Abstract
A previously healthy 10-year-old boy was hospitalized for a left cervical abscess associated with massive tonsillar hypertrophy. He underwent abscess drainage and bilateral tonsillectomy. At H36 post-surgery, he presented with tonsillar hemorrhage requiring surgical revision. Hemorrhage relapsed 2 days later, with a total of 7 episodes, 5 of which required surgical revisions. Laboratory investigations were normal except for a markedly low factor XIII (FXIII) activity at 7%. After administration of a single dose of 40 IU/kg plasma-derived FXIII (Fibrogammin®) I.V., the bleeding stopped with no further recurrence. FXIII activity gradually normalized (75%) at 6 weeks, confirming the transient character of factor XIII deficiency.
Severe congenital FXIII deficiency (FXIIID) (<1%) is very rare (1:2,000,000 births), whereas partial congenital deficiency and/or acquired deficiency may be more frequent but likely underreported. Acquired FXIIID may result from impaired synthesis (liver failure) or increased consumption (surgery, sepsis, leukemia, Henoch-Schönlein, inflammatory bowel disease, stroke, disseminated intravascular coagulation). FXIII replacement in form of fresh frozen plasma (FFP) or plasma-derived FXIII may be necessary for the presence of bleeding.
Keywords: Tonsillectomy, Bleeding, Transient factor XIII deficiency, Management
1. Introduction
Tonsillectomy is a common pediatric procedure with a post-operative course that is often uneventful. The reported prevalence of postoperative hemorrhage is variable spanning from 2 to 12% depending on the series and also on the patients' risk factors [1]. Older children aged 11 years and above, those with recurrent tonsillitis and/or those with attention deficit hyperactivity disorder have been reported as having a higher risk of bleeding [[1], [2], [3]]. According to some authors, post-tonsillectomy hemorrhage (PTH) can be classified into primary PTH (occurring within first 24 hours) usually related to inadequate hemostasis during surgery on one side, and secondary PTH (occurring beyond 24 hours) mainly due to either sloughing or infection on the other side [4]. Additionally, coagulopathies have also been reported in up to 4.5% cases of post-operative bleedings, with von Willebrand disease as the most common associated bleeding disorder [2,5]. We report the case of a young boy who presented several bouts of bleeding following adeno-tonsillectomy, and in whom a transient deficiency of Factor XIII (FXIIID) was diagnosed. Our aim is to draw the clinician's attention on this eventual complication and share our experience of its management.
2. Case report
A 10-year-old boy was referred to our emergency department with a 5 days history of febrile left cervical lymphadenopathy. He had been treated with paracetamol and non-steroidal inflammatory drugs, with good evolution initially; however, pain and swelling relapsed and gradually increased, and even worsened. His past medical history was positive for adenoidectomy and circumcision without any postoperative complication reported. Upon clinical examination, he presented with a left torticollis associated with erythematous left-lateral cervical swelling measuring around 7 cm in diameter. The swelling was indurated, tender on palpation, and filling the mandibular angle. The oral cavity examination was difficult because of trismus but could reveal a diffuse bulge of the veil of the soft palate predominantly on the left side, with hypertrophied tonsils. A CT-scan was performed and showed left cervical adenitis with abscess, adjacent cellulitis, and massive tonsillar hypertrophy. He was admitted to the hospital, and treated with intravenous antibiotics and steroids (methylprednisolone), he also underwent surgical abscess drainage with a bilateral tonsillectomy by our hospital ENT surgeon.
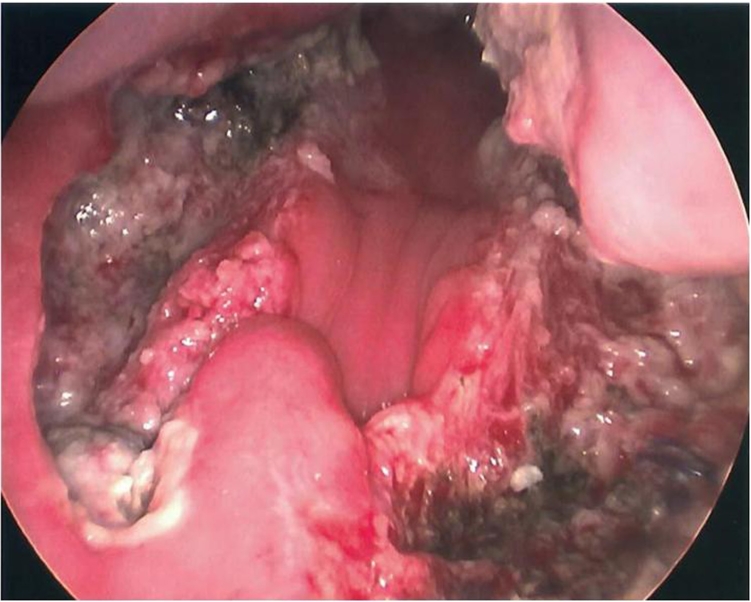
Thirty-six hours after the operation, the boy presented with tonsillar hemorrhage that required surgical revision (Fig. 1). Hemorrhage episodes again relapsed two days later requiring another surgical revision. At this point, the boy was investigated for a bleeding disorder. His first laboratory results showed unremarkable platelets count, PT, aPTT, fibrinogen, and von Willebrand factor. During the first week of hospitalization, postoperative hemorrhages recurred, for a total of 7 episodes, 5 of which required surgical revisions. He received platelets, fresh frozen plasma (FFP) and packed RBC transfusions as well as Tranexamic acid and DDAVP. Further hemostasis work-up results showed markedly reduced factor XIII (FXIII) activity of 7%. A single dose 40 IU/kg I.V. of plasma-derived FXIII (Fibrogammin®) was administered, the bleeding stopped without further recurrence.
Fig. 1.
Oral cavity inflammation post surgical revision.
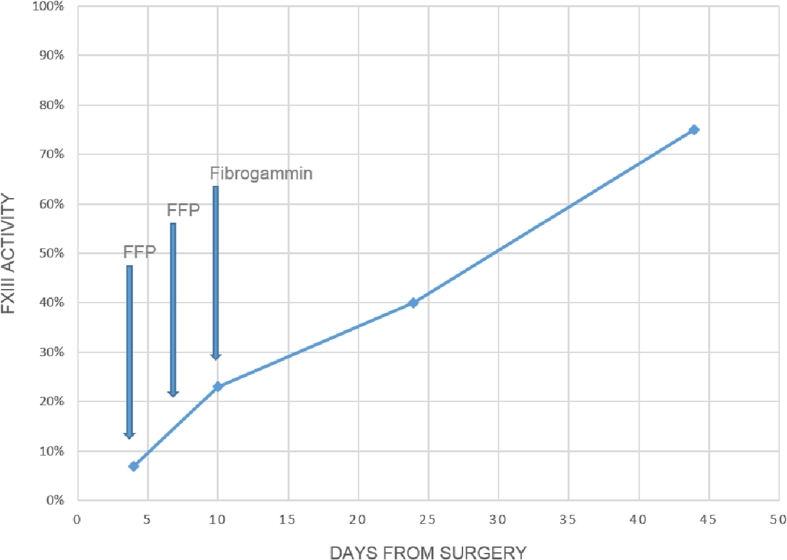
On control follow-ups, FXIII activity gradually normalized (75%) at the 6th postoperative week (Fig. 2), thus confirming the transient character of the deficiency. Furthermore, the presence of eventual FXIII inhibitor was excluded by measuring FXIII activity in mixing study (according to the Bethesda assay). The screening for antiphospholipid antibodies was negative.
Fig. 2.
Plasma FXIII activity and therapies administered over time.
3. Discussion
FXIII is a heterodimer (2A2B). FXIIIa subunit is essential for the stabilization of the fibrin-clot by covalent linkage of fibrin. Both its insufficiency and/or deficiency may lead to bleeding consequent to unstable clot formation [[6], [7], [8], [9]]. Studies have suggested that FXIIID should be suspected in infants with intracranial bleeding, prolonged bleeding and/or poor healing of the umbilical stump in newborn infants and/or delayed bleeding after surgery or trauma [[6], [7], [8], [9], [10]].
Severe congenital FXIIID, defined by a plasma Factor XIII levels <1%, is an autosomal recessive disorder that is a very rare condition with an estimated prevalence of 1:2′000′000 births, whereas partial congenital deficiency and/or acquired deficiency may be more frequent, but is likely underreported [6,[8], [9], [10]]. Acquired FXIIID may result from impaired synthesis in case of liver failure or it may result from increased consumption (surgery, sepsis, leukemia, Henoch-Schönlein, inflammatory bowel disease, stroke, disseminated intravascular coagulation). Rarely, the development of autoantibodies (FXIII inhibitors) can also cause acquired FXIIID, whose treatment (plasmapheresis, immunosuppression) is beyond the scope of our report [9,10]. The diagnosis post-tonsillectomy hemorrhage secondary to FXIIID is extremely rare, with only few cases reported in the literature [2,4,5]. In the largest case series by Mohammed et al. (4 adults and 2 children), the mean plasma FXIII level at time of diagnosis was 46.8% (range 15–58%), well above that presented by our patient (7%) [4]. In the management of our patient, the decision to perform tonsillectomy at the time of abscess drainage, intended to avoid a second anesthesia later, may have triggered bleeding both through the surgical act and associated sepsis, but this is speculative.
On the specific hematologic management standpoint, FXIII replacement may be necessary in the presence of bleeding and/or poor healing. Several FXIII replacement products are available: recombinant FXIIIa subunit (e.g. NovoThirteen®) or plasma-derived factor XIII concentrate (e.g. Fibrogammin®) [9,10].
The usual recommended dosages are 35 UI/kg of NovoThirteen® and 40 UI/kg of Fibrogammin®, but higher doses may be required in case of major and/or life-threatening bleedings. For patients who do not have access to these products, FFP (2–3 ml/kg) or cryoprecipitate (1 bag/10kg) can be used to supply FXIII [10]. We observed that Mohammed et al. treated their patients solely with FFP and/or packed red blood cells transfusions (PRBC) with results that seem to be suboptimal in comparison to ours with regard to control plasma FXIII levels at follow-up. The rarity of this pathology makes it difficult to comments on the ideal management (FFP versus Fibrogammin) [4].
4. Conclusion
Although rare, FXIIID (congenital or acquired) should be considered in the setting of recurrent postoperative hemorrhage, even in the absence of an evocative family and/or personal medical history, normal coagulation tests do not exclude the diagnosis. We, therefore, suggest that a patient with recurrent post-tonsillectomy bleedings beyond two episodes, and in whom no clear cause is identified, be screened for an eventual transient FXIIID. This attitude is, obviously, not evidence-based as severe FXIIID is extremely rare in clinical practice.
We speculate, on the pathophysiological point, that our patient may have presented a transient post inflammatory and/or consumption FXIIID. The overall prognosis was favorable.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
M. Jankovic, Email: mirela.jankovic@hopitalvs.ch.
M.L. Choucair, Email: marie-louise.choucair@chuv.ch.
B. Hallak, Email: Bassel.Hallak@hopitalvs.ch.
E. Hernandez, Email: estefania.hernandez@hopitalvs.ch.
M. Russo, Email: michel.russo@hopitalvs.ch.
J. Llor, Email: juan.llor@hopitalvs.ch.
S. Kayemba-Kay's, Email: kabangu.kayemba-kay's@hopitalvs.ch.
References
- 1.Spektor Z., Saint-Victor S., Kay D.J., Mandell D.L. Risk factors for pediatric post-tonsillectomy hemorrhage. Int J Pediatr Otorhinolaryngol. 2016 May;84:151–155. doi: 10.1016/j.ijporl.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Wall J.J., Tay K.-Y. Postoperative tonsillectomy hemorrhage. Emerg Med Clin N Am. 2018 May;36(2):415–426. doi: 10.1016/j.emc.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Sarny S., Ossimitz G., Habermann W., Stammberger H. Hemorrhage following tonsil surgery: a multicenter prospective study. The Laryngoscope. 2011 Dec;121(12):2553–2560. doi: 10.1002/lary.22347. [DOI] [PubMed] [Google Scholar]
- 4.Mohammed H., ALtamimi Z.A.R., Sheikh R., Al Taweel H., Ganesan S. Recurrent post tonsillectomy secondary hemorrhage in patients with factor XIII deficiency: a case series and review of literature. Am J Case Rep. 2016 15;17:850–854. doi: 10.12659/AJCR.900391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bidlingmaier C., Olivieri M., Stelter K., Eberl W., von Kries R., Kurnik K. Postoperative bleeding in paediatric ENT surgery. First results of the German ESPED trial. Hämostaseologie. 2010 Nov;30(Suppl 1) S108–111. [PubMed] [Google Scholar]
- 6.Muszbek L., Yee V.C., Hevessy Z. Blood coagulation factor XIII: structure and function. Thromb Res. 1999 Jun 1;94(5):271–305. doi: 10.1016/s0049-3848(99)00023-7. [DOI] [PubMed] [Google Scholar]
- 7.Karimi M., Peyvandi F., Naderi M., Shapiro A. Factor XIII deficiency diagnosis: challenges and tools. Int J Lab Hematol. 2018 Feb;40(1):3–11. doi: 10.1111/ijlh.12756. [DOI] [PubMed] [Google Scholar]
- 8.De Moerloose P., Schved J.-F., Nugent D. Rare coagulation disorders: fibrinogen, factor VII and factor XIII. Haemoph Off J World Fed Hemoph. 2016 Jul;22(Suppl 5):61–65. doi: 10.1111/hae.12965. [DOI] [PubMed] [Google Scholar]
- 9.Tahlan A., Ahluwalia J. Factor XIII: congenital deficiency factor XIII, acquired deficiency, factor XIII A-subunit, and factor XIII B-subunit. Arch Pathol Lab Med. 2014 Feb;138(2):278–281. doi: 10.5858/arpa.2012-0639-RS. [DOI] [PubMed] [Google Scholar]
- 10.Biswas A., Ivaskevicius V., Thomas A., Oldenburg J. Coagulation factor XIII deficiency. Diagnosis, prevalence and management of inherited and acquired forms. Hämostaseologie. 2014;34(2):160–166. doi: 10.5482/HAMO-13-08-0046. [DOI] [PubMed] [Google Scholar]