOS subscale for patients 1 to 5 years after ACLR. The most specific measure was the IKDC, where a score of 75.9 yielded 96% specificity and 83% sensitivity, whereas the most sensitive measure was the KOOS Sports/Rec subscale threshold of 75.0 (88% specificity, 87% sensitivity).34 In the present study, 96% and 100% of participants in the ACL-SPORTS cohort achieved the thresholds for the IKDC and KOOS Sports/Rec, respectively. In contrast, 95% of Delaware-Oslo and 78% of MOON participants achieved the IKDC PASS threshold, and 90% of the Delaware-Oslo and 78% of MOON cohorts met the KOOS Sports/Rec PASS threshold. Postoperative RTS training may lead to a greater likelihood of successful outcomes among young female athletes after ACLR.
The findings provide a strong model for improving outcomes after ACLR without imposing additional rehabilitation costs, a growing concern in our health care system.29,37,52 Given that perturbation training provided no additional benefit, the common elements of the RTS training protocol (Table 3), including strength, agility, and plyometric exercises, are likely the only critical components of the training regimen. These critical components include basic strength and conditioning exercises that could be performed within a group setting or under the supervision of a variety of professionals, including athletic trainers and strength and conditioning coaches. The critical components do not require a physical therapist or other rehabilitation specialist. Future studies should explore the effectiveness of delivering the strength, agility, and plyometric exercise components using different models of supervision in various settings outside the confines of a physical therapy clinic.
TABLE 3.
Common Elements of the RTS Training Program Performed by Participants in the ACL-SPORTS Cohorta
| Exercise | Sets × Repetitions | Notes/Progressions |
|---|---|---|
| Nordic hamstrings | 2 × 5 | Progress depth from 30° initially to 60° over the course of 10 sessions. |
| Standing squat | 3 × 10 | Perform bilaterally to 90° of knee flexion; add resistance band around knees after first session and progress resistance of band during later sessions; not performed during sessions 7-10 (replaced by tuck jumps). |
| Drop jump | 3 × 10 | Progress height of box (10 cm, 15 cm, 20 cm); begin taking off bilaterally and landing bilaterally, progressing to unilateral (involved limb) landing and then unilateral takeoff and landing on the involved limb only over the course of 10 sessions. |
| Triple single-legged hop | 10-15 × 3 hops each direction for each condition | Sessions 1-3: 10 × 3 hops forward/backward, 10 × 3 hops side to side, over flat ground. Sessions 4-6: 15 × 3 hops forward/backward, 15 × 3 hops side to side, over low (∼5 cm) object (eg, cup or low cone). Sessions 7-10: 15 × 3 hops forward/backward, 15 × 3 hops side to side, over higher object appropriate to athlete (eg, 10-cm cones or 15-cm hurdles). |
| Tuck jumps | 2 or 3 × 10-30 s | Perform during sessions 7-10; progress from 2 sets of 10-20 s to 3 sets of 20-30 s. |
| Agility drills | 3 or 4 drills per session | Progress gradually from 50% to 100% effort over the 10 training sessions; agility drills include forward/backward running, side shuffles, carioca, figure-of-8 around cones, circles around cones, and 90° turns around cones. |
aACL-SPORTS, Anterior Cruciate Ligament Specialized Post-Operative Return-to-Sports; RTS, return to sport.
The ACL-SPORTS protocol also yielded exceptionally high RTS rates, far superior to those previously reported in the literature. According to a 2014 systematic review by Ardern et al,4 75% of female athletes return to sport after ACLR, and just 52% of women return to their preinjury level of sport after ACLR. In stark contrast, 100% (39/39) of female athletes in the ACL-SPORTS trial returned to sport by 2 years after ACLR, including 87% (34/39) who returned to their preinjury level. Female athletes in the ACL-SPORTS cohort were required to meet stringent, objective criteria,1 including at least 90% quadriceps strength index and hop test LSI,36 in order to be cleared by their physical therapist to return to sport.49 Completing the ACL-SPORTS postoperative RTS training program, which is informed by these criteria,1,23,49 likely facilitated the very high functional performance and RTS rates observed in the ACL-SPORTS participants.
Strengths of the present study include that it was the first to compare (1) RTS training with and without perturbation training on medium-term outcomes in female athletes after ACLR and (2) the addition of a supplementary, postoperative RTS training program versus criterion-based postoperative rehabilitation alone, the current standard of care for patients after ACLR. The present study used homogeneous subsets of 2 highly successful cohorts17,18,22 who received quality, criterion-based postoperative rehabilitation for comparison. The findings also provide a prototype for RTS training that could be implemented in a variety of settings, making its inclusion into standard of care quite feasible.
Limitations should be considered when interpreting the results of the study. A cohort design was used to evaluate RTS training compared with postoperative rehabilitation alone and in combination with extended preoperative rehabilitation, such that cause and effect cannot be determined, and the numbers of participants in each cohort differed greatly. Surgeons and physical therapists also varied across and within studies. Baseline differences in factors such as motivation, function, or activity levels could have affected the findings, but preoperative data are not available for the participants of the ACL-SPORTS trial. Athletes were required to meet objective criteria prior to enrollment in the ACL-SPORTS trial, but the criteria are consistent with the criterion-based rehabilitation programs followed by the athletes in the MOON and Delaware-Oslo cohorts.1,50 The ACL-SPORTS enrollment criteria are basic clinical measures, well below those recommended or supported for RTS clearance.1,11,23,30,41,49 Moreover, only 8 of 147 (5%) women who were screened were deemed ineligible because they were unable to resolve these impairments; thus, it is unlikely that requiring patients to achieve these basic clinical milestones dramatically affected the findings. Another consideration is that the comparative analysis included only high-level, female athletes age 13 to 24 years; thus, the findings may not be generalizable to other individuals. The study cohorts, however, were well-matched by age and preinjury sport level, and they address a subset of individuals who are at particularly high risk for poor outcomes after ACLR4,10,16,21,25,38–40,46; this limitation, therefore, may also be a strength. Additionally, no differences were found between men and women on quadriceps strength index, hop tests, or patient-reported outcomes immediately following completion of the ACL-SPORTS training protocol.7 Future studies should evaluate the comparative effectiveness of postoperative RTS training in various settings using randomized controlled trials.
Conclusion
We found that 10 sessions of postoperative RTS training (ACL-SPORTS), compared with criterion-based postoperative rehabilitation alone (MOON), provided clinically meaningful, higher 2-year functional outcomes among young level 1 and level 2 female athletes after primary ACLR. RTS training also led to superior knee-related quality of life compared with extended preoperative plus postoperative rehabilitation (Delaware-Oslo).
Acknowledgment
The authors thank Kathleen Cummer, Amelia J.H. Arundale, Elizabeth Wellsandt, and Hege Grindem for their assistance with data collection; Martha Callahan and the Delaware Rehabilitation Institute for assistance with participant recruitment and retention; the University of Delaware Physical Therapy Clinic; and all participants for their involvement in this work.
Appendix
TABLE A1.
Participant Demographics Between the SAPP and SAPP + PERT Groupsa
| Variable | SAPP (n = 20) | SAPP + PERT (n = 19) | P Value |
|---|---|---|---|
| Age, y | 18.9 ± 5.8 | 19.0 ± 8.8 | .986 |
| Time from surgery to enrollment, wk | 24.8 ± 7.8 | 26.2 ± 8.9 | .621 |
| Weight, kg | 68.8 ± 10.9 | 67.9 ± 14.3 | .820 |
| Height, m | 1.65 ± .06 | 1.65 ± .08 | .827 |
| BMI, kg/m2 | 25.3 ± 3.3 | 24.7 ± 3.9 | .631 |
| Graft type | 4 allo, 8 BPTB, 8 hamstring | 1 allo, 8 BPTB, 10 hamstring | .368 |
| Mechanism of injury | 14 noncontact, 6 contact | 14 noncontact, 5 contact | .798 |
| Preinjury sport level | 19 were level 1; 1 was level 2 | 15 were level 1; 4 were level 2 | .182 |
| Concomitant medial meniscal treatment | 11 none, 4 partial meniscectomy, 2 repair, 3 no data | 12 none, 4 partial meniscectomy, 1 repair, 1 rasping, 1 no data | .671 |
| Concomitant lateral meniscal treatment | 8 none, 7 partial meniscectomy, 2 repair, 3 no data | 12 none, 5 partial meniscectomy, 1 repair, 1 no data | .486 |
aValues are presented as mean ± SD for continuous variables and as patient numbers for other variables. Allo, allograft; BPTB, bone–patellar tendon–bone autograft; BMI, body mass index; hamstring, hamstring autograft; SAPP, strength, agility, plyometric, and secondary prevention; SAPP + PERT, SAPP with perturbation training.
TABLE A2.
Results for Quadriceps Strength Index, Hop LSI, Functional Outcome Measures, and the Marx Activity Rating Scale Between the SAPP and SAPP + PERT Groupsa
| Variable | 1 Year | 2 Years | P Value | ||||
|---|---|---|---|---|---|---|---|
| SAPP | SAPP + PERT | SAPP | SAPP + PERT | Interaction | Time | Group | |
| Quadriceps index, % | 94 ± 9 | 100 ± 14 | 101 ± 13 | 102 ± 14 | .417 | .194 | .414 |
| Single-hop LSI, % | 98 ± 7 | 100 ± 11 | 97 ± 10 | 101 ± 9 | .616 | .780 | .375 |
| Crossover-hop LSI, % | 99 ± 6 | 97 ± 8 | 101 ± 6 | 97 ± 8 | .612 | .536 | .181 |
| Triple-hop LSI, % | 101 ± 5 | 97 ± 4 | 100 ± 5 | 99 ± 6 | .260 | .684 | .188 |
| 6-m timed hop LSI, % | 103 ± 5 | 102 ± 4 | 98 ± 7 | 100 ± 5 | .313 | .006 | .725 |
| KOS-ADLS | 97 ± 4 | 97 ± 4 | 98 ± 3 | 98 ± 3 | .888 | .213 | .648 |
| Global rating | 94 ± 8 | 94 ± 9 | 98 ± 4 | 97 ± 4 | .662 | <.001 | .940 |
| IKDC | 92 ± 9 | 92 ± 8 | 97 ± 6 | 95 ± 9 | .426 | .043 | .744 |
| KOOS Pain | 96 ± 4 | 95 ± 5 | 98 ± 4 | 97 ± 4 | .901 | .007 | .400 |
| KOOS Symptom | 92 ± 6 | 88 ± 8 | 92 ± 10 | 92 ± 7 | .177 | .178 | .404 |
| KOOS ADL | 99 ± 1 | 99 ± 2 | 99 ± 2 | 100 ± 1 | .388 | .388 | .840 |
| KOOS Sports/Rec | 96 ± 9 | 90 ± 10 | 98 ± 4 | 93 ± 9 | .897 | .164 | .081 |
| KOOS QoL | 78 ± 14 | 80 ± 14 | 88 ± 15 | 89 ± 15 | .910 | <.001 | .764 |
| Marx | 11.7 ± 2.4 | 13.0 ± 4.9 | 13.9 ± 3.0 | 13.2 ± 3.5 | .186 | .109 | .783 |
aValues for 1-year and 2-year results are presented as mean ± SD. No main effects of group or interaction effects of Group × Time were found; however, main effects of time were found for the 6-m timed hop, IKDC, KOOS Pain, and KOOS QoL. There were 13 SAPP and 13 SAPP + PERT participants for quadriceps index, 12 SAPP and 12 SAPP + PERT participants for each hop test, and 14 SAPP and 14 SAPP + PERT participants for each patient-reported outcome measure who had complete data at both 1 and 2 years and who did not sustain a reinjury and were thus included in the primary analyses (2 × 2 analyses of variance). ADL, Activities of Daily Living; IKDC, International Knee Documentation Committee Subjective Knee Evaluation Form; KOOS, Knee injury and Osteoarthritis Outcome Score; KOS-ADLS, Knee Outcome Survey–Activities of Daily Living Subscale; LSI, Limb Symmetry Index; Marx, Marx activity rating scale; QoL, Knee-Related Quality of Life; SAPP, strength, agility, plyometric, and secondary prevention; SAPP + PERT, SAPP with perturbation training; Sports/Rec, Sports and Recreation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding provided by the National Institutes of Health: NIH/NIAMS Grant No. R01 AR048212 (L.S.-M.) for the ACL-SPORTS trial; NIH/NICHD Grant No. R37 HD037985 (L.S.-M.) for the Delaware-Oslo Cohort; NIH/NIAMS Grant No. R01 AR053684 (K.P.S.) for the MOON Cohort; and NIH/NICHD Grant No. F30 HD096830 (J.J.C.) for the NRSA predoctoral fellowship award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. J.J.C.’s work was supported in part by the Foundation for Physical Therapy Promotion of Doctoral Studies, Level I and Level II Scholarships. K.P.S. has received consulting fees from Cytori, the National Football League, and Mitek; research support from Smith & Nephew Endoscopy and DonJoy Orthopaedics; and hospitality payments from DePuy and Biosense Webster. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Delaware and Vanderbilt University Human Research Protections Program.
References
- 1. Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–530. [DOI] [PubMed] [Google Scholar]
- 3. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 5. Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. Am J Sports Med. 1995;23(6):694–701. [DOI] [PubMed] [Google Scholar]
- 6. Arundale A, Capin JJ, Zarzycki R, Smith AH, Snyder-Mackler L. Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-SPORTS). Int J Sports Phys Ther. 2018;13(3):422–431. [PMC free article] [PubMed] [Google Scholar]
- 7. Arundale AJH, Capin JJ, Zarzycki R, Smith AH, Snyder-Mackler L. Outcomes improve over the course of rehabilitation: a secondary analysis of the ACL-SPORTS trial. Sports Health. 2018;10(5):441–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arundale AJH, Cummer K, Capin JJ, Zarzycki R, Snyder-Mackler L. Report of the clinical and functional primary outcomes in men of the ACL-SPORTS trial: similar outcomes in men receiving secondary prevention with and without perturbation training 1 and 2 years after ACL reconstruction. Clin Orthop Relat Res. 2017;475(10):2523–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. [DOI] [PubMed] [Google Scholar]
- 10. Brophy RH, Schmitz L, Wright RW. et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Capin JJ, Behrns W, Thatcher K, Arundale A, Smith AH, Snyder-Mackler L. On-ice return-to-hockey progression after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2017;47(5):324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Capin JJ, Khandha A, Zarzycki R. et al. Gait mechanics and tibiofemoral loading in men of the ACL-Sports randomized control trial. J Orthop Res. 2018;36(9):2364–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Capin JJ, Zarzycki R, Arundale A, Cummer K, Snyder-Mackler L. Report of the primary outcomes for gait mechanics in men of the ACL-SPORTS trial: secondary prevention with and without perturbation training does not restore gait symmetry in men 1 or 2 years after ACL reconstruction. Clin Orthop Relat Res. 2017;475(10):2513–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Capin JJ, Zarzycki R, Ito N. et al. Gait mechanics in women of the ACL-SPORTS randomized control trial: interlimb symmetry improves over time regardless of treatment group [published online May 1, 2019]. J Orthop Res. doi:10.1002/jor.24314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22:632–644. [DOI] [PubMed] [Google Scholar]
- 16. Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Failla M, Logerstedt D, Grindem H. et al. Corrigendum. Am J Sports Med. 2017;45(5):NP9.28267929 [Google Scholar]
- 18. Failla MJ, Logerstedt DS, Grindem H. et al. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? A comparative effectiveness study between the MOON and Delaware-Oslo ACL cohorts. Am J Sports Med. 2016;44(10):2608–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fitzgerald GK, Axe M, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30(4):194–203. [DOI] [PubMed] [Google Scholar]
- 20. Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physically active individuals. Phys Ther. 2000;80(2):128–140. [PubMed] [Google Scholar]
- 21. Gans I, Retzky JS, Jones LC, Tanaka MJ. Epidemiology of recurrent anterior cruciate ligament injuries in National Collegiate Athletic Association sports: the Injury Surveillance Program, 2004-2014. Orthop J Sports Med. 2018;6(6):2325967118777823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015;49(6):385–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. [DOI] [PubMed] [Google Scholar]
- 25. Hurd WJ, Axe MJ, Snyder-Mackler L. Influence of age, gender, and injury mechanism on the development of dynamic knee stability after acute ACL rupture. J Orthop Sports Phys Ther. 2008;38(2):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Irrgang JJ, Anderson AF, Boland AL. et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567–1573. [DOI] [PubMed] [Google Scholar]
- 27. Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–1145. [DOI] [PubMed] [Google Scholar]
- 28. Joreitz R, Lynch A, Rabuck S, Lynch B, Davin S, Irrgang J. Patient-specific and surgery-specific factors that affect return to sport after ACL reconstruction. Int J Sports Phys Ther. 2016;11(2):264–278. [PMC free article] [PubMed] [Google Scholar]
- 29. Kiadaliri AA, Englund M, Stefan Lohmander L, Carlsson KS, Frobell RB. No economic benefit of early knee reconstruction over optional delayed reconstruction for ACL tears: registry enriched randomised controlled trial data. Br J Sports Med. 2016;50(9):558–563. [DOI] [PubMed] [Google Scholar]
- 30. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 31. Logerstedt D, Scalzitti D, Risbery M. et al. Knee stability and movement coordination impairments: knee ligaments sprain revision 2017. J Orthop Sports Phys Ther. 2017;47(11):A1–A47. [DOI] [PubMed] [Google Scholar]
- 32. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1–A37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 34. Muller B, Yabroudi MA, Lynch A. et al. Defining thresholds for the patient acceptable symptom state for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med. 2016;44(11):2820–2826. [DOI] [PubMed] [Google Scholar]
- 35. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. [DOI] [PubMed] [Google Scholar]
- 36. Noyes F, Barber S, Mangine R. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. [DOI] [PubMed] [Google Scholar]
- 37. Núñez M, Sastre S, Núñez E, Lozano L, Nicodemo C, Segur JM. Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort—a randomized trial with 2 years of follow-up. Arthroscopy. 2012;28(7):929–935. [DOI] [PubMed] [Google Scholar]
- 38. Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med. 2017;5(12):2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reid A, Birmingham T, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable valid outcome measure during rehab after ACLR. Phys Ther. 2007;87(3):337–349. [DOI] [PubMed] [Google Scholar]
- 42. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;3(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 44. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after ACL reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Snyder-Mackler L, De Luca PF, Williams PR, Eastlack ME, Bartolozzi A. Reflex inhibition of the quadriceps femoris muscle after injury of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76(4):555–560. [DOI] [PubMed] [Google Scholar]
- 46. Spindler KP, Huston LJ, Wright RW. et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sturgill LP, Snyder-Mackler L, Manal TJ, Axe MJ. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther. 2009;39(12):845–849. [DOI] [PubMed] [Google Scholar]
- 48. Thrush C, Porter TJ, Devitt BM. No evidence for the most appropriate postoperative rehabilitation protocol following anterior cruciate ligament reconstruction with concomitant articular cartilage lesions: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1065–1073. [DOI] [PubMed] [Google Scholar]
- 49. White K, Di Stasi SL, Smith AH, Snyder-Mackler L. Anterior cruciate ligament-specialized post-operative return-to-sports (ACL-SPORTS) training: a randomized control trial. BMC Musculoskelet Disord. 2013;14:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wright RW, Haas AK, Anderson J. et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000-2015. Med J Aust. 2018;208(8):354–358. [DOI] [PubMed] [Google Scholar]
- 52. Zhang JY, Cohen JR, Yeranosian MG. et al. Rehabilitation charges associated with anterior cruciate ligament reconstruction. Sports Health. 2015;7(6):538–541. [DOI] [PMC free article] [PubMed] [Google Scholar]