Abstract
Background
Whether outdoor time is linked to dietary patterns of children has yet to be empirically tested. The objective of this study was to examine the association between outdoor time and dietary patterns of children from 12 countries around the world.
Methods
This multinational, cross-sectional study included 6229 children 9–11 years of age. Children self-reported the time that they spent outside before school, after school and on weekends. A composite score was calculated to reflect overall daily outdoor time. Dietary patterns were assessed using a food frequency questionnaire, and two components were used for analysis: healthy and unhealthy dietary pattern scores.
Results
On average, children spent 2.5 h outside per day. After adjusting for age, sex, parental education, moderate-to-vigorous physical activity, screen time and body mass index z-score, greater time spent outdoors was associated with healthier dietary pattern scores. No association was found between outdoor time and unhealthy dietary pattern scores. Similar associations between outdoor time and dietary patterns were observed for boys and girls and across study sites.
Conclusions
Greater time spent outside was associated with a healthier dietary pattern in this international sample of children. Future research should aim to elucidate the mechanisms behind this association.
Keywords: diet, eating behavior, food intake, outside, pediatric
Background
Non-communicable diseases such as obesity, type 2 diabetes and cardiovascular diseases are a major burden worldwide. Unhealthy diets and lack of physical activity are two important modifiable behavioral risk factors that have been shown to increase the risk of developing non-communicable diseases.1,2 The consumption of energy-dense and nutrient-poor foods has become a fixture of today’s food environment,3 while habitual physical activity levels have decreased such that few children achieve the recommended 60 min of moderate-to-vigorous physical activity (MVPA) required each day for good health.4 Strategies that can help to improve diet and enhance physical activity levels of children are very much needed.
Recent evidence suggests that the current generation of children play outside less frequently and for shorter durations than their parents’ generation.5 Reasons for this shift from outdoor to indoor play include the prioritization of academic achievement,6 an overload of extracurricular activities,7 safety concerns8 and interest for indoor screen-based activities.9 Thus, physical activity is moving away from unstructured and unsupervised outdoor play towards structured and supervised indoor activities.10 Whether this shift is linked to changes in eating behaviors of children is, however, unknown.
Anecdotal evidence suggests that greater time spent indoors results in increased food intake (i.e. less inhibited eating behavior, increased snacking) tied to availability and convenience to household stored food items. Conversely, greater time spent outside may be associated with better dietary patterns due to clustering of healthy lifestyle behaviors in children. However, these claims have yet to be empirically tested. What is currently known is that children with higher amounts of outdoor time engage in greater amounts of physical activity and lower amounts of sedentary behavior than children who spend less time outdoors.11 Given the recent societal shift from outdoor to indoor play, it is important to also understand the implications of this new reality on dietary patterns of children if we want to better inform the development of effective interventions aimed at improving lifestyle behaviors and, ultimately, reduce the incidence of non-communicable diseases and improve quality of life. Examining how outdoor time may be linked to dietary patterns of children across countries at different levels of economic and human development is also important in order to inform public health policies and tailor interventions that are context and setting-specific.
The objective of this study was to investigate for the first time the association between outdoor time and dietary patterns of children from low- and high-income settings, situated in all inhabited continents of the world. We hypothesized that greater time spent outdoor would be associated with a healthier dietary pattern in children, irrespective of geographic location.
Methods
Study design and setting
The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) is a cross-sectional, multinational study designed to examine the relationships between lifestyle behaviors and obesity in 12 study sites located in Australia, Brazil, Canada, China, Colombia, Finland, India, Kenya, Portugal, South Africa, the UK and the USA. These countries represent a wide range of economic development (low to high income), Human Development Index (0.509 in Kenya to 0.929 in Australia), and inequality (Gini index of 26.9 in Finland to 63.1 in South Africa).12 The rationale, design and methods of ISCOLE have previously been published in detail elsewhere.12 The primary sampling frame was schools, which were typically stratified by an indicator of socioeconomic status to maximize variability within sites. In an effort to maximize comparisons across ISCOLE sites, the sampling frame included students from urban and suburban areas only. Rural areas were excluded from the sampling frame due to logistical concerns related to data collection raised by site investigators located in research institutes without access to rural populations. Some of the instruments have also not been adapted for use in rural areas. Data collection was conducted during the school year across all sites and was split into phases to cover the spanned seasons. This approach was used to minimize the influence of seasonality on the findings. A standardized protocol was used to collect data across all sites, and all study personnel underwent rigorous training and certification to ensure data quality. The Pennington Biomedical Research Center Institutional Review Board as well as Institutional/Ethical Review Boards at each site approved the study. Written informed consent was obtained from parents/legal guardians, and child assent was also obtained as required by local ethics review boards. Data were collected during the school year at each study site and occurred between September 2011 and December 2013.
Participants
ISCOLE targeted grade levels likely to ensure minimal variability around a mean age of 10 years. All children within the targeted grade level in a sampled school were eligible to participate; hence, the sample included 9–11-year-old children. Based on a priori sample size and power calculations,12 each site aimed to recruit a sex-balanced sample of at least 500 children. Of the 7372 children who participated in ISCOLE, a total of 6229 remained in the analytical sample after excluding participants without information on outdoor time (n = 53), valid physical activity data (n = 800), information on screen time (n = 2), reported level of parental education (n = 283), and body mass index (BMI) z-scores (n = 5). Except for significantly higher BMI z-scores, children who were excluded for missing data did not significantly differ from those who were included in the present analysis.
Measurements
Outdoor time
Children were asked to complete a Diet and Lifestyle Questionnaire which included items about outdoor time.12 Specifically, children were asked: ‘On a school day, how much time did you spend outside before school?’; ‘On a school day, how much time did you spend outside after school before bedtime?’; and ‘On a weekend day, how much time did you spend outside?’. Response options were: ‘<1 h’, ‘1 h’, ‘2 h’, ‘3 h’, ‘4 h’, and ‘5 or more hours’. A composite score was also calculated to reflect ‘overall outdoor time’ in hours per day. To do so, the response options ‘<1 h’ and ‘5 or more hours’ were converted to 0.5 and 5 h, respectively. Outdoor time before and after school were then summed to obtain the time spent outside on weekdays. Outdoor time in hours per week was calculated as: (5 × outdoor time on weekdays) + (2 × outdoor time on weekend days). Finally, the result was divided by 7 to obtain overall daily outdoor time (h/day).
Dietary patterns
Dietary patterns of children were assessed using a food frequency questionnaire (FFQ) adapted from the Health Behavior in School-aged Children Survey.13,14 The FFQ asks about usual consumption of 23 different food groups, with response options including ‘never’, ‘less than once a week’, ‘once a week’, ‘2–4 days a week’, ‘5–6 days a week’, ‘once a day every day’ and ‘more than once a day’. This FFQ has been reported to be reliable (r = 0.52–0.82) for ranking the frequency of consumption of food items in children.15 Dietary patterns were examined by employing principal components analyses to identify derived variables (components). Reported frequencies were converted into portions per week, and analyses were performed using the total sample and for each country separately. Eigenvalues and a scree plot analysis were used as the criteria for deciding the number of components extracted. The two criteria led to similar conclusions and two components were chosen for analysis. The components were then rotated using an orthogonal varimax transformation to force non-correlation of the components and to enhance their interpretation. The two components represented a ‘healthy dietary pattern’ (with positive loadings for vegetables, fruit, whole grains, low-fat milk, etc.) and an ‘unhealthy dietary pattern’ (with positive loadings for fast food, hamburgers, soft drinks, sweets, fried food, etc.). The component scores computed were standardized to ensure normality, and higher values for each score represent either a ‘healthier’ or ‘unhealthier’ dietary pattern, respectively. Most of the food items in both components were common for all 12 countries. For this analysis, we have chosen to use the country-specific component scores to be more representative of each site, although the differences between these and the component scores from the pooled data were small.14
Covariates
Age, sex, level of parental education, physical activity level, screen time, and BMI z-scores were included as covariates in statistical models. Highest level of parental education was used as a proxy measure of socioeconomic status and coded into three categories based on the highest level of education attained by either parent: ‘did not complete high school’, ‘completed high school or some college’, or ‘completed bachelor’s or postgraduate degree’. Physical activity data were obtained via a 24-h protocol using waist-worn accelerometers (Actigraph GT3X+, ActiGraph LLC, Pensacola, FL, USA), as described in detail elsewhere.16 After removal of sleep duration from the data file using a published algorithm,17,18 awake non-wear time was defined as at least 20 consecutive minutes of zero activity counts,19 and MVPA was defined as all activity ≥574 counts per 15 s.20 Child-reported screen time was assessed using questions from the US Youth Risk Behavior Surveillance System.21 Children were asked to report how many hours they typically watched TV, and how many hours they played video games and/or used the computer per weekday, and per weekend day. As previously reported,22 a daily average screen time was calculated by weighting the responses for each question (2/7 for weekend and 5/7 for weekday). Height and body weight were objectively measured using standardized procedures by trained and certified study personnel.12 BMI (kg/m2) was calculated and age- and sex-specific BMI z-scores were computed using reference data from the World Health Organization.23
Statistical analysis
Statistical analyses were performed using JMP version 13 and SAS version 9.4 (SAS Institute, Cary, NC, USA). Multilevel mixed-effects models accounting for clustering at the school and study site levels were used to examine the relationships between outdoor time (weekday before/after school, weekend day, overall) and dietary patterns (healthy dietary pattern score and unhealthy dietary pattern score). Study sites were considered to have fixed effects, and school nested within study sites were viewed as having random effects. The denominator degrees of freedom for statistical tests pertaining to fixed effects were calculated using the Kenward and Roger approximation.24 Age, sex, highest level of parental education, MVPA time, screen time and BMI z-scores were included as covariates in statistical models. Trends in dietary patterns were also examined across quintile categories of overall daily outdoor time. The level of significance was set at P < 0.05 for all analyses.
Results
Table 1 presents descriptive characteristics of the sample. Children engaged in ~60 min/day of MVPA and spent ~3 h/day in screen-based activities. On weekdays, the majority of children (79%) reported spending <1 h outside before school while 43% of them indicated that they spent ≥2 h outside after school. On a typical weekend day, 73% of children reported spending ≥2 h outside. Overall daily outdoor time was 2.5 h on average. Children in South Africa (3.70 ± 1.86 h/day) and Brazil (3.46 ± 1.96 h/day) reported the highest overall daily outdoor time, while children in Portugal (1.75 ± 0.86 h/day) and China (1.87 ± 1.09 h/day) reported the lowest amount. Healthy and unhealthy dietary pattern scores are not reported in the table as they are meaningless for descriptive purposes, as by definition they have an overall mean of 0.00 ± 1.00 SD.
Table 1.
Descriptive characteristics of participants
| Total sample (N = 6229) | Boys (N = 2838) | Girls (N = 3391) | |
|---|---|---|---|
| Age (year) | 10.4 (0.6) | 10.5 (0.6) | 10.4 (0.6) |
| Highest parental education (%) | |||
| Did not complete high school | 19.7 | 19.3 | 20.1 |
| Completed high school or some college | 42.5 | 43.1 | 41.8 |
| Completed bachelor’s or postgraduate degree | 37.8 | 37.6 | 38.1 |
| BMI (kg/m2) | 18.4 (3.4) | 18.4 (3.4) | 18.4 (3.5) |
| Obesity (%)a | 12.4 | 15.1 | 10.1 |
| Moderate-to-vigorous physical activity (min/day) | 60.3 (24.8) | 69.8 (25.8) | 52.3 (20.9) |
| Screen time (h/day) | 2.9 (1.7) | 3.2 (1.8) | 2.6 (1.6) |
| Outdoor time (%) | |||
| Before school | |||
| <1 h | 78.8 | 78.6 | 79.0 |
| 1 h | 12.4 | 12.3 | 12.5 |
| 2 h | 4.5 | 4.8 | 4.3 |
| 3 h | 2.0 | 2.0 | 2.0 |
| 4 h | 1.1 | 1.1 | 1.0 |
| ≥5 h | 1.2 | 1.2 | 1.2 |
| After school | |||
| <1 h | 32.4 | 30.2 | 34.2 |
| 1 h | 24.5 | 23.2 | 25.6 |
| 2 h | 20.0 | 20.3 | 19.8 |
| 3 h | 11.1 | 12.2 | 10.2 |
| 4 h | 6.0 | 7.5 | 4.7 |
| ≥5 h | 6.0 | 6.6 | 5.5 |
| On weekends | |||
| <1 h | 12.4 | 11.5 | 13.2 |
| 1 h | 14.7 | 12.6 | 16.5 |
| 2 h | 21.4 | 20.0 | 22.6 |
| 3 h | 18.6 | 18.7 | 18.5 |
| 4 h | 14.3 | 15.3 | 13.4 |
| ≥5 h | 18.6 | 21.9 | 15.8 |
| Outdoor time (h/day) | |||
| Before school | 0.77 (0.75) | 0.77 (0.75) | 0.77 (0.74) |
| After school | 1.68 (1.33) | 1.79 (1.37) | 1.59 (1.28) |
| On weekends | 2.69 (1.54) | 2.85 (1.56) | 2.57 (1.51) |
| Overallb | 2.52 (1.45) | 2.64 (1.47) | 2.42 (1.42) |
BMI, body mass index.
aObesity defined according to the World Health Organization criteria.23
bOverall outdoor time (h/day) was calculated as [(5 × outdoor time on weekdays) + (2 × outdoor time on weekend days)]/7.
Data are shown as mean (standard deviation) unless otherwise indicated.
Results from the multilevel models showed that the largest proportion of total variance in dietary pattern scores occurred at the individual level, followed by the school and site levels (individual, school, site: 89%; 4%; 7% for healthy dietary pattern scores and 63%; 11%; 26% for unhealthy dietary pattern scores). We did not find significant sex interactions in the associations between outdoor time and dietary patterns across study sites. Therefore, boys and girls were pooled together for presentation. Also, only adjusted models are presented for subsequent analyses for clarity purposes. Of note, unadjusted associations were very similar to the fully adjusted models; adding covariates did not result in meaningful changes in the estimates reported. Adding active transportation time to go to school to the models also did not change the results (data not shown).
Table 2 shows the associations between outdoor time and dietary patterns of children participating in ISCOLE. After adjustment for covariates, all four outdoor time variables were significantly and positively associated with healthy dietary pattern scores, i.e. that greater time spent outdoors was related to a healthier dietary pattern. However, no association was found between outdoor time and unhealthy dietary pattern scores. Similar values were found in unadjusted models (results not shown).
Table 2.
Associations between outdoor time and dietary patterns of children (N = 6229)
| Outdoor time (h/day) | Healthy dietary pattern score | Unhealthy dietary pattern score | ||||
|---|---|---|---|---|---|---|
| β | SE | P | β | SE | P | |
| Before school | 0.05 | 0.02 | <0.001 | 0.01 | <0.01 | 0.46 |
| After school | 0.06 | 0.01 | <0.0001 | 0.01 | <0.01 | 0.38 |
| On weekends | 0.08 | 0.01 | <0.001 | <0.001 | <0.01 | 0.93 |
| Overalla | 0.08 | 0.01 | <0.001 | 0.02 | 0.01 | 0.22 |
SE, standard error.
aOverall outdoor time (h/day) was calculated as [(5 × outdoor time on weekdays) + (2 × outdoor time on weekend days)]/7.
Unstandardized beta coefficients are presented and models are adjusted for age, sex, highest level of parental education, moderate-to-vigorous physical activity, screen time and body mass index z-scores.
Table 3 presents the associations between overall daily outdoor time and dietary patterns of children by study site. Overall, significant and positive associations were observed between overall outdoor time and healthy dietary pattern scores (except for Brazil, Colombia, Kenya and South Africa). Associations between overall outdoor time and unhealthy dietary pattern scores were generally non-significant with the exception of India and USA. We did not find a significant World Bank classification25 of economic development-by-outdoor time interaction for dietary patterns, suggesting that the associations did not differ between sites (e.g. low versus high-income countries).
Table 3.
Associations between overall outdoor time and dietary patterns of children stratified by site (N = 6229)
| Outdoor time (h/day)a | Healthy dietary pattern score | Unhealthy dietary pattern score | ||||
|---|---|---|---|---|---|---|
| β | SE | P | β | SE | P | |
| Australia (Adelaide) | 0.17 | 0.03 | <0.0001 | 0.04 | 0.03 | 0.17 |
| Brazil (Sao Paulo) | 0.03 | 0.02 | 0.20 | 0.03 | 0.02 | 0.18 |
| Canada (Ottawa) | 0.16 | 0.03 | <0.0001 | 0.004 | 0.03 | 0.91 |
| China (Tianjin) | 0.18 | 0.04 | <0.0001 | 0.04 | 0.04 | 0.23 |
| Colombia (Bogotá) | 0.05 | 0.04 | 0.21 | 0.05 | 0.04 | 0.16 |
| Finland (Helsinki, Espoo and Vantaa) | 0.18 | 0.03 | <0.0001 | 0.04 | 0.03 | 0.15 |
| India (Bangalore) | 0.11 | 0.04 | <0.01 | 0.10 | 0.04 | <0.01 |
| Kenya (Nairobi) | 0.04 | 0.03 | 0.19 | 0.03 | 0.03 | 0.21 |
| Portugal (Porto) | 0.16 | 0.05 | <0.0001 | 0.03 | 0.04 | 0.44 |
| South Africa (Cape Town) | −0.05 | 0.03 | 0.05 | 0.04 | 0.03 | 0.21 |
| UK (Bath and North East Somerset) | 0.09 | 0.04 | 0.03 | 0.05 | 0.04 | 0.15 |
| USA (Baton Rouge) | 0.10 | 0.03 | <0.001 | 0.08 | 0.02 | <0.01 |
SE, standard error.
aOverall outdoor time (h/day) was calculated as [(5 × outdoor time on weekdays) + (2 × outdoor time on weekend days)]/7.
Unstandardized beta coefficients are presented and models are adjusted for age, sex, highest level of parental education, moderate-to-vigorous physical activity, screen time and body mass index z-scores.
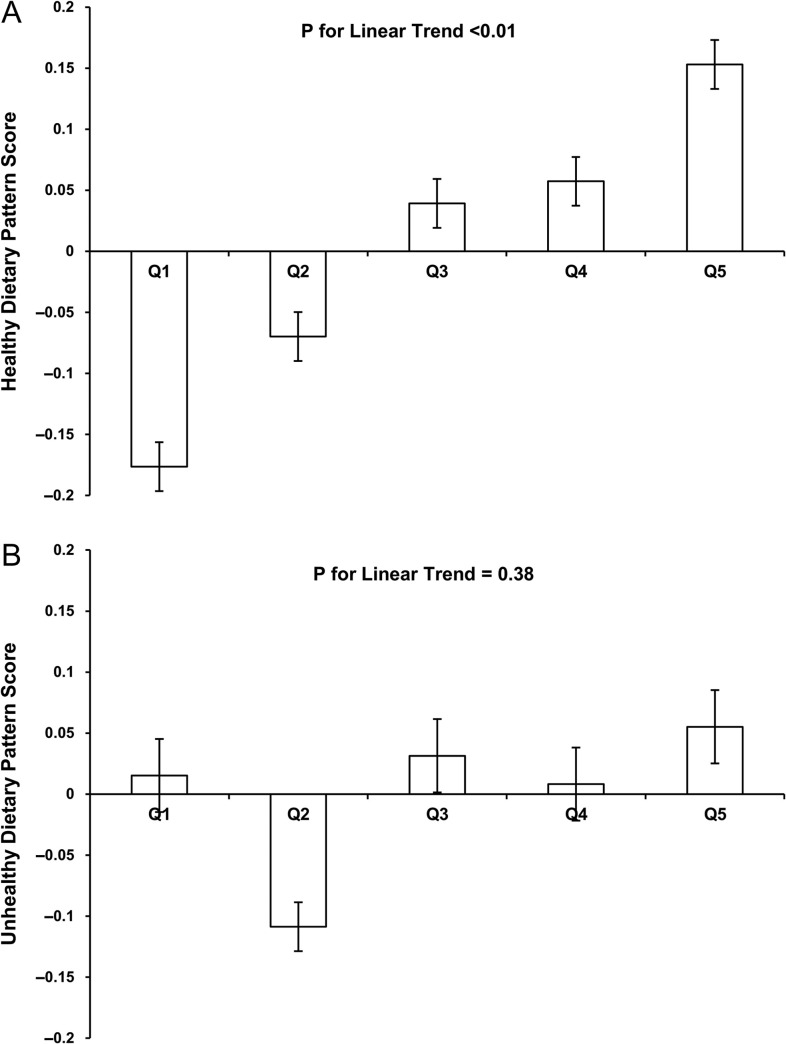
Figure 1A and B presents trends in dietary pattern scores across quintiles of overall daily outdoor time in the full study sample. There was a significant positive trend in healthy dietary pattern across levels of daily outdoor time (Fig. 1A). The association between unhealthy dietary pattern and overall outdoor time was not significant (Fig. 1B).
Fig. 1.
Trends in healthy (A) and unhealthy (B) dietary pattern scores across quintiles of overall daily outdoor time (N = 6229). (A) Q1:1.02 ± 0.02 h/day; Q2:1.55 ± 0.02 h/day; Q3:2.15 ± 0.02 h/day; Q4:3.00 ± 0.02 h/day; and Q5:4.87 ± 0.02 h/day. (B) Q1:1.02 ± 0.02 h/day; Q2:1.55 ± 0.02 h/day; Q3:2.15 ± 0.02 h/day; Q4:3.00 ± 0.02 h/day; and Q5:4.87 ± 0.02 h/day.
Discussion
Main finding of this study
To our knowledge, the present study was the first to examine the relationships between outdoor time and dietary patterns in children, representing such a broad range of levels in economic and human development. Collectively, we observed that children reporting a greater amount of time spent outside also reported healthier dietary patterns. However, no association was found between outdoor time and unhealthy dietary pattern scores. Similar associations between outdoor time and dietary patterns were observed across study sites and for boys and girls.
What is already known on this topic
Technological and societal changes have resulted in secular trends that have impacted the types of activities performed by children.5 Structured indoor achievement-oriented activities (e.g. competitive sports, excessive homework and music practice) seem to be replacing children’s outdoor free time.11 Electronic entertainment and parental concerns about child safety are also responsible for this secular shift from outdoor play to indoor play.5,8,9 Yet, whether this gradual change from outdoor to indoor time can have an influence on eating behaviors has been under-studied despite anecdotal evidence pointing towards unhealthy dietary patterns with easy access to energy-dense, nutrient-poor foods due to close proximity to the kitchen. Conversely, one may expect better eating behaviors with longer time spent outside on a daily basis. However, none of the claims have been empirically tested.
What this study adds
Findings from this multinational study of children suggest that healthier dietary patterns are associated with longer time spent outside. This finding is novel and adds to the many benefits associated with outdoor time.11 The fact that outdoor time was not associated with unhealthy dietary patterns suggests that unhealthy foods (e.g. fast food, soft drinks, sweets) may still be consumed by children who spend a lot of time outside, together with the consumption of more healthy foods (e.g. vegetables, fruit, whole grains). It is also plausible that children who spend more time outdoors have a higher overall energy intake to account for higher levels of energy expenditure. Further, although the positive relationship between outdoor time and healthy dietary pattern scores was statistically significant, the small effect size obtained suggests that a large proportion of the variance is explained by other factors. Nevertheless, the present data also suggest that more attention needs to be paid to the outdoor time-eating behavior relationship in future studies.
Future work should build on these findings to provide a more in-depth assessment of dietary intake including portion size, setting, and/or context (e.g. if the food was brought from home or purchased at a store/restaurant, and/or eaten alone or with friends). The quality of available food may also play an important role. For example, if a parent is in the habit of buying energy-dense, nutrient-poor foods, the home environment may play an important role in consumption. In this case, interventions would need to focus on parenting practices rather than child behavior. Coleman et al.26 examined physical activity and eating opportunities in the after-school environment in children and concluded that the quality of after-school programs should be improved by providing fruits and vegetables as snacks, offering more free play activities, and training the after-school staff to promote and model MVPA and healthy eating in and out of the after-school setting. Additionally, proximity to natural outdoor settings (e.g. green spaces) versus living in a neighborhood marked by high levels of physical disorder or crime may lead to different effects on lifestyle behaviors. Future studies should use GPS and geographic information systems in order to provide greater insights into the objective characteristics of outdoor environments.
Future work should also quantify indoor time, and examine impact of the ratio of indoor versus outdoor time on dietary patterns of children. Unfortunately, we are not aware of any large datasets that include a measure of indoor versus outdoor time in children. Previous work on child-reported preferences for outdoor play suggests that interventions aimed at increasing outdoor time are well received by children.27,28 Nevertheless, some public health campaigns have recommended to keep children indoors for almost the entire day for safety concerns, i.e. to avoid sun exposure and melanoma risk,29 traffic-related air pollution during rush-hour periods,30 or communicable diseases (e.g. West Nile virus via mosquitos).31 Interestingly, a diverse group of partners, stakeholders and researchers recently released an evidence-informed Position Statement on active outdoor play for children.32 It states that access to active play in nature and outdoors, with its risks, is essential for healthy child development, and the group also recommended to increase children’s opportunities for self-directed play outdoors in all settings. By continuing to show that outdoor time is also associated with healthy behaviors, we hope to reach a more balanced perspective to health promotion with regard to outdoor play.
This study included sites from countries varying widely in levels of economic and human development. We did not find a significant World Bank classification of economic development-by-outdoor time interaction for dietary patterns, suggesting that the associations were similar across study sites. We also observed that the associations between outdoor time and dietary patterns were similar for boys and girls. Such findings suggest that interventions aimed at increasing outdoor time could be generalized across different settings and demographic subgroups.
Although research in this specific area has been limited, time-use is an established methodological approach and can provide contextual information about children’s use of time away from home and school.33 Examples include the Harmonized European Time Use Survey and the Millennium Cohort Study in the UK. Future investigations should continue to examine time-use patterns of children to better inform policies and intervention strategies.
Limitations of this study
First, the cross-sectional nature of the data precludes inferences about causality or temporality. Second, self-reported measures of outdoor time and dietary patterns were used, which are prone to social desirability responding and recall bias. This also includes an underestimation of overall outdoor time because the upper category (i.e. ≥5 h) was used as 5 h for analysis. Future research should also test the psychometric properties of the outdoor time questions. Third, ISCOLE was not designed to provide nationally representative data and therefore the degree to which the results are generalizable to the studied countries is not known. Future research should also examine the relationship between outdoor time and dietary patterns in rural areas to determine if differences exist. Fourth, the narrow age range limits our ability to extrapolate our findings to other age groups and it is possible that different patterns would be observed in adolescents or adults for example. Fifth, only a FFQ was used in ISCOLE and information on energy intake (kcal) or context was not available. Finally, the potential confounding effects of unmeasured variables cannot be discounted.
Conclusion
Findings from this study show that greater time spent outside was positively associated with a healthier dietary pattern in this large multinational study of children. However, no association was found between outdoor time and unhealthy dietary pattern scores, suggesting that although longer time spent outdoor was associated with healthier dietary patterns it was not also related to a lower frequency of consumption of unhealthy foods such as fast foods, soft drinks or sweets. Finally, similar associations between outdoor time and dietary patterns were observed across study sites. Further studies using objective measures (e.g. GPS and geographic information systems) and longitudinal research designs are needed to better understand the prospective associations among outdoor time and dietary patterns in children. Future work should also examine mechanisms linking outdoor time with dietary patterns, and include 24-h time-use data, to have a broader picture of overall behaviors and their influence on health outcomes.
Acknowledgements
We wish to thank the ISCOLE External Advisory Board and the ISCOLE participants and their families who made this study possible. The ISCOLE Research Group includes: Coordinating Center, Pennington Biomedical Research Center: Peter T. Katzmarzyk, PhD (Co-PI), Timothy S. Church, MD, PhD (Co-PI), Denise G. Lambert, RN (Project Manager), Tiago Barreira, PhD, Stephanie Broyles, PhD, Ben Butitta, BS, Catherine Champagne, PhD, RD, Shannon Cocreham, MBA, Kara D. Denstel, MPH, Katy Drazba, MPH, Deirdre Harrington, PhD, William Johnson, PhD, Dione Milauskas, MS, Emily Mire, MS, Allison Tohme, MPH, Ruben Rodarte MS, MBA; Data Management Center, Wake Forest University: Bobby Amoroso, BS, John Luopa, BS, Rebecca Neiberg, MS, Scott Rushing, BS; Australia, University of South Australia: Timothy Olds, PhD (Site Co-PI), Carol Maher, PhD (Site Co-PI), Lucy Lewis, PhD, Katia Ferrar, B Physio (Hon), Effie Georgiadis, BPsych, Rebecca Stanley, BAppSc (OT) Hon; Brazil, Centro de Estudos do Laboratório de Aptidão Física de São Caetano do Sul (CELAFISCS): Victor Keihan Rodrigues Matsudo, MD, PhD (Site PI), Sandra Matsudo, MD, PhD, Timoteo Araujo, MSc, Luis Carlos de Oliveira, MSc, Luis Fabiano, BSc, Diogo Bezerra, BSc, Gerson Ferrari, MSc; Canada, Children’s Hospital of Eastern Ontario Research Institute: Mark S. Tremblay, PhD (Site Co-PI), Jean-Philippe Chaput, PhD (Site Co-PI), Priscilla Bélanger, MA, Mike Borghese, MSc, Charles Boyer, MA, Allana LeBlanc, PhD, Claire Francis, MSc,Geneviève Leduc, PhD; China, Tianjin Women’s and Children’s Health Center: Pei Zhao, MD (Site Co-PI), Gang Hu, MD, PhD (Site Co-PI), Chengming Diao, MD, Wei Li, MD, Weiqin Li, MSc, Enqing Liu, MD, Gongshu Liu, MD, Hongyan Liu, MD, Jian Ma, MD, Yijuan Qiao, MD, Huiguang Tian, PhD, Yue Wang, MD, Tao Zhang, MSc, Fuxia Zhang, MD; Colombia, Universidad de los Andes: Olga Sarmiento, MD, PhD (Site PI), Julio Acosta, Yalta Alvira, BS, Maria Paula Diaz, Rocio Gamez, BS, Maria Paula Garcia, Luis Guillermo Gómez, Lisseth Gonzalez, Silvia Gonzalez, RD, Carlos Grijalba, MD, Leidys Gutierrez, David Leal, Nicolas Lemus, Etelvina Mahecha, BS, Maria Paula Mahecha, Rosalba Mahecha, BS, Andrea Ramirez, MD, Paola Rios, MD, Andres Suarez, Camilo Triana; Finland, University of Helsinki: Mikael Fogelholm, ScD (Site-PI), Elli Hovi, BS, Jemina Kivelä, Sari Räsänen, BS, Sanna Roito, BS, Taru Saloheimo, MS, Leena Valta; India, St. Johns Research Institute: Anura Kurpad, MD, PhD (Site Co-PI), Rebecca Kuriyan, PhD (Site Co-PI), Deepa P. Lokesh, BSc, Michelle Stephanie D’Almeida, BSc, Annie Mattilda R, MSc, Lygia Correa, BSc, Vijay Dakshina Murthy, BSc; Kenya, Kenyatta University: Vincent Onywera, PhD (Site Co-PI), Mark S. Tremblay, PhD (Site Co-PI), Lucy-Joy Wachira, PhD, Stella Muthuri, PhD; Portugal, University of Porto: Jose Maia, PhD (Site PI), Alessandra da Silva Borges, BA, Sofia Oliveira Sá Cachada, Msc, Raquel Nichele de Chaves, MSc, Thayse Natacha Queiroz Ferreira Gomes, PhD, MSc, Sara Isabel Sampaio Pereira, BA, Daniel Monteiro de Vilhena e Santos, PhD, Fernanda Karina dos Santos, MSc, Pedro Gil Rodrigues da Silva, BA, Michele Caroline de Souza, MSc; South Africa, University of Cape Town: Vicki Lambert, PhD (Site PI), Matthew April, BSc (Hons), Monika Uys, BSc (Hons), Nirmala Naidoo, MSc, Nandi Synyanya, Madelaine Carstens, BSc(Hons); United Kingdom, University of Bath: Martyn Standage, PhD (Site PI), Sean Cumming, PhD, Clemens Drenowatz, PhD, Lydia Emm, MSc, Fiona Gillison, PhD, Julia Zakrzewski, PhD; United States, Pennington Biomedical Research Center: Catrine Tudor-Locke, PhD (Site-PI), Ashley Braud, Sheletta Donatto, MS, LDN, RD, Corbin Lemon, BS, Ana Jackson, BA, Ashunti Pearson, MS, Gina Pennington, BS, LDN, RD, Daniel Ragus, BS, Ryan Roubion, John Schuna, Jr., PhD; Derek Wiltz. The ISCOLE External Advisory Board includes Alan Batterham, PhD, Teesside University, Jacqueline Kerr, PhD, University of California, San Diego; Michael Pratt, MD, Centers for Disease Control and Prevention, Angelo Pietrobelli, MD, Verona University Medical School.
Funding
This work was supported by The Coca-Cola Company. With the exception of requiring that the study be global in nature, the funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the article and decision to submit the article for publication.
References
- 1. Moodie R, Stuckler D, Monteiro C et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013;381:670–9. [DOI] [PubMed] [Google Scholar]
- 2. Ding D, Lawson KD, Kolbe-Alexander TL et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 2016;388:1311–24. [DOI] [PubMed] [Google Scholar]
- 3. Lobstein T, Jackson-Leach R, Moodie ML et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385:2510–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hallal PC, Andersen LB, Bull FC et al. , Lancet Physical Activity Series Working Group . Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. [DOI] [PubMed] [Google Scholar]
- 5. Bassett DR, John D, Conger SA et al. Trends in physical activity and sedentary behaviors of United States youth. J Phys Act Health 2015;12:1102–11. [DOI] [PubMed] [Google Scholar]
- 6. Singh A. Contexts of childhood and play: exploring parental perceptions. Childhood 2012;19:235–50. [Google Scholar]
- 7. Wolf Fritz R, Smyrni K, Roberts K. The challenges of bringing the waldkindergarten concept to North America. Child Youth Environ 2014;24:215–27. [Google Scholar]
- 8. Carver A, Timperio A, Crawford D. Playing it safe: the influence of neighbourhood safety on children’s physical activity. A review. Health Place 2008;14:217–27. [DOI] [PubMed] [Google Scholar]
- 9. Larson LR, Green GT, Cordell HK. Children’s time outdoors: results and implications of the National Kids Survey. J Park Recreat Adm 2011;29:1–20. [Google Scholar]
- 10. Skår M, Krogh E. Changes in children’s nature-based experiences near home: from spontaneous play to adult-controlled, planned and organised activities. Child Geogr 2009;7:339–54. [Google Scholar]
- 11. Gray C, Gibbons R, Larouche R et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int J Environ Res Public Health 2015;12:6455–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katzmarzyk PT, Barreira TV, Broyles ST et al. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health 2013;13:900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Currie C, Gabhainn SN, Godeau E et al. Inequalities in Children’s Health: HBSC International Report from the 2005/2006 Survey. Copenhagen, Denmark: WHO Regional Office for Europe, 2008. Health Policy for Children and Adolescents, No. 5. [Google Scholar]
- 14. Mikkilä V, Vepsäläinen H, Saloheimo T et al. An international comparison of dietary patterns in 9-11-year-old children. Int J Obes Suppl 2015;5:S17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vereecken CA, Maes L. A Belgian study on the reliability and relative validity of the Health Behaviour in School-Aged Children food-frequency questionnaire. Public Health Nutr 2003;6:581–8. [DOI] [PubMed] [Google Scholar]
- 16. Tudor-Locke C, Barreira TV, Schuna JM Jr et al. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nutr Phys Act 2015;12:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tudor-Locke C, Barreira TV, Schuna JM Jr et al. Fully automated waist-worn accelerometer algorithm for detecting children’s sleep-period time separate from 24-h physical activity or sedentary behaviors. Appl Physiol Nutr Metab 2014;39:53–7. [DOI] [PubMed] [Google Scholar]
- 18. Barreira TV, Schuna JM Jr, Mire EF et al. Identifying children’s nocturnal sleep using a 24-h waist accelerometry. Med Sci Sports Exerc 2015;47:937–43. [DOI] [PubMed] [Google Scholar]
- 19. Mark AE, Janssen I. Dose-response relation between physical activity and blood pressure in youth. Med Sci Sports Exerc 2008;40:1007–12. [DOI] [PubMed] [Google Scholar]
- 20. Evenson KR, Catellier DJ, Gill K et al. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–65. [DOI] [PubMed] [Google Scholar]
- 21. U.S. Centers for Disease Control and Prevention Youth Risk Behavior Surveillance System (YRBSS, 2012) www.cdc.gov/HealthyYouth/yrbs/.
- 22. Chaput JP, Katzmarzyk PT, LeBlanc AG et al. Associations between sleep patterns and lifestyle behaviors in children: an international comparison. Int J Obes Suppl 2015;5:S59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. de Onis M, Onyanga AW, Borghi E et al. Development of a WHO growth reference for school-aged children and adolescents. Bull WHO 2007;85:660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 1997;53:983–97. [PubMed] [Google Scholar]
- 25. World Bank World Development Indicators. Washington, DC: The World Bank, 2012. [Google Scholar]
- 26. Coleman KJ, Geller KS, Rosenkranz RR et al. Physical activity and healthy eating in the after-school environment. J Sch Health 2008;78:633–40. [DOI] [PubMed] [Google Scholar]
- 27. Glenn N. Meanings of play among children. Childhood 2013;20:185–99. [Google Scholar]
- 28. Miller E, Kuhaneck H. Children’s perceptions of play experiences and play preferences: a qualitative study. Am J Occup Ther 2008;62:407–15. [DOI] [PubMed] [Google Scholar]
- 29. Whiteman DC, Whiteman CA, Green AC. Childhood sun exposure as a risk factor for melanoma: a systematic review of epidemiological studies. Cancer Causes Control 2001;12:69–82. [DOI] [PubMed] [Google Scholar]
- 30. Jerrett M, Shankardass K, Berhane K et al. Traffic-related air pollution and asthma onset in children: a prospective cohort study with individual exposure measurement. Environ Health Perspect 2008;116:1433–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. HealthLinkBC West Nile Virus http://www.healthlinkbc.ca/healthfiles/pdf/hfile88.pdf (12 March 2018, date last accessed).
- 32. Tremblay MS, Gray C, Babcock S et al. Position statement on active outdoor play. Int J Environ Res Public Health 2015;12:6475–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Keung A. Children’s time and space In: Bradshaw J (ed). The Well-being of Children in the UK, 4th edn Bristol, UK: Policy Press, 2016:149–78. [Google Scholar]