Abstract
Epstein-Barr virus nuclear antigen 1 (EBNA1) is associated with the pathogenesis of Epstein-Barr virus-associated gastric carcinoma (EBVaGC). However, the function of EBNA1 in the growth of EBVaGC cells remains unclear. In the present study, the effects of silencing EBNA1, by RNA interference (RNAi), on the growth of EBVaGC cells were investigated in vitro and in vivo. A lentivirus-mediated RNAi targeting EBNA1 was transfected into the EBVaGC cell line GT-38. Reverse transcription-quantitative polymerase chain reaction (RT-qPCR), western blot analysis, MTT, colony formation and flow cytometry were performed to evaluate the biological behavior of GT-38 cells that were transfected with EBNA1 small interfering RNA (siRNA) in vitro. The effects of silencing EBNA1 on tumor growth were assessed in a tumor xenograft model using BALB/c nude mice. The results demonstrated that the proliferative and clonogenic abilities of GT-38 cells were significantly downregulated in response to EBNA1 siRNA (P<0.01). Furthermore, EBNA1 siRNA induced cell cycle arrest in the G0/G1 phase and promoted apoptosis of GT-38 cells (P<0.01). The tumorigenicity of GT-38 cells was significantly inhibited in the EBNA1 siRNA group. The results revealed that lentivirus-mediated RNAi of EBNA1 inhibited the growth of the EBVaGC cell line GT-38 in vitro and in vivo. Therefore, EBNA1 may be a potential target for gene therapy in EBVaGC.
Keywords: Epstein-Barr virus nuclear antigen 1, Epstein-Barr virus-associated gastric carcinoma, RNA interference, lentivirus
Introduction
Epstein-Barr virus (EBV) is the first human tumor virus to be identified, affecting >95% of the human population worldwide. EBV establishes a life-long persistent infection, causing a variety of human malignancies, including Burkitt's lymphoma, Hodgkin's lymphoma, nasopharyngeal carcinoma (NPC) and gastric cancer (GC) (1). EBV-associated (EBVaGC) accounts for ~7.5–10% of gastric carcinoma cases, which is estimated to exceed 75,000 cases/year (2,3). EBV is involved in the pathogenesis of EBVaGC. EBV is present in all tumor cells but not in the surrounding normal epithelium. EBVaGC exhibits unique morphological features (4). Further research on the key genes of EBV may provide novel targets for the treatment of EBVaGC.
EBVaGC cells express a well-defined set of latent genes including Epstein-Barr virus nuclear antigen 1 (EBNA1), EBV-encoded small RNA and latent membrane protein 2A. EBNA1 is a viral antigen expressed in all EBVaGC cells, and there are an increasing number of studies, which suggest that EBNA1 may alter the cellular environment and promote genomic instability, therefore leading to tumorigenesis (5–7). To the best of our knowledge, a limited number of studies have utilized EBV-positive gastric carcinoma cells containing a wild-type EBNA1 gene (8), including the GT-38 cell line.
The present study aimed to investigate the biological function of EBNA1 in gastric carcinoma. Gene silencing by RNA triggers an evolutionarily conserved process known as RNA interference (RNAi) (9). Lentiviral vectors have emerged as powerful vectors for gene transfer (10). Therefore, several experiments have been conducted to detect whether EBNA1 suppression could inhibit GT-38 cell proliferation in vitro and in vivo.
Materials and methods
Cell line and culture condition
EBVaGC cell line GT-38 and 293 cell lines were obtained from American Type Culture Collection (ATCC, Manassas, VA, USA) and cultured in RPMI-1640 (Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS; Excell Bio, Shanghai, China), 50 U/ml penicillin and 50 U/ml streptomycin (both from Thermo Fisher Scientific, Inc.) at 37°C in a humidified atmosphere containing 5% CO2. The medium was changed every 2 days and cells were passaged every 4–5 days.
Lentiviral infection
Small interfering RNAs (siRNAs) targeting the EBNA1 sequence were purchased from Dharmacon. The siRNA sequences for EBNA1 were: 3′-GGAGGTTCCAACCCGAAAT-5′. A non-silencing siRNA was used as a negative control (cat. no. D001810-01-20). One day before transfection, a total of 1×105 GT-38 cells in the logarithmic growth phase were seeded in 6-wells plates at 37°C in RPMI-1640 (10% FBS). 200 nM siRNA and 5 µl Lipofectamine 200 (Thermo Fisher Scientific, Inc.) were mixed in fresh RPMI-1640 (without FBS) and incubated for 20 min at room temperature. When the cell reached 80–90% confluence, the media was replaced with fresh RPMI-1640 (without FBS) and the mixtures was dropwise addition to cells. After 8 h, the media was replaced with fresh RPMI-1640 (supplemented with 10% FBS). At 48 h later, the cells were split for subsequent experiments. Three groups were used in the in vitro experiments, including untreated cells (Blank control group), cells transfected with non-silencing siRNA (Control siRNA group) and cells transfected with the EBNA1 siRNA (EBNA1 siRNA group).
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
GT-38 cells were harvested after infection. Total RNA was isolated from GT-38 cells using TRIzol (Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. RNA was transcribed into cDNA using the cDNA Synthesis kit (Thermo Fisher Scientific, Inc.). The cDNA was amplified using the SYBR-Green PCR Master Mix (Takara Biotechnology Co., Ltd., Dalian, China) according to the manufacturer's protocol. The thermocycling conditions were as follows: Initial denaturation of 95°C for 1 min followed by 40 cycles of 95°C for 5 sec and final extension of 60°C for 20 sec. The following primers were used: EBNA1 forward, 5′-CGCATCATAGACCGCCAGTA-3′ and reverse, 5′-CTGGCCCCTCGTCAGACAT-3; GAPDH forward, 5′-CTCAGACACCATGGGGAAGGTGA-3′ and reverse, 5′-ATGATCTTGAGGCTGTTGTCATA-3′. The reactions were performed in triplicate. The relative expression of target gene was evaluated using the 2−ΔΔCq method with GAPDH as the internal reference (11).
Western blot analysis
Protein lysates from cells were harvested using a radioimmunoprecipitation assay buffer (Beyotime Institute of Biotechnology, Haimen, China). The concentration of protein was determined using a bicinchoninic acid assay (Beyotime Institute of Biotechnology). Equal amounts of protein (10 µg) were separated by 10% SDS-PAGE and transferred onto polyvinylidene fluoride membranes (EMD Millipore, Billerica, MA, USA). The membranes were blocked with 5% non-fat milk for 1 h. Following blocking, the membranes incubated overnight at 4°C with he following primary antibodies: Anti-EBNA1 (cat. no. sc-81581, 1:10,000) and anti-GAPDH (cat. no. sc-66163, 1:10,000) (both from Santa Cruz Biotechnology, Inc., Dallas, TX, USA). The membranes were washed and incubated with horseradish peroxidase-conjugated goat anti-mouse with secondary antibodies for 1 h at room temperature (cat. no. sc-2005, 1:3,000; Santa Cruz Biotechnology, Inc.). The bands were detected using enhanced chemiluminescence (Thermo Fisher Scientific, Inc.). Densitometric analysis was performed using Quantity One 4.6.9 software (Bio-Rad Laboratories, Inc., Hercules, CA, USA). A total of three independent experiments were performed.
MTT assay
Following lentivirus infection, the viability of GT-38 cells was evaluated using a MTT assay at 24, 48 and 72 h. The cells were seeded in 96-wells plates at a cell density of 3,000 cells/well in 200 µl RPMI-1640. MTT solution was added into each well, and the cells were incubated at 37°C in a humidified atmosphere containing 5% CO2 for 4 h. Next, 150 µl acidic isopropanol (0.01 M HCl, 10% SDS, 5% isopropanol) was added in each well to stop the reaction. The absorbance was assessed at 450 nm using a microplate reader (Epoch; Bio-Rad Laboratories, Inc., Hercules, CA, USA). A total of 5 parallel MTT experiments were performed for each group. The experiments were performed in triplicates.
Colony formation assay
Following lentivirus transfection, GT-38-transfected cells were seeded into 6-cm dishes at a density of 8×102 cells cells/dish and cultured in RPMI-1640 at 37°C for 2 weeks. Then, the cells were fixed with 4% paraformaldehyde for 15 min, stained with Giemsa (both from Beijing Solarbio Science & Technology Co., Ltd., Beijing, China) for 20 min and washed twice with ddH2O. Visible colonies containing ≥50 cells were manually counted under fluorescence microscopy (Olympus Corporation, Tokyo, Japan). Image analysis was performed using Image-Pro® Plus (version 6.0; Media Cybernetics, Inc., Rockville, MD, USA). A total of 5 parallel experiments were performed for each group. The experiments were performed in triplicates.
Cell cycle analysis
Following lentivirus infection, GT-38 cells were seeded in 6-cm dishes at 5×104 cells/dish and incubated at 37°C for 48 h. The cells were harvested using 0.25% trypsin-EDTA and fixed with 70% ice-cold ethanol for 2 h. Then, the cells were resuspended in 0.1% sodium citrate, 0.1% Triton X-100 and 20 mg/ml propidium iodide (PI; BD Biosciences, Franklin Lakes, NJ, USA) for 1 h in the dark. At least 10,000 events were collected for each sample. The cells were analyzed using a flow cytometer (FACSCalibur™; BD Biosciences) and the results were analyzed using ModFit 3.0 software (Verity Software House, Inc., Topsham, ME, USA). Five parallel were performed for each group. The experiments were performed in triplicates.
Apoptosis assay
At 48 h post-transfection, a total of 1.0×106 cells were collected and stained with Annexin V-fluorescein isothiocyanate (FITC; BD Biosciences) and PI according to the manufacturer's protocol. Briefly, 1×106 cells were washed with 1X binding buffer and centrifuged at 300 × g for 10 min. The cell pellet was resuspended in 100 µl 1X binding buffer. Then, 10 µl Annexin V-FITC/106 cells were added, mixed and incubated for 15 min in the dark at room temperature prior to analysis by a flow cytometer. Five parallel were performed for each group. The experiments were performed in triplicate.
Tumor xenograft model
A total of 6 SPF male BALB/c nude mice (age, 4–6 weeks; weight, 20–24 g) were obtained from Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai, China), and were maintained inverse 12 light/dark cycle had free access food and water at room temperature under a specific pathogen-free condition. GT-38 cells (2×106 cells/tumor) were injected subcutaneously into the left axilla of nude mice. When the xenografts reached a size of approximately 0.5 cm in diameter, the mice were randomly divided into two groups (the EBNA1-siRNA and blank control group, 3 mice per group). Then the mice were injected with EBNA1-RNAi and Lipofectamine or Lipofectamine alone every 2 days for a total of 2 weeks. At 2 weeks of treatment, the mice were sacrificed and the tumors were harvested. All animal experiments in the present study were approved by the Ethics Committee of Linyi People's Hospital (Shandong, China).
Statistical analysis
All Statistical analysis were conducted using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). The relevant data are expressed as the mean ± standard deviation (SD). One-way analysis of variance followed by Bonferroni's post hoc test was used to examine differences among multiple groups. P<0.05 was considered to indicate a statistically significant difference.
Results
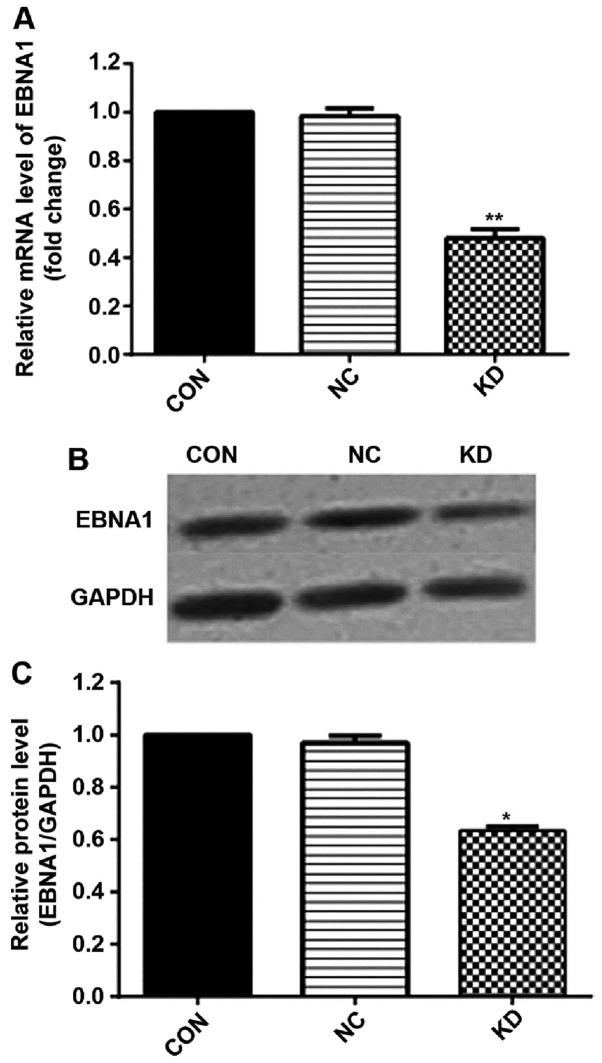
EBNA1 siRNA downregulates EBNA1 expression in GT-38 cells
The GT-38 cell line was selected to investigate the function of EBNA1 in EBVaGC. GT-38 cells were transfected using a lentiviral vector system expressing siRNA that targets EBNA1. RT-qPCR and western blot analysis revealed that mRNA and protein levels of EBNA1 exhibited a 52 and 42.7% reduction, respectively, in response to treatment with EBNA1-siRNA compared with the control-siRNA or blank control groups (Fig. 1A-C). These results indicated an efficient downregulation of EBNA1 using the lentiviral vector delivery system.
Figure 1.
EBNA1-siRNA downregulates the expression levels of EBNA1 in GT-38 cells. (A) EBNA1-siRNA downregulated the mRNA expression levels of EBNA1 in GT-38 cells. **P<0.01, n=5. (B) EBNA1-RNAi-LV downregulated the protein expression levels of EBNA1 in GT-38 cells. (C) Densitometric analysis of western blots from three independent experiments, respectively. β-actin was used as internal controls. *P<0.05 vs. the blank control groups. EBNA1, Epstein-Barr virus nuclear antigen 1; siRNA, small-interfering RNA.
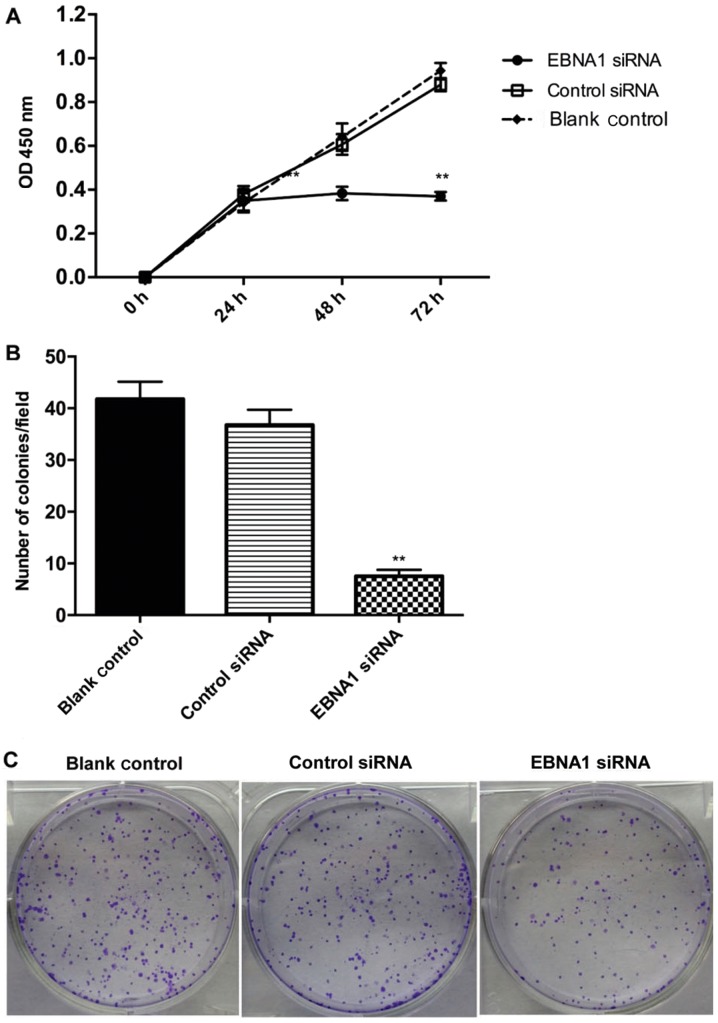
Knockdown of EBNA1 suppresses the viability and proliferation of GT-38 cells
The effects of knocking down EBNA1 on the viability and proliferation of GT-38 cells was evaluated using a MTT and colony forming assay. The results demonstrated that the knockdown of EBNA1 decreased the viability of GT-38 cells by 65% when compared with the blank control group (P<0.01; Fig. 2A). Furthermore, colony formation assay demonstrated that the knockdown of EBNA1 resulted in smaller and fewer colonies compared with the control siRNA and blank control groups (P<0.01; Fig. 2B and C). These results suggested EBNA1 might inhibit proliferation and suppress the clonogenic potential of GT-38 cells.
Figure 2.
Knockdown of EBNA1 suppresses the viability and proliferation of GT-38 cells. (A) Cell proliferation was determined using a MTT assay. A total of 5 parallel MTT assays were performed for each group. The experiments were performed in triplicates. (B) Cell proliferation in blank, control-siRNA and EBNA1-siRNA groups was evaluated using the colony formation assay. (C) Representative images of colonies in the blank, control-siRNA and EBNA1-siRNA groups. A total of three independent experiments were performed. **P<0.01 vs. the blank control groups. EBNA1, Epstein-Barr virus nuclear antigen 1; siRNA, small-interfering RNA; OD, optical density.
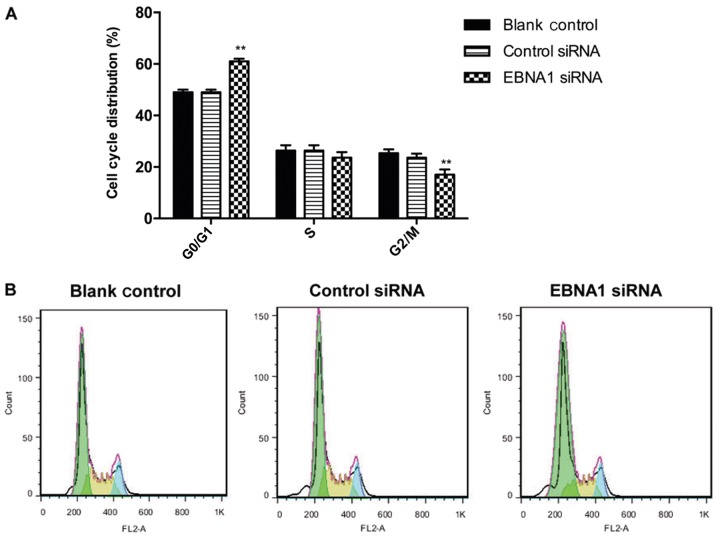
Knockdown of EBNA1 induces cell cycle arrest in the G0/G1 phase in GT-38 cells
Flow cytometric analysis of cell cycle distribution of EBNA1 siRNA-infected GT-38 cells was performed to examine how EBNA1 promotes the proliferation and colony formation potential of GT-38 cells. The results demonstrated a significant increase in the percentage of cells in the G0/G1 phase and a decreased number of cells in the G2/M phase (P<0.01) in response to treatment with EBNA1 siRNA (Fig. 3). However, no differences in cell numbers were observed in the S phase in the EBNA1 siRNA group compared with the control siRNA and blank control groups (Fig. 3). These results suggested that down regulating EBNA1 might induce cell cycle arrest in the G0/G1 phase.
Figure 3.
Knockdown of EBNA1 induces G0/G1 phase arrest in GT-38 cells. (A) The proportion of cells in the G0/G1 phase was significantly increased, whereas the proportion of cells in the G2/M phase was decreased in the EBNA1-siRNA group compared with the control siRNA and blank control groups. Three individual experiments were performed. **P<0.01 vs. the blank control groups (B) Flow cytometric analysis demonstrated EBNA1-RNAi induced cell cycle arrest in the G0/G1 phase in GT-38 cells. EBNA1, Epstein-Barr virus nuclear antigen 1; siRNA, small-interfering RNA; RNAi, RNA interference.
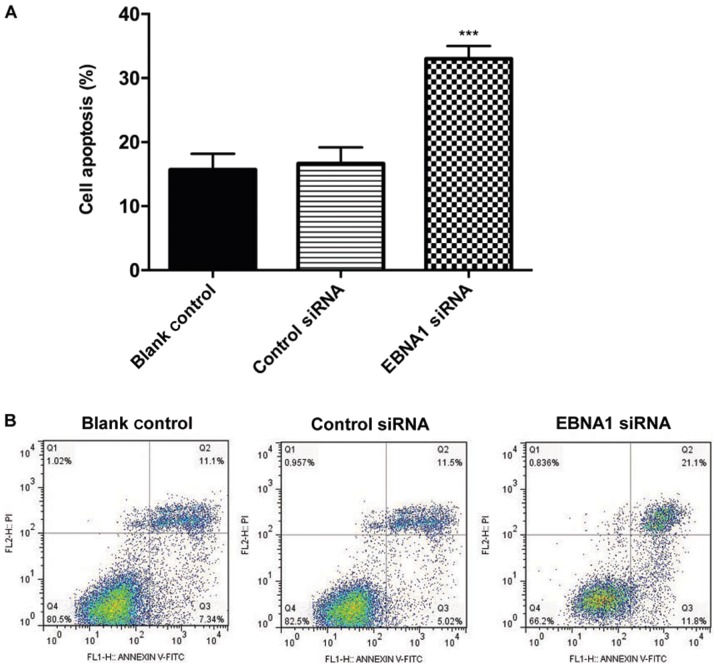
Knockdown of EBNA1 induces the apoptosis of GT-38 cells
The effects of downregulating EBNA1 on the apoptosis of GT-38 cells was examined by Annexin V/PI double staining and flow cytometry. The results demonstrated that the downregulation of EBNA1 promoted apoptosis (Fig. 4). The percentage of early and late apoptotic cell population increased by 11.8 and 21.1% in the EBNA1-siRNA group compared with the control-siRNA and blank control groups, respectively (P<0.01; Fig. 4). These results indicated that the knockdown of EBNA1 might promote cell apoptosis in EBVaGC cells.
Figure 4.
Knockdown of EBNA1 promotes the apoptosis of GT-38 cells. (A) Flow cytometric analysis of apoptosis at 48 h post-transfection with EBNA1-siRNA. EBNA1-RNAi significantly promoted cell apoptosis. Three individual experiments were performed. ***P<0.001 vs. the blank control group. (B) Representative images of Annexin V/PI double staining and flow cytometric analysis of apoptosis in response to treatment with EBNA1-siRNA. The cells in the lower left, lower right, upper right and upper left quadrant correspond to viable, early apoptotic, late apoptotic or necrotic cells, respectively. EBNA1, Epstein-Barr virus nuclear antigen 1; siRNA, small-interfering RNA; RNAi, RNA interference; FITC; fluorescein isothiocyanate; PI, propidium iodine.
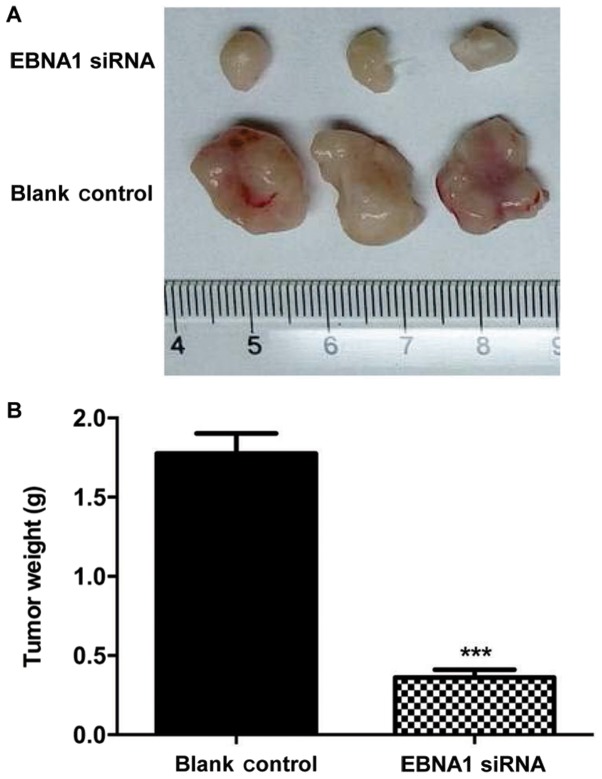
Knockdown of EBNA1 inhibits the growth of GT-38 cells in vivo
To study the in vivo tumorigenic potential of EBNA1, GT-38 cells were inoculated under the skin of nude mice and the mice were injected with EBNA1-siRNA with lipofectamine or lipofectamine alone. After 2 weeks, tumor development was observed in the control group (Fig. 5A). The median tumor weight was significantly decreased by >79.7% (P<0.001; Fig. 5B) in the EBNA1-siRNA group, suggesting that downregulating EBNA1 may inhibit the growth GT-38 cells in vivo.
Figure 5.
Knockdown of EBNA1 inhibits the growth of GT-38 cells in vivo. (A) Images of tumors that were extracted after 2 weeks. (B) Tumor weights were significantly decreased in response to treatment with EBNA1-siRNA. n=3 mice per group; ***P<0.001 vs. the blank siRNA group. EBNA1, Epstein-Barr virus nuclear antigen 1; siRNA, small-interfering RNA.
Discussion
Tumor viruses account for 50% of cases of human cancer (4), which may be increasing as novel human tumor viruses are being identified. In order to identify these types of virus-associated cancer, it is essential to examine the viral ability to maintain tumor phenotypes; therefore providing a non-host target for therapeutic interventions. EBV has been associated with the pathogenesis of GC (12). The present study investigated the underlying molecular mechanisms by which EBV might contribute to the development of EBVaGC that is mediated by EBNA1.
EBNA1 has been considered to be a novel biomarker of human GS (13). The results of the present study demonstrated that transfection with a specific siRNA that targets EBNA1 decreases the mRNA and the protein levels of EBNA1 by 52 and 42.7%, respectively. Ian et al (14), demonstrated that the silencing of EBNA1 leads to decreased proliferation and apoptosis of EBV-positive natural killer (NK)/T cell lymphoma cells. The results of the present study demonstrated that the proliferation of EBVaGC cells was significantly decreased by 65% in response to treatment with EBNA1-siRNA. Sivachandran et al (15) demonstrated that EBNA1 causes the disruption of promyelocytic leukemia (PML) nuclear bodies (NBs) in nasopharyngeal carcinoma (NPC) cells. A previous study demonstrated that human adenocarcinoma cell lines that contain an integrated EBNA1 expression cassette exhibited a decreased activation of p53 and cell apoptosis as well as an increased survival rate (16). Additionally, the knockdown of EBNA1 might decrease the proliferative and colony formation abilities of SKOV3 ovarian cancer cells (17), Burkitt's lymphoma Raji cells (18) and NPC cells (19) by inducing G0/G1 phase arrest. The results of the present study demonstrated that the downregulation of EBNA1 negatively regulated the progression of gastric cancer via induction of cell cycle arrest and late apoptosis in GT-38 cells. Our results are consistent with the results from the aforementioned studies.
To investigate the effects of EBNA1 on the proliferation of gastric cancer cells in vivo, BALB/c nude mice were inoculated with GT-38 cell tumors that were treated with continued intratumoral injection of EBNA1 siRNA. The results demonstrated that silencing EBNA1 downregulated tumor weight by 79.7% in the gastric cancer tumor xenografts compared with the control group. These results indicated that downregulation of EBNA1 by RNAi significantly inhibited the growth of GT-38 gastric cancer cells in vitro and in vivo.
The molecular mechanisms by which EBNA1 may facilitate viral replication and maintain viral episome are unclear. Saridakis et al (20), demonstrated that EBNA1 might decrease the levels of p53 by sequestering the ubiquitin-specific protease 7N. Sivachandran et al (4) demonstrated that EBNA1 caused the disruption of PML NBs, which serve important functions in apoptosis, activation of p53 and tumor suppression, indicating that EBV infection of GC cells might lead to EBNA1-mediated disruption of PML NBs. The present study demonstrated that knocking down EBNA1 might decrease proliferation and induce apoptosis in EBVAGC cells, which might be caused by the loss of PML NBs. However, future studies are required to confirm the results of the present study and investigate novel therapies for EBVAGC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
JW, FM, XX and YW designed and performed the experiments. JW, LL and CL interpreted the experimental results, wrote and revised the manuscript. All authors contributed to this manuscript. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
All animal experiments in the present study were approved by the Ethics Committee of Linyi People's Hospital (Shandong, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Daskalogianni C, Pyndiah S, Apcher S, Mazars A, Manoury B, Ammari N, Nylander K, Voisset C, Blondel M, Fåhraeus R. Epstein-Barr virus-encoded EBNA1 and ZEBRA: Targets for therapeutic strategies against EBV-carrying cancers. J Pathol. 2015;235:334–341. doi: 10.1002/path.4431. [DOI] [PubMed] [Google Scholar]
- 2.Nishikawa J, Yoshiyama H, Iizasa H, Kanehiro Y, Nakamura M, Nishimura M, Saito M, Okamoto T, Sakai K, Suehiro Y, et al. Epstein-Barr Virus in Gastric Carcinoma. Cancers. 2014;6:2259–2274. doi: 10.3390/cancers6042259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen JN, Ding YG, Feng ZY, Li HG, He D, Du H, Wu B, Shao CK. Association of distinctive Epstein-Barr virus variants with gastric carcinoma in Guangzhou, southern China. J Med Virol. 2010;82:658–667. doi: 10.1002/jmv.21731. [DOI] [PubMed] [Google Scholar]
- 4.Sivachandran N, Dawson CW, Young LS, Liu FF, Middeldorp J, Frappier L. Contributions of the Epstein-Barr virus EBNA1 protein to gastric carcinoma. J Virol. 2012;86:60–68. doi: 10.1128/JVI.05623-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy G, Komano J, Sugden B. Epstein-Barr virus provides a survival factor to Burkitt's lymphomas. Proc Natl Acad Sci USA. 2003;100:14269–14274. doi: 10.1073/pnas.2336099100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young SL, Dawson WC, Eliopoulos GA. The expression and function of Epstein-Barr virus encoded latent genes. Mol Pathol. 2000;53:238–247. doi: 10.1136/mp.53.5.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Humme S, Reisbach G, Feederle R, Delecluse HJ, Bousset K, Hammerschmidt W, Schepers A. The EBV nuclear antigen 1 (EBNA1) enhances B cell immortalization several thousandfold. Proc Natl Acad Sci USA. 2003;100:10989–10994. doi: 10.1073/pnas.1832776100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iizasa H, Nanbo A, Nishikawa J, Jinushi M, Yoshiyama H. Epstein-Barr virus (EBV)-associated gastric carcinoma. Viruses. 2012;4:3420–3439. doi: 10.3390/v4123420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hannon GJ. RNA interference. Nature. 2002;418:244–251. doi: 10.1038/418244a. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Z, Wang J, Shen B, Peng C, Zheng M. The ABCC4 gene is a promising target for pancreatic cancer therapy. Gene. 2012;491:194–199. doi: 10.1016/j.gene.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 11.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Ma BB, Chan AT, Chan FK, Murray P, Tao Q. Epstein-Barr virus-induced epigenetic pathogenesis of viral-associated lymphoepithelioma-like carcinomas and natural killer/T-cell lymphomas. Pathogens. 2018;7:E63. doi: 10.3390/pathogens7030063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tokunaga M, Land CE. Epstein-Barr virus involvement in gastric cancer: Biomarker for lymph node metastasis. Cancer Epidemiol Biomarkers Prev. 1998;7:449–450. [PubMed] [Google Scholar]
- 14.Ian MX, Lan SZ, Cheng ZF, Dan H, Qiong LH. Suppression of EBNA1 expression inhibits growth of EBV-positive NK/T cell lymphoma cells. Cancer Biol Ther. 2008;7:1602–1606. doi: 10.4161/cbt.7.10.6564. [DOI] [PubMed] [Google Scholar]
- 15.Sivachandran N, Sarkari F, Frappier L. Epstein-Barr nuclear antigen 1 contributes to nasopharyngeal carcinoma through disruption of PML nuclear bodies. PLoS Pathog. 2008;4:e1000170. doi: 10.1371/journal.ppat.1000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frappier L. Contributions of Epstein-Barr nuclear antigen 1 (EBNA1) to cell immortalization and survival. Viruses. 2012;4:1537–1547. doi: 10.3390/v4091537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chuang TC, Lee YJ, Liu JY, Lin YS, Li JW, Wang V, Law SL, Kao MC. EBNA1 may prolong G(2)/M phase and sensitize HER2/neu-overexpressing ovarian cancer cells to both topoisomerase II-targeting and paclitaxel drugs. Biochem Biophys Res Commun. 2003;307:653–659. doi: 10.1016/S0006-291X(03)01235-X. [DOI] [PubMed] [Google Scholar]
- 18.Hong M, Murai Y, Kutsuna T, Takahashi H, Nomoto K, Cheng CM, Ishizawa S, Zhao QL, Ogawa R, Harmon BV, et al. Suppression of Epstein-Barr nuclear antigen 1 (EBNA1) by RNA interference inhibits proliferation of EBV-positive Burkitt's lymphoma cells. J Cancer Res Clin Oncol. 2006;132:1–8. doi: 10.1007/s00432-005-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yin Q, Flemington EK. siRNAs against the Epstein-Barr virus latency replication factor, EBNA1, inhibit its function and growth of EBV-dependent tumor cells. Virology. 2006;346:385–393. doi: 10.1016/j.virol.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 20.Saridakis V, Sheng Y, Sarkari F, Holowaty MN, Shire K, Nguyen T, Zhang RG, Liao J, Lee W, Edwards AM, et al. Structure of the p53 binding domain of HAUSP/USP7 bound to Epstein-Barr nuclear antigen 1 implications for EBV-mediated immortalization. Mol Cell. 2005;18:25–36. doi: 10.1016/j.molcel.2005.02.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.