Abstract
Nonalcoholic fatty liver disease (NAFLD) is a spectrum of diseases ranging from simple hepatic steatosis to nonalcoholic steatohepatitis (NASH) to advanced fibrosis and cirrhosis as well as liver cancer. Despite the significant morbidity associated with NAFLD, there are no global consensus guidelines to screen for liver fibrosis in patients considered high risk, including patients older than 50 years with type 2 diabetes or metabolic syndrome. Multiple therapies are currently being investigated and may soon receive regulatory approval for use in the clinic. It is suggested that patients at high risk for NAFLD be screened in the outpatient setting. This article aims to supply primary care providers (PCPs) with the knowledge and tools needed to properly evaluate a patient at high risk of developing significant liver disease from NASH. A tripartite algorithm is described to help PCPs identify patients with NAFLD using liver enzymes and abdominal ultrasound, assess the presence of advanced liver fibrosis using clinical prediction rules, and, if appropriate, determine when to refer patients to specialist care.
Keywords: Nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, fatty liver, primary care, outpatients, ambulatory care, screening
Nonalcoholic fatty liver disease (NAFLD) is a constellation of conditions ranging from simple hepatic steatosis to nonalcoholic steatohepatitis (NASH), with or without fibrosis, culminating in liver cirrhosis and end-stage liver disease in its most severe form. For many patients, primary care providers (PCPs) are both the initial and the most common ongoing point of contact with the health care system. Thus, providing PCPs with guidelines that encourage proper screening and improve identification of patients at high risk for NAFLD is becoming increasingly important, as the prevalence of NAFLD is substantially increasing worldwide. A 2016 meta-analysis calculated that the global prevalence of NAFLD is 25.24%, with the rise reflecting similar increases in the rates of type 2 diabetes and obesity.1 In the United States, data from the National Health and Nutrition Examination Surveys showed that from 1988 to 2008, the prevalence of NAFLD increased from 5.51% to 11.01%.2 The large Multiethnic Cohort study of 215,000 patients found that NAFLD is the most common cause (52%) of chronic liver disease across all ethnic groups.3 In a prospective study of 328 patients (ages 18-70 years) seeking treatment for any condition at a US Army medical center, the overall prevalence of NAFLD was found to be 46% based on a right upper quadrant ultrasound, with a diagnosis of hepatic steatosis confirmed by biopsy when available.4 NASH was detected in 12.2% of the total cohort and in 29.9% of patients with positive ultrasounds. With such a high prevalence in the United States, it is not surprising that NAFLD was found to be the leading cause of cirrhosis in the Multiethnic Cohort3 and that NASH is currently the leading indication for liver transplantation among women and the second leading indication for men in the United States.5
Due to a large and increasing population, the diagnosis and treatment of NAFLD and NASH is costly and will continue to rise. Younossi and colleagues estimated the annual economic burden of NAFLD within the United States to be $103 billion using a Markov chain model that took into consideration the ability of individual patients to transition to different liver disease states, with the final being post–liver transplantation.6 NAFLD alone accounted for nearly $87.0 billion of the total cost across all age groups, while NASH accounted for nearly $15.4 billion. It is estimated that if the annual rate of increase in NAFLD prevalence continues to parallel that of obesity in the United States, the 10-year burden of NAFLD will surpass $1 trillion before taking into consideration the cost of treatment. With the increasing prevalence of NAFLD along with its high clinical and economic costs, the development of a diagnostic and treatment algorithm remains important. However, consensus screening guidelines for NAFLD do not exist among professional organizations in the United States. Routine screening is not recommended by the American Association for the Study of Liver Diseases (AASLD) practice guidance.7 No general screening recommendations are put forth by the US Preventive Services Task Force, the largest preventive health care organization in the United States, or by the National Institute for Health and Care Excellence (NICE), which provides national guidance and advice to improve health and social care in England.8 In contrast, the European Association for the Study of the Liver (EASL) does make such recommendations.9 It is expected that new NASH medications that may effectively stop progression or reverse NASH, with an effect on the inflammation or ballooning and/or fibrosis that are associated with it, may be approved for use by 2020,10,11 with additional approvals likely to occur over the subsequent 2 years.11 Cost-effectiveness analyses of screening have been made difficult by the current lack of data to prove the benefits of screening during the early stages of disease progression and the lack of effectiveness data on treatment of patients with NASH.12 The cost of the medications that are likely to be approved in the next few years is not yet known. However, cost must be considered in light of the extremely high cost of end-stage liver disease and transplantation that could be the outcomes in patients who are not screened in a timely manner and, thus, are not given important recommendations for diet and lifestyle changes as well as effective treatment, when available. Experts in the field have expressed the opinion that NASH screening will be cost-effective with the availability of effective medications.12 This article summarizes the screening guidelines and imaging modalities currently being implemented worldwide, and discusses whether they can be put to use in a primary care setting. As such, an algorithm to guide the screening and treatment of NAFLD among PCPs is provided. The importance of screening in high-risk patients is also reviewed.
Current Recommendations for Screening
American Association for the Study of Liver Diseases Practice Guidance
Routine screening of patients for NAFLD is currently not recommended by the AASLD’s practice guidance7 because there are uncertainties about diagnostic tests and options for treatment as well as a lack of evidence showing the long-term benefits and cost-effectiveness of screening (Table). The AASLD practice guidance was based in large part on a cost-effectiveness analysis for NAFLD screening.13 For this analysis, Corey and colleagues performed a simulation to compare quality-adjusted life years (QALYs) between patients who were screened at least once with ultrasound and patients who did not undergo screening.13 Among those screened, a biopsy was performed if fatty infiltration was present, and pioglitazone was administered upon confirmation of a NASH diagnosis. The results of this hypothetical model revealed that the screening strategy performed worse than no screening, primarily due to a loss of 0.02 QALYs among the screening group. A 12.0% reduction in the number of patients who developed cirrhosis as well as an 11.9% reduction in liver-related deaths was also reported among the screening group. The loss in QALYs was largely attributed to the side effects of pioglitazone. The screening strategy was found to be more cost-effective compared with the no-screening strategy when the side effects of pioglitazone were excluded. Furthermore, a sensitivity analysis that assumed the same costs as pioglitazone but superior adherence, efficacy, and side effects was performed and demonstrated a 0.07-point improvement in QALYs vs the no-screening strategy. The authors reported that NASH screening was cost-effective if superior treatment was made available when assessing both quality of life–adjusted and –unadjusted models. The authors concluded that even incremental improvements in treatment options create an environment where NASH screening is cost-effective.13
Table.
Current Recommendations for NAFLD Screening
| AASLD, 20187 | EASL, 20169 | NICE, 20168 | |
|---|---|---|---|
| Screening Recommendations | No recommendations are made for screening, even in high-risk groups (obesity, type 2 diabetes), due to uncertainties in diagnostic testing, long-term management, and cost-effectiveness. Maintain a high degree of suspicion for NAFLD or NASH in patients with type 2 diabetes. |
Patients with obesity or metabolic syndrome should be routinely screened with liver enzymes and/or ultrasound. High-risk patients (age >50 years, type 2 diabetes, or metabolic syndrome) should be assessed for more advanced disease. Patients with persistently elevated liver enzymes should be screened for NAFLD. | No recommendations are made for screening due to lack of evidence. Providers should be made aware that patients with type 2 diabetes or metabolic syndrome are more likely to have NAFLD. If NAFLD is already diagnosed, patients should be offered the ELF test to screen for fibrosis every 3 years. |
| Diagnosis or Workup | Rule out other common causes of chronic liver disease. If workup is negative and other comorbidities such as features of metabolic syndrome, hypothyroidism, polycystic ovarian syndrome, or sleep apnea are present, further investigation should take place. | Ultrasound is the first-line test for diagnosis. If ultrasound is unavailable or not feasible, serum biomarkers or steatosis scores should be used. Proton-MRI is generally not recommended for diagnosis due to expense. |
Rule out other common liver diseases. Liver enzymes should not be used to rule out NAFLD. Ultrasound is not recommended due to lack of cost-effectiveness. |
| Noninvasive Tests to Diagnose NASH and Stage Fibrosis | NFS or FIB-4 clinical prediction rules can be used to identify patients at higher risk of advanced fibrosis. VCTE or MRE may also be used to identify fibrosis. | Biomarkers, fibrosis prediction scores, or VCTE are acceptable methods of identifying patients at low risk of advanced fibrosis. | The ELF test should be offered to everyone with NAFLD to assess for advanced fibrosis. If the initial testing was negative, repeat every 3 years. |
| Liver Biopsy Recommendations | Liver biopsy should be considered in patients who have been identified as being at higher risk for fibrosis with noninvasive measures or in patients with metabolic syndrome in whom advanced disease is suspected. | If advanced fibrosis or cirrhosis has been identified, patients should undergo liver biopsy for confirmation. | No recommendations are given. |
| Treatment | Lifestyle changes are the primary recommendation, with an ideal targeted weight loss of 7%-10% of body weight. Pharmacotherapy should only be given to patients with biopsy-proven NASH. Vitamin E can be given to nondiabetic patients with biopsy-proven NASH. Pioglitazone can be considered in patients with or without type 2 diabetes. |
Lifestyle changes are the primary recommendation, with an ideal targeted weight loss of 7%-10% of body weight. Pharmacotherapy should be reserved for cases of biopsy-proven NASH or for patients at risk of advancement. Pioglitazone or vitamin E can be used for NASH, but if enzymes do not normalize within 6 months, these therapies should be stopped. |
Patients should be referred to specialists if advanced fibrosis is identified. Vitamin E or pioglitazone can be used in patients with advanced fibrosis, although comorbidities should be considered. Repeat the ELF test 2 years after starting medications. If the score rises, consider stopping medication. |
AASLD, American Association for the Study of Liver Diseases; EASL, European Association for the Study of the Liver; ELF, Enhanced Liver Fibrosis; FIB-4, Fibrosis-4; MRE, magnetic resonance elastography; MRI, magnetic resonance imaging; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; NFS, NAFLD Fibrosis Score; NICE, National Institute for Health and Care Excellence; VCTE, vibration-controlled transient elastography.
The AASLD practice guidance does not recommend NAFLD screening even among high-risk patients with diabetes or obesity. Instead, the use of clinical prediction rules such as the NAFLD Fibrosis Score (NFS), Fibrosis-4 (FIB-4) score, or transient elastography is recommended to risk-stratify patients with a high index of clinical suspicion. These higher risk groups clearly have an increased prevalence of hepatic steatosis.14 Thus, the lack of a recommendation to screen these patients will likely change in the future. In a study of 939 randomly selected patients with type 2 diabetes, the prevalence of hepatic steatosis was 56.9%.15 Additionally, the presence of obesity and/or diabetes is a known independent risk factor for more severe liver fibrosis.16 New cost-effectiveness studies are needed for this patient population.
European Association for the Study of the Liver Guidelines
In contrast to the AASLD practice guidance, the Clinical Practice Guidelines cowritten by EASL, the European Association for the Study of Diabetes, and the European Association for the Study of Obesity do recommend routine screening for NAFLD with liver enzymes and/or ultrasound in all patients with obesity or metabolic syndrome (Table).9 In addition, patients with persistently elevated liver enzymes should be screened for NAFLD. In patients considered to be at high risk (age >50 years with type 2 diabetes or metabolic syndrome), assessment for more advanced disease is advised. EASL also recommends that, regardless of liver enzymes, all patients found to have NAFLD should be evaluated for metabolic syndrome. Family screening is not recommended except in cases of known inherited diseases such as lysosomal acid lipase deficiency.
The noninvasive screening modalities endorsed by EASL offer an all-encompassing strategy to identify both patients with steatosis and patients with more advanced disease. Ultrasound should be utilized to diagnose NAFLD. Magnetic resonance imaging (MRI) is not recommended given its higher cost and lesser availability. EASL also recommends the use of serum biomarkers for larger-scale screening studies or if imaging is unavailable. These biomarkers include the fatty liver index, the commercial biomarker test SteatoTest (BioPredictive), and the NAFLD Liver Fat Score, as these have been validated in a general population. Patients with identified NAFLD can be assessed for advanced fibrosis using transient elastography. Clinical prediction rules such as the NFS or FIB-4 score, or commercial biomarker tests such as the Enhanced Liver Fibrosis (ELF; Siemens Healthcare Diagnostics Inc) test or FibroTest (BioPredictive; marketed as FibroSure in the United States), can also be utilized to identify advanced fibrosis. Per EASL guidelines, if advanced fibrosis is identified, it should be confirmed by biopsy.9
National Institute for Health and Care Excellence Guidance
The NICE guidance does not recommend screening patients for NAFLD, even in those with metabolic syndrome or type 2 diabetes, due to lack of evidentiary support (Table).8 Instead, clinicians should be made aware that NAFLD is more prevalent within those populations and that routine blood tests should not be used to rule out disease. Lifestyle modification is endorsed as a therapeutic strategy for patients with simple hepatic steatosis. In order to identify advanced fibrosis, the commercial ELF test is recommended. Patients with negative scores should undergo surveillance consisting of repeat testing every 3 years, whereas patients with positive scores should be referred to a specialist.
Summary of Current Guidelines and Recommendations
Consensus standards do not exist with regard to NAFLD screening. Current recommendations include a no-screening strategy (AASLD/NICE)7,8 and screening directed toward a high-risk population (EASL).9 Moreover, the methods used to identify patients with NAFLD are vague. Recent studies have suggested that screening patients with type 2 diabetes for NAFLD may be both feasible and effective for identifying patients at risk for advanced fibrosis.17,18 Proactive screening in high-risk patients is essential, as these patients are at a higher risk of developing more advanced stages of fibrosis.16 Further cost-effectiveness studies are needed in this patient population and should consider the costs of the quality-of-life decrement from NAFLD, liver cancer, end-stage liver disease, liver transplantation, and premature deaths.
A shortcoming of the cost-effectiveness study by Corey and colleagues13 is that it did not include costs related to the development of hepatocellular carcinoma (HCC), which has become more prevalent with the rise of NAFLD and NASH.19,20 NAFLD can progress to the development of HCC without cirrhosis. In a study by Kim and colleagues, the associated hazard ratio for the development of HCC was 16.73.21 Additional studies reported that HCC was found in 30% to 50% of patients with NAFLD in the absence of cirrhosis.22,23
Given the increasing prevalence of NAFLD, the promise of new medications in the near future, and the effects of untreated NAFLD, PCPs should begin screening high-risk patients, including those greater than 50 years of age with type 2 diabetes or metabolic syndrome, for NAFLD.
The Role of the Primary Care Provider in the Detection of Nonalcoholic Fatty Liver Disease
PCPs remain on the frontline of identifying patients with diabetes, hyperlipidemia, and hypertension, all components of metabolic syndrome. Thus, they are the optimal providers to identify patients with NAFLD, make appropriate referrals to specialists, and arrange appropriate surveillance for complications of metabolic syndrome that may occur. PCPs are essential in the development of a comprehensive understanding of the etiology and progression of this disease. Several studies have suggested that PCPs neither screen asymptomatic individuals as often as specialists do nor are they completely aware of the differences between NAFLD and NASH.24,25 A prospective cohort study designed to assess the severity of NAFLD in the primary care setting found an incidence rate of NAFLD of 26.4%.26 A total of 1118 patients with incidental abnormal liver function tests and no history or current signs of liver disease were recruited. NAFLD was confirmed with ultrasound after exclusion of other liver diseases. Elevated serum levels of gamma-glutamyl transpeptidase were the most common laboratory abnormalities found in patients with NAFLD, followed by elevation in alanine amino-transferase (ALT) levels. Advanced fibrosis as assessed by the NFS was found in 7.6% of patients, and could not be ruled out in another 35.2%. The number of primary care patients with abnormal liver enzymes and NAFLD may underestimate the true prevalence of the disease given the poor association between liver enzymes and the presence of NAFLD.27
The possible underdiagnosis of NAFLD and lack of appropriate care was further demonstrated in a large study conducted via a US Veterans Affairs database.28 Persistently elevated ALT levels (≥40 U/L measured on 2 occasions at least 6 months apart) were used to identify a subpopulation of patients who were deemed to have NAFLD after exclusion of other etiologies for abnormal liver enzymes. Only 39.4% of patients received any kind of NAFLD-appropriate care, which was defined as recognition of elevated transaminases, consideration of NAFLD and/or NASH as a diagnosis, lifestyle and diet recommendations being offered, and referral to a specialist. The strongest predictor of care was an ALT level greater than 80 U/L or patients whose ALT levels were consistently above 40 U/L. Calculated NFS did not correlate with a referral to a specialist within this study. The authors suggested that a lack of knowledge regarding current NAFLD guidelines was the underlying basis of these results and that further education and didactics could ameliorate the situation.
These studies27,28 indicate that NAFLD is underdiagnosed, and even their findings may underestimate its true prevalence. These prior studies were limited by reliance on the use of abnormal laboratory findings to identify patients with NAFLD. This is problematic as NAFLD frequently occurs in the absence of laboratory abnormalities.27 A discordance between laboratory abnormalities and imaging studies was shown in a small screening study carried out in the primary care setting by Doycheva and colleagues.17 MRI–proton density fat fraction (MRI-PDFF) and magnetic resonance elastography were used to estimate prevalence. In this population of patients with type 2 diabetes, imaging studies detected NAFLD in nearly 65.0% of patients and advanced fibrosis in 7.1% of patients despite the presence of elevated ALT levels in only 26.2% of the studied population.
Imaging Modalities
Of the 3 major imaging modalities (ultrasound, computed tomography, MRI), ultrasound offers the best combination of cost and ease of performance for detecting NAFLD. With a sensitivity of 85%, ultrasound imaging also offers an acceptable detection rate of fatty liver.29 The main drawback of this modality is its reduced detection rates if hepatic steatosis is less than 30%.30,31 This is in contrast to the more expensive MRI studies, which have a nearly 100% sensitivity in detecting steatosis greater than 5%.32 In addition, newer MRI techniques, including MRI-PDFF, offer enhanced and novel methods to detect and quantitate hepatic steatosis.33
Clinical Prediction Rules for Detecting Advanced Fibrosis
Once NAFLD has been detected, clinical prediction rules can be used to identify patients with fibrosis. These rules can be quickly calculated in the office setting and offer an easy way to risk-stratify patients who may need referral to a specialist. Liver fibrosis scores are based on the METAVIR scoring system. It ranks liver fibrosis as F0 (no fibrosis), F1 (mild fibrosis), F2 (moderate fibrosis), F3 (advanced fibrosis), or F4 (frank cirrhosis using liver biopsy).34
Nonalcoholic Fatty Liver Disease Fibrosis Score
The NFS is a simple and easy-to-use clinical prediction rule to identify patients with more advanced fibrosis. Using routinely obtained blood laboratory tests (platelet count, albumin, and aspartate aminotransferase [AST]/ALT ratio) and body parameters (age, body mass index, and impaired fasting glucose/diabetes), the NFS can reliably diagnose advanced fibrosis (positive predictive value, 90%) using the high cutoff score (>0.676) and exclude advanced fibrosis (negative predictive value, 93%) using the low cutoff score (<-1.455).35
Fibrosis-4 Score
Originally designed to evaluate liver fibrosis in patients coinfected with chronic hepatitis C virus and HIV, the FIB-4 score has been extended beyond this initial application.36-38 As with the NFS, the FIB-4 score uses a combination of routine laboratory values (AST, ALT, and platelets) and a clinical parameter (age) to produce a score that predicts the presence of advanced fibrosis. The validity of this test in the setting of NAFLD was studied in 541 NAFLD patients.38 The study demonstrated that a cutoff score of greater than 2.67 offered a positive predictive value of 80% for detecting advanced fibrosis, and a cutoff score of less than 1.30 offered a 90% negative predictive value for ruling out advanced fibrosis. The simplicity and ease of deriving the score makes it amenable for PCPs to calculate within an office setting. The FIB-4 score can be used in combination with the NFS to help determine the presence of advanced fibrosis.
Enhanced Liver Fibrosis Test
The ELF test is a commercial panel of markers of matrix turnover that is used as an indicator of the severity of fibrosis. These markers include tissue inhibitors of metalloproteinase-1, amino-terminal propeptide of type III procollagen, and hyaluronic acid.39 The ELF test was found to have a sensitivity and specificity of 90% for identifying severe liver fibrosis.40 Although some guidelines recommend that this test should be offered to patients with NAFLD, PCPs may start with one of the other clinical prediction rules before pursuing further expensive testing, as these are not routine laboratory tests that are easily obtained. The ELF test is recommended by NICE and available in the United Kingdom, but it is not currently available in the United States.
Transient Elastography
Transient elastography is a newer, relatively inexpensive and noninvasive method that uses ultrasound and low-frequency elastic waves to evaluate liver fibrosis as well as hepatic steatosis.41 This method converts the velocity of a shear wave passed through the liver into a liver stiffness measurement by application of Hooke’s law. The measurement can then be used to estimate the amount of liver fibrosis. Vibration-controlled transient elastography (VCTE; FibroScan, Echosens) is the most widely studied and used of these modalities using transient elastography, and was the first to be approved by the US Food and Drug Administration for this purpose.42 VCTE has an additional benefit in that it can estimate the amount of hepatic steatosis with the controlled attenuation parameter.43 VCTE offers good sensitivity and specificity for establishing high degrees of advanced fibrosis (stages F3-F4).44 Although not as accurate as magnetic resonance elastography to estimate liver stiffness, transient elastography has the benefit of being a point-of-care device that could allow measurement of liver stiffness within the context of a primary care office visit.45 In the future, transient elastography may be incorporated into the general armamentarium of a primary care office to help screen patients for liver fibrosis.
Some success has been achieved using transient elastography for screening purposes in the outpatient setting. Kwok and colleagues used it to screen for liver steatosis and fibrosis in a prospective study of patients with type 2 diabetes in an outpatient diabetes center.46 Of the 1918 patients screened, 72.8% had an increased controlled attenuation parameter measurement that was indicative of hepatic steatosis, and 17.7% had increased liver stiffness measurement indicating fibrosis. Many of these patients had confirmed fibrosis on liver biopsy.
Screening and Treatment Algorithm for Nonalcoholic Fatty Liver Disease in Primary Care Clinics
Although the gold standard for diagnosing NAFLD and NASH with and without fibrosis is liver biopsy, this method is often impractical, expensive, and not without risk. Figure 1 illustrates an algorithm to be used by PCPs to screen for NAFLD. Because laboratory values alone are not a reliable indicator of NAFLD,27 a 3-pronged approach is suggested to screen for NAFLD in high-risk patients (those with diabetes or metabolic syndrome above the age of 50 years).
Figure 1.
Suggested screening and treatment algorithm for NAFLD.
ALT, alanine aminotransferase; FIB-4, Fibrosis-4; NAFLD, nonalcoholic fatty liver disease; NFS, NAFLD Fibrosis Score.
First, patients should be screened for NAFLD with abdominal ultrasound and ALT, with healthy ALT levels defined as 19 to 25 U/L for women and 29 to 33 U/L for men.47 Second, if fatty liver is determined to be present, patients should be assessed for the severity of liver fibrosis using clinical prediction rule(s). PCPs are recommended to use both the NFS and the FIB-4 score, as they have been shown to have the best diagnostic accuracy of the noninvasive scores in detecting advanced fibrosis and are simple to calculate in the clinic.48 If the NFS and the FIB-4 score are indeterminate or discordant, patients should be referred for transient elastography. Finally, patients who are at high risk for advanced fibrosis or who are found to have this condition should be referred to a hepatologist or gastroenterologist for further evaluation (Figure 1).
Follow-Up Based on Screening Findings
If both the NFS and FIB-4 score are reassuring (NFS <-1.455 and FIB-4 score <1.30), the PCP should recommend appropriate lifestyle and diet changes, including recommendations for weight loss if needed, with continued surveillance and repeat testing in 1 year (Figure 1). However, if the scores are indicative of advanced fibrosis (NFS >0.676 and FIB-4 score >2.67), patients should receive an immediate referral to a specialist for further testing and evaluation. If only 1 score is elevated, patients should be referred to a specialist for further testing with transient elastography. The burden for PCPs following the NAFLD screening and treatment algorithm should be relatively low. A similar strategy was proposed in a study by Tapper and Lok,49 suggesting that PCPs could play a key role in both identifying at-risk patients and reducing the overall economic burden of NAFLD. Figure 2 shows suggested treatment strategies that PCPs can follow.
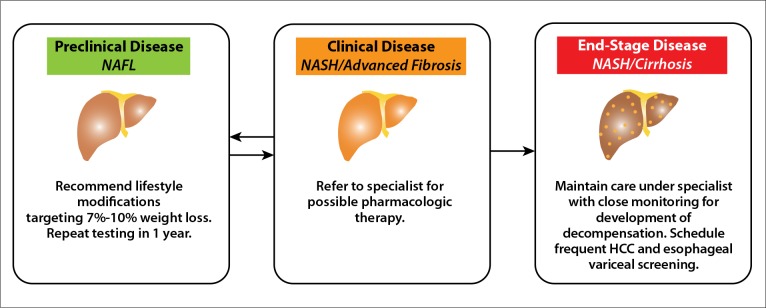
Figure 2.
Suggested treatment for patients with different forms of fatty liver disease.
HCC, hepatocellular carcinoma; NAFL, nonalcoholic fatty liver; NASH, nonalcoholic steatohepatitis.
Summary
NAFLD is a range of clinical conditions with high clinical and economic costs associated with screening and diagnosis. Finding the most cost-effective and least invasive methods of detection is increasingly important, as disease prevalence continues to rise in the United States and globally. When taken together, the current guidelines for screening NAFLD are inconsistent and reflect the uncertainty of disease etiology and imprecision of existing detection tools. As NAFLD is often clinically silent, the PCP is on the frontlines of screening and detection. It is suggested that PCPs begin screening their high-risk patients with a 3-fold approach. First, screen patients at high risk for liver disease (age >50 years with type 2 diabetes or metabolic syndrome) with liver enzymes and ultrasound. Second, employ either clinical prediction rules or imaging to detect the presence of advanced fibrosis. Third, refer patients to specialists if advanced fibrosis is identified. This algorithm will assist in the appropriate treatment of NAFLD patients. As NAFLD and NASH become more prevalent, knowledge of disease etiology, screening, and detection methods among PCPs becomes increasingly important.
References
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, Stepanova M, Afendy M et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9(6):524–530.e1. doi: 10.1016/j.cgh.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: the Multiethnic Cohort. Hepatology. 2016;64(6):1969–1977. doi: 10.1002/hep.28677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams CD, Stengel J, Asike MI et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 5.Noureddin M, Vipani A, Bresee C et al. NASH leading cause of liver transplant in women: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol. 2018;113(11):1649–1659. doi: 10.1038/s41395-018-0088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Younossi ZM, Blissett D, Blissett R et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–1586. doi: 10.1002/hep.28785. [DOI] [PubMed] [Google Scholar]
- 7.Chalasani N, Younossi Z, Lavine JE et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 8.Glen J, Floros L, Day C, Pryke R. Guideline Development Group. Non-alcoholic fatty liver disease (NAFLD): summary of NICE guidance. BMJ. 2016;354:i4428. doi: 10.1136/bmj.i4428. [DOI] [PubMed] [Google Scholar]
- 9.European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Banini BA, Sanyal AJ. Current and future pharmacologic treatment of nonalcoholic steatohepatitis. Curr Opin Gastroenterol. 2017;33(3):134–141. doi: 10.1097/MOG.0000000000000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuschwander-Tetri BA. Pharmacologic management of nonalcoholic steatohepatitis. Gastroenterol Hepatol (N Y) 2018;14(10):582–589. [PMC free article] [PubMed] [Google Scholar]
- 12.Younossi Z, Anstee QM, Marietti M et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 13.Corey KE, Klebanoff MJ, Tramontano AC, Chung RT, Hur C. Screening for nonalcoholic steatohepatitis in individuals with type 2 diabetes: a cost-effectiveness analysis. Dig Dis Sci. 2016;61(7):2108–2117. doi: 10.1007/s10620-016-4044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ong JP, Younossi ZM.Epidemiology and natural history of NAFLD and NASH Clin Liver Dis 20071111–16.vii [DOI] [PubMed] [Google Scholar]
- 15.Williamson RM, Price JF, Glancy S et al. Edinburgh Type 2 Diabetes Study Investigators. Prevalence of and risk factors for hepatic steatosis and nonalcoholic fatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care. 2011;34(5):1139–1144. doi: 10.2337/dc10-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30(6):1356–1362. doi: 10.1002/hep.510300604. [DOI] [PubMed] [Google Scholar]
- 17.Doycheva I, Cui J, Nguyen P et al. Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther. 2016;43(1):83–95. doi: 10.1111/apt.13405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong VW, Chalasani N. Not routine screening, but vigilance for chronic liver disease in patients with type 2 diabetes. J Hepatol. 2016;64(6):1211–1213. doi: 10.1016/j.jhep.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 19.Hashimoto E, Yatsuji S, Tobari M et al. Hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. J Gastroenterol. 2009;44(suppl 19):89–95. doi: 10.1007/s00535-008-2262-x. [DOI] [PubMed] [Google Scholar]
- 20.Younossi ZM, Otgonsuren M, Henry L et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology. 2015;62(6):1723–1730. doi: 10.1002/hep.28123. [DOI] [PubMed] [Google Scholar]
- 21.Kim GA, Lee HC, Choe J et al. Association between non-alcoholic fatty liver disease and cancer incidence rate. J Hepatol. 2018;68(1):140–146. doi: 10.1016/j.jhep.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Noureddin M, Rinella ME. Nonalcoholic fatty liver disease, diabetes, obesity, and hepatocellular carcinoma. Clin Liver Dis. 2015;19(2):361–379. doi: 10.1016/j.cld.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mittal S, Sada YH, El-Serag HB et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the Veteran Affairs population. Clin Gastroenterol Hepatol. 2015;13(3):594–601.e1. doi: 10.1016/j.cgh.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kallman JB, Arsalla A, Park V et al. Screening for hepatitis B, C and nonalcoholic fatty liver disease: a survey of community-based physicians. Aliment Pharmacol Ther. 2009;29(9):1019–1024. doi: 10.1111/j.1365-2036.2009.03961.x. [DOI] [PubMed] [Google Scholar]
- 25.Polanco-Briceno S, Glass D, Stuntz M, Caze A. Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialists. BMC Res Notes. 2016;9:157. doi: 10.1186/s13104-016-1946-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Armstrong MJ, Houlihan DD, Bentham L et al. Presence and severity of nonalcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol. 2012;56(1):234–240. doi: 10.1016/j.jhep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 27.Mofrad P, Contos MJ, Haque M et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286–1292. doi: 10.1053/jhep.2003.50229. [DOI] [PubMed] [Google Scholar]
- 28.Blais P, Husain N, Kramer JR, Kowalkowski M, El-Serag H, Kanwal F. Nonalcoholic fatty liver disease is underrecognized in the primary care setting. Am J Gastroenterol. 2015;110(1):10–14. doi: 10.1038/ajg.2014.134. [DOI] [PubMed] [Google Scholar]
- 29.Hernaez R, Lazo M, Bonekamp S et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54(3):1082–1090. doi: 10.1002/hep.24452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saadeh S, Younossi ZM, Remer EM et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123(3):745–750. doi: 10.1053/gast.2002.35354. [DOI] [PubMed] [Google Scholar]
- 31.Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez R, McCullough AJ. Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol. 2009;51(6):1061–1067. doi: 10.1016/j.jhep.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reeder SB, Cruite I, Hamilton G, Sirlin CB. Quantitative assessment of liver fat with magnetic resonance imaging and spectroscopy. J Magn Reson Imaging. 2011;34(4):729–749. doi: 10.1002/jmri.22580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Permutt Z, Le TA, Peterson MR et al. Correlation between liver histology and novel magnetic resonance imaging in adult patients with non-alcoholic fatty liver disease—MRI accurately quantifies hepatic steatosis in NAFLD. Aliment Pharmacol Ther. 2012;36(1):22–29. doi: 10.1111/j.1365-2036.2012.05121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bedossa P, Poynard T. The METAVIR Cooperative Study Group. An algorithm for the grading of activity in chronic hepatitis C. Hepatology. 1996;24(2):289–293. doi: 10.1002/hep.510240201. [DOI] [PubMed] [Google Scholar]
- 35.Angulo P, Hui JM, Marchesini G et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 36.Vallet-Pichard A, Mallet V, Nalpas B et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and FibroTest. Hepatology. 2007;46(1):32–36. doi: 10.1002/hep.21669. [DOI] [PubMed] [Google Scholar]
- 37.Kim BK, Kim DY, Park JY et al. Validation of FIB-4 and comparison with other simple noninvasive indices for predicting liver fibrosis and cirrhosis in hepatitis B virus-infected patients. Liver Int. 2010;30(4):546–553. doi: 10.1111/j.1478-3231.2009.02192.x. [DOI] [PubMed] [Google Scholar]
- 38.Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ. NASH Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104–1112. doi: 10.1016/j.cgh.2009.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lichtinghagen R, Pietsch D, Bantel H, Manns MP, Brand K, Bahr MJ. The Enhanced Liver Fibrosis (ELF) score: normal values, influence factors and proposed cut-off values. J Hepatol. 2013;59(2):236–242. doi: 10.1016/j.jhep.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 40.Guha IN, Parkes J, Roderick P et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology. 2008;47(2):455–460. doi: 10.1002/hep.21984. [DOI] [PubMed] [Google Scholar]
- 41.Sandrin L, Fourquet B, Hasquenoph JM et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29(12):1705–1713. doi: 10.1016/j.ultrasmedbio.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 42.Bonder A, Afdhal N. Utilization of FibroScan in clinical practice. Curr Gastroenterol Rep. 2014;16(2):372. doi: 10.1007/s11894-014-0372-6. [DOI] [PubMed] [Google Scholar]
- 43.Sasso M, Beaugrand M, de Ledinghen V et al. Controlled attenuation parameter (CAP): a novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36(11):1825–1835. doi: 10.1016/j.ultrasmedbio.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Tapper EB, Challies T, Nasser I, Afdhal NH, Lai M. The performance of vibration controlled transient elastography in a US cohort of patients with nonalcoholic fatty liver disease. Am J Gastroenterol. 2016;111(5):677–684. doi: 10.1038/ajg.2016.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loomba R. Role of imaging-based biomarkers in NAFLD: recent advances in clinical application and future research directions. J Hepatol. 2018;68(2):296–304. doi: 10.1016/j.jhep.2017.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kwok R, Choi KC, Wong GL et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Gut. 2016;65(8):1359–1368. doi: 10.1136/gutjnl-2015-309265. [DOI] [PubMed] [Google Scholar]
- 47.Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112(1):18–35. doi: 10.1038/ajg.2016.517. [DOI] [PubMed] [Google Scholar]
- 48.Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66(5):1486–1501. doi: 10.1002/hep.29302. [DOI] [PubMed] [Google Scholar]
- 49.Tapper EB, Lok ASF. Use of liver imaging and biopsy in clinical practice. N Engl J Med. 2017;377(23):2296–2297. doi: 10.1056/NEJMc1712445. [DOI] [PubMed] [Google Scholar]