Abstract
Background
Stress fractures (SFs) occur because of repetitive submaximal stresses to the bone over a period of time. SFs cause an economic loss to the organization and to the individuals who get invalided out of army because of SFs. This study was conducted to determine the incidence, distribution, onset of SFs, and invalidment patterns due to SFs.
Methods
This prospective study was carried out among recruits undergoing training at training centres in a cantonment of Central India. The recruits enrolled were followed up through their training period for occurrence of SF. On occurrence of SF, the clinical features, site of bone involved, and the weeks of completed military training were noted. The SFs were graded into four grades based on clinicoradiological features and managed accordingly.
Results
A total of 8974 recruits were enrolled into the study, of which 208 recruits suffered SFs. The commonest bone involved was the tibia (86.5%), commonest site being the proximal one-third of the tibia shaft (46.2%). Average week of developing SF was the 15th week of training. Seven recruits were invalided out of army because of SFs, the commonest cause being femoral neck SFs.
Conclusion
Prevention is the best approach for SFs. It is suggested to increase the intensity of training gradually over the first 16 weeks and recruits are to be given a training pause at around the 12th week for healing of stressed bones just before the peak time of occurrence of SFs. Femoral neck SFs are the commonest SFs responsible for invalidment of recruits.
Keywords: Stress fractures, Army recruits, Military medicine
Introduction
Stress fractures (SF) are one of the most common overuse injuries. SFs occur as result of repetitive cumulative submaximal stress to the bone over a period of time.1 The first description of SFs in literature is by a Prussian military physician Breithaupt. In 1855, he described soldiers with oedematous painful feet which a few decades later, in 1897, were described as march fractures on imaging by Stechow.2, 3, 4, 5 SFs can occur in all age groups and is a common ailment in military recruits undergoing military training. Aetiologically, SFs can be classified into two types—fatigue fractures and insufficiency fractures. Insufficiency fractures occur due to application of normal stress to an abnormal bone, and fatigue fractures occur due to application of repeated abnormal stress to a normal bone.6
In military recruits, the type of stress fractures which occur are invariably fatigue fractures, which are associated with a new or different activity of the person that is repeated over sometime and is strenuous enough to ultimately produce the typical signs and symptoms of SFs.7 The incidence of SFs ranges from 1.5% to 31% depending on the population studied.8, 9, 10, 11, 12 SFs in military recruits are a cause of concern. SFs not only cause increased morbidity and long absence from training but are also a cause of an economic loss to the organization and the individual. The individual stands to lose an employment opportunity if boarded out of the military because of his inability to cope with the training, subsequent to a SF.
The presenting symptom of SFs is pain at the site, which increases on exertion or weight bearing. Clinically, findings of SF include bony tenderness and swelling. History of undue exertion and clinical assessment provide a preliminary diagnosis of SFs. The same can be confirmed radiologically. A plain radiograph can identify an SF as a periosteal reaction or cortical break. If clinical suspicion is high and radiographs are equivocal, magnetic imaging resonance or bone scans can identify the SFs that were not identified using conventional radiographs. Preventing the SFs is the best but practically a difficult approach for avoiding SFs. Management strategies include early diagnosis by identification of the symptoms, a training pause which is sufficiently long to allow the bone to heal, and in some cases, surgical intervention for an impending or complete fracture may be required.13, 14
Studies on SFs in Indian Army recruits are limited especially in terms of invalidments out of the service. In addition, information about the actual incidence is important to provide a platform for recommending prevention strategies for the future and increase the overall health of the troops. This study was conducted in a cantonment of Central India, where nearly 8000 recruits undergo training at any point of time.
Materials and methods
A prospective study was carried out from January 2016 to August 2017 to study the incidence and patterns of SFs and incidence of invalidments among recruits undergoing training at training centres located in one of the biggest cantonments in Central India. All these recruits were in a similar phase of military training and in the age group of 18–22 years. Details were recorded about their demographic parameters, dietary habits, training activities, and the training schedule followed. The recruits enrolled were followed up through their training period for occurrence of SF. Upon development of symptoms of SFs, they were subjected to radiography. On radiological confirmation of SF, the clinical features, site of the bone involved, any particular training event leading to the recruit seeking medical help, and the weeks of military training completed were noted. Recruits who were symptomatic with pain but no radiological abnormality were not included in the study. The SFs were graded into four grades based on clinicoradiological classification proposed by Agarwal15 (Table 1).
Table 1.
Clinicoradiological grading of SFs by Agarwal.15
| Grade | Clinical Picture | Radiography |
|---|---|---|
| Grade 0 | Mild pain, limp & tenderness which comes while walking without support | Normal even after 3 wk of onset of symptoms |
| Grade I | Same as above | Periosteal reaction |
| Grade II | Severe pain & may walk with support | Unicortical break |
| Grade III | Severe pain and inability to stand/walk | Complete undisplaced fracture |
| Grade IV | Same as above | Complete, displaced fracture |
Clinicoradiological grading of stress fractures by Agarwal.15
They were appropriately managed by rest/Plaster of Paris cast immobilization or surgery depending on the grade of SF. Thereafter, they were given a period of convalescence in the form of sick leave and followed up every four–six weeks for clinical and radiological recovery until the time of healing. Following this, they were gradually reintroduced into the training schedule. A few of these recruits who were not able to start with training within the stipulated time period or were deemed unfit for rigorous military training were recommended to be invalided out of service.
Results
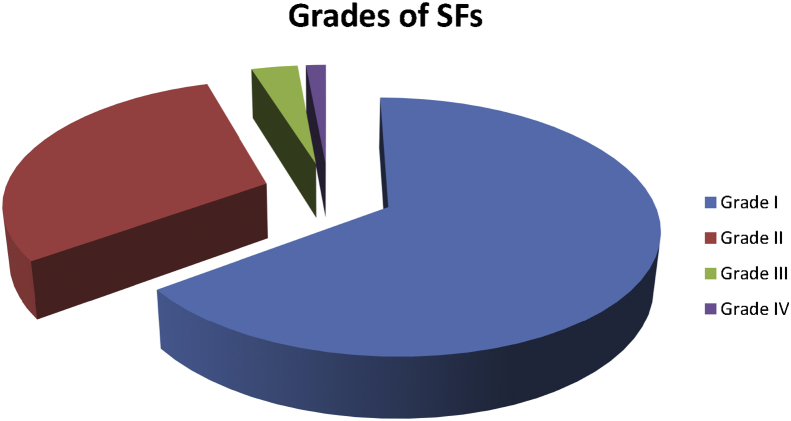
A total of 8974 military recruits undergoing military training in the training centres in this cantonment during that period were enrolled into the study. Of these, during followups, 208 recruits suffered from SFs. The total incidence of SFs in the study population of military recruits at these training centres was found to be 2.3%. As far as clinicoradiological grading is concerned, the most common grade of SF was Grade I (65%) i.e. the patient had pain and tenderness at the site of SF but could walk without support, and the radiograph showed periosteal reaction. The least common grade of SF was Grade IV i.e. they had complete displaced fracture on presentation, and they were unable to stand/walk (Fig. 1).
Fig. 1.
Distribution of grades of stress fractures. SFs, stress fractures.
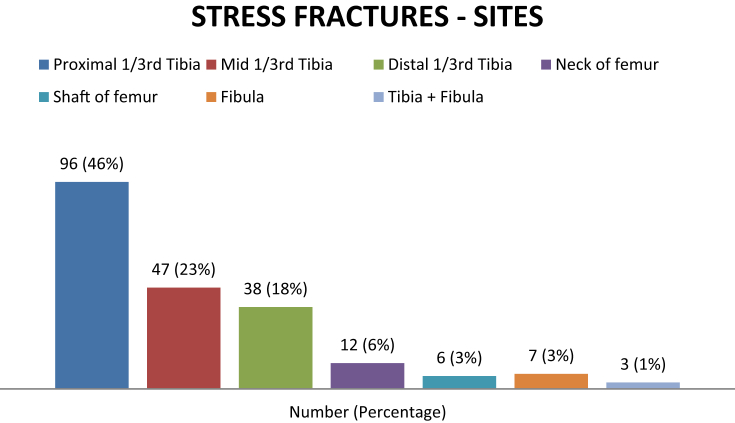
As far as the site of SFs is concerned, the most common bone involved was the tibia (86.5%). In the tibia, the most common site of the involvement was proximal one-third of shaft of the tibia (46.2%). Of 208 SFs, seven occurred only in the fibula, whereas three of them involved shafts of the tibia and fibula together. The femur was involved in 18 patients, of whom 12 had SF of the neck of the femur, and six patients had SF of the shaft of the femur (Fig. 2). The study population did not have any patient with SFs of the metatarsals. There was one patient who presented with fracture shaft of the third metatarsal who had no prior history of pain in the foot, but there was history of fall. Hence, he was not included in the group of SFs.
Fig. 2.
Graph showing number of Stress fractures at each site.
Average week of onset of SF was during the 15th week of training. The earliest a recruit had a SF was in the 8th week of training, and two recruits developed SF as late as during the 34th week of training.
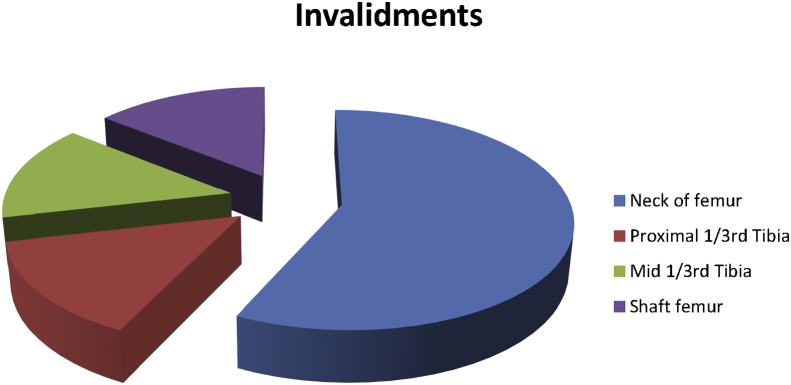
A total of seven recruits (3.3% of SFs) could not return to training or were deemed unfit for rigorous military training within the stipulated period of their absence and were therefore invalided out of army because of this condition. Four of these seven patients invalided out of service suffered from femoral neck SFs (57%). Of 12 patients who suffered from femoral neck SFs (FNSF), four patients (33%) had to be invalided out of service (Fig. 3). Of these, three were managed with surgery, (screw fixation) and one was managed conservatively. Other recruits who were invalided out of service had SFs involving the shaft of the femur, proximal one-third of the tibia and mid one-third of the tibia (one patient in each category). There was no significant difference in the incidence of SFs in vegetarians and non-vegetarians.
Fig. 3.
Invalidments out of service as per sites of Stress fractures.
Discussion
SFs are one of the most common overuse injuries that are caused because of excessive and repetitive stress on the bone. This causes accelerated bone remodelling, production of microfractures because of insufficient time for bone repair, the occurrence of bone stress injury/stress reaction and finally, a SF.1, 16, 17 SFs are the most common cause of loss of military training among recruits.18 The incidence of SFs has been reported differently in various Indian as well as western studies. It ranges from as low as 0.25% as reported by Prasanna et al.1 in a study on 2000 Indian paramilitary recruits to as high as 31% in a study on 295 Israeli recruits by Milgrom et al.12 Studies in Indian army recruits showed an incidence of SFs of 7.04% by Dash et al.18 and 11.4% in another series.15 However, the incidence of SFs in this study was found to be 2.3% which was similar to an Indian study published by Singh et al. who reported the incidence of SFs as 3.65%.19
For the purpose of classification of SFs, we used a classification system as proposed in the study by Agarwal (Table 1). Similar classification system has been used in a study by Dash et al. In their study, they found that the most common grade of SFs was Grade II followed by Grade I.18 The most common grade of SFs in our study was Grade I, which is same as the one observed in a study by Agarwal.15 The time of onset of SF in our study was found to be the 15th week. This is similar to the one reported by Sterling et al.20 In addition, Giladi et al. reported the peak time of occurrence of SFs as 14 weeks.21
The most common bone which was found to develop SF in our study was tibia. Various sites of SFs have been described in literature including tibia, metatarsals, fibula, femur, neck of femur, etc. Few atypical sites of SFs have also been described in athletes and soldiers like ribs, scaphoid, patella, tarsal bones, etc.22 However, the percentage of SFs developing in these sites were different in different studies. The most commonly involved bone in SFs was the tibia in many studies18, 19, 20, 21, 23, 24 and the metatarsals in some studies.2 The percentage of SFs in the tibia was 88.57% in the study by Dash et al.18, 76.8% in study by Milgrom et al.12 and 87.6% in the study by Bhatnagar et al.14 Our study found the percentage of SFs in the tibia to be 86.5% which is similar to most of the studies. Other sites of SFs in our study were the fibula, femoral shaft, neck of the femur and involvement of tibia and fibula together. We did not encounter any recruit with a SF of the metatarsals. We divided the tibia in one-thirds as proximal, mid and distal to further categorize the sites of SFs of the tibia and found that the most common site of affection was proximal one-third (46.2%) which is similar to what is reported by Dash et al. and Singh et al. in their study.18, 19
Boarding out/invalidment of a recruit from the military has got financial implications which strain the military budget as the costs involved in recruitment, training, accommodation, clothing, food, medical care, wages, etc cannot be recovered once the recruit is discharged from military service. There is also the added burden of lifelong disability pension to deal with. SFs are a major reason for attrition of recruits from military training. In a study by Trone et al., it was found that occurrence of SFs during basic training was the most powerful predictor of invalidment out of military service and recruits who suffered from SFs were four times more likely to get invalided out of service than those who did not suffer a SF.25
In our study, we found that the incidence of invalidments among all recruits who suffered SFs was 3.3%. FNSF was the most common culprit for attrition as 57% of the total invalidments because of SF were due to FNSF, and of 12 patients who had suffered FNSF (i.e. 6% of total diagnosed SFs), four patients (33%) had to be invalided out of service. These findings are similar to the study conducted by Dash et al. in which they found the incidence of invalidments as 3.47% of total recruits who suffered SFs. The study also observed that 60% of patients who developed SFs involving femur were boarded out, although the study does not specifically mention the neck of the femur as a separate site.18 Talbot et al. have reported an incidence of FNSF as 8% of total SFs and invalidments rate of 40% in recruits who developed FNSF.26
Conclusion
Our study brings out the incidence, patterns of distribution, and most importantly, patterns of invalidments of recruits who suffer from SFs during their basic military training. Prevention is definitely the best approach for SFs. It is suggested that the intensity of training shall be increased gradually over the first four months (16 weeks) of training and recruits are to be given a training pause at around the 12th week for healing of stressed bones just before the peak time of occurrence of SFs. The neck of the femur is the most morbid of all the sites once it develops a SF and is a major cause of invalidment of recruits. To study the stressors leading to a SF, more studies are need to be undertaken in future with emphasis on interventions related to possible stressors like shoes, training ground and intensity of training.
Conflicts of interest
The authors have none to declare.
References
- 1.Prasanna C., Vijay Baba N., Rajinikanth S. A preliminary study of stress fractures among paramilitary trainees. J Evol Med Dent Sci. 2014;3(10):2565–2569. [Google Scholar]
- 2.Wood A.M., Hales R., Keenan A. Incidence and time to return to training for stress fractures during military basic training. J Sports Med. 2014 doi: 10.1155/2014/282980. Article ID 282980, 5 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson M.W., Greenspan A. Stress fractures. Radiology. 1996;199:1–12. doi: 10.1148/radiology.199.1.8633129. [DOI] [PubMed] [Google Scholar]
- 4.Vasiliadis A.V. Common stress fractures in runners: an analysis. Saudi J Sports Med. 2017;17(1):1–6. [Google Scholar]
- 5.Breithaupt M.D. The pathology of the human foot. Med Zeitung. 1855;24:169–175. [Google Scholar]
- 6.Hong S.H., Chu I.T. Stress fracture of the proximal fibula in military recruits. Clin Orthop Surg. 2009;1(3):161–164. doi: 10.4055/cios.2009.1.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daffner R.H., Pavlov H. Stress fractures: current concepts. AJR. 1992;159:245–252. doi: 10.2214/ajr.159.2.1632335. [DOI] [PubMed] [Google Scholar]
- 8.Kowal D. Nature and causes of injuries in women resulting from an endurance training program. Am J Sports Med. 1980;8:265–269. doi: 10.1177/036354658000800410. [DOI] [PubMed] [Google Scholar]
- 9.Mcbryde A.M. Stress fractures in runners. Clin Sports Med. 1985;4:737–752. [PubMed] [Google Scholar]
- 10.Milgrom C., Giladi M., Simkin A. The area moment of inertia of the tibia: a risk factor for stress fractures. J Biomech. 1989;22:1243–1248. doi: 10.1016/0021-9290(89)90226-1. [DOI] [PubMed] [Google Scholar]
- 11.Reinker K., Ozburne S. A comparison of male and female orthopaedic pathology in basic training. Mil Med. 1979;144:532–536. [PubMed] [Google Scholar]
- 12.Milgrom C., Giladi M., Stein M. Stress fractures in military recruits: a prospective study showing an unusually high incidence. J Bone Joint Surg (Br) 1985;67:732–735. doi: 10.1302/0301-620X.67B5.4055871. [DOI] [PubMed] [Google Scholar]
- 13.Jones B.H., Thacker S.B., Gilchrist J., Kimsey C.D., Sosin D.M. Prevention of lower extremity stress fractures in athletes and soldiers: a systematic review. Epidemiol Rev. 2002;24:228–247. doi: 10.1093/epirev/mxf011. [DOI] [PubMed] [Google Scholar]
- 14.Bhatnagar A., Kumar M., Shivanna D., Bahubali A., Manjunath D. High incidence of stress fractures in military cadets during training: a point of concern. J Clin Diagn Res. 2015;9(8):RC01–RC03. doi: 10.7860/JCDR/2015/12535.6282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agarwal P.K. Stress fractures: management using a new classification. Indian J Orthop. 2004;38:112–120. [Google Scholar]
- 16.Fayad L.M., Kamel I.R., Kawamoto S., Bluemke D.A., Frassica F.J., Fishman E.K. Distinguishing stress fractures from pathologic fractures: a multimodality approach. Skeletal Radiol. 2005;34(5):245–259. doi: 10.1007/s00256-004-0872-9. [DOI] [PubMed] [Google Scholar]
- 17.Niva M.H., Mattila V.M., Kiuru M.J., Pihlajamäki H.K. Bone stress injuries are common in female military trainees: a preliminary study. Clin Orthop Relat Res. 2009;467(11):2962–2969. doi: 10.1007/s11999-009-0851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dash N., Kushwaha A.S. Stress fractures: a prospective study amongst recruits. MJAFI. 2012;68:118–122. doi: 10.1016/S0377-1237(12)60021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh S.C., Banerjee A. Stress fractures: effect of prior physical activity, sports participation and military training. MJAFI. 2000;56:24–26. doi: 10.1016/S0377-1237(17)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterling J.C., Edelstein D.W., Calvo R.D., Webb R. Stress fractures in the athlete. Diagnosis and management. Sports Med. 1992;14:336–346. doi: 10.2165/00007256-199214050-00005. [DOI] [PubMed] [Google Scholar]
- 21.Giladi M., Milgrom C., Danon Y.L. Stress Fractures in military recruits. Med Corps Int. 1998;3:21–28. [Google Scholar]
- 22.Miller T.L., Best T.M. Taking a holistic approach to managing difficult stress fractures. J Orthop Surg Res. 2016;11:98. doi: 10.1186/s13018-016-0431-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waterman B.R., Gun B., Bader J.O., Orr J.D., Belmont P.J., Jr. Epidemiology of lower extremity stress fractures in the United States military. Mil Med. 2016;181(10):1308. doi: 10.7205/MILMED-D-15-00571. [DOI] [PubMed] [Google Scholar]
- 24.Greaney R.B., Gerber F.H., Laughlin R.L. Distribution and natural history of stress fractures in US marine recruits. Radiology. 1983;146:339–346. doi: 10.1148/radiology.146.2.6217486. [DOI] [PubMed] [Google Scholar]
- 25.Trone D., Reis J., Rauh C.M.M. Factors associated with discharge during marine corps basic training. Mil Med. 2007;172:936–941. doi: 10.7205/milmed.172.9.936. [DOI] [PubMed] [Google Scholar]
- 26.Talbot J.C., Cox G., Townend M., Langham M., Parker P.J. Femoral neck stress fractures in military personnel--a case series. J Roy Army Med Corps. 2008;154(1):47–50. doi: 10.1136/jramc-154-01-13. [DOI] [PubMed] [Google Scholar]