Abstract
Aims
To evaluate sex‐specific disparities in acute kidney injury (AKI) complicating acute myocardial infarction‐related cardiogenic shock (AMI‐CS) in the United States.
Methods and results
This was a retrospective cohort study from 2000 to 2014 from the National Inpatient Sample (20% sample of all hospitals in the United States). Patients >18 years admitted with a primary diagnosis of AMI and concomitant CS that developed AKI were included. The endpoints of interest were the prevalence, trends, and outcomes of men and women with AKI in AMI‐CS. Multivariable hierarchical logistic regression was used to control for confounding, and a two‐sided P < 0.05 was considered statistically significant. During this 15 year period, 440 257 admissions with AMI‐CS met the inclusion criteria, with AKI noted in 155 610 (35.3%). Women constituted 36.3% of the cohort and were older, of non‐White race, and with higher co‐morbidity compared with men. Women with AKI less often received coronary angiography (59% vs. 66%), percutaneous coronary intervention (39% vs. 43%), mechanical circulatory support (39% vs. 48%), mechanical ventilation (49% vs. 54%), and haemodialysis (9% vs. 10%) compared with men (all P < 0.001). Adjusted in‐hospital mortality was higher in women—odds ratio 1.16 (95% confidence interval 1.14–1.19); P < 0.001—compared with men. Women had shorter lengths of stay (12 ± 14 vs. 13 ± 14 days), lower hospital costs ($150 071 ± 180 796 vs. $181 260 ± 209 674), and were less often discharged to home (19% vs. 31%) (all P < 0.001).
Conclusions
Women with AKI in AMI‐CS received fewer cardiac and non‐cardiac interventions, had higher in‐hospital mortality, and were less often discharged to home compared with men.
Keywords: Cardiogenic shock, Acute myocardial infarction, Acute kidney injury, Sex‐based disparities, Haemodialysis
Introduction
Cardiogenic shock complicating acute myocardial infarction (AMI‐CS) is frequently associated with acute kidney injury (AKI), which has an adverse prognosis.1, 2, 3 In unselected AKI patients, female sex was noted to be associated with lower mortality.4 However, there are limited data on sex‐specific differences in AKI in hospitalized US patients with AMI‐CS.4, 5 Using a 15 year nationally representative US database, this study sought to assess sex‐specific differences in AKI in AMI‐CS. We hypothesized that women with AKI would have higher in‐hospital mortality consistent with other literature in acute care cardiology.6, 7
Methods
The Healthcare Cost and Utilization Project National (Nationwide) Inpatient Sample (HCUP‐NIS) is the largest all‐payer database of hospitalized inpatients in the United States. The HCUP‐NIS contains discharge data from a 20% stratified sample of non‐federal hospitals and can be weighted to estimate national trends and prevalence. In the period from 1 January 2000 through 31 December 2014, a retrospective cohort study of admissions with a primary diagnosis of AMI [International Classification of Disease‐9 Clinical Modification (ICD‐9CM) 410.x] and concomitant secondary diagnosis of CS (ICD‐9CM 785.51) was identified. CS was defined as shock resulting from diminution of cardiac output in heart disease, shock resulting from primary failure of the heart in its pumping function, as in myocardial infarction, severe cardiomyopathy, or mechanical obstruction or compression of the heart, or shock resulting from the failure of the heart to maintain adequate output. Previously validated methodology was used to identify patient, hospital, co‐morbidities, procedures, and outcomes.1, 8, 9, 10 AKI was identified using ICD‐9CM 584 [acute renal failure (ARF)], 584.5 (ARF with tubular necrosis), 584.6 (ARF with renal cortical necrosis), 584.7 (ARF with papillary necrosis), 584.8 (ARF with other pathological lesion), and 584.9 (ARF, unspecified), which has been shown to have a high specificity (98%) and negative predictive value (96%), albeit with low sensitivity (35.4%) and positive predictive value (47.9%).11 Admissions that had prior maintenance dialysis (ICD‐9CM V45.11) were excluded. The Deyo's modification of Charlson Comorbidity Index was used to identify co‐morbid diseases.12 The endpoints of interest were the prevalence, trends, and outcomes of men and women with AKI in AMI‐CS. As recommended by HCUP‐NIS, survey procedures using discharge weights provided with HCUP‐NIS database were used to generate national estimates. Trend weights provided by the HCUP‐NIS were used to re‐weigh the data to adjust for the 2012 HCUP‐NIS redesign.13 χ2 test and t‐test were used to compare categorical and continuous variables, respectively. The inherent restrictions of the HCUP‐NIS database related to research design, data interpretation, and data analysis were reviewed and addressed, such as consideration of each record as an ‘admission’ instead of a patient, no state‐level/hospital‐level estimates, re‐weighing the sample using trend weights (to adjust for 2012 redesign), and citing relevant literature for administrative codes.13 Multivariable hierarchical logistic regression analysis was performed for prevalence and outcomes adjusting for age, co‐morbidity, chronic kidney disease, race, socio‐economic status, hospital characteristics, acute organ failure, cardiac arrest, and cardiac and non‐cardiac interventions. All statistical analyses were performed using SPSS v25.0 (IBM Corp, Armonk, NY).
Results
During this 15 year period, 440 257 admissions with AMI‐CS met the inclusion criteria of which AKI was noted in 155 610 (35.3%). Women comprised 36.3% of the AKI cohort. Acute on chronic kidney disease was present in 23.8% of the total population, with a higher prevalence in men (24.5% vs. 22.5%; P < 0.001). Women with AKI were more likely to be older (74 ± 12 vs. 69 ± 12 years), of non‐White race (38% vs. 36%), bearing Medicare insurance (76% vs. 62%), with higher co‐morbidity (Charlson Comorbidity Index 6 ± 2 vs. 5 ± 2), and with less non‐cardiac organ failure (respiratory 53% vs. 57%, hepatic 16% vs. 17%, neurologic 15% vs. 21%, and cardiac arrest 18% vs. 22%) compared with men (all P < 0.001). Women with AKI less often received coronary angiography (59% vs. 66%), percutaneous coronary intervention (39% vs. 43%), mechanical circulatory support (39% vs. 48%), mechanical ventilation (49% vs. 54%), and haemodialysis (9% vs. 10%) compared with men (all P < 0.001). The 15 year unadjusted and adjusted trends of AKI stratified by sex are presented in Figure 1A,B (P < 0.001 for trend). All‐cause in‐hospital mortality was higher in women—51% vs. 45%; odds ratio 1.28 (95% confidence interval 1.25–1.31); P < 0.001. Unadjusted and adjusted temporal trends of in‐hospital mortality are presented in Figure 1C,D (P < 0.001 for trend). Women had shorter lengths of stay (12 ± 14 vs. 13 ± 14 days), lower hospital costs ($150 071 ± 180 796 vs. $181 260 ± 209 674), were less often discharged to home (19% vs. 31%), and more often discharged to a skilled nursing facility (52% vs. 39%) (all P < 0.001). Adjusting for age, co‐morbidity, chronic kidney disease, race, socio‐economic status, hospital characteristics, acute organ failure, cardiac arrest, and cardiac and non‐cardiac interventions, female sex was an independent predictor of higher in‐hospital mortality [odds ratio 1.16 (95% confidence interval 1.14–1.19); P < 0.001].
Figure 1.
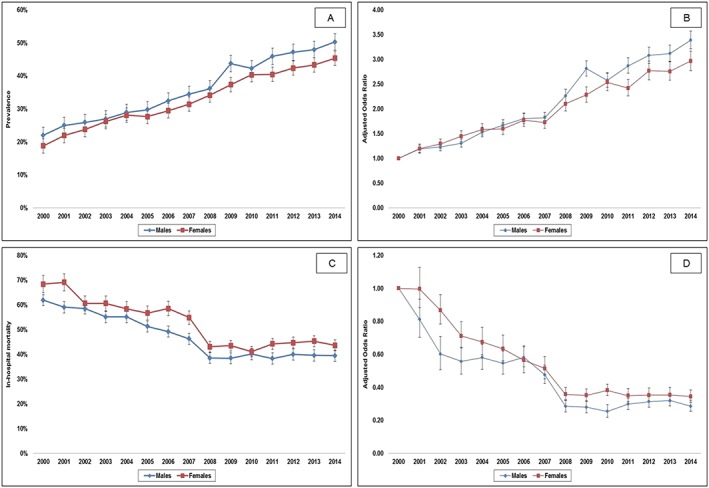
Unadjusted and adjusted 15 year temporal trends for the prevalence and in‐hospital mortality of AKI stratified by sex in AMI‐CS. (A) Unadjusted temporal trends of AKI stratified by sex in AMI‐CS (P < 0.001 for trend); (B) adjusted temporal trends of AKI stratified by sex in AMI‐CS* (P < 0.001 for trend); (C) unadjusted temporal trends in the in‐hospital mortality of AKI stratified by sex in AMI‐CS (P < 0.001 for trend); and (D) adjusted temporal trends of in‐hospital mortality of AKI stratified by sex in AMI‐CS^ (P < 0.001 for trend). *Adjusted for age, race, primary payer, socio‐economic status, hospital location/teaching status, hospital bedsize, hospital region, and co‐morbidity (referent year 2000). ^Adjusted for age, race, primary payer, socio‐economic status, hospital location/teaching status, hospital bedsize, hospital region, co‐morbidity, acute respiratory failure, acute hepatic failure, acute haematologic failure, acute neurologic failure, cardiac arrest, type of AMI, use of coronary angiography, percutaneous coronary intervention, invasive haemodynamic monitoring, mechanical circulatory support, invasive mechanical ventilation, and haemodialysis (referent year 2000). AKI, acute kidney injury; AMI‐CS, acute myocardial infarction‐related cardiogenic shock.
Discussion
In the largest study of AKI complicating AMI‐CS admissions, we noted that despite lower acuity of illness, female sex was independently associated with higher in‐hospital mortality in contrast to what has been reported in the AKI literature assessing all comers.4 Although there has been a significant decrease in in‐hospital mortality between 2000 and 2014, AKI still, not unsurprisingly, was associated with high mortality in AMI‐CS. Female patients consistently received fewer cardiac and non‐cardiac procedures and were discharged to assisted care more often in comparison with male patients.
There are no prior studies looking at sex‐specific differences in AKI in AMI‐CS, and therefore, we were unable to compare this study with prior literature directly. We did note that there remain significant sex‐specific disparities in the management and outcomes of AMI‐CS independent of other risk factors.14 It is possible that women, who were older as a group, had delays in diagnosis of AKI because of lower muscle mass.15 However, the differences remained significant despite adjusting for age. Our results are consistent with prior European studies that demonstrated that women developed AKI less often and had higher in‐hospital mortality than men.2, 3 Despite the increasing prevalence of AKI, our data revealed that in‐hospital mortality declined over time, which was likely because of greater recognition and awareness in AMI‐CS management.1 Furthermore, judicious use of contrast media, increased AKI awareness, and avoidance of nephrotoxic agents may influence mortality because of their detrimental effect on renal function.5 The reasons for these disparities are incompletely understood. Prior data have noted that women present later with AMI, have more atypical symptoms, and receive guideline‐directed medical therapy less often.7 Furthermore, differences in cultural and religious beliefs, treatment preferences, and incomplete knowledge may present additional barriers for timely and guideline‐directed care in women. Further qualitative studies evaluating patient and provider beliefs and biases on sex‐specific care of AKI in AMI‐CS are warranted.
This study has several limitations. It is possible that the higher occurrence of AKI over the years is related to greater recognition and improved coding practices.16 A minority of the included admissions may have had creatinine elevations without AKI (i.e. no tubular injury). Haemodynamic and fluid balance parameters, which influence the development of AKI, were not available in this administrative database.3 Unfortunately, the administrative data used in this study do not provide information related to the serum creatinine level or urine output for appropriate adjudication of AKI cases based on the current definition criteria. ICD9‐CM codes for AKI are known to be very specific while having low sensitivity. Knowing that AKI cases described in this paper are mostly patients with real AKI, we believe our results still provide valuable information.17, 18 The reasons for not obtaining cardiac and non‐cardiac organ support therapies because of treatment‐limiting decisions could not be assessed in this administrative database.
In conclusion, in this 15 year study, women had AKI less frequently in AMI‐CS compared with men. Women with AKI tended to be older, of non‐white race, and with higher co‐morbidity but developed less frequent organ dysfunction. Women received fewer cardiac and non‐cardiac interventions, had higher in‐hospital mortality, and were less often discharged to home.
Conflict of interest
A.S.J. presently or has in the past consulted for most of the major diagnostic companies. All other authors report no financial or intellectual conflicts of interest related to this manuscript.
Author contributions
S.V., L.Y., S.M.D., S.V., S.V., and P.R.S. performed the study design, literature review, data analysis, and statistical analysis. S.V., L.Y., S.V., S.V., and P.R.S. performed the data management, data analysis, and drafting the manuscript. S.V., L.Y., S.M.D., S.V., S.V., P.R.S., A.S.J., B.J.G., and K.K. have access to the data. S.M.D., A.S.J., B.J.G., and K.K. performed the manuscript revision, intellectual revisions, and mentorship. S.V., L.Y., S.M.D., S.V., S.V., P.R.S., A.S.J., B.J.G., and K.K. gave the final approval.
Funding
None declared.
Vallabhajosyula S., Ya'Qoub L., Dunlay S. M., Vallabhajosyula S., Vallabhajosyula S., Sundaragiri P. R., Jaffe A. S., Gersh B. J., and Kashani K. (2019) Sex disparities in acute kidney injury complicating acute myocardial infarction with cardiogenic shock, ESC Heart Failure, 6, 874–877. 10.1002/ehf2.12482.
References
- 1. Vallabhajosyula S, Dunlay SM, Prasad A, Kashani K, Sakhuja A, Gersh BJ, Jaffe AS, Holmes DR, Barsness GW. Acute noncardiac organ failure in acute myocardial infarction with cardiogenic shock. J Am Coll Cardiol 2019; 73: 1781–1791. [DOI] [PubMed] [Google Scholar]
- 2. Lauridsen MD, Gammelager H, Schmidt M, Rasmussen TB, Shaw RE, Botker HE, Sorensen HT, Christiansen CF. Acute kidney injury treated with renal replacement therapy and 5‐year mortality after myocardial infarction‐related cardiogenic shock: a nationwide population‐based cohort study. Crit Care 2015; 19: 452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tarvasmaki T, Haapio M, Mebazaa A, Sionis A, Silva‐Cardoso J, Tolppanen H, Lindholm MG, Pulkki K, Parissis J, Harjola VP, Lassus J, Investigators CSS. Acute kidney injury in cardiogenic shock: definitions, incidence, haemodynamic alterations, and mortality. Eur J Heart Fail 2018; 20: 572–581. [DOI] [PubMed] [Google Scholar]
- 4. Neugarten J, Golestaneh L, Kolhe NV. Sex differences in acute kidney injury requiring dialysis. BMC Nephrol 2018; 19: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Amin AP, Salisbury AC, McCullough PA, Gosch K, Spertus JA, Venkitachalam L, Strolker JM, Parikh CR, Masoudi FA, Jones PG, Kosiborod M. Trends in the incidence of acute kidney injury in patients hospitalized with acute myocardial infarction. Arch Intern Med 2012; 172: 246–253. [DOI] [PubMed] [Google Scholar]
- 6. Nehme Z, Andrew E, Bernard S, Smith K. Sex differences in the quality‐of‐life and functional outcome of cardiac arrest survivors. Resuscitation 2019; 137: 21–28. [DOI] [PubMed] [Google Scholar]
- 7. Liakos M, Parikh PB. Gender disparities in presentation, management, and outcomes of acute myocardial infarction. Curr Cardiol Rep 2018; 20: 64. [DOI] [PubMed] [Google Scholar]
- 8. Vallabhajosyula S, Arora S, Lahewala S, Kumar V, Shantha GPS, Jentzer JC, Stulak JM, Gersh BJ, Gulati R, Rihal CS, Prasad A, Deshmukh AJ. Temporary mechanical circulatory support for refractory cardiogenic shock before left ventricular assist device surgery. J Am Heart Assoc 2018; 7: e010193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vallabhajosyula S, Arora S, Sakhuja A, Lahewala S, Kumar V, Shantha GPS, Egbe AC, Stulak JM, Gersh BJ, Gulati R, Rihal CS, Prasad A, Deshmukh AJ. Trends, predictors, and outcomes of temporary mechanical circulatory support for postcardiac surgery cardiogenic shock. Am J Cardiol 2019; 123: 489–497. [DOI] [PubMed] [Google Scholar]
- 10. Vallabhajosyula S, Dunlay SM, Kashani K, Vallabhajosyula S, Vallabhajosyula S, Sundaragiri PR, Jaffe AS, Barsness GW. Temporal trends and outcomes of prolonged invasive mechanical ventilation and tracheostomy use in acute myocardial infarction with cardiogenic shock in the United States. Int J Cardiol 2019; 285: 6–10. [DOI] [PubMed] [Google Scholar]
- 11. Waikar SS, Wald R, Chertow GM, Curhan GC, Winkelmayer WC, Liangos O, Sosa MA, Jaber BL. Validity of international classification of diseases, ninth revision, clinical modification codes for acute renal failure. J Am Soc Nephrol 2006; 17: 1688–1694. [DOI] [PubMed] [Google Scholar]
- 12. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases. J Clin Epidemiol 1992; 45: 613–619. [DOI] [PubMed] [Google Scholar]
- 13. Khera R, Krumholz HM. With great power comes great responsibility: big data research from the national inpatient sample. Circ Cardiovasc Qual Outcomes 2017; 10: e003846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fengler K, Fuernau G, Desch S, Eitel I, Neumann FJ, Olbrich HG, de Waha A, de Waha S, Richardt G, Hennersdorf M, Empen K, Hambrecht R, Fuhrmann J, Böhm M, Poess J, Strasser R, Schneider S, Schuler G, Werdan K, Zeymer U, Thiele H. Gender differences in patients with cardiogenic shock complicating myocardial infarction: a substudy of the IABP‐SHOCK II‐trial. Clin Res Cardiol 2015; 104: 71–78. [DOI] [PubMed] [Google Scholar]
- 15. Coca SG. Acute kidney injury in elderly persons. Am J Kidney Dis 2010; 56: 122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Siew ED, Davenport A. The growth of acute kidney injury: a rising tide or just closer attention to detail? Kidney Int 2015; 87: 46–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Kashyap R, Kashani K, Jentzer JC. Clinical profile and outcomes of acute cardiorenal syndrome type‐5 in sepsis: an eight‐year cohort study. PLoS One 2018; 13: e0190965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: a narrative review. J Crit Care 2018; 43: 122–127. [DOI] [PubMed] [Google Scholar]


