Abstract
Background:
Large wounds following surgery for neural tube defects are difficult to close; physical wound characteristics such as position and dimension would serve as a guide for their surgical closure.
Aim:
To study how wound dimension determines the choice between primary and rhomboid flap closure of skin defects following surgery for neural tube defects.
Materials And Methods:
A retrospective study was carried out on cases of neural tube defects operated in the department of paediatric surgery at a tertiary center for 3 years from January 2015 to December 2017. Data regarding clinical features, location, wound dimensions following surgery, any bony deformity, method of closure used, distance of wound from anus, and postoperative complications were collected and analyzed.
Results:
A total of 114 cases were operated during this period; 86/114 had primary closure, whereas 28/114 needed rhomboid flap for tension-free cover. Primarily closed wounds had a biphasic distribution of (long axis)/(short axis) ratio (with values either >1.65 or <0.63), whereas those covered by rhomboid flaps had a mean ratio of 1.25 (range, 0.71–1.45). All six cases with bony deformity needed rhomboid flaps. Although all lipomeningomyelocele defects could be primarily closed, all rachischisis needed flap cover. Infected lesions had a mean wound distance of 5.3cm from posterior anal margin.
Conclusion:
Defect’s position, its size and shape, and any bony deformity determine the choice of closure of postoperative wound. The versatile, safe, and universal rhomboid flap is an aesthetic solution to the large skin defects in patients of neural tube defects.
Keywords: Neural tube defects, primary wound closure, rhomboid flap
Introduction
Key message: Wound dimensions, its area, and nature of neural tube defect have an important role in determining the choice of wound closure after surgery.
Compared to the worldwide prevalence of neural tube defects (NTD) of around 300,000 per year, recent Indian data show a higher overall pooled prevalence of 4.5/1,000 live births.[1,2] We commonly encounter large defects after excision of the primary lesion, which if closed primarily often dehisce and increase the morbidity and cost of care. Several reconstructive methods using local cutaneous, fasciocutaneous, myocutaneous, and graft procedures have been described in literature.[3] This retrospective study was an attempt to summarize the wound characteristics and the results of wound closure with local rhomboid flaps in case of large defects.
Materials and Methods
This was a retrospective cohort study performed over 3 years from January 2015 to December 2017 in the department of paediatric surgery at a tertiary care hospital after approval by the institutional ethics committee. All the cases of NTD operated during this period were included after obtaining written informed consent from each patient’s parent.
Data regarding nature of the lesion (meningomyelocele (MMC)/meningocele/rachischisis/lipo-MMC), its location, its dimension (maximum transverse diameter [X], maximum vertical diameter [Y] of the wound, and the transverse diameter [Z] of the back passing through the center of the wound in between both posterior axillary lines) [Figure 1], whether leaking, any bony deformity, availability of surrounding skin, method of closure of postoperative defects, and postoperative complications were collected. Data thus collected were analyzed statistically by calculating the mean and range of the data for different measures. The dimensions of the wound were measured after excision of the sac and closure of the dura.
Figure 1.
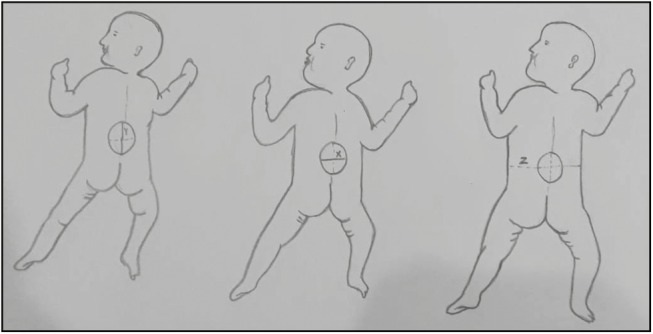
Transverse (X) and vertical (Y) wound dimension and transverse diameter of back (Z)
Raising a Rhomboid Flap for Large Defects
Our protocol is to avoid primary closure with tension in all surgical wounds. Large defects, which would be impossible to close without tension, are closed using universal rhomboid flaps, provided ample skin is available on any of the sides of the wound. These flaps are versatile fasciocutaneous flaps, whose advantages have been described by Limberg.[4] While raising a rhomboid flap, incision with length equivalent to one of the sides of the rhomboid defect is given perpendicular to defect’s long axis and a second incision is given parallel to the side of the defect from the end of this perpendicular line [Figure 2]. This flap is then mobilized in the fasciocutaneous plane and transposed to cover the primary defect, which distributes the tension of primary wound closure [Figure 3].
Figure 2.

Post-excision wound with incision for rhomboid flap
Figure 3.

Transposed rhomboid flap over wound
Results
Demography and lesion characteristics: Table 1 describes the lesion characteristics.
-
Wound characteristics for primary closure vs. flap cover: Table 2 summarizes the wound characteristics of the wounds closed primarily and those using flap cover.
Figure 4 shows the wound dimension results and the method of closure chosen in the study.
Postoperative complications in flap cover wounds: Table 3 describes the postoperative complications.
Table 1.
Demography and lesion characteristics
| Total no. of operated patients | 114 (N) |
| Mean age at surgery | 83.8 days (range, 4 days to 3.5 years) |
| Type of NTD | MMC, 68 (59.65%); lipo-MMC, 28 (24.56%); rachischisis, 6 (5.26%); meningocele, 12 (10.53%) |
| Location of NTD | Lumbosacral, 101 (88.6%); cervical, 8 (7%); thoracic, 3 (2.6%); sacral, 2 (1.7%) |
| Leaking MMC | 9 (operated in emergency) |
| Bony deformity | Kyphosis, 6 |
| Primary closure:flap cover | 86:28 (24.56% needed flap cover) |
Table 2.
Wound characteristics for primary closure vs. flap cover
| Nature of wound closure | Wound characteristics |
|---|---|
| Primary closure | X/Y ratio, biphasic distribution (either <0.63 or >1.65) |
| Mean Z/X, 3.3 | |
| Average defect area, 45.4cm2 | |
| All lipo-MMC primarily closed | |
| Flap cover | X/Y ratio, ranged from 0.71 to 1.45 (mean, 1.25) |
| Mean Z/X, 2.3 | |
| Average defect size, 55.6cm2 | |
| All patients with rachischisis and kyphosis needed flap cover |
Figure 4.
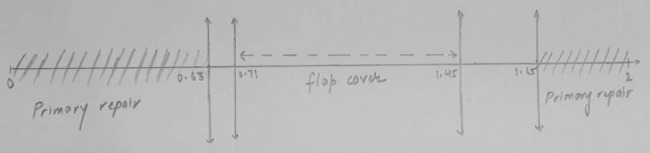
Line diagram showing ratio (X/Y) in relation to method of wound closure
Table 3.
Postoperative complications in flap cover wounds
| Wound infection | 2 |
| Dehiscence | 1 (at tip) |
| Hematoma | 1 |
| Flap necrosis | 0 |
| Mean postoperative stay | 7.4 days |
| Mean stay in cases of wound complications | 20.2 days |
Infected lesions had a mean wound distance of 5.3cm from posterior anal margin
Discussion
Every fourth patient who undergoes surgery for NTD will have a large wound, difficult to be closed primarily.[5] Effective closure provides tension-free repair, ensuring adequate soft tissue cover of the repaired site; thereby preventing cerebrospinal fluid leakage and promoting wound healing, especially in larger defects. Different local flaps and grafts have been described with variable results in literature.[6,7,8] Rhomboid flaps, often popularly known as Limberg flap, are universal, versatile fasciocutaneous flaps, which can be raised at any site where ample skin surrounds the defect.[4] These flaps have been extensively used throughout the body with considerable success.[9] In our study, 24.56% patients needed rhomboid flap for wound closure. This is comparable to the findings of Bevan et al.,[10] who in their study of post-MMC excision defects closure observed that as many as 22.5% of their patients needed additional plastic surgical procedure to achieve tension-free wound closure.
Factors determining the choice of closure of postsurgical wounds in patients with NTD have been studied earlier; nature of NTD, its size and location, any underlying bony deformity, and amount of soft tissue available for closure are instrumental in choosing appropriate surgical options.[6] A few studies have classified the defect according to the size of one axis, thereby defining large defects as those exceeding 5cm in diameter and considering the need for additional procedures and prolonged admission after surgery.[11,12] But, we have observed that it is not one dimension, which needs measurement for decision, rather both dimensions (in long axis) play equally important role, much more important is the relative ratio of these dimensions along with the area of the defect to guide toward a proper decision. We concluded that squarer defects with a range of axis ratio (X/Y) from 0.71 to 1.45 needed a flap cover; as against this, oval defects with axis ratios (<0.63 or >1.65) could be primarily closed without much complications. In lesions that have ratio value between 0.63 and 0.71 or 1.45 and 1.65, we believe that it would be better to close them using rhomboid flap to ensure better results. Also, although all lipo-MMC could be closed primarily, all six patients with kyphosis and six patients with rachischisis needed rhomboid flaps for wound closure. In a recent study, Kemaloğlu et al.[5] emphasized the importance of ratio of the dimensions of the wound in decision-making for wound closure. Campobasso et al.[8] found Limberg’s flap to provide stable wound closure with minimal complications in their series of large MMC.
The simplicity in the technique of raising rhomboid flap and its safety makes it a versatile option to be used universally where adequate skin is available.[13,14,15]
Minor complications were present in 4/28 (14.3%) patients having rhomboid flap cover, which were managed conservatively. Other investigators have also reported similar complication rates.[5,6,8] Infected lesions were located closer to the posterior anal margin (mean distance, 5.3cm).
Conclusion
We concluded that the versatile, safe, and universal rhomboid (Limberg’s) flap is an aesthetic solution to the large skin defects in patients of NTD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Flores AL, Vellozzi C, Valencia D, Sniezek J. Global burden of neural tube defects, risk factors, and prevention. Indian J Community Health. 2014;26:3–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Allagh KP, Shamanna BR, Murthy GV, Ness AR, Doyle P, Neogi SB, et al. Wellcome Trust-PHFI Folic Acid project team. Birth prevalence of neural tube defects and orofacial clefts in India: a systematic review and meta-analysis. PLoS One. 2015;10:e0118961. doi: 10.1371/journal.pone.0118961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kesan K, Kothari P, Gupta R, Gupta A, Karkera P, Ranjan R, et al. Closure of large meningomyelocele wound defects with subcutaneous based pedicle flap with bilateral V-Y advancement: our experience and review of literature. Eur J Pediatr Surg. 2015;25:189–94. doi: 10.1055/s-0034-1368796. [DOI] [PubMed] [Google Scholar]
- 4.Limberg AA. Modern trends in plastic surgery. Design of local flaps. Mod Trends Plast Surg. 1966;2:38–61. [PubMed] [Google Scholar]
- 5.Kemaloğlu CA, Özyazgan İ, Ünverdi ÖF. A decision-making guide for the closure of myelomeningocele skin defects with or without primary repair. J Neurosurg Pediatr. 2016;18:187–91. doi: 10.3171/2016.2.PEDS15702. [DOI] [PubMed] [Google Scholar]
- 6.Shim JH, Hwang NH, Yoon ES, Dhong ES, Kim DW, Kim SD. Closure of myelomeningocele defects using a Limberg flap or direct repair. Arch Plast Surg. 2016;43:26–31. doi: 10.5999/aps.2016.43.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-khatib HA. Large thoracolumbar meningomyelocele defects: incidence and clinical experiences with different modalities of latissimus dorsi musculocutaneus flap. Br J Plast Surg. 2004;57:411–7. doi: 10.1016/j.bjps.2003.12.035. [DOI] [PubMed] [Google Scholar]
- 8.Campobasso P, Pesce C, Costa L, Cimaglia ML. The use of the Limberg skin flap for closure of large lumbosacral myelomeningoceles. Pediatr Surg Int. 2004;20:144–7. doi: 10.1007/s00383-003-1056-8. [DOI] [PubMed] [Google Scholar]
- 9.Aydin OE, Tan O, Algan S, Kuduban SD, Cinal H, Barin EZ. Versatile use of rhomboid flaps for closure of skin defects. Eurasian J Med. 2011;43:1–8. doi: 10.5152/eajm.2011.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bevan R, Wilson-Jones N, Bhatti I, Patel C, Leach P. How much do plastic surgeons add to the closure of myelomeningoceles? Childs Nerv Syst. 2018;34:737–40. doi: 10.1007/s00381-017-3674-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherian J, Staggers KA, Pan IW, Lopresti M, Jea A, Lam S. Thirty-day outcomes after postnatal myelomeningocele repair: a national surgical quality improvement program pediatric database analysis. J Neurosurg Pediatr. 2016;18:416–22. doi: 10.3171/2016.1.PEDS15674. [DOI] [PubMed] [Google Scholar]
- 12.Sherrod BA, Johnston JM, Rocque BG. Risk factors for unplanned readmission within 30 days after pediatric neurosurgery: a nationwide analysis of 9799 procedures from the American College of Surgeons National Surgical Quality Improvement Program. J Neurosurg Pediatr. 2016;18:350–62. doi: 10.3171/2016.2.PEDS15604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gwynn BR, Williams CR. Use of the Limberg flap to close breast wounds after partial mastectomy. Ann R Coll Surg Engl. 1985;67:245–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Gümüş N. A new approach to the antecubital scar contracture: rhomboid rotation flap. J Plast Reconstr Aesthet Surg. 2010;63:1392–3. doi: 10.1016/j.bjps.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010;40:757–62. doi: 10.1007/s00595-008-4098-7. [DOI] [PubMed] [Google Scholar]


