Abstract
Background
The objective of the study was to analyze the quality control of the treatment within the orthodontic department by determining the workload, type of treatment, and quality of outcome.
Method
Two hundred eighty patients were selected from departmental archives, who underwent orthodontic treatment since January 2010 and assessed using index of complexity, outcome and treatment need. Descriptive statistics was performed by SPSS, version 21 (IBM, USA). Mann–Whitney U test was applied to assess the difference between complexity and improvement grade.
Result
Orthodontic treatment was provided to 56.43% of female and 43.57% male patients with a mean age of 16.91 years. Angle's class I type malocclusion was the highest with 35.71%. Preadjusted edgewise metal appliance with 95% dominated the mechanics. About 12.14% and 3.57% patients got benefited with myofunctional and orthopedic treatment, respectively. Ten percent of patients were treated with orthognathic surgery. The mean duration of treatment was 31.19 months with a range of minimum of 17 months to a maximum of 46 months. Among 87.14% patients treated by faculty, 47.95% had difficult complexity grading and 22.95% had very difficult complexity grading. Residents had provided treatment with 63.88% difficult and 19.44% very difficult grade. Mann–Whitney U test of overall complexity and improvement grade showed Z score of −9.25715 which was highly significant.
Conclusion
The present study concludes that fair quality control is being maintained by the department considering the number of patients, its severity, and excellent outcomes. However, being the premier institute of Indian Armed Forces, regular clinical audit should be conducted to fulfill demand and supply ratio in appropriation.
Keywords: Clinical audit, Malocclusion, Orthodontics
Introduction
Clinical audit is a systematic method to assess whether the stated goal is being reached and identifies area of improvement. Therefore, it is imperative to assess patients load, treatment facilities, available inventories, and quality of results.
The Tertiary Military Dental Centre, with its inception since 2000, is providing free dental care from basic to advanced treatment to serving and retired Armed Force personnel and their dependents and other referral patients from the entire Indian Armed Forces dental centers. Orthodontic department, in particular, provides comprehensive orthodontic care from fixed and removable orthodontic mechanotherapy to various growth modification and surgical orthodontic treatments, which includes distraction osteogenesis and obstructive sleep apnea treatment as well.
This Tertiary Military Dental Centre also runs 3-year postgraduate program for serving officers as "Master in Dental Surgery" in Orthodontics, making it one of the few institutions of Indian Armed Forces to provide such high class educational facilities.
Kamat et al.1 reported a retrospective audit of orthodontic treatment need and outcome of adults in Army Dental Centre (R & R) and showed that larger number of adults treated at the center belonged to severe handicapping malocclusion. Various indices available to ascertain handicapping and output of treatment in orthodontics include index of orthodontic treatment need (IOTN), peer assessment rating (PAR) index, dental esthetic index (DAI), and index of complexity, outcome and treatment need (ICON).2, 3, 4
Brook et al. devised IOTN as a result of a government initiative of the United Kingdom in 1989. It had proposed to determine the likely impact of a malocclusion on an individual's dental health and psychosocial well-being.2 It consisted of dental health component and esthetic component. The single worst feature of a malocclusion is weighted and categorized into one of the five different grades depicting the need for treatment. However, there is no provision of assessment of treatment outcome in IOTN.
Richmond et al.3 developed the PAR index to evaluate the success or failure of orthodontic treatment. A number of variables are recorded as scores, before and at the end of treatment, using study models. Its scores are cumulative, and the malocclusion was recorded and multiplied by different numbers. The difference between the PAR scores at the start and on completion of treatment can be measured in percentage and reflects the success or failure of treatment.
Because IOTN only helps in determining the need of treatment by assessing the severity of malocclusion and PAR index evaluates only the results after treatment, Daniels et al.4 devised the "ICON" to fulfill the requirement of both in one index. ICON is a relatively simple index requiring few occlusal traits and grading system to assess the need, complexity, and outcome with limited instrumentation.
Templeton showed that the suitability of ICONs was comparable to dental health component of IOTN for pretreatment assessment as well as PAR index for post-treatment result evaluation.5 Literature also reports that the ICON had merits over IOTN on interpretation of need and the complexity of malocclusion and assessing their treatment outcomes.6
Because the present institution is the premier institute of Indian Armed Forces, regular clinical audit assessment deemed necessary to fulfill demand and supply in appropriation. Hence, the present study was conducted to analyze the quality control of the orthodontic treatment within the orthodontic department by determining retrospectively, the workload, type of treatment, and quality of outcome of the treatment that had been provided to patients since January 2008 using ICON.
Material and method
The present retrospective observational study was conducted in the Department of Orthodontics of the Tertiary Care Military Dental Centre after taking appropriate clearance from departmental and institutional ethical committee. Samples were collected from patients who had undergone orthodontic treatment from January 2008 till December 2017. Patients with incomplete records or data were excluded from the study. Data were collected from two sources: register for orthodontic treatment and its archives of photographs stored in departmental stand-alone computer and study models before and after orthodontic treatment. ICON was used to assess the workload, complexity of treatment, and its outcomes (Table 1). A total of 280 patients' records (122 males and 158 females) were evaluated (Table 2). The following characteristics of ICON were used for analysis: esthetic, crowding, spacing crossbite, overbite, overjet, and buccal segment relationship.
Table 1.
ICON traits and grade table.
| Traits | 0 | 1 | 2 | 3 | 4 | 5 | Weight |
|---|---|---|---|---|---|---|---|
| Esthetic | Score 1–10 | 7 | |||||
| Upper arch crowding/spacing | <2 mm | 2.1–5 mm | 5.1–9 mm | 9.1–13 mm | 13.1–17 mm | >17 mm | 5 |
| Cros-bite | No crossbite | Crossbite present | – | – | – | 5 | |
| Incisor open bite/overbite | Edge to edge | <1 mm/1/3rd- 2/3rd coverage | 1.1–2 mm/2/3rd coverage | 2.1–4 mm/gully covered | >4 mm | – | 4 |
| Buccal segment | Cusp to embrasure classes I, II, and III | Any cups relation up to but not including cusp to cusp | cusp to cusp | – | – | – | 3 |
| Grades | |||||||
| Complexity grade | Easy (<29) | Mild (29–50) | Moderate (51–63) | Difficult (64–77) | Very difficult (>77) | – | |
| Improvement grade | Greatly (>−1) | Substantially (−25 to −1) | Moderately (−53 to −26) | Minimally (−85 to −54) | No or worse (<−85) | – | |
ICON, index of complexity, outcome and treatment need.
Table 2.
Descriptive Statistics of age, sex, duration, and ICON score.
| Serial no. | Parameters | Value (age and sex) | Value (duration in months) | Pretreatment (ICON score) | Post-treatment (ICON score) |
|---|---|---|---|---|---|
| 1 | Na | 280 | 280 | 280 | 280 |
| 2 | Mean | 16.91 | 31.19 | 69.55 | 16.87 |
| 3 | SD | 4.714 | 7.29 | 18.86 | 4.77 |
| 4 | SEM | 0.393 | 0.61 | 1.57 | 0.40 |
| 5 | 95% CI | 16.14–17.69 | 29.99–32.39 | 66.44–72.66 | 16.08–17.65 |
| 6 | Min | 0.1 | 17 | 25 | 7 |
| 7 | Max | 49 | 46 | 106 | 29 |
| 8 | Male | 122 (43.57%) | |||
| 9 | Female | 158 (56.43%) | |||
CI, confidence interval; ICON, index of complexity, outcome and treatment need; SD, standard deviation; SEM, standard error of the mean.
Sample size.
All the patient's records were analyzed by the primary author (R.M.) by visual inspection and manual measurement method using digital Vernier caliper with the nearest measurement of 0.1 mm. Intraobserver and interobserver's reproducibility were assessed by randomly repeating measurement after 3 weeks by the primary author (R.M.) and coauthors (R.M. and U.K.), respectively.
The grading of pretreatment scores in different levels of complexity was done as follows: easy <29, mild 29–50, moderate 51–63, difficult 64–77, very difficult >77. The post-treatment scores were calculated from the study model taken at the end of the treatment. Summary scores of less than 31 were taken as acceptable outcome.4 (Table 1).
Treatment efficiency and success were evaluated by assessing improvement grade using ICON according to the following formula: Improvement grade = pretreatment score – (4 × post-treatment score). The improvement was graded as follows: greatly improved > −1, substantially improved −25 to −1, moderately improved −53 to −26, minimally improved −85 to −54, not improved or worse < −85.4 (Table 1).
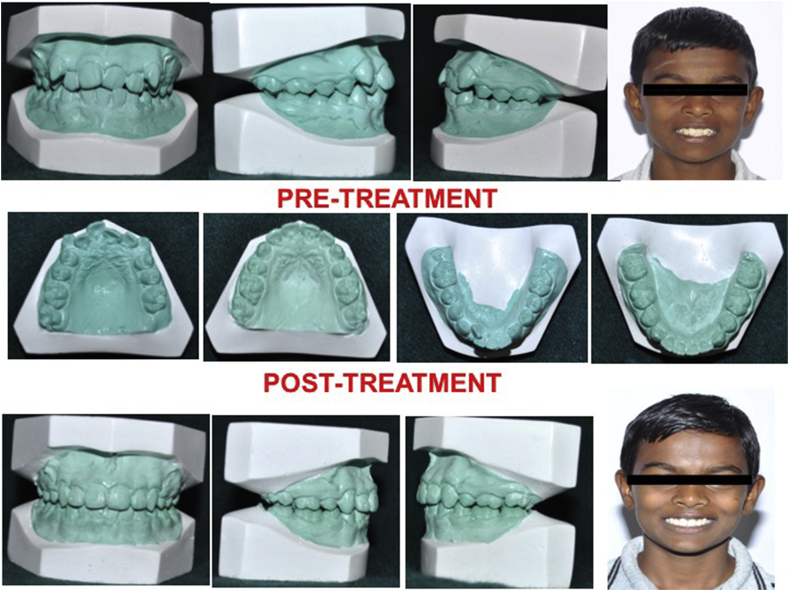
Fig. 1 depicts an example case for the calculation of pretreatment and post-treatment ICON score and grading. Based on study models and clinical photographs, the calculations of ICON score were assessed at T0 i.e., before placement of appliance (Fig. 1). The patient's pretreatment photograph was graded as 6 on the scale of esthetic component, which was multiplied with 7 according to the calculation table. Crowding was graded as 1 (2.1–5 mm), which was multiplied with 5. Crossbite, which was present, was graded as 1 and was multiplied with 5. The open bite was graded as 1 and buccal segment in anteroposterior aspect was graded as 1, and both were multiplied with 4. The total calculated pretreatment ICON score was 60, thereby rated on complexity grade to difficult case as per ICON (<77). At T1, i.e. after completion of treatment, records were reassessed (Fig. 1). Rest of the component were given the score "0’" giving a post-treatment ICON score of 7. Finally, the improvement grade was calculated using the following T0 score − 4 × T1 score.
Fig. 1.
An example case for assessment of ICON. ICON, index of complexity, outcome and treatment need.
Thus, the present case under study showed an improvement grade of 32, i.e. (60 − [4 × 7]), suggestive of a greatly improved outcome (greater than "−1") (Table 1).
Statistical analysis
The database was formulated in MS Excel sheet, and SPSS, version 21 (IBM, USA), software was used for data analysis. Descriptive statistics and frequency distribution of sample was carried out based on age, sex, malocclusion, mechanotherapy, treatment provider, pretreatment and post-treatment ICON score, complexity grade, and improvement grade.7
Application of Shapiro–Wilks test indicated non-normality of data distribution. Therefore, Mann-Whitney U test was used to assess the comparison between complexity and improvement grade, with a two-tailed p value < 0.05 considered as statistically significant. To determine the measurement reliability, the same observer repeated measurements of 30 randomly chosen study models and photographs 3 weeks after the first measurement. Intraclass correlation value of 0.970 indicated excellent intraobserver reliability. The reproducibility of the double determinations for interobserver variability of measurements was expressed using the Dahlberg formula, which showed minimal error (within 0.05 mm) that did not affect the reliability of the measurements.
Result
The present study was a retrospective analysis of the quality control of the orthodontic treatment within the orthodontic department of one of the Apex Dental Centre of Indian Army by determining retrospectively, the workload, type of treatment, and quality of outcome of the treatment that had been provided to patients from January 2010 till December 2017 using ICON. A total of 280 patients were evaluated with ICON.
Frequency distribution of patients: age and sex wise
Among the overall load of the department, 56.43% female and 43.57% male patients had undergone orthodontic treatment. Their mean age was 16.91 years with standard deviation (SD) of approximately 4 years (Table 2).
Duration of orthodontic treatment
The mean duration of orthodontic treatment was 31.19 months with a range of minimum of 17 months to a maximum of 46 months. It had an SD of 7.29 months (Table 2).
Frequency distribution and comparison of pretreatment and post-treatment ICON score in different severity and improvement grades
Pretreatment and post-treatment ICON score had a mean of 69.55 and 16.87, respectively, with a range of 25–106 and 7–29, respectively. Mann-Whitney U test analysis of overall complexity grade and improvement grade showed Z score of −9.25715 which was found to be highly significant considering p < 0.05 (Table 2, Table 7).
Table 7.
Mann–Whitney U test analysis of overall complexity grade and improvement grade.
| Serial no. | Complexity grade | Mean pretreatment ICON score | Improvement grade | Mean post-treatment ICON score |
|---|---|---|---|---|
| 1 | Easy | 25.55 | Greatly improved | 7.72 |
| 2 | Mild | 41.87 | Substantially improved | −11.80 |
| 3 | Moderate | 54.80 | Moderately improved | 0 |
| 4 | Difficult | 72.40 | Minimally improved | 0 |
| 5 | Very difficult | 94.50 | No improvement/worsening | 0 |
Mann–Whitney U test showed a Z-score of −9.25715.
The result is significant as the value is less than p < 0.05.
ICON, index of complexity, outcome and treatment need.
Frequency distribution of patients: malocclusion
Among the analyzed sample, Angle's class I type 2 malocclusion, i.e., bimaxillary protrusion, was found to be the highest with 35.71%, followed by 24.28% of Angle's class II div 1 malocclusion. The prevalence of Angle's class I type 3 and class III type 1 was approximately 6.78% and 6.42%, respectively. Patients with posterior crossbite showed the lowest incidence with 3.92% (Table 3).
Table 3.
Frequency distribution of patients: malocclusion.
| Serial no. | Malocclusion | Frequency | Percentage |
|---|---|---|---|
| 1 | Angle class I type 1 | 42 | 15 |
| 2 | Angle class I type 2 | 100 | 35.71 |
| 3 | Angle class I type 3 | 19 | 6.78 |
| 4 | Angle class I type 4 | 11 | 3.92 |
| 5 | Angle class II div 1 | 68 | 24.28 |
| 6 | Angle class II div 2 | 18 | 6.42 |
| 7 | Angle class III | 22 | 7.85 |
Frequency distribution of mechanotherapy and treatment modalities
Treatment modalities and associated mechanics were predominantly preadjusted edgewise appliance with 95%. Other type of brackets types such as ceramic and lingual brackets showed 3.92% and 1.08% in frequency. As far as growth modification was concerned, 12.14% and 3.57% of patients got benefitted with such treatment facility. Ten percent of patients were treated with orthognathic surgical treatment procedure in conjunction with comprehensive orthodontics (Table 4).
Table 4.
Frequency distribution of mechanotherapy and treatment provider.
| Serial no. | Types of mechanotherapy | Frequency | Percentage |
|---|---|---|---|
| 1 | Preadjusted edgewise appliance | 266 | 95 |
| 2 | Ceramic | 11 | 3.92 |
| 3 | Lingual | 03 | 1.08 |
| 4 | Myofunctional appliance | 34 | 12.14 |
| 5 | Orthopedic appliance | 10 | 3.57 |
| 6 | Surgical (single jaw/bijaw or both) | 28 | 10 |
| 7 | Faculty | 244 | 87.14 |
| 8 | PG trainee | 36 | 12.86 |
PG, postgraduate.
Frequency distribution of treatment provider
About 87.14% patients were provided treatment by teaching faculty and 12.86% by postgraduate residents (Table 4).
Frequency distribution of Complexity and improvement grade: overall
Results showed that the department has 50% difficult and 22.84% very difficult complexity grade patient load, which later on showed improvement where they greatly increased to 55.35% and 32.85%, respectively (Table 5).
Table 5.
Frequency distribution of complexity and improvement grade.
| Serial no. | Complexity grade | Frequency | Percentage |
|---|---|---|---|
| 1 | Easy | 11 | 3.92 |
| 2 | Mild | 23 | 8.21 |
| 3 | Moderate | 32 | 11.42 |
| 4 | Difficult | 140 | 50 |
| 5 | Very difficult | 74 | 26.42 |
| Serial no. | Improvement grade | Frequency | Percentage |
|---|---|---|---|
| 1 | Greatly improved | 155 | 55.35 |
| 2 | Substantially improved | 92 | 32.85 |
| 3 | Moderately improved | 30 | 10.71 |
| 4 | Minimally improved | 03 | 1.71 |
| 5 | No improvement/worsening | 00 | 00 |
Frequency distribution of complexity grade: by treatment provider
Among 87.14% patients treated by faculty, 47.95% had difficult and 22.95% had very difficult complexity grading. Similarly, postgraduate residents had provided treatment with 63.88% difficult and 19.44% very difficult complexity grade (Table 6).
Table 6.
Comparative frequency distribution of complexity and improvement grade: by treatment provider.
| Serial no. | Complexity grade | Faculty | Percentage | PG trainee | Percentage |
|---|---|---|---|---|---|
| 1 | Easy | 11 | 4.50 | 0 | 0 |
| 2 | Mild | 23 | 9.42 | 0 | 0 |
| 3 | Moderate | 26 | 10.65 | 6 | 16.66 |
| 4 | Difficult | 117 | 47.95 | 23 | 63.88 |
| 5 | Very difficult | 56 | 22.95 | 7 | 19.44 |
| Serial no. | Improvement grade | Faculty | Percentage | PG trainee | Percentage |
|---|---|---|---|---|---|
| 1 | Greatly improved | 126 | 51.63 | 29 | 63.88 |
| 2 | Substantially improved | 87 | 35.65 | 5 | 19.44 |
| 3 | Moderately improved | 28 | 11.47 | 2 | 16.66 |
| 4 | Minimally improved | 03 | 1.25 | 0 | 0 |
| 5 | No improvement/worsening | 00 | 00 | 0 | 0 |
PG, postgraduate.
Discussion
The present study was a retrospective analysis of the quality control of the orthodontic treatment within the orthodontic department of one of the Apex Dental Centre of Indian Army by determining retrospectively, the workload, type of treatment, and quality of outcome of the treatment that had been provided to patients from January 2010 till December 2017 using ICON. Total of 280 patients were evaluated with ICON.
With average daily attendance of 65 patients, monthly and yearly attendance of approximately 1500 and 18000 patients, respectively, it becomes imperative to assess the frequency of treatment need and its complexity as well as the outcome of the treatment provided by both faculty and residents. This retrospective study is the form of clinical audit, which is a systematic method to assess whether the goal is being reached and identifies the area of improvement and lacunae.
In this, we shortlisted treatment records of 280 patients, by following inclusion criteria, who had undergone comprehensive orthodontic treatment in the department. Pretreatment and post-treatment study models and photographs were assessed by using ICON. Although several indices have been used for the assessment of orthodontic treatment need and treatment outcome in the past by researchers, ICON is a more pliable and convenient index. The only inventory required for assessment was measuring ruler along with study models and photographs of the patients. Ease of scoring and easily reproducible distinct cutoff value were other added advantages of the ICON.6
In a previous retrospective audit of orthodontic treatment need and outcome of adults in Army Dental Centre (R & R), Kamat et al.1 showed that a larger number of adults treated at the center had severe handicapping malocclusion. Their assessment was based on the DAI which have been adopted by the World Health Organization. The present study carried forward the same audit with wider inclusion sample and variables. However, the DAI were replaced with ICON because of its aforementioned advantages. Similarly, Ali Borzabadi-Farahani6 had also shown that in comparison to the DAI, the ICON does not suffer from deficiencies of lack of assessment of some occlusal anomalies such as posterior crossbite, impacted teeth, and deep overbite.
Yijin et al.8 investigated the subjective perception and objective treatment need and complexity of a number of patients seeking orthodontic retreatment. These patients had good perception of dental aesthetics and strong motivation. The study showed that they had an objective treatment need, indicated by the ICON scores. Although the present study did not consider retreatment patients, it shows that there is an increased treatment demand by late adolescent and adult population with a mean age of approximately 16 years with an SD of 4 years. It could be because of increased awareness with wider accessibility and reach of the present institution. Ngom et al.9 reported the treatment need for 665 Senegalese school children aged 12–13 years using IOTN and ICONs. The authors concluded that, despite the heavily weighted esthetic factor, treatment need according to the ICON does not differ much from the results with IOTN.9 Hence, the present study also used ICON rather than DAI or IOTN because of its multifacet advantages and accuracy.
The present study observed that 56.43% female and 43.57% male patients had been provided orthodontic treatment. Among the analyzed sample, Angle's class I type malocclusion, i.e. bimaxillary protrusion, was the highest with 35.71%, followed by 24.28% of Angle's class II div 1 malocclusion. The prevalence of Angle's class I type 3 and class III type 1 were approximately 6.78 and 6.42%, respectively. Patients with posterior crossbite showed a lowest incidence with 3.92%. The patient's load was in accordance with prevalence and severity of malocclusion reported in India by Kharbanda et al10 who reported that bimaxillary protrusion and class II div 1 malocclusion due to mandibular deficiency is among the commonest malocclusion in Indian population. Proffit et al.11 also showed similar demographic distribution in class II div 1 malocclusion in Caucasian population. Onyeaso12, 13 reported orthodontic treatment need in Nigerian and North American population in his two-series article and showed that 35.30% and 47% population had severe orthodontic treatment need. The present study also found that treatment modalities and associated mechanics were predominantly preadjusted edgewise metal appliance within Armed Forces with result over 95%. Other type of bracket variations such as ceramic and lingual showed 3.92% and 1.08% in frequency. The variation could be because of easy availability and supply of preadjusted edgewise metal appliance in comparison to more expensive tooth-colored ceramic and lingual brackets in Indian Armed Forces.
As far as growth modification was concerned, 12.14% and 3.57% of patients got benefited with such treatment facility. Ten percent of patients were treated with orthognathic surgical treatment procedure in conjunction with comprehensive presurgical and postsurgical orthodontics. The higher incidence of orthognathic surgical procedures in the present institution is supported by the reports of Proffit et al.11 who have shown that the incidence of orthognathic surgery procedures is increasing. Similarly, in 2015, around 1000 orthognathic treatment procedures were performed in Denmark for dentofacial esthetic improvement.11 Increased awareness among adults reporting for orthodontic treatment, receiving referral of more complex dentofacial deformities, and better surgical techniques and facilities could be the reasons for increased orthognathic surgical procedures.
About 87.14% of patients were provided treatment by teaching faculty and 12.86% of patients by postgraduate residents. The late inception of postgraduate program in the orthodontic department, i.e. 2013 onwards, was the reason of this disparity in particular. Among 87.14% patients treated by faculty, 47.95% had "difficult" and 22.95% had "very difficult" complexity grading. Similarly, postgraduate residents had provided treatment with 63.88% "difficult" and 19.44% "very difficult" complexity grade. Owing to the requirement of the university, residents were not allotted patients below "moderate" complexity grade.
The mean duration of orthodontic treatment was 31.19 months, range varying from 17 months to 46 months and an SD of 7.29 months. In another study, Bhattarai et al.14 reported the duration of orthodontic treatment in Nepalese population to be 30.38 months for adolescent and 28.83 months for adults. Similarly, Flink et al.15 also reported that the average duration of orthodontic treatment was 23.1 months. The difference could be related to different sample size, severity of malocclusion, and choice of appliance.15
Fields16 reported that dental education is at the crossroads, and the associated background papers in the "Journal of Dental Education" by him have encouraged educators to improve knowledge of “what works and what does not work in the prevention and treatment of oral health problems.”17
Conclusion
The present study concludes that fair quality control is being maintained by the department considering the number of patients load, its severity, and excellent outcome. However, because the concepts of evidence-based and patient-centered treatment dominates orthodontic field day by day, clinical audit of the department at the regular interval will not only help us to deliver quality care according to the patient's realistic expectations but also justify the expenditure of orthodontic inventory in Armed Forces. Hence, being the premier institute of Indian Armed Forces, regular clinical audit assessment should be conducted to fulfill demand and supply ratio appropriately.
Conflicts of interest
The authors have none to declare.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.mjafi.2018.09.002.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Kamat U., Jayan B., Kotwal A. Retrospective audit of orthodontic treatment need and outcomes in Army dental centre (R &R) J Dent Defence Sec. 2008;3:3–6. [Google Scholar]
- 2.Brook P.H., Shaw W.C. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 3.Richmond S., Shaw W.C., O'Brien K.D., Buchanan I.B., Jones R., Stephens C.D. The development of the PAR index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 4.Daniels C., Richmond S. The development of the index of complexity, outcome and need (ICON) J Orthod. 2000;27:149–162. doi: 10.1093/ortho/27.2.149. [DOI] [PubMed] [Google Scholar]
- 5.Templeton K.M., Powell R., Moore M.B., Williams A.C., Sandy J.R. Are the peer assessment rating index and the index of treatment complexity, outcome, and need suitable measures for orthognathic outcomes? Eur J Orthod. 2006;28:462–466. doi: 10.1093/ejo/cji120. [DOI] [PubMed] [Google Scholar]
- 6.Borzabadi-Farahani Ali. The relationship between the ICON index and Esthetic components of the IOTN index. World J Orthod. 2010;11:43–48. [PubMed] [Google Scholar]
- 7.Pandis N., Polychronopoulou A., Eliades T. Sample size estimation: an overview with applications to orthodontic clinical trial designs. Am J Orthod Dentofacial Orthop. 2011;140:e141–e146. doi: 10.1016/j.ajodo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Yijin R. Patient's perceptions, treatment need and complexity of orthodontic re-treatment. Eur J Ortho. 2009;31:189–195. doi: 10.1093/ejo/cjn096. [DOI] [PubMed] [Google Scholar]
- 9.Ngom P.I., Diane F., Dieye F. Orthodontic treatment need and demand in Senegalese school children aged 12-13 years. An appraisal using IOTN and ICON. Angle Orthod. 2007;77:323–330. doi: 10.2319/0003-3219(2007)077[0323:OTNADI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Kharbanda O.P. What is the prevalence of malocclusion in India? Do we know the orthodontic treatment needs of our country? J Indian Orthod Soc. 1999;32:33–41. [Google Scholar]
- 11.Proffit W.R., Fields H.W., Moray L.J. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthod Orthognath Surg. 1998;13:97–106. [PubMed] [Google Scholar]
- 12.Onyeaso C.O. Orthodontic treatment need of Nigerian out patients assessed with the Dental aesthetic index. Aust Orthod J. 2004;20:19–23. [PubMed] [Google Scholar]
- 13.Onyeaso C.O. Orthodontic treatment need in a accredited graduate orthodontic center in North America: a Pilot study. J Contemp Dent Pract. 2006;7:1–7. [PubMed] [Google Scholar]
- 14.Bhattaraj P.M., Shrestha R.M. Comparative duration of orthodontic treatment among Napalese adolescent and adult patients. Orthod J Nepal. 2011;1:28–30. [Google Scholar]
- 15.Flink D.F., Smith R.J. The duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102:45–52. doi: 10.1016/0889-5406(92)70013-Z. [DOI] [PubMed] [Google Scholar]
- 16.Fields M.J., Institute of Medicine . 1995. Dental Education at the Crossroads: Challenges and Change. Washington, DC. [PubMed] [Google Scholar]
- 17.Fields M.J. Background papers and summary from the IOM report-dental education at the crossroads: challenges and change. J Dent Educ. 1995;59:7–237. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.